


© Crown copyright 2024
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3.
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at www.gov.uk/official-documents.
Any enquiries regarding this publication should be sent to us at [email protected].
ISBN 978-1-5286-4685-7
E03066671 05/24
This chapter examines whether government discharged its fundamental responsibility to ensure that treatment given through the National Health Service was safe. It looks at how government responded to the risk of viral infections in blood and blood products and considers whether actions could have been taken earlier and more effectively.
May 1975 despite Hepatitis B risk, “Dr Doctor” letter allows blood collections from prisons.
15 September 1980 Dr Walford describes the risks from non-A non-B Hepatitis in a DHSS minute: “can be rapidly fatal … or can lead to progressive liver damage”
16 July 1982 Dr Gunson warns civil servants in DHSS of the possibility of AIDS being transmitted through blood.
May 1983 “no conclusive proof ” first used in line to take drafted for the Prime Minister.
9 May 1983 Dr Galbraith writes to DHSS recommending the temporary withdrawal of US blood products. His paper is not brought to the attention of ministers or the CMO.
June 1983 Council of Europe’s Committee of Ministers recommends taking “all necessary steps and measures” to help avoid AIDS.
1 September 1983 First AIDS donor leaflet is distributed to RTCs to be reviewed after three months.
29 January 1985 Expert Advisory Group on AIDS meets for the first time.
February 1985 Second AIDS donor leaflet.
Sir Donald Acheson Chief Medical Officer (1983 - 1991)
Professor Arthur Bloom chairman, UKHCDO
Kenneth Clarke Minister of State for Health (March 1982 - September 1985)
Dr John Craske virologist and chairman, UKHCDO’s Hepatitis Working Party (from 1977)
Norman Fowler Secretary of State for Health and Social Services
Dr Spence Galbraith director, Communicable Disease Surveillance Centre
Lord Simon Glenarthur (Lords) Parliamentary Under-Secretary of State for Health (June 1983 - March 1985)
Dr Harold Gunson consultant adviser to the Chief Medical Officer
Dr Archibald McIntyre principal medical officer, SHHD
John Patten (Commons) Parliamentary Under-Secretary of State for Health (June 1983 - September 1985)
Dr Diana Walford principal medical officer, DHSS
Sir Henry Yellowlees Chief Medical Officer (1973 - 1983)
ACVSB Advisory Committee on the Virological Safety of Blood
EAGA Expert Advisory Group on AIDS
MRC Medical Research Council
SHHD Scottish Home and Health Department
RTC Regional Transfusion Centre
As a matter of principle, a first duty of the state is to look after the safety of its population. That duty must extend to the safety of patients receiving blood or blood products.[1]
Put another way, and with specific reference to the role of the Secretary of State for Health (in the words of one who held that office between 2009 and 2010), “The job as I see it is to get the best possible health care – the safest, highest quality health care – for the people of England. And to protect them from risks. I guess that’s it really.”[2] That applies, of course, with equal force to the people of Scotland, Wales, and Northern Ireland.
It was the responsibility of the Department of Health and Social Security (“DHSS”),[3] and of the Secretary of State for Health, and of those in positions of equivalent responsibility in Scotland, Wales and Northern Ireland, to ensure, as much as possible, that treatment given through the National Health Service was safe.[4] Norman Fowler, now Lord Fowler, who was the Secretary of State for Health and Social Services for nearly six years during the 1980s, described the DHSS’s role as being to keep up the review of public health, and take any action necessary to try to preserve it. Public health was, he said, “one of the most important things that we had to do … an absolutely vital issue.”[5]
Ensuring the safety of the public from risks to their health is not just a question of taking steps to protect them. Kenneth Clarke, now Lord Clarke, who was Minister of State for Health between March 1982 and September 1985, accepted in evidence that an emerging potential threat to public health needs to be dealt with speedily.[6] The right steps should not only be taken – but taken without any unreasonable delay.
This chapter examines whether government discharged this fundamental responsibility.
Some specific and significant aspects of government activity (or inactivity) are addressed in other chapters of this Report: the failure to achieve self-sufficiency; failures in relation to the licensing of blood products, including the decision in July 1983 not to ban the importation of factor concentrates; whether there was delay in the introduction of HIV screening of blood donations; whether there was delay in the introduction of Hepatitis C screening of blood donations; the failures of decision-making in relation to surrogate testing for both HIV and Hepatitis C; government responsibilities in matters relating to the organisation and activities of the blood services and guidance on transfusion practice; all these are addressed separately elsewhere in the Report.
This chapter explores the following issues in particular: departmental policy on the collection of blood from prisons; the government’s response to the emergence of AIDS as a threat to the safety of blood and blood products; the response – or lack of it – to the letter and paper from Dr Spence Galbraith in May 1983; the response – or lack of it – to the Council of Europe’s Committee of Ministers’ June 1983 recommendations; the adoption of the “no conclusive proof” line; the production of the first and second AIDS donor leaflets; the role of ministers and of the Chief Medical Officer (“CMO”) during this period; the use of committees and working groups; the actions of the Scottish Home and Health Department (“SHHD”) at this time; and decision-making with regard to Wales and Northern Ireland.
It does not examine the governments’ responses to claims, made later, that governments had failed in their basic duty to keep the public safe and in doing so to act with all due speed. The chapters in volumes 6 and 7 of this Report explore those responses.
It was well known to government in the early 1970s (and indeed much earlier[7]) that treatment with blood and blood products carried a risk of transmission of viral hepatitis. The seriousness of Hepatitis B was also well understood. Not only did the DHSS and SHHD have their own in-house medical expertise[8] to enable them to understand the risks of viral transmission but they had access to a range of external expertise through the multiplicity of committees and working groups that existed at various stages in the 1970s and 1980s.
Dr Diana Walford confirmed that throughout the period of time she was a principal medical officer in Med SEB[9] (ie from the end of 1979 to the end of 1983) she knew both that the transmission of non-A non-B Hepatitis (“NANBH”) through blood products and blood was a significant problem, and that it had the potential to have serious consequences in terms of chronic liver disease.[10] There was a general understanding too, which she shared, that the larger the pool size the greater the risk. She had a sense that not everyone within the DHSS was conscious of the fact that NANBH could potentially give rise to severe chronic disease; this was one of the reasons why she spoke about it “really quite forcibly” in her minute of 15 September 1980, where she wrote that “This form of hepatitis can be rapidly fatal (particularly when acquired by patients with pre-existing liver disease) or can lead to progressive liver damage. It can also result in a chronic carrier state, thus increasing the pool of these viruses in the community.”[11] Dr Walford deliberately copied her minute “pretty widely”: it was addressed to John Harley in HS1A[12] and copied not only to her boss (Dr Ronald Oliver) but to Peter Wormald (John Harley’s boss), Stanley Godfrey (principal grade civil servant in HS1), Mr Hart (head of supply division) and others within the DHSS.[13]
No one receiving this minute could have been under any illusion from this point onwards about the seriousness of NANBH. No steps, however, were taken by the DHSS to ensure that the serious nature of this condition was also properly understood by doctors, patient cohorts or representative bodies (such as the Haemophilia Society) or the public.[14]
AIDS would soon emerge, in 1982, as a further threat to the safety of the blood supply and the safety of blood products. As detailed later in this chapter, the DHSS was well aware from mid 1982 of the possibility of transmission of AIDS through blood.
The ministerial structure within the DHSS, as with other Westminster government departments at the time, involved three tiers of ministers: the Secretary of State, the Minister of State, and the Parliamentary Under-Secretary of State.
The role of Secretary of State for Health and Social Services had been filled by Barbara Castle (1974-1976) and David Ennals (1976-1979). Following the Conservative election victory in May 1979 Patrick Jenkin became Secretary of State. Norman Fowler took over in September 1981 (succeeding Patrick Jenkin) and remained in post until June 1987.[15]
David Owen was Minister of State for Health between 1974 and 1976, followed by Roland Moyle (1976-1979); their role is considered further in the chapter on Self-Sufficiency. Gerard Vaughan became Minister of State for Health in 1979 and was succeeded by Kenneth Clarke in March 1982; Kenneth Clarke remained in that position until September 1985.[16]
There were two Parliamentary Under-Secretaries of State with responsibility for health: one in the House of Commons and one in the House of Lords.[17] Geoffrey Finsberg was the Parliamentary Under-Secretary of State in the House of Commons from September 1981 to June 1983, replacing George Young, and was succeeded by John Patten (later Lord Patten) in June 1983 who remained in post until September 1985. Lord David Trefgarne was the Parliamentary Under-Secretary of State in the House of Lords from April 1982 to June 1983; he was succeeded by Lord Simon Glenarthur from June 1983 to March 1985.
Lord Fowler told the Inquiry that rapid ministerial change was very common and too rapid.[18]
Ministers below the level of Secretary of State had particular areas of responsibility allocated to them. Blood and blood products fell under the responsibility of Geoffrey Finsberg during his time in post; they then became the responsibility of Lord Glenarthur in June 1983. For a short period of time in 1983 – from 9 May 1983, when a general election was called, to 9 June 1983 when the election took place – there was a period of “purdah”[19] during which, to Lord Trefgarne’s recollection, he was responsible for the day-to-day control of the DHSS, although it was made clear to him by the Permanent Secretary (Sir Kenneth Stowe) that he should not make any substantive new policy decisions during that period.[20]
The Chief Medical Officer[21] (“CMO”) was Sir Henry Yellowlees, who had held that role since 1973, and then Dr (later Sir) Donald Acheson, who took over in late 1983 (with a three month period of overlap). Sir Henry was described by Lord Fowler as a somewhat distant character with whom he did not have regular meetings and as someone who “wasn’t really in the public health, general public health, area”.[22] Lord Clarke was less flattering still.[23]
There were two parallel civil service hierarchies within the DHSS at this time: a medical (and scientific) hierarchy, which ultimately reported to the CMO, and an administrative hierarchy which would take the lead on policy development, financial matters and support for ministers and which would report through the conventional civil service structure and ultimately to the Permanent Secretary.[24]
HS1 (divided into HS1A and HS1B) was a division in the administrative hierarchy which had responsibility for, amongst other health services, the blood transfusion services, blood supply and blood safety.[25] As at 1983 HS1A took the lead on AIDS-related problems within the DHSS.[26] There were two medical branches of particular relevance: Med SEB (whose responsibility encompassed blood and blood products) and Med IMCD (with responsibility for the surveillance of infectious/communicable diseases). It was Med IMCD which would receive data gathered through the Public Health Laboratory Service (“PHLS”) and sent to the Communicable Disease Surveillance Centre (“CDSC”).
The senior medical officer with particular responsibility for blood and blood products generally attended the annual meetings of the UK haemophilia centre directors, and thus the DHSS would have a good insight into trends and patterns of treatment for bleeding disorders. Thus, for example, the medical officer attending the United Kingdom Haemophilia Centre Directors’ Organisation (“UKHCDO”) meeting on 30 September 1980 – by this time Dr Walford – would know about the substantial usage of commercial concentrates (because Dr Charles Rizza gave a presentation on his report on the 1979 annual returns); would hear the expression of concern from Professor James Stewart as to the increasing usage of commercial Factor 8; would hear the discussion of Dr John Craske’s report of the findings of the Hepatitis Working Party and reference to the results of liver biopsy studies; would glean that first-time exposure to large pooled Factor 8 concentrates resulted in many cases of hepatitis; and would learn that there was an increasing number of people with haemophilia on prophylactic therapy.[27] Dr Walford indicated that the UKHCDO represented, for the DHSS, “the group” with relevant expertise, and that on questions of treatment and risks and benefits the DHSS would very much be guided by and defer to the UKHCDO’s views.[28]
It is important to record that not all material generated within the DHSS would be seen by ministers. Civil servants had to decide whether or not documents or information should be sent to ministers. If they exercised their judgement to do so, the material would be sent to the minister’s private office. There would then be a judgement by the private office as to whether the material actually needed to be seen by the minister. Where there was a change of minister, the incoming minister would not necessarily be briefed about developments that had occurred earlier and on decisions which had been made by one of their predecessors.
In 1971-1972, the United Kingdom introduced screening for Hepatitis B among blood donors.[30] Around this time, evidence emerged suggesting a higher prevalence of Hepatitis B in the UK’s prison populations compared to the general population, mirroring findings observed in the US.
The following year, in 1971, the World Health Organization (“WHO”) published A Guide to the Formation and Operation of a Transfusion Service[31]which identified prisons as optimal locations for blood collection.[32]
At a National Blood Transfusion Service (“NBTS”) regional transfusion directors’ (“RTDs”) meeting on 6 October 1971, chaired by Dr William d’A Maycock and attended by officials from the DHSS, it was confirmed that all regional transfusion centres (“RTCs”) in the UK were involved in collecting donations from prisons, borstals, or equivalent institutions. It was noted at the meeting that the American Red Cross had stopped collecting blood from donors in “correctional institutions” due to the incidence of Hepatitis B; two RTDs reported a greater incidence of Hepatitis B positive donations among prisoners than among other donors; and it was recognised that there was great difficulty in following up prisoners or keeping records of prison donors. The meeting agreed that prison governors should be asked to prevent known drug users from volunteering as donors but that before deciding whether to stop collecting blood from such institutions, more information should be obtained about the association with cases of serum hepatitis.[33]
Despite this indication that prison donation might not be safe, throughout the 1970s and early 1980s blood collection from prisons was a common practice in the UK. The Annual Reports on the Work of the Prison Department noted the practice of blood donation sessions in prisons throughout this period.[34] Similarly, in Scotland this practice was briefly noted in the SHHD’s annual prison reports presented to Parliament for the years 1978,[35] 1979,[36] and 1980,[37] indicating its ongoing nature and the significance attached to prisons as sources for blood donations during this period.
At a meeting of RTDs on 26 September 1973, again chaired by Dr Maycock and attended by representatives from the DHSS and from the SHHD, the primary focus was the prevalence of the Australian antigen (HBsAg) in blood donors. A key concern raised was the higher incidence of “antigenaemia”[38] in prisoners compared to the general public. The minutes recorded that the RTDs debated whether to continue blood collection in prisons, with half of them arguing against continuing to bleed prisoners and half advocating for continuing blood collection in prisons at least until the statistical significance of the figures was thoroughly examined. No decision was reached although it was resolved that any decision to discontinue bleeding prisoners would necessitate the DHSS first informing the Home Office, who supported the practice.[39] A report prepared for the meeting observed that “It seems clear that the incidence of antigenaemia among donors who are inmates of prisons, borstals etc. is higher than among other donors.”[40]
Shortly thereafter, on 4 October 1973, there was a meeting of the Scottish National Blood Transfusion Service (“SNBTS”) directors, chaired by Dr Albert Bell of the SHHD, during which it was reported that Dr Maycock had presented data on the incidence of Au-positive blood[41] among prisoner donors and that “English directors were considering withdrawal of prison sessions.”[42]
Subsequently, on 24 April 1974, the RTDs met again, with Dr Bell representing the SHHD and six representatives attending from the DHSS. They discussed an article from The Sunday Times regarding the North London Blood Transfusion Centre’s decision to suspend the use of blood from donors from tropical areas, who were considered a high risk group due to a higher incidence of Hepatitis B antigen. The RTDs agreed to form an ad hoc committee to determine which donor groups required special consideration and whether any groups should be excluded entirely from blood donation.[43] This might have afforded the opportunity for all concerned to agree to the exclusion of prisoners as donors, but this did not happen and the collection from prisoners continued in most RTCs.
In July 1974 a document prepared for RTDs in England and Wales reported the frequency of Hepatitis B in various donor groups, including new general public and factory donors, Armed Forces personnel, and inmates from prisons and borstals.[44] The incidence of Hepatitis B antigen in donations from new general public and factory donors in 1973 was relatively low,[45] whereas in prisons and similar institutions, it was approximately five times higher.[46]
In February 1975, the Advisory Group on Testing for the Presence of Hepatitis B Surface Antigen (the Maycock Group), established in 1970, produced a draft of their second report. This included findings from a sub-group formed in May 1974, which specifically considered populations with a high incidence of HBsAg. The appendix to the draft report addressed blood collection in prisons, acknowledging the “relatively high risk” of hepatitis transmission but suggesting that it was comparable to risks in other groups, such as drug addicts, who were less easy to identify in advance than prisoners. The sub-group recommended not discontinuing blood collection in prisons, provided that all donations underwent one of the more sensitive tests, such as RPH or RIA.[47] Two civil servants from the DHSS (one of whom was Dr Sheila Waiter, a medical officer) were secretaries to the Maycock Group and Dr Maycock, chair of both the overall group and the sub-group, was, of course, the consultant adviser on blood transfusion to the CMO.
This appendix was not included in the final version of the report published in September 1975.[48] Instead, in May 1975 the conclusions reached by the sub-group were communicated by means of a “Dear Doctor” letter from Dr Yellowlees, the CMO for England, to all regional medical officers in England. This letter repeated the sub-group’s advice that, despite the higher risk of Hepatitis B in prison donations, collections could continue if all donations were subjected to more sensitive Hepatitis B tests.[49] The deeply flawed logic in this letter (and also in the advice on which it drew) – namely, its reliance on the fact that there were other high risk groups such as drug users as a reason for continuing to collect from prisons – is discussed in the chapter on Response to Risk by the Blood Services.
SHHD and SNBTS received[50] the CMO’s letter but, in subsequent discussions, focused their attention more on donors from high-risk geographical areas than on prison donations. Dr Graham Scott, Deputy CMO at the SHHD, noted in a memorandum on 8 May 1975 that the Maycock Group had established a small working group to consider “geographical and racial factors” in blood donation which had produced recommendations in an appendix for an early draft of their report. However, Dr Scott revealed that, upon further deliberation by the Advisory Group, it was believed that including such an appendix could be inflammatory, which led to its omission from the final report.[51] In response to Dr Yellowlees’ letter, Dr Scott intended to ask his colleague Dr Archibald McIntyre[52] to discuss the recommendations with Major-General Hugh Jeffrey,[53] and to assess the practices in Scotland at that time, especially concerning the more sensitive methods of antigen screening.[54] Subsequently, on 16 May 1975, Dr McIntyre wrote to Major-General Jeffrey; the focus of his letter was the question of donations from high-risk malarial and hepatitis areas.[55] There was no mention of blood donations from prisoners. The SNBTS directors reviewed the CMO’s letter during their meeting on 11 June 1975, but the discussions were, again, centred on blood donors from endemic malarial areas, without any recorded deliberation on the continuation of blood collections from prisoners.[56]
Unsurprisingly, given the contents of the Dear Doctor letter from the CMO, blood donations from prisoners continued to be collected in most RTCs in the UK, as described further in the chapter on Blood Services and Addressing Risk: Regional Transfusion Centres.
In February 1980, the DHSS produced a note regarding the establishment of an Advisory Group on Hepatitis, in which it recognised that certain groups, including drug addicts and the prison population, exhibited significantly higher rates of infection.[57] However, no action was taken by the Advisory Group, which began to meet in October 1980, in relation to this issue.
In 1982 the Medicines Inspectorate of the DHSS began to examine the practice of collecting blood from prisons and borstals during their visits to transfusion centres and other facilities in Scotland. Their scrutiny included an inspection of the Dundee RTC on 25 March 1982. The inspectors’ report raised significant concerns about the practice of collection from prisons and borstals, noting the absence of prison medical officers in assessing the suitability of donors, the increased risk of infection within the prison population, and the potential unreliability of answers to pre-donation questionnaires from such donors, whose motivations were questionable.[58] Similarly, during their visits to the Edinburgh and Southeast Scotland BTS, the inspectors questioned the appropriateness and necessity of collecting blood from donors in prisons and borstals.[59]
The issue of prison donations continued to be a point of discussion in Scotland in 1982, with Dr John Cash writing to John Watt that they needed “to consider, formally, in the not too distant future, the question of Sessions in Prisons” and whether “we should abandon this practice”.[60] It was discussed at a meeting of the SNBTS directors on 29 March 1983, attended by representatives of SHHD: blood collection sessions were being held in penal institutions across all regions, though some planned to review this practice in their respective regions.[61] Despite these discussions, the directors did not agree on a unified future policy.
On 12 April 1983, Dr Cash wrote to David Haythornthwaite of the DHSS Medicines Division conveying the lack of consensus among the SNBTS directors on the question of donor sessions at prisons and borstals.[62] On 6 May 1983 John Davies, Assistant Secretary in the SHHD, sent a minute to the Parliamentary Under-Secretary of State for Scotland, John Mackay (later Lord), concerning the emerging issue of AIDS, in which he indicated that the RTDs in Scotland were very aware of the problem of AIDS and that among their considerations was the avoidance of blood collection “in high risk locations, such as prisons” or areas with a high proportion of homosexuals or drug abusers.[63] The minister merely expressed gratitude for the note: he did not request or require any action to be taken.[64]
In July 1983, the matter was raised within the DHSS: J B Brown (Medicines Division) wrote to John Parker in HS1, referring to the concerns of the Medicines Division’s Inspection Action Group about the collection and use of blood from prisons and borstal institutions. The Group deemed the practice “highly questionable” due to the prevalence of homosexual activity in prisons, coupled with the growing unease about the incidence of AIDS among homosexuals. The note sought advice on the departmental policy regarding this practice.[65]
On 16 August 1983, a handwritten SHHD note recorded a conversation with Paul Winstanley of the DHSS concerning the Medicines Inspectorate’s inquiry about departmental policy on donor sessions in prisons and borstals. Paul Winstanley appeared to be of the view that the RTDs in England and Wales had tended to avoid such collections partly due to hepatitis concerns[66] and inquired about Scottish practices. He emphasised that if a policy of withdrawal was to be considered, it would likely necessitate consultation with the Home Office, given the “importance placed on the social responsibility aspect of such sessions.”[67]
On 23 August 1983, Paul Winstanley responded to J B Brown (copying his response to SHHD) indicating that it was “difficult to advise any particular Departmental policy on the collection of blood from borstals and prisons at the moment.” It was, he said, for individual RTDs to determine how, and from where, donations were sought in the light of the targets they needed to achieve and the numbers of donors on their panels. However, RTDs had been aware of the dangers of relying too heavily on prisons as a source of donations for some time prior to the advent of AIDS, because of the risk of hepatitis in prisons (also connected to the higher incidence of homosexuality) which could be spread through blood transfusion. Although most regions might not need to use prisons, there was at least one which had to view them as a major source of donations in order to meet targets. He continued: “AIDS has of course now called the wisdom of continuing to view prisons as a source of blood even further into question”. The RTDs were due to discuss it at their next meeting in September. Paul Winstanley concluded: “We shall obviously need to liaise closely with Home Office also since they have in the past been very much in favour of blood donation by prisoners.”[68]
In a letter dated 23 August 1983 to Dr Cash, Dr Ewa Brookes, the director of the Dundee RTC, reporting on a recent meeting of the Working Party on the Selection of Donors/Notes for Transfusion, informed Dr Cash that in England and Wales, the practice of hosting donor sessions at prisons and borstals had already been discontinued.[69] This left the decision to the Scottish regions to determine whether they would follow suit. However, at their meeting on 13 September, SNBTS directors could not reach agreement on a blanket decision to cease visiting prisons.[70]
The collection of blood finally stopped from closed prisons and borstals in England and Wales at the end of 1984 and from the last open prison in 1986.[71] By December 1983, Dr Brookes told the SNBTS directors’ meeting that “the only Scottish region to continue holding sessions” was now Glasgow,[72] which held its final session on 25 March 1984.[73] In Northern Ireland, the last prison session occurred in Belfast on 26 October 1983.[74]
It was plainly known to both the DHSS and the SHHD from the early 1970s that the collection of blood from prisons and similar institutions gave rise to an increased risk of transmission of Hepatitis B.[75] Despite this no action was taken, as it should have been, to bring an end to this practice: on the contrary, the CMO’s misguided letter in May 1975 effectively endorsed and encouraged its continuance.
The increased awareness of the extent and potential seriousness of NANBH during the second half of the 1970s, as well as continuing knowledge that Hepatitis B screening was still imperfect, should have refocused attention on the practice of prison collection, but did not. NANBH was highly likely to be more prevalent in prisons, just as Hepatitis B was known to be. Both seemed to share similar modes of transmission.
The emergence of AIDS finally brought the issue back into focus, but should have led to the immediate cessation of all prison collections by the beginning of 1983: instead it continued in some regions into 1983 and 1984.
The hands off approach of the DHSS and the SHHD – leaving the matter entirely to the judgement of local RTDs – was wholly unacceptable. This was a matter of blood safety: it should have been taken seriously by government and was not. There should have been a “departmental policy” and there was not. This was wrong.
The failure to bring the question of prison donation to the attention of ministers was also wrong. It was not raised with a Scottish minister until May 1983; it was not raised with ministers within the DHSS at all. Whether that would have made any difference is debatable – the Parliamentary Under-Secretary of State for Scotland took no action when the matter was finally drawn to his attention; the Minister of State, Kenneth Clarke, appeared somewhat blasé about the collection of prison blood as late as 1983 in his oral evidence to the Inquiry: he did not think he knew that prison blood was collected but did not seem to think that ministers needed to know about it.[76] However a minister properly addressing their mind to the risks ought to have taken decisive action if the matter was brought to their attention. It is disappointing also that no minister appears to have thought proactively to inquire as to whether blood was collected from prisoners in the UK.[77]
The next part of this chapter looks at the Government’s response to the emergence of AIDS as a threat to those receiving treatment with blood or blood products. Two important aspects which overlap with the chronology of events described below are, however, considered elsewhere: the role of the Licensing Authority in responding to the threat of AIDS (and in particular the decisions of the Committee on Safety of Medicines (“CSM”) and Sub-Committee on Biological Products (“CSM(B)”) in July 1983, and decision-making regarding concentrates manufactured from plasma collected pre March 1983) is addressed in the chapter entitled Regulation of Commercial Factor Concentrates and the question of screening for HIV is examined in the chapters on HIV Surrogate Screening and HIV Screening.
The emergence of AIDS as a threat to people who received blood or blood products was a part of a much larger picture. What became a world-wide epidemic first came to notice in the western world on 5 June 1981. Five cases of immune failure amongst young gay men in Los Angeles were reported.[78] By July there were 10 cases and by August 70 more.[79] By December, 160 were being investigated.[80] The mortality rate was very high – 40%.[81] On 10 December 1981 the New England Journal of Medicine carried an editorial, and three separate articles about the disease – including one speaking of an outbreak of “community acquired” pneumocystis carinii pneumonia.[82] It was in January 1982 that the first case of AIDS in a person with haemophilia was identified by the CDC.[83] If the same exponential growth in the numbers infected were to happen amongst people with haemophilia as was happening overall, it would then have been obvious that their lives would be put significantly at risk.
The point arising from this last paragraph is that unless the wider context was considered, a single case of AIDS in a person with haemophilia was unlikely to suggest a significant risk to others with haemophilia. Where that context was one of exponential growth of an infection which was likely to be fatal for almost half of those infected amongst a variety of people (not all of whom were homosexual), a single case was no longer something which could be dismissed so easily. It would more likely be the tip of the iceberg.
That very phrase – “tip of the iceberg” – was one the New England Journal of Medicine used in January 1982 when it returned to the theme of AIDS again. This time the article had the added weight that it was penned by a CDC task force; and, chillingly, the phrase was used to describe not just one case but all the cases so far known in the population.[84] In short, AIDS was epidemic. It was spreading. One infection presaged others. There was already a large number of cases, increasing monthly. And many more were coming, even if (to use the iceberg analogy) they were below the water line and not visible. Yet.
On 16 July 1982 – the same date as the Morbidity and Mortality Weekly Report (“MMWR”) carried a report of pneumocystis pneumonia in three haemophilia patients in the US[85] – the possibility of AIDS being transmitted through blood was explicitly drawn to the attention of civil servants within the DHSS by Dr Harold Gunson, in his capacity as the consultant adviser in blood transfusion. Dr Gunson warned that there “may be considerable publicity in the next couple of weeks concerning the safety of American Factor VIII.”[86] Stanley Godfrey[87] wrote to Dr John Holgate[88] in the following terms:
“From the DHSS point of view, we can defend the National Blood Transfusion Service’s own record.[89] Someone taking drugs (gay or not) would not be bled provided that the injection marks showed. In any case with our voluntary unpaid donor system we do not have the same problem as in the States where drug addicts are tempted to give blood simply for the money. However, about half of the Factor VIII bought from commercial companies is imported from the USA. Your Division … may have to consider revoking licences of certain manufacturers. Of course it may turn out that none of the Factor VIII involved is supplied to this country.”[90]
Dr Holgate responded four days later, confirming his awareness of the “potentially adverse publicity concerning the safety of Factor VIII in the USA (and certain other blood products, in my opinion)”. Although he did not think Stanley Godfrey had got some of the technicalities right, “that makes no difference to the eventual outcome.” Dr John Griffin[91] was said to be aware of this, as was Dr Leslie Fowler[92] “who will have to take any action that proves necessary.” Referring to the risks from homosexual activities, Dr Holgate added that “our own blood production system may not be exempt.”[93] It may be inferred from Dr Holgate’s response, given his knowledge that Drs Griffin and Fowler were already aware of the position, that some discussion had already taken place regarding AIDS within the DHSS, and that Dr Holgate had a sufficient understanding of the issue to doubt the particular thesis posited by Stanley Godfrey.
Beyond this, however, there is no evidence of there being, over the next few months, within the DHSS, any documented discussions or planning or any consideration of what steps might need to be taken with regard to the safety of blood or blood products in light of this grave new threat. Indeed, except for the discussion regarding Stanley Godfrey’s note, there is no record of discussions about AIDS and blood within the DHSS between 16 July 1982 and the end of 1982.
Although there was little or no action within or by the DHSS, some steps began to be taken by the PHLS and CDSC. In August 1982, the CDSC set up a surveillance scheme to monitor opportunistic infections and cases of Kaposi’s sarcoma, based on death certificates identified by the Office of Population, Censuses, and Surveys,[94] information on opportunistic infections on laboratory report forms,[95] and information from venereologists and dermatologists.[96] Dr Galbraith wrote to venereologists and dermatologists in England and Wales in September 1982 seeking their “cooperation” in a trial clinical reporting system of Kaposi’s sarcoma due to the “inadequacies of existing surveillance systems”.[97]
There was a passing discussion of AIDS at the UKHCDO annual meeting on 13 September 1982, where Dr Trevor Barrowcliffe, Anthony Curtis and Geoffrey Kemball-Cook of the National Institute for Biological Standards and Control, Dr Craske of PHLS and Dr Richard Lane of BPL, were all listed as in attendance, although there were no officials present from the DHSS.[98]
In early November 1982 Dr Craske produced a paper on AIDS for the Medical Research Council (“MRC”) Hepatitis Vaccine Working Group which met on 12 November 1982.[99] Present at that meeting was a representative from the DHSS: Dr Mary Sibellas of Med IMCD. Whilst the particular focus of the discussion at the Working Group’s meeting was the potential for contamination of batches of the source plasma for Hepatitis B vaccines, it would have been clear to those attending, including Dr Sibellas, that Dr Craske considered an infectious agent to be the most likely cause of AIDS.[100]
On 3 December 1982 the newly established Central Blood Laboratories Authority (“CBLA”) held its first meeting; members included Dr Edmund Harris (one of the Deputy CMOs), and attendees included John Parker,[101] Stanley Godfrey and Dr Walford of the DHSS.[102] Surprisingly there was no discussion about AIDS.
Dr Walford told the Inquiry that by or at the beginning of 1983 her sense was that it was likely that AIDS was transmissible through blood and blood products. She thought that the view developed incrementally, but that the San Francisco baby case was “a sort of watershed” and “rang all sorts of alarm bells.”[103] She thought that gradually the feeling within the wider DHSS too was that it was “looking more and more likely that blood and blood products are certainly capable of transmitting this agent” and was not aware of anyone voicing any markedly different views (other than, perhaps, Dr Fowler, whose later report for the Committee on Safety of Medicines is considered in the chapter on Regulation of Commercial Factor Concentrates).[104]
On 10 January 1983 Dr Craske wrote to Dr Walford, informing her of arrangements for the investigation of “factor VIII related” AIDS: any patient detected in the UK who had received commercial concentrate would be reported directly to CDC and to CDSC.[105]
On the same date the Advisory Committee on the National Blood Transfusion Service met at the DHSS, under the chairmanship of Dr Harris, and with Dr Walford, Stanley Godfrey and Steven Green of the DHSS in attendance as the secretariat.[106] There was, again surprisingly, no discussion about AIDS.
On 16 January 1983 The Observer carried an article under the heading “Mystery disease threat” which suggested that imported Factor 8 concentrates “may pose a grave threat to the health of haemophiliacs who inject it.”[107] It reported that the deaths of at least ten people with haemophilia in the US were known to have been caused by AIDS, and referred to an imminent meeting of directors of British haemophilia centres to discuss the problem. This prompted someone in the DHSS to send the article to Dr Walford, suggesting that it would be useful to know the outcome of that meeting and adding “Perhaps we can discuss at an opportune moment.”[108] On 19 January Dr Walford wrote to Professor Arthur Bloom noting that recent publicity about AIDS cases in people with haemophilia in the US had “generated quite a bit of interest in the Department.”[109] In the meantime, an internal DHSS minute of 18 January reported Dr Walford as having confirmed that the value to people with severe haemophilia of Factor 8 and 9 concentrates “far outweigh the possible, and as yet unproven hazards of the transmission of acquired immune deficiency syndrome”.[110] Dr Walford described her thinking at the time that the hazards of transmission were unproven and that it was known that people with severe haemophilia desperately needed factor concentrates.[111] From all the evidence available to the Inquiry it appears that was likely to have been the thinking of the Department as a whole at the time. But it was wrong – and not just with hindsight. The hazards of AIDS may have been “unproven”, and the extent of the risk at that stage unclear, but that there was a risk, and that the consequences of infection were grave, was clear and should have weighed more heavily in the balance. As for the “desperate” need for concentrates, the DHSS had insufficient appreciation of the availability of alternative treatment strategies and over-inflated the risks to people with bleeding disorders.
The CBLA, now under the chairmanship of David Smart, but with the Deputy CMO as a member and Stanley Godfrey in attendance, met for the second time on 26 January 1983. Any response to AIDS was still not considered.[112]
On 17 February 1983 Dr Gunson wrote to Dr Walford, drawing her attention to statements from the American Association of Blood Banks (“AABB”) as well as a recent article on AIDS. He stated that the most important recommendation coming from the US was the increased usage of cryoprecipitate, commenting that “if this philosophy takes off in the U.K. it will have considerable implications for the Regional Centres and for the plasma supply situation.”[113]
Other than exchanges such as those set out above, and despite continuing reports in medical and other journals, a number of which concluded that transmission through blood was likely,[114] there is no evidence of the DHSS taking any particular steps at all in response to the risk of AIDS in relation to blood or blood products in the period up to April 1983.[115] There was a brief discussion of AIDS at the CBLA’s fourth meeting on 23 March 1983:[116] Professor Bloom suggested that the CBLA should discuss AIDS at a future meeting and Dr Gunson told the meeting that it would be discussed at a forthcoming Council of Europe meeting in May.[117]
April itself saw little activity. Dr Craske sent Dr Walford a copy of his March 1983 paper (itself an update of his November 1982 paper).[118] Civil servants attended the fifth meeting of the CBLA on 27 April 1983 as observers.[119] The minutes record a brief discussion of AIDS, with Dr Gunson reporting that at the next meeting of RTDs it would be recommended that no further measures be taken, apart from those already being carried out, and Professor Bloom reporting his impression, following a talk on AIDS to the Haemophilia Society’s AGM, that “haemophiliacs were not greatly concerned about AIDS”.[120] Reference was made to Paul Winstanley trying to ascertain the number of calls made following a TV programme which had recently been aired.[121]
There is no evidence, during this period, of any issues relating to AIDS and blood being brought to the attention of the Secretary of State or other ministers.[122]
It was not until May 1983 that there was within the DHSS any real focus on how best to respond to the risks of AIDS from blood or blood products and that was as a response to press reporting.[123] On 1 May 1983 reports appeared in the Sunday newspapers: The Mail On Sunday carried Susan Douglas’ article under the headline Hospitals using killer blood[124] and the Observer carried two articles: one headed Killer disease alert over gay blood donors and the other headed The epidemic spreads.[125] This triggered a response within the DHSS: a minute dated 3 May 1983 records that officials were asked to provide a briefing for Prime Minister’s Questions on the stories which appeared over the weekend about AIDS. A background note and suggested “lines to take” were sent to Number 10 and to Geoffrey Finsberg, the Parliamentary Under-Secretary of State at the DHSS with responsibility for blood policy, and copied to the Private Office of the Secretary of State.[126]
The “line to take” for the Prime Minister – although not actually used by her – read as follows:
“I was very concerned to read this weekend’s Press reports and can well understand the anxiety which some sensational reports may have caused. It is important to put this in perspective: there is as yet no conclusive proof that AIDS has been transmitted from American blood products. The risk that these products may transmit the disease must be balanced against the obvious risks to haemophiliacs of withdrawing a major source of supplies. Already, in this country, there is a special surveillance system, established by the Communicable Disease Surveillance Centre, to monitor the occurrence of AIDS, in collaboration with the Centres for Disease Control in the USA. Every opportunity is being taken for this country to learn from the experience of this disease in the USA.”[127]
The briefing note which accompanied the “line to take” noted that people with haemophilia requiring treatment with Factor 8 concentrates had been identified as being at increased risk. It explained that the cause of AIDS was unknown and that “although medical opinion is tending to favour a virus as the agent responsible, there is no proof that this is the case.” The mortality rate was described as high, with at least 40% dying. In response to the question “Is it transmitted in blood or blood products?” the note read “As yet there is no conclusive proof that AIDS is transmitted by blood as well as by homosexual contact but the evidence is suggestive that this is likely to be the case”. Reference was made to 11 people with haemophilia in the US and three in Spain in whom the most likely explanation for the development of AIDS was their exposure to US Factor 8 concentrates, and to evidence that AIDS had been transmitted to babies in blood transfusions. There were said to be “no proven cases” of AIDS in people with haemophilia in the UK, although there was a “suspect case” in Cardiff.[128] Noting that this patient had received a great deal of British concentrate since 1980 (having last received US concentrate in 1980), the note recorded that it was not possible to know whether British concentrate might contain the AIDS agent. In response to the question “Should a ban be placed on imports of US Factor VIII concentrate?” the note responded that at present haemophilia experts in the UK “take the view that to ban the imports of US FVIII would be to place haemophiliacs at greater risk from bleeding than they would be from acquiring AIDS.”[129] The note then explained the action that was being taken. This was threefold: blood transfusion directors would avoid wherever possible bleeding donors known to be homosexual (it being considered “impossible to ask donors if they are homosexual”); all haemophilia centre directors had received instructions to report any suspect case of AIDS to Oxford and to the CDSC; and the CBLA’s Blood Transfusion Research Committee would be considering “the problems posed by AIDS to the Blood Transfusion Service.”[130]
Lord Fowler rightly described the information in this paper as something that “should have been ringing alarm bells more widely”.[131]
On 6 May 1983 Dr Galbraith of CDSC telephoned Dr Sibellas at the DHSS to report that the Cardiff patient had the right symptoms and signs for a diagnosis of AIDS, and to flag up the three cases in Spain. He asked that the DHSS “consider the matter as a priority – and asks that any top level meeting should include CDSC”.[132] Three days later, on 9 May 1983, Dr Galbraith wrote to Dr Ian Field at the DHSS. Having referred to known, or likely, cases of AIDS in people with haemophilia in Spain and the US, and to the Cardiff patient, he said this:
“I have reviewed the literature and come to the conclusion that all blood products made from blood donated in the USA after 1978 should be withdrawn from use until the risk of AIDS transmission by those products has been clarified … Perhaps the subject could be discussed at an early meeting with haematologists, virologists and others concerned so that a decision may be made as soon as possible.”[133]
Appended to the letter was a paper in which Dr Galbraith set out his reasons for the temporary withdrawal of such blood products. His reasons can be summarised as follows:
Dr Galbraith’s reasoning was impeccable and his views deserved to be given great weight and to be circulated widely. Unfortunately, and as described further below, that did not happen.
On 12 May 1983 Dr Sibellas sent Dr Field a minute setting out her understanding that Dr Galbraith had written to him suggesting that there should be a Working Party on AIDS.[136] Dr Sibellas suggested that papers could be sought from Dr Walford, Dr Gunson, Dr Craske, Dr Galbraith and Dr Catterall.[137] Handwritten across the minute are the words “this idea has now been abandoned. Drs will now have ad hoc discussions.”[138]
Dr Galbraith’s letter to Dr Field, and his paper, was the subject of internal comment by Dr Walford following her attendance at the reference centre directors’ special meeting on 13 May 1983,[139] but does not otherwise appear to have been acted on or shared more widely (either within the DHSS or externally) and was not provided to the reference centre directors at or for their meeting.[140] Dr Walford’s view was that the suggestion was “premature” and “unbalanced” because it did “not take into account the risks to haemophiliacs of withdrawing a major source of their FVIII supplies.” She suggested that the situation was “best put in perspective” by a statement in the reference centre directors’ minutes, then in draft.[141] This statement (which was not for publication, as the final wording might not be precisely the same) read as follows:
“Many Directors have until now restricted their use of FVIII in young children (under the age of 4 years) and in mild haemophiliacs to NHS materials and we consider that it would be circumspect to continue with that policy.
There is not sufficient evidence to restrict the use of imported FVIII concentrates in other patients in view of the benefits of the treatment but the situation will be kept continuously under review by means of a surveillance system which has been instituted and by means of regular meetings of the Reference Centre Directors…
The Directors welcome the fact that the Regional Transfusion Directors would be meeting to consider steps which could be taken to avoid bleeding donors who might be in a category thought capable of transmitting AIDS.” [142]
Dr Walford suggested, with regard to the Working Party on AIDS proposed by Dr Galbraith, that Professor Bloom be invited to represent haemophilia centre directors.[143]
It appears that Dr Field responded to Dr Walford in a minute of 19 May which has not been found. Her subsequent response was to “agree entirely with your suggestion for handling this issue” and she said that she “certainly would not wish to press for a formal Working Party at this stage.”[144]
The DHSS’s response to Dr Galbraith’s letter and paper was wholly inadequate. It was not placed before the CSM(B) or the CSM, as it should have been.[145] It was not brought to the attention of ministers,[146] or to the CMO, as it should have been. Lord Patten told the Inquiry “unequivocally” that ministers should have been informed about it – and that if he had seen it “I think I probably would have pressed the panic button.”[147] It was not circulated to haemophilia centre directors or to RTDs, so as to allow a fully informed and comprehensive debate and discussion, as it should have been. The only internal DHSS consideration of which the Inquiry has any evidence is Dr Walford’s response.
In dismissing, or at least ignoring, Dr Galbraith’s position, the whole issue of concentrate use seems to have been seen as a binary choice, an all or nothing scenario of continuing unabated with the status quo or providing people with haemophilia with no treatment at all. That was the wrong way to look at it. There were, moreover, other ways in which the risks to people with haemophilia could be addressed at least on a temporary basis, which were not considered, adequately or at all, by the DHSS.[148]
Not only were ministers not told of Dr Galbraith’s paper, they were not told about the CSM’s decision-making. This failure to tell ministers of the CSM’s decision meant that they could not then explore whether there were less radical steps that could nonetheless be taken to minimise the risks.[149] It was Lord Fowler’s expectation that Lord Glenarthur and the CMO would be fully briefed about the results of the meeting; but without being aware of it, a minister could not consider whether they agreed or whether there needed to be challenge to it.[150]
In Lord Glenarthur’s statement to the Inquiry he talked about people with haemophilia being “in peril” from the unavailability of Factor 8 if imports were stopped, and agreed with not stopping importation because “There seemed no practical alternative, other than to suddenly imperil the lives of haemophiliac patients.”[151] He believed that the risk to people with haemophilia of not having treatment was very grave.[152] His understanding, therefore, was that the only choice was a stark all or nothing one and that there was no alternative to the continuation of use of imported concentrates.[153] In fact there were a whole range of strategies that could have been considered: the increased use of cryoprecipitate, the postponement of elective surgery, a more conservative approach to treatment, the temporary cessation of home and prophylactic treatment, reserving concentrates for life threatening or essential surgery only, a system of batch dedication, greater use of DDAVP. Moreover, if concentrate were thought essential for treatment in individual cases, NHS concentrates were likely to be much safer than imported commercial products. There is no evidence to suggest any of this was considered, explored or assessed by the DHSS, and Dr Walford acknowledged that it was “fair” to say no one applied their minds to a more nuanced strategy than Dr Galbraith proposed.[154]
On 3 June 1983 an internal DHSS meeting took place to consider AIDS. An agenda identified 8 issues for consideration:
A number of papers were prepared for the meeting, including a background paper which included the “no conclusive proof” line.[156] The second paper referred to the recommendations of the reference centre directors at their meeting on 13 May 1983 and their agreement that no restriction should be placed on the use of imported Factor 8 concentrate “other than to continue with the present policy of using only NHS material for children under the age of 4 years and for mild haemophiliacs”.[157] The sixth paper dealt with the implications of AIDS for BPL and suggested, amongst other matters, that there would be major operational and financial problems for RTCs if there were to be a significantly increased demand for cryoprecipitate. This assertion appears to have been based on Dr Gunson’s views alone.[158]
The meeting on 3 June was attended by a range of policy and medical civil servants from different divisions within the department. Ministers were not involved. It was opened by John Parker explaining that the meeting had been arranged to consider the implications “for the Department” of “recent media reports on AIDS” and to consider possible courses of action.[159] This language is telling of the DHSS’s stance and priorities.
The actions that were agreed as a result of the meeting were limited: Dr Walford would approach the chair of the RTDs to ascertain their views on questioning donors about the presence of symptoms such as night sweats; the Medicines and Supply Divisions would instigate informal discussions with pharmaceutical companies regarding concentrate manufactured from plasma donated pre 23 March;[160] HS1A should keep a close watch on developments in relation to heat-treated Factor 8; John Parker would write again to regional administrators rehearsing the benefits of self-sufficiency and pressing for urgent action;[161] there would be liaison with the Medical Research Council (“MRC”) group on AIDS regarding research; Dr Harris should be asked to seek the CBLA’s comments on greater use of single donor or small pool products and the introduction of heat-treated concentrate; and a recommendation would be made for an early meeting between ministers and the Haemophilia Society.[162]
The meeting also considered Dr Gunson’s report on the proposed Council of Europe resolution. It is of note that rather than considering each element of the resolution and determining what steps would need to be taken to comply, the meeting instead agreed that “when the opportunity to comment arose” the potential problems to the UK created by small pool production and the ban of imports “should be brought to the Council’s attention.”[163]
There was no discussion whatsoever of Dr Galbraith’s letter and paper. Nor was there any discussion about any different approaches to the treatment of bleeding disorders: should different policies be adopted for different classifications (mild/moderate/severe)? Should treatment be minimised? Should home and prophylactic treatment be temporarily suspended? Should there be a reversion to cryoprecipitate? Should non-elective surgery be deferred? Dr Walford suggested that this reflected the departmental position that, having regard to the principle of clinical freedom, it was not the role of the DHSS to provide guidance or advice to clinicians.[164] She was no doubt right when she said this was the departmental position, but it was a short-sighted position for the DHSS to adopt and a dereliction of its responsibility to patients. There was no discussion either of patients being informed – again reflecting the departmental position that this was the responsibility of haemophilia centre directors. On an individual patient-doctor basis it is obviously correct that it is the primary duty of the doctor to provide such information to their patients, but that does not, and did not at the time, absolve the Department of all responsibility for ensuring that there was sufficient information available for patients regarding this new and deadly risk.
The CSM(B) and CSM meetings took place in July 1983 and their decision-making is considered separately in the chapter on Regulation of Commercial Factor Concentrates. However, as set out in that chapter, the decision taken in July 1983 does not appear to have been kept under any kind of active review as it should have been. Whilst that is a matter for which the CSM(B)/CSM/Medicines Division bears primary responsibility, it is also right to note that the non-licensing divisions within the DHSS, in particular HS1A as the “lead”, did not take any steps to bring the matter back before the CSM(B)/CSM or to tell ministers, as they should have done.
The need to take steps to protect people with bleeding disorders from AIDS was not a question solely for the UK. Other countries in Europe were affected too. The Council of Europe’s Committee of Ministers met to consider what could and should be done.
The DHSS had advance notice of the Council of Europe’s Committee of Experts’ intended recommendations from Dr Gunson in May 1983.[165] Dr Gunson wrote to Dr Walford on 16 May 1983 telling her that:
“You can see that what they are leading to is the greater use of cryoprecipitate, and we saw two years ago that this tends to be the standard product in many European countries. Although I put forward the UK view of this product the consensus was against us. Like you, I do not think BPL could change to freeze-dried cryo rapidly and the logistic problems would be considerable … Fortunately everyone here was in agreement that it was vital to present a balanced view of this problem and to avoid emotive over-reaction”.[166]
The DHSS’s International Relations Division asked for comments on the draft recommendations,[167] which were provided by Dr Walford on 13 June. The DHSS’s main difficulty was, Dr Walford said, with the first part of the recommendation: avoiding the use of large pool concentrates. This was said to be “theoretically desirable” but that in practice there was “no option but to treat the majority of our haemophiliacs with large-pool products”, and the risks of non-treatment were greater than the risks of treatment. The DHSS would prefer the recommendation to be reworded by the insertion of the phrase “wherever possible” or “wherever practicable”.[168]
The Council of Europe’s Committee of Ministers’ resolution was adopted on 23 June 1983. Its recommendations were addressed to the governments of member states. The overarching recommendation was “to take all necessary steps and measures with respect to” AIDS and there were then three specific recommendations “in particular”.
The first was “to avoid wherever possible[169] the use of coagulation factor products prepared from large plasma pools; this is especially important for those countries where self-sufficiency in the production of such products has not yet been achieved”.[170] The Government took no steps in response to this recommendation. It took the view that the continuing use of imported concentrates was unavoidable[171] and because self-sufficiency had not been achieved there was nothing that could be done. That missed the point of the second part of this recommendation – the particular importance of taking steps where self-sufficiency had not been achieved (because the risks would be greater). To decide that there was nothing to be done because the UK was not self-sufficient was to misunderstand the whole point of the recommendation.
The second was “to inform attending physicians and selected recipients, such as haemophiliacs, of potential health hazards of haemotherapy and the possibilities of minimising these risks”.[172] This was a recommendation to tell two different cohorts – clinicians and patients – about two matters: the risks of treatment with blood/blood products and the possibilities of minimising the risks. The UK Government took no steps in response to this recommendation, either to provide information to clinicians or to provide information to patients, it being the DHSS’s position that providing such information was not its role.[173] Nor did the DHSS contact relevant professional bodies, medical royal colleges or the like to see what information was being provided either to clinicians or to people with bleeding disorders.[174] It did not take any steps to ascertain what haemophilia clinicians were in general telling their patients. Dr Walford pointed in her evidence to the Inquiry to a report from Dr Gunson dated 13 June 1983, prepared for the CBLA,[175] in which he asserted that “Physicians and patients, especially haemophiliacs are being informed of the risks of AIDS.” It is unclear what Dr Gunson meant by the statement that physicians were being informed of the risks of AIDS; as for patients, it is difficult to understand how Dr Gunson, who was not involved in the care and treatment of people with haemophilia, could give any kind of reliable assurance that patients were being informed, and his CBLA report contained no further information or detail in that regard. It was almost certainly no more than an assumption on his part that haemophilia clinicians would be telling patients of the risks, because that was, of course, the right thing to do.[176] The evidence that the Inquiry has heard establishes beyond doubt that patients were as a general rule not being informed of the risks.
Dr Walford did not accept that it was a failure on the part of the DHSS not to take some steps in accordance with the Council of Europe’s recommendation to ensure that people with haemophilia had the requisite information to enable them to make an informed decision about balance of risks. She said this:
“It would only have been a failure if it had been the normal process, the normal procedure, for the Department to intervene in this sort of way, with -- after all, there was a plethora of conditions, in each case, important findings, important developments taking place. The Department could not -- and did not -- provide relevant information to clinicians about clinical matters of that kind. It was simply not set up to do and it did not do it … it wasn’t a failure because it’s not what we normally did.”[177]
Though I acknowledge that what Dr Walford was being asked to consider would be a departure from its habitual practice, I find it difficult to accept this. Whether or not it was something that the DHSS normally did, in respect of other conditions, is not the point. This was not one of the plethora of conditions in which there might be multiple side effects of varying degrees of severity. This was a situation in which there was a very real risk that the very treatment being provided by the NHS – and for which the DHSS bore ultimate responsibility – would directly transmit to patients a fatal, untreatable and new viral disease. It was a situation in which there was a specific Council of Europe recommendation, to which the Government had effectively signed up, that the Government take all practical steps to inform patients both of the risks and of the possibilities of minimising that risk. Whatever the normal approach of the DHSS might be, this was a different situation, and one in which there was a culpable failure by the Government to act.
The third specific recommendation was “to provide all blood donors with information on the Acquired Immune Deficiency Syndrome so that those in risk groups will refrain from donating”.[178] The Government did take steps to comply with this – as detailed below under the heading The AIDS leaflet – but it was not until early 1985 that all donors were being provided with information.
In July 1983 Mr A Cumming of the International Relations branch sent to ministers a minute regarding the Council of Europe’s Recommendation R(83)8; a copy of the recommendation was provided and the covering minute explained that it was normal practice during the preparation of such documents “to ensure that the UK is not committed to policies which would not otherwise be followed, so that there is, correspondingly, no action to be taken if and when they are adopted.” It was noted, however, that such recommendations “are often of interest to pressure groups” and it was thought ministers might wish to be aware of it. The minute stated that “the recommendation aims to ensure that appropriate precautions are taken in the preparation of certain blood products, and that specific groups of recipients such as haemophiliacs are accordingly reassured.” The recommendation did not, ministers were told, prevent the UK from continuing to import concentrates from the US.[179] No reference was made in the text of the minute to the second recommendation regarding the provision of information to clinicians and patients. The minute – wrongly – did not explain that there were areas in which the UK was failing to meet the recommendation and ministers were not asked to take any particular decisions. They should have been.
Lord Glenarthur responded on 22 July, expressing the view that “we should accept the Recommendation” and querying whether there was a publication date for the AIDS leaflet.[180] In his written statement to the Inquiry he was certain that any recommendations on avoiding products from large plasma pools would have been “fully considered by officials including medical advisors”, likewise the provision of information to practitioners and patients.[181] The evidence available to the Inquiry demonstrates that was not the case. He said that officials did not come forward with any particular direction which they encouraged ministers to take – which is correct.[182] He did, however, accept that he would at least expect the DHSS to have made some steps to satisfy itself as to what information clinicians had about the risks of treatment and ways of minimising risks, agreeing that this was a rapidly developing field and that “unless you ask, you don’t know.”[183] He agreed also that it was incumbent upon the DHSS to seek to ascertain what information was generally being given to patients, and to have considered the adequacy of it and whether further information needed to be provided to comply with the recommendation.[184] He could think of no practical or principled reason why an equivalent process to the production of the AIDS donor leaflet could not have been undertaken, to provide to the cohort of people with haemophilia.[185]
Lord Clarke thought he would have read the recommendation.[186] That should have led him to ask what was being done to comply with it, but he did not. Lord Clarke, when giving evidence, took the view that so far as the second recommendation was concerned it was really a matter for haemophilia clinicians to tell their patients of the risks: although the recommendation said in terms that haemophilia patients should be told, as well as clinicians, and should also be told anything relevant about minimising risk.[187] As a simple matter of reading what the recommendation says, it cannot be interpreted in that way. He spoke, too, of doctors taking the decisions on what treatment a patient should have in terms which suggested this was matter solely for the doctor. Though I accept (as he says) that attitudes were different in the 1980s from those that operate today, it was already well established that as part of the central ethical principle of patient autonomy the patient should ultimately determine their own treatment, though the clinician has a role as an expert in giving the information which should help the patient to do so. The result was that the DHSS did not honour the second recommendation, although the Government had signed up to it, and ministers did not ensure that they did so.
There is little doubt that patients, as was generally reflected in their evidence to this Inquiry,[188] were not told adequately or at all of the risks they ran; nor were they advised of what might be done to minimise those risks in their own case, or that of their child. These are serious failures, which resulted in exposure to infection which may never have occurred if they had been told, and advised. These failures resulted, too, in a sense in many of betrayal by doctors they had relied on to give them such information and advice; and in a loss of trust in the Department of Health. There can be little doubt that the Government’s failure to honour a recommendation, despite having accepted it, played a part in this.
As already described, no consideration was given by the DHSS to alternatives to treatment with imported concentrates. In particular there was no consideration of a policy encouraging a reversion to cryoprecipitate use, at least as a temporary measure. The DHSS’s belief appears to have been that there was not enough cryoprecipitate and that it could not have been made quickly.[189] But no assessment was undertaken by the DHSS of the ability of RTCs to produce cryoprecipitate in much larger quantities in at least the short/medium term. The issue was simply not explored with regional transfusion directors. Dr Walford pointed to the position of Dr Gunson,[190] who said it was not feasible, and Dr Lane who said that he could not produce small pool freeze-dried cryoprecipitate.[191] She acknowledged, however, that she was not aware of anyone asking each RTC questions such as “What’s your capacity to produce cryoprecipitate? How much do you produce? Could you produce more? If so, over what period of time? Would you need new equipment or have you got the right equipment?”.[192]
This was not solely a matter for the RTCs and prescribing clinicians to consider. In circumstances where there was a significant public health risk giving rise to the possibility of children and adults being infected through their NHS treatment with a disease known to have an extremely high mortality rate and for which there was no treatment, it was not good enough for the DHSS to say that it was a matter for others. The Secretary of State was ultimately responsible for the NHS and for the safety of patients, and it was incumbent upon him to act.
The DHSS neither issued nor even considered issuing any kind of advice or guidance or steer to clinicians advising, or even simply encouraging them to consider alternative approaches to treatment. This was because the DHSS did not regard it as its role to do so.[193]
It both could have done, and should have done.
Thus when Lord Glenarthur was asked in Parliament on 14 July 1983 by Baroness Rachel Gardner the question “Will the Minister issue instructions to practitioners, or ask his department to look into the need to do so?” he answered yes.[194] On 19 July 1983 Christopher Joyce from his Private Office wrote to Margaret Edwards in the DHSS asking for a draft “which tells Lady Gardner what the Department is doing to promote practitioners’ awareness and diagnosis of AIDS.”[195] An answer then appears to have been provided in a letter of 30 August to Baroness Susan Masham (rather than by way of a separate letter to Baroness Gardner) in the following terms: “We have been looking very carefully at our position on this matter and our medical advisers consider that the publications which have already appeared in the medical press provide sufficient and adequate guidance and information about this disease for practitioners, given the present state of knowledge.” Reference was made to the communicable disease reports issued by CDSC and to a British Medical Journal article published on 6 August, before the letter concluded that “We shall, however, be keeping the matter under close review to see whether any further Departmental action might be appropriate in due course”.[196]Neither the CDSC reports nor the British Medical Journal article addressed the question of risk reduction measures and alternative approaches to treatment, and there is no evidence of the matter being kept under any kind of review, let alone a close one.
It is in truth no answer at all to say that the DHSS (or CMO – as to which see further below) did not provide advice to doctors. It actually did – though not in 1983. Such advice was indeed provided from time to time. In August 1985 a summary of action taken in response to AIDS was provided to John Patten. This showed that all sorts of advice had by this stage been provided to health professionals from a variety of different sources (including the CMO); that further advice was planned; that information had been provided to health and local authorities; and that information had been provided to at risk groups and the public, with reference being made to a Health Education Council leaflet and the NBTS leaflet.[197]
That ministers could provide information to the public, or sectors of the public, in the interests of their health is both obvious as a matter of principle and demonstrated by a further example. In September 1982 the Secretary of State for Health, Norman Fowler, issued a statement regarding whooping cough. That statement gave information about the numbers of cases; the importance of immunisation; the state of knowledge about the risks of the disease and the benefits of vaccination in reducing that risk.[198] This was a campaign initiated by the Secretary of State himself – a “specific campaign in response to a perceived public health risk ... the purpose of which [was] to enable people to be better informed and take better informed decisions.” It was, moreover, a campaign which the DHSS believed saved lives.[199]
It was a failing on the part of the DHSS not to take measures to ensure that both clinicians and people with haemophilia were made aware of the risks of concentrate therapy and of possible alternative approaches to treatment. There was no impediment to it doing so.
In September 1983 Lord Glenarthur asked for a meeting with fellow ministers to discuss what he described as “the balance of risk”: the risk to people with haemophilia if they did not get Factor 8 and the risk of AIDS if they did. That meeting took place on 15 September 1983 with Kenneth Clarke and John Patten (Norman Fowler being unavailable).[200] Lord Glenarthur wanted to ensure that what the DHSS was doing was “correct and justifiable and defensible in every single sense.” There is no record of what was discussed at this meeting but it was a missed opportunity for a reset: for the DHSS finally to take some proactive steps. By this time, of course, the DHSS was aware of a second haemophiliac with AIDS, who had died.[201]
Dr Walford attended the reference centre directors’ meeting on 19 September “to hear the latest on AIDS”. She sent a summary of the“salient points” to Paul Winstanley. These included the fact that some of the commercial Factor 8 concentrate from the batches administered to the patient in Bristol, who had died, had found their way to hospitals which were not haemophilia centres. This was described as “undesirable”, “both from the point of view of patient care, but also because these patients and the treatment they receive do not get included in the national statistics on the use of FVIII which provide so much valuable information”.[202] This fact should have – but did not (or, if it did, no action was taken) – alerted the DHSS to the fact that, given that some people with haemophilia were treated elsewhere than at haemophilia centres, those treating them might have a limited understanding of the risks of treatment. Neither the CMO nor the DHSS could have made any assumptions about the state of knowledge of those hospitals.[203] Two cases described by Dr Mark Winter in his oral evidence to the Inquiry vividly demonstrated the consequences of treatment in such circumstances.[204] That people with bleeding disorders could find themselves being treated in hospitals that were not haemophilia centres and that transfusion might be needed by a member of the public at any time were two scenarios where Dr Walford agreed there might have been particular reasons for a Dear Doctor communication.[205] This risk should have been an impetus to the dissemination of information, whether by the CMO or the DHSS directly, but did not lead to any action.
The first use of “no conclusive proof” appears in the “line to take” drafted for the Prime Minister in early May 1983: “It is important to put this in perspective: there is as yet no conclusive proof that AIDS has been transmitted from American blood products.”[206]The briefing note accompanying this line to take included the sentence: “As yet there is no conclusive proof that AIDS is transmitted by blood as well as by homosexual contact but the evidence is suggestive that this is likely to be the case.”[207]
On 31 May 1983 a letter from Lord Trefgarne to Nicholas Baker MP stated: “I can well appreciate the anxiety, particularly amongst haemophiliacs and their families, which recent press reports on AIDS may have caused and would first of all like to put matters into perspective: the cause of AIDS is as yet unknown and there is no conclusive proof that the disease has been transmitted by American blood products.”[208] This letter was drafted by officials for Lord Trefgarne and, it being the purdah period before a general election, he “would have assumed that any letters put before me for signature would have been drafted by officials based on well-established policy.”[209] Lord Trefgarne did not know why the caveat in the briefing note (“but the evidence is suggestive that this is likely to be the case”) had been omitted from the letter he signed.[210]
On 22 June a paper on AIDS produced by Dr Walford was provided to Lord Glenarthur.[211] This paper did not use the language of “no conclusive proof ”. It explained, amongst other things, that there was thought to be considerable under-reporting of cases of AIDS to the CDC (some 1,450 cases having been reported to date); that there was a “so-called four ‘H’ list of those particularly susceptible to the disease”;[212]that a handful of cases had developed in recipients of ordinary blood transfusions which had provided valuable evidence to indicate that the incubation period might vary from several months to up to four years; and that people with haemophilia “seem at greatest risk of acquiring AIDS” through the secondary method of spread (transfusion). In respect of the one case of AIDS in a person with haemophilia reported to CDSC, the paper said that there was “still some uncertainty over the diagnosis.”[213] The cause of AIDS was unknown “but the evidence is suggestive that it may be a virus.” The paper went on to discuss the “steps which are being taken to prevent the spread of AIDS in the UK”. The first was case reporting (to CDSC and CDC); the second was in relation to blood donors – a leaflet had been prepared and would be published by the DHSS – and the regional transfusion directors were currently considering whether to introduce additional questioning for donors as regards their general health or the presence of key symptoms;[214] the third was in relation to people with haemophilia – the DHSS’s Medicines and Supply Divisions were “endeavouring to ensure that there will be no ‘dumping’ of high-risk plasma products on the UK market and are seeking various assurances from the manufacturers in relation to the quality of their product”; and the fourth involved research into male homosexual patients attending the Department of Genito-Urinary Medicine at the Middlesex Hospital.[215]
On 1 July 1983 a further paper (together with the draft AIDS donor leaflet) was sent to Lord Glenarthur. This paper referred to “increasing evidence that AIDS may be transmitted by the transfusion of blood … Blood products … may also transmit AIDS and haemophiliacs are at particular risk ... It is believed that there may be under-reporting of cases … Although there is no conclusive evidence, it seems very likely that AIDS is caused by an as yet unidentified virus.”[216]
On 14 July 1983 the “no conclusive proof” line to take was used in Parliament: Lord Glenarthur, answering a question about AIDS, stated that “Although there is no conclusive evidence that AIDS is transmitted by blood or blood products, the department is considering the publication of a leaflet indicating the circumstances in which blood donations should be avoided.” In the course of the debate, Baroness Masham posed a question to which Lord Glenarthur did not know the answer; he said that he would “find out and let her know.”[217]
On 19 July Christopher Joyce, of Lord Glenarthur’s Private Office, wrote to John Parker, referring to the fact that Lord Glenarthur undertook to write to Baroness Masham about possible transmission through Factor 8: “I do not know that there is much more we can say than to refer to the balance of risk to haemophiliacs and the development of production at the new Elstree lab, but Lord Glenarthur is concerned to allay Lady Masham’s anxieties so far as possible. She is an energetic lobbyist.”[218]
On 20 July Dr Walford produced some wording for a reply by Lord Glenarthur to the question from Baroness Masham, which included the following: “There is no conclusive proof that AIDS can be transmitted by blood, cryoprecipitate or Factor VIII concentrates but the assumption is that such transmission may be possible.”[219] By the time John Parker of HS1 sent Lord Glenarthur’s Private Office a fuller text for the suggested letter to Baroness Masham on 26 July 1983, the wording had become “I should emphasise that there is no conclusive proof that AIDS can be transmitted by blood, cryoprecipitate or Factor VIII concentrates.”[220]
The letter as sent to Baroness Masham on 30 August 1983 stated that “There is, in fact, no conclusive proof that AIDS can be transmitted by blood, cryoprecipitate or Factor VIII concentrates.”[221] Thus, it can be seen that not only did “no conclusive proof” become part of the line to take, but the qualifying phrase in Dr Walford’s original draft (“but the assumption is that such transmission may be possible”) was dropped.[222] Lord Glenarthur did not know why that qualification had been omitted from the version sent to his office, and duly sent by him to Baroness Masham: “Mr Winstanley, or somebody else in the Department, took it upon themselves to remove that, I don’t know why they never referred it back to Dr Walford to say no -- so that she could say, ‘No, I really think it ought to go in, and if necessary, ministers have got to be consulted about whether it should go in.’” In retrospect, this troubled him.[223]
On 25 August 1983 Lord Glenarthur wrote to Nicholas Baker, providing information about the monitoring of AIDS cases by CDSC; his letter ended “Finally, I would like to stress that there is as yet no proof that AIDS is transmitted by blood or blood products.”[224]
On 26 August 1983 Lord Glenarthur wrote to Clive Jenkins, the general secretary of the Association of Scientific Technical and Managerial Staffs. His letter read: “I think that I should emphasise, firstly, that there is no conclusive evidence that AIDS is transmitted through blood products.” It continued “Nevertheless we are taking all practicable measures to reduce any possible risks to recipients of blood and blood products.”[225]
On 1 September 1983 the publication of the AIDS donor leaflet was announced with a press release in which Kenneth Clarke said “It has been suggested that AIDS may be transmitted in blood or blood products. There is no conclusive proof that this is so.” He went on to say that nevertheless he could “well appreciate the concern that this suggestion may cause”.[226] A draft of the press release and a Q&A brief were sent to Kenneth Clarke for approval in advance.[227] The Q&A brief suggested that in response to the question “What is being done to protect haemophiliacs?” the answer should be “I must emphasise that there is no conclusive evidence that AIDS has been transmitted by American blood products”. In response to the question “What is the Government doing to stop imports of Factor VIII from America?” the suggested answer was “Factor VIII is essential to the treatment of many haemophiliacs and the possible risk of infection from AIDS must be balanced against the obvious risks of not having enough Factor VIII”.[228] In response to the question “Why issue a leaflet at all?”the suggested answer was: “While there is no conclusive evidence that AIDS is transmitted through blood or blood products we believe that it is right that blood donors should be fully informed about AIDS”.[229]
The purpose of Kenneth Clarke making a ministerial statement that would be incorporated into a press release had been discussed earlier in August 1983. The arguments for so doing were twofold: political and media interest, and “the need for the Government to be seen to be taking a positive step in an area where, because of the lack of knowledge of the cause of the disease and its treatment, there is limited scope for action.”[230] It was, therefore, a deliberate decision to make the statement by way of press release on 1 September, in part to portray the Government as acting proactively, and it was made in the expectation that it would excite political and media interest.
The ministerial statement was indeed reported in the press on 2 September: The Daily Telegraph carried a story which included the paragraph that “Mr Kenneth Clarke, Health Minister, said there was no conclusive proof that AIDS was transmitted in blood or blood products”; and The Times likewise reported that “Announcing publication of the leaflet, Mr Kenneth Clarke, Minister for Health, said: ‘It has been suggested that Aids may be transmitted in blood and blood products. There is no conclusive proof that this is so.’”[231] The British Medical Journal on 17 September 1983 reported in “Medical News” the publication of the leaflet and repeated that “The Minister of Health said that although it has been suggested that AIDS may be transmitted in blood or blood products there is no conclusive proof that that is so.”[232]
At the 17 October 1983 meeting of the Advisory Committee on the NBTS the minutes record a contribution from Dr Walford that “Although there was as yet no conclusive proof of a link between AIDS and blood products the Department had, in conjunction with RTDs produced a leaflet aimed at reducing the risk of transmission of AIDS by blood donation.”[233]
On 1 November 1983 The Guardian carried an article about the death (in the summer) from AIDS of a British person with haemophilia from Bristol, quoting from Dr Helena Daly and Dr Geoffrey Scott (director of the Bristol Haemophilia Centre) that “It seems highly probable that the development of Aids was related to this treatment. This case provides further evidence for a link between blood products and Aids.” This report prompted Steven Green to ask Dr Walford on 23 November “is it Ok for me to continue to say ‘there is no conclusive proof that the disease has been transmitted by American blood products’”, to which Dr Walford replied “Yes it is ok”.[234]
On 14 November 1983 Kenneth Clarke told Parliament that “There is no conclusive evidence that acquired immune deficiency syndrome (AIDS) is transmitted by blood products.” That same statement asserted that professional advice had been made available to all haemophilia centres in relation to the possible risks of AIDS from Factor 8 concentrates.[235]
On 16 November 1983 Lord Glenarthur wrote to Jerry Wiggin, in response to a letter from the latter to Kenneth Clarke and an enclosed letter from a constituent whose 14 year old son had haemophilia. The letter read “I can well appreciate the anxiety, particularly amongst haemophiliacs and their families which recent press reports on AIDS may have caused and would first of all like to put matters into perspective: the cause of AIDS is as yet unknown and there is no conclusive proof that the disease has been transmitted by American blood products.” Forwarding the letter to his constituent, Jerry Wiggin expressed the hope that “Lord Glenarthur’s reply will reassure you on the Government’s stand on this issue”.[236]
On 16 December 1983 Lord Glenarthur wrote to John Maples MP, in response to a letter to Kenneth Clarke, in which he stated “I can well appreciate the anxiety, particularly amongst haemophiliacs and their families which recent press reports on AIDS may have caused and would first of all like to put matters into perspective: the cause of AIDS is as yet unknown and there is no conclusive proof that the disease has been transmitted by American blood products.”[237] This letter was, as Lord Glenarthur acknowledged, designed to provide a degree of reassurance, and there was nothing within it that recognised the strong circumstantial evidence.[238]
Clive Jenkins rightly took issue with the statement that there was no conclusive evidence that AIDS was transmitted through blood products. In a letter of 27 October 1983, he argued that the evidence was very strong; he set out his understanding that the number of people with haemophilia with AIDS in the US was likely an underestimate because of the long incubation period; he stated that people with haemophilia in Europe were contracting AIDS; and he pointed to a paper submitted to a recent meeting of the Advisory Committee on Dangerous Pathogens (“ACDP”) which recorded that there “is now strong circumstantial evidence that AIDS may be transmitted by blood and blood products.”[239] Clive Jenkins then posed a pertinent question: “I am tempted to ask you what you would consider to be conclusive evidence, particularly in the circumstances where the agent or agents for AIDS are as yet unidentified?”.[240] Lord Glenarthur did not think he would have seen this letter until he was sent a suggested reply in January 1984; he did not recall being made aware of the situation in Europe or of the paper for the ACDP. He would, he said, have expected officials to examine what was in Clive Jenkins’ letter and advise him if there was evidence of a real cause for concern or conflict with what the Government was saying.[241] Lord Glenarthur told the Inquiry that had he seen that paper it would have given him pause for thought as to whether it was right to emphasise the absence of conclusive proof, and that he would have asked questions about it.[242]
The reply that Lord Glenarthur sent reiterated that there was no conclusive evidence, acknowledged that the circumstantial evidence was strong and suggested that the two statements in no way contradicted each other.[243]
On 25 March 1984 The Sunday Times carried an article titled “New Aids alarm over blood link” which suggested that doctors “now have conclusive proof that the mysterious and generally fatal ailment known as Aids has been passed to a hospital patient through a blood transfusion.”[244] In a handwritten note from Steven Green of the DHSS dated 26 March 1984 it was confirmed that “We dropped ‘there is no conclusive proof that AIDS is transmitted through blood or blood products’ from our standard line some time ago.”[245] Lord Glenarthur had no recollection of the dropping of the line to take coming to him for consideration or approval.[246]
In 1987-88 the “no conclusive proof” line to take was looked at by the DHSS. Dr Roger Moore’s assessment was that: “Throughout 1983 the Government’s public line in Private Office cases and Parliamentary replies was that there was no conclusive evidence that AIDS was transmitted by blood products. This statement was strictly true and in view of the very small number of UK cases was intended to reduce public anxiety.”[247] Dr Moore thought that it was clear from the files that:
“the Department adopted a precautionary stance and assumed in its policy decisions that AIDS was transmitted by an infective agent … Not until April 1984 when the AIDS virus was isolated could it be said that conclusive evidence was available.[248] However by then public interest had waned and not until December 1984 did a Departmental Press Release need to refer to the AIDS virus in Factor VIII thereby acknowledging the fact for the first time.”[249]
Dr Hilary Pickles, writing to the CMO on 19 April 1988, and referring to Kenneth Clarke’s parliamentary response of 14 November 1983, said that the reply was “strictly true at the time. Although with the benefit of hindsight, in November 1983 there were strong indications that AIDS could be transmitted by blood products conclusive proof was not available.”[250]
By the summer of 1983 (indeed, as Dr Walford confirmed, from at least the beginning of 1983), the DHSS rightly understood that, as a matter of probability, AIDS could be transmitted by blood. In a briefing for the then minister, Geoffrey Finsberg, on 20 May 1983, Dr Walford wrote that “The general view is that the transmission of AIDS seems to follow the pattern seen with the hepatitis B virus, that is, it may be transmitted … by contact with blood”[251] Dr Gunson’s report on 19 May 1983 of the proceedings of the Council of Europe’s Committee of Experts stated that “Absolute proof that AIDS is caused by a transmissible infectious agent is not yet available, but the consensus in the Committee was that it should be regarded as such”.[252] Dr Richard Tedder’s letter of 20 May 1983 to Dr Walford explained that “This condition is likely to be caused by an infectious agent or agents.”[253] The donor leaflet that was going through the process of approval by the DHSS posed the very question “Can AIDS be transmitted by transfusion of blood and blood products?” and answered it in these terms: “Almost certainly yes”.[254]
The line “no conclusive proof”, whilst technically correct, was indefensible. It did not spell out the real risk. It gave false reassurance. It lacked candour and, by not telling the whole truth, it was misleading. There was no good reason for the decision to adopt and maintain this line. It represented a deliberate choice by the DHSS to emphasise the absence of conclusive proof rather than the presence of a likely risk. Its motives for so doing are likely to have been a combination of reassuring people who might need a transfusion and encouraging people with bleeding disorders to continue to accept treatment with concentrates[255] and because it might mitigate the fact that the DHSS was not taking more radical or proactive steps.[256] It is noteworthy that at a meeting on 6 July 1983 Kenneth Clarke said, in relation to the oral Parliamentary Question that Lord Glenarthur would be answering on 14 July, that the latter should, if asked about the transfusion service, “emphasise that the risk to haemophiliacs was very small.”[257] This too was part of the DHSS’s wish to downplay the risks to people with bleeding disorders.
The line to take was not an accurate reflection of the DHSS’s actual understanding and belief, which was that it was likely that AIDS was transmitted through blood and blood products. It did not, therefore, set out the true internal understanding within government. As one submission to the Inquiry points out, to explain that use of the phrase was to avoid alarming the public, showed a disrespect for the right of citizens to know the truth, and was a mismanagement of the response to a risk to public health.[258]
No minister challenged the “no conclusive proof” line. They could have. If they had, it is likely that the qualification – “but that it is very likely that it does” – would have been given to them, and then to the public.
As Dr Walford pointed out in relation to the language used in the AIDS donor leaflet, donors needed something that was clear and unambiguous. But it was equally, if not more, important, that those who might be exposed to the risk should have that risk clearly spelt out to them.
The line to take was used in Parliament, in press releases, in communications with members of Parliament who were raising matters on behalf of constituents and would no doubt report back to them. It was designed to influence public opinion and may well have done so.[259] It is of course right that there was some scientific uncertainty about a number of matters. But that reinforced the importance of clarity and transparency. Both the public and the particular cohorts of patients most likely to be directly affected were entitled to be told what was known for sure, what was thought to be likely, and what was recognised as a possibility. Far from seeking to reassure those taking blood or blood products that doing so came without significant risk, the authorities ought to have been emphasising that there were indeed risks.[260]
Until such time as a screening test was available, the only means of reducing the risk of AIDS transmission within the domestic blood supply was to ensure, as far as possible, that those donors most likely to transmit the virus did not donate. The risk was pressing.[261] A leaflet for potential donors was, therefore, a key measure. Unhappily, however, and as set out below, this took far too long.
On 16 May 1983 Dr Gunson wrote to Dr Walford to inform her of discussions at the Council of Europe meeting which he was attending. Amongst the measures which were expected to be in the Committee of Ministers’ resolution was the provision of information “to all donors so that those at risk will abstain from donating.”[262] Dr Walford attended the meeting of regional transfusion directors two days later;[263] it was her recollection that she asked to be invited and that her purpose was to urge the regional transfusion directors to produce a leaflet for donors discouraging high risk groups from donating.[264] It was, she said, the DHSS’s view by this time that blood donors in the risk groups (men who had sex with men and injecting drug abusers) should as far as possible be excluded from donating, and she requested at the meeting that a leaflet be prepared, which she envisaged could be used in conjunction with questioning by the transfusion doctor to elicit possible risk factors. The proposal was not, she recalled, well received, but Dr Gunson had also written to the regional transfusion directors with options,[265] and although there was reluctance to proceed with a leaflet the RTDs agreed one should be prepared. The RTDs were adamant, however, that there should be no questioning of donors about their sexual habits or injecting drug use.[266]
When Dr Walford received the original draft leaflet, she did not think it was sufficiently clear and asked Dr Gunson to redraft it. The redraft was sent to Paul Winstanley, for onward transmission to the DHSS’s Information Division, on 17 June 1983.[267] Paul Winstanley had, in an earlier minute to the Information Division, already set out concerns about the lack of speed:
“The object of this exercise is to take, and to be seen to be taking, urgent action to reduce the risk of AIDS being spread through blood transfusions by seeking to exclude those donors thought most likely to be carriers of AIDS. Any delay obviously reduces its effectiveness. It is not beyond the realms of possibility that a minor epidemic of AIDS could break out in the near future … I should have thought we are not likely to earn the gratitude of Ministers for delaying a measure designed to reassure blood donors and reduce the risk of AIDS when they are being asked awkward questions about what the Department is doing and why action was not taken before. It is worth remembering that this leaflet is a low-key measure compared to the examination and questioning of donors which the FDA in the USA has instituted.”
Paul Winstanley added that “it was essential to act without delay” and that “As it is, the time for printing and distribution seems painfully slow.”[268]
Despite Paul Winstanley’s concerns, matters did not proceed particularly swiftly thereafter. On 1 July a paper and the revised leaflet were sent to Lord Glenarthur[269] by John Parker (HS1) with the observation that the issue of the leaflet “would be seen as a positive step to minimise the risk of the transmission of the disease through blood donation in this country.”[270] The paper suggested that ministers’ agreement was being sought to the funding (£5,000) and publication of the leaflet in view of“the sensitivity of the issue as it relates to homosexuals”.[271] The recommendation was that, despite the potential sensitivity, “early publication of the information leaflet is in the best interests of the public health.”[272]
Lord Glenarthur responded promptly on 4 July: he was content with the proposed leaflet and cost.[273] John Patten expressed the view that “public concern on this issue is mounting, and rightly” and that the “earliest possible publication seems desirable”.[274]The Minister of State, however, Kenneth Clarke, appears to have been less convinced and a meeting took place on 6 July 1983 between Kenneth Clarke, Lord Glenarthur and officials to discuss the issue.[275]
The note of the meeting records that Kenneth Clarke had two main concerns: to establish the necessity of a leaflet and to agree how the inevitable publicity surrounding it should be handled. Officials having explained the main objective of the leaflet (to discourage those who were most at risk from AIDS from giving blood), Kenneth Clarke accepted the argument, but wanted it to “emphasise unequivocally that donors would not be questioned about sexual matters” and that a press notice should “repeat that there was no question of donors being quizzed about their sexual habits.” The main objective, he said, “was to minimise any damage to the transfusion service.”[276]
A letter from Dr Gunson to Dr Ronald Oliver (who was present at the meeting on 6 July and had subsequently spoken about it to Dr Gunson) gives a sense of Kenneth Clarke’s concern: “that the issuing of the leaflet may be regarded as a panic measure by the Government and lead to resentment amongst donors and alarm amongst patients.”[277]“[Against] the background of the need for a low-key approach to the publication of the leaflet and the need to ensure that we do not spread unnecessary alarm and despondency amongst donors”, the Minister of State did not want the leaflet to be distributed with call-up cards.[278] Dr Oliver, by contrast, held the strong view that the leaflet should be sent out with the call-up cards:
“I am quite sure that the best way is to send out the leaflet with the call-up cards so that the contents can be studied by individuals in private. I do not think donors would take exception to receiving a leaflet in this way, couched in the way it is as general information on a subject of public interest. I personally would have thought this would entirely satisfy the low key approach that Ministers and all of us want.
The only alternative is to make the leaflet available at donor sessions or positively hand it out at donor sessions. In either event it could place a donor in an impossibly embarrassing situation or defeat the objective of the leaflet. For example, if having read the leaflet before donation the donor feels he should decline to give blood it is embarrassing to walk out as everyone will suspect the reason for his doing so. If he reads the leaflet or considers it while actually donating blood, again he can hardly say anything without embarrassment, and if he is in the high risk group of donors possibly infected blood will get into the system.” [279]
John Bolitho, of the Information Division, thought that Kenneth Clarke would be “very irritated if we are not able to control distribution the way he wants it. He reacted very unfavourably when this was suggested at the meeting.” He expressed the concern that if it was distributed with call-up cards “it will soon be in the news media and we could have a similar furore to the Gillick case with family planning.”[280]
Whilst John Parker acknowledged the need to “bow to Ministers’ wishes on the matter of handling the distribution”, he was not convinced that ministers “have fully understood the pros and cons”, and they needed to weigh the possible disadvantage of letting “risky” blood “slip through the net” against the advantage of minimising adverse publicity. He was convinced that sending the leaflet out with the call-up cards was “the only sensible thing to do”.[281]
On 29 July 1983 a submission was sent to ministers seeking their agreement to the printing, distribution arrangements and publicity for the proposed AIDS leaflet.[282] The submission stated that opinion amongst regional transfusion directors as to the best means of distribution was divided. Two methods were described: issuing the leaflet with the donor call-up cards and making the leaflet available at donor sessions. The pros and cons of each were set out.[283] It is obvious from the articulation of those pros and cons in the ministerial submission that the issue of the leaflet with the donor call-up cards was more likely to meet the public health objective of the exercise. Yet the submission surprisingly continued by stating that it was “not immediately obvious which method is to be preferred” and recommended that regional transfusion directors should be given the discretion to decide, for a six month trial period, the most effective means of distribution in their own regions.
Lord Glenarthur, responding (again promptly) on 3 August, approved the text of the leaflet. He favoured using both methods of distribution and felt that “the risk of embarrassment to potential donors is outweighed by the need to achieve wide distribution”, adding that “We may be at the tip of an iceberg with AIDS and find ourselves in trouble in 18 months’ time unless we are really positive in our approach.”[284] John Patten expressed very similar views: the arrangements should go ahead “as soon as possible” and, like Lord Glenarthur, he asked whether there was any reason why regional transfusion directors could not follow both methods of distribution for the trial period.[285]
Kenneth Clarke, by contrast, in a minute of 2 August, thought the arguments in terms of the methods of distribution were “finely balanced” and was “prepared to allow directors discretion on how to distribute for six months”.[286] Kenneth Clarke’s preference was for the leaflet not to go out with call-up cards: his reasoning was the reaction of recipients – some people would say “What are you calling me gay for? I’m not gay” and others would say “Good grief, what have they got against gays? The Department of Health is getting homophobic.”[287]
Somewhat bizarrely, just over three weeks later, on 26 August, Kenneth Clarke commented that the range of views from regional transfusion directors was alarming, queried whether there had been agreement from the Department on one method of using the leaflet, and asked what authority he had to insist on one national method.[288] On 31 August, however, he clarified that he had “forgotten” that he had earlier agreed to regional transfusion directors having discretion on a six month trial period. At the same time his Private Office asked that Lord Glenarthur’s comments on the six month trial proposal be obtained as soon as possible.[289]
On 1 September Lord Glenarthur suggested that the trial period should last three months rather than six, a proposal with which Kenneth Clarke agreed.[290] It had seemed to Lord Glenarthur that “a six-month trial was unnecessarily long … was excessive in my view. I was used to dealing with stuff much more rapidly than that and it seemed an unconscionably, whatever the word is, long period of time.”[291]
The leaflet went into distribution with effect from 1 September 1983. In a press release of the same date, Kenneth Clarke stated that:
“It has been suggested that AIDS may be transmitted in blood or blood products. There is no conclusive proof that this is so. Nevertheless I can well appreciate the concern that this suggestion may cause. We must continue to minimise any possible risk of transmission of the disease by blood donation but it is not possible to test a person’s blood for the presence of AIDS. The best measure which can be taken at the present time is to ask people who think they may have AIDS or be at risk from it, to refrain from giving blood. This is what this leaflet sets out to do.”
The press release emphasised that there was “no question” of donors being asked about their sex lives at blood donation sessions or at any other time.[292]
Given that the risk of transmission of AIDS through blood or blood products was something the DHSS knew about since mid 1982,[293] it took far too long until the production of a leaflet was first discussed in May 1983.
Though rightly described as urgent internally within the DHSS,[294] it then took too long for the leaflet to be finalised and made available to RTCs at the beginning of September 1983.
When the matter finally did come to the attention of Lord Glenarthur, he was in no doubt that the leaflet was required and needed to be done quickly: “I felt that there was a degree of urgency … and we ought to get it out as soon as possible.”[295]He told the Inquiry that it all took “too long”.[296]
Lord Clarke was less troubled by the delay (which was contributed to by the belief that ministerial approval was necessary and by the time then taken for that ministerial approval to be obtained). He identified two concerns: he “didn’t want it to be done in such a way that we stopped people volunteering to donate blood”and he “really was very worried that we didn’t want people put off from blood transfusions.”[297]He intervened “because I just wanted to make sure that we didn’t start setting off some sort of mayhem that damaged the Transfusion Service.”[298] He wanted there to be emphasis in the leaflet on how few cases of AIDS there had been, describing this as “trying to minimise panic before we knew more about it.”[299] His reason for not supporting the sending out of the leaflet with the donor call-up cards was that it would result in the DHSS being regarded as homophobic;[300] he also thought that the donor receiving the leaflet with the call-up card “would get the impression that when you went to the blood donation you were going to be quizzed about your sex life.”[301] In terms of the time taken to produce the first leaflet, he asserted first in his oral evidence that “any delay in issuing the first leaflet had had no effect on anybody’s health at all” – which he was not in any position to know – and then said “I will concede that in the five weeks between the first leaflet being proposed and it going off to the printers, it is conceivably faintly possible that such a case[302] had occurred.”[303]
A concern that the DHSS might be seen as homophobic should not have slowed the process down, nor should it have influenced the method of distribution of the leaflet as it did; as for the concern to avoid panic or mayhem, this was never a realistic scenario.
It is unclear why the submission to ministers in July 1983 suggested that it was not immediately obvious which method of distribution of leaflets was to be preferred: it ought to have been obvious (as it plainly was to both Dr Oliver and John Parker) that sending the leaflet out with the call-up invitation was the method most likely to achieve the objective of preventing donation by high risk donors. It is conceivable that the submission was framed in the way that it was because civil servants knew that Kenneth Clarke preferred that the leaflets not be distributed with call up. In any event, the decision to leave the method of distribution to regional transfusion directors rather than ensure from the outset that the leaflets reached donors to the greatest possible extent was wrong.
The three month trial period for distribution of the first leaflet should have led to a review at the end of November or the beginning of December. It did not. Instead, there was substantial delay in evaluating whether the content of the first leaflet was sufficient to achieve its purpose and whether there should be a changed approach to distribution of the leaflets.
There was some limited communication between officials and ministers on the subject of the AIDS leaflet in late November 1983, but this appears to have been limited to the question of distributing the leaflet to sexually transmitted disease (“STD”) clinics.[304]
At a meeting of the CBLA’s Working Group on AIDS on 14 October 1983, there was a discussion about the AIDS leaflet, with Dr Gunson commenting that it was at present “the only practical step being taken by the Transfusion Service.”[305] The minutes record that approximately half of the RTCs were distributing the leaflet with call-up cards with the others either having the leaflet available at sessions or being handed out to donors. The Working Group’s view was that a uniform system of distribution[306] would be advantageous. The minutes also noted that RTCs had been asked by the DHSS to report on the distribution at the end of November 1983.[307] Other steps were discussed (including distribution to special clinics, approaches to health education councils and gay societies and highlighting the importance of the message not to give blood if in a high risk group) and it was agreed that these would be raised with the DHSS on 17 October when the Advisory Committee on the NBTS was next to meet.
It is unclear whether these matters were in fact raised with the DHSS as proposed: the minutes of the Advisory Committee’s meeting on 17 October 1983 merely refer to the existence of the leaflet.[308]
The three month period came and passed with little further action. Such as there was consisted of Paul Winstanley making enquiries of regional transfusion directors by phone at around the end of the three month trial period;[309] and Dr Wagstaff (director of Sheffield RTC) also seeking information from regional transfusion directors regarding their use of the leaflet in around late November 1983,[310] which he then tabulated for Paul Winstanley at the start of the next year.[311]
Action seems to have been prompted by a request on behalf of the Medical Society for the Study of Venereal Diseases for copies of the AIDS leaflet to be provided to STD consultants. On 8 February 1984 this request[312] was passed to Dr Smithies by Dr Sibellas under cover of a minute which suggested that RTCs would soon be needing more leaflets, adding “? Preferably the amended version when the others have run out.”[313] Handwritten notes on the minute asked “what is the amended version?”.[314]
The DHSS belatedly realised it needed to take some action. On 14 February 1984 Dr Smithies, who was relatively new in post, wrote to Alun Williams,[315] raising the concern that “our current advice to donors could seem too lax” and that it “may also be necessary to take up with the Transfusion Directors the need for more positive distribution rather than the negative approach that some of the Centres have used.”[316] On 6 March she wrote to Dr Sibellas, referring to the intention to revise the pamphlet (a handwritten note added that this proposal was likely to need ministerial agreement, adding “did we not promise Ministers a progress report on the usefulness of the pamphlet?”);[317] and on 12 March 1984 Steven Green wrote to all transfusion directors, explaining that the leaflet was “due for review”[318] and asking for information about usage, the method of distribution and impact on donor attendance.[319] Regional transfusion directors were also invited to comment on the content of the leaflet.[320]
By now, what ministers had agreed should be a three month trial had begun more than six months earlier.
At the 10 April 1984 meeting of the Advisory Committee on the NBTS, Dr Smithies reported that “The 6 month trial period of the leaflet ‘AIDS and how it concerns blood donors’ was now complete and the survey of RTDs showed little adverse comment. DHSS now proposed to prepare, in consultation with RTDs, a revised version of the leaflet for submission to Ministers.”[321] The Advisory Committee recommended that, in contrast to the trial period when the method of distribution had been left to the discretion of regional transfusion directors, ministers should now consider the issue of the revised leaflet with donor call-up cards in all regions. It is unclear why Dr Smithies referred to a six month trial period: those present from the DHSS (Dr Harris, the Deputy CMO; Dr Smithies, Alun Williams and Steven Green) ought all to have known that ministers had decided upon a three month trial period, not six months.
On 17 April 1984 a submission was sent to ministers, covering a range of matters relating to AIDS.[322] In relation to the AIDS donor leaflet, the submission repeated the (inaccurate) reference to a six month trial, which was described as successful,[323] and explained that both leaflet and method of distribution were “under review”.[324] Lord Glenarthur, in response, sought a fuller note on the NBTS leaflet trial.[325]
It took nearly four months for that note to be provided – an astonishing delay, all the more remarkable when added to the mistake about the length of the trial period, and the relaxed approach to reviewing the results of it.
What happened in the intervening period was to-ing and fro-ing, with no real sense of urgency, regarding amendments to the leaflet. Thus, Dr Smithies sent Dr Sibellas (and others within the Department) a draft amended leaflet on 9 May 1984;[326] comments were received from the Information Division on 16 May[327] and from others within the Department on 23 May;[328] on 6 and 7 June Dr Smithies sent regional transfusion directors the redrafted leaflet for comment, requesting any suggested amendments or comments by 6 July;[329] at the regional transfusion directors’ meeting on 11 July it was recorded that amendments had been sent to Dr Smithies;[330] on 18 July Dr Smithies sent Alun Williams a revised draft of the leaflet and the outline of a draft submission to ministers;[331] on 23 July Dr Smithies wrote to Dr Sibellas and others asking for comments on the redraft before it was sent to ministers;[332] and on 31 July Dr Smithies wrote to Alun Williams saying that the redrafted leaflet had been cleared with Med IMCD and the Information Divisions and was ready for printing “provided Ministers agree.”[333]
A submission was finally sent to Lord Glenarthur on 10 August 1984, almost a year after the first leaflet had been introduced. There was no good reason for it to take so long, and no evidence that any minister chased for it. The submission explained that the current AIDS leaflet was now out of date and that there was a need to strengthen its warning to high risk groups not to donate. Ministers were told that there had been, “as anticipated”, a wide variation in the manner in which the leaflet had been distributed by RTCs and that there should be a “more uniform and consistent distribution system to be adopted by Regional Transfusion Centres in England and Wales.” All regional transfusion directors that did not send out the leaflet individually to registered donors should now be asked to do so;[334] donor teams should also make certain that new or unregistered donors had an opportunity to read the leaflet before they were committed to donation. Ministers were asked to agree to this action and to the revision of the leaflet.[335]
Lord Glenarthur agreed, his approval being communicated by a minute dated 21 August 1984. A handwritten note on the minute suggests that the submission was sent to the Minister of State for Health (Kenneth Clarke) on 14 September, asking if he had any comments or was content for the leaflet to be revised as suggested.[336] On 16 October a minute on behalf of Kenneth Clarke, to Alun Williams, reported that the Minister had now seen the August submission and was “content for the leaflet to be revised and distributed in the way in which you suggest”, adding “I am sorry this has taken so long to clear.”[337]
Despite the clearance of the contents of the revised leaflet and its method of distribution from the minister responsible for blood (Lord Glenarthur) on 21 August, and its (already belated) approval by the Minister of State for Health (Kenneth Clarke) on 16 October, it was another three and a half months before the revised leaflet was put into circulation. Events during that period (described below) would strike an almost farcical note, if the underlying subject matter were not so serious.
On 19 November 1984 Dr Smithies provided a note summarising the current situation on AIDS which had been requested by the Secretary of State for Health (Norman Fowler).[338] Insofar as the leaflet was concerned, the note stated that the revised version was now being printed and would be given to every donor. However on 22 November Janet Hewlett-Davies, in the Information Division, wrote attaching “a revised version of the leaflet drafted by my Publicity Branch.” This endorsed a view which had apparently been expressed by John Cashman[339] that the revised draft circulated previously by Alun Williams had to be looked at again “in the light of recent developments[340] and ministerial statements”[341] and that the need was for “a much more strongly worded leaflet and for urgent approval, production and distribution.”[342] This intervention had the unfortunate effect of slowing down the process even further.
On 22 November 1984 a briefing session with Kenneth Clarke, in preparation for an ITV interview, revealed that, in addition to having strong views on spending money on the blood test for HTLV-3, he was “content to hold up the donor leaflet until after the Working Group meeting”, but was “obviously satisfied with it as it is at present.”[343] His mention of a meeting was to the first meeting (on 27 November) of the new Working Group on AIDS of the Advisory Committee on the NBTS. When it met, it generally endorsed the latest donor leaflet (with “a few small but important changes suggested”) although the closer questioning of donors was not supported.[344]
The importance of the leaflet as a central plank of DHSS policy was apparent from Kenneth Clarke’s statement in Parliament on 28 November, the day after the meeting: “After consulting the Advisory Committee on the National Blood Transfusion Service we have decided to ask all regional blood transfusion centres to issue, on an individual basis to all blood donors, a revised leaflet ‘AIDS and how it concerns blood donors’. This leaflet reinforces our previous advice that persons at high risk of transmitting the AIDS virus should not donate blood.”[345] The statement to Parliament made no reference to the delay in reaching that stage, or to the fact that the wording for the revised leaflet had not yet been agreed.
On 30 November John Patten, having seen Janet Hewlett-Davies’ minute and redrafted leaflet, indicated that he was “Content with this line if MS(H)/PS(L) are.”[346]
On 3 December a revised version with the Working Group’s suggestions was sent to Kenneth Clarke for approval; the covering minute from Dr Michael Abrams set out the Working Group’s view that it was not necessary to adopt the stronger line proposed by the Information Division.[347]
On 4 December Lord Glenarthur indicated that he was content with the revised wording – but he was referring to the Information Division’s rewrite and not the Working Group’s.[348] A handwritten note from Dr Smithies to Alun Williams on 5 December then posed the question “Are we sure that Dr Abrams leaflet is the accepted version now?”[349]
On 14 December – John Patten and Lord Glenarthur having both confirmed approval of the Information Division’s rewrite of the leaflet – Mr Harris of HS1 sent a chasing minute to Kenneth Clarke’s Private Office, referring to the version approved by the Working Group and stressing that it was “highly desirable that action on this is taken forward in the near future.”[350] Kenneth Clarke was chased again on 20 December by Alun Williams: his “urgent” clearance of the revised text of the AIDS leaflet (the Working Group version) was sought, it being pointed out that NBTS could not be asked to effect a more positive distribution of the leaflets until ministers had approved the text.[351] By this time there had been media reports of transmission of HIV by blood transfusion in the UK.[352]
The Minister responded promptly on 20 December, setting out his preference for the Information Division leaflet and asking that officials “co-operate with Information Division in producing a third (and hopefully final) version of the leaflet based upon the ID text to take account of any recent significant developments, and amended as necessary to ensure medical accuracy.”[353] A revised version was sent to the Minister the following day.[354] The Minister responded on 31 December by asking whether it was still true to say that there was only a remote chance of anyone getting AIDS from an ordinary blood transfusion[355] and by requesting the omission of a paragraph describing what else was being done because he remained “wary of offering to promise blood screening tests and heat treatments.”[356]
Attention then moved to the need for a health circular to accompany the publication of the leaflet, which required “to be issued fast.”[357] On 3 January 1985 ministers were sent a draft circular and asked to agree to its issue.[358] Lord Glenarthur and John Patten confirmed their agreement on 15 January 1985.[359]
The health circular was sent to regional health authorities and regional transfusion directors on 23 January 1985 with the leaflets being – finally – available to RTCs by or on 1 February 1985.[360] The circular explained that ministers had decided that it was essential that the revised leaflet be brought to the attention of each donor“on an individual basis”, continuing:
“This would normally be achieved by sending each donor a copy of the leaflet with his next call-up notification. It is realised that this may not be practicable for industrial sessions (or for new donors presenting at sessions) – in these cases alternative arrangements should be made to ensure that each donor is individually given the leaflet before any blood is taken. Displays of leaflets, whilst continuing to be useful, will not meet these new distribution requirements. Because the advice has changed significantly, the revised leaflet should be sent even to those who received the 1983 version.”[361]
The DHSS met the costs of printing the revised leaflet, but any resource implications in distribution, postage etc for RTCs would “have to be found from within existing RHA funding.”[362]
The trial period for the initial leaflet finished at the end of November 1983. It had been delayed in coming, despite it being the only available line of defence against the possibility of infection through blood and domestically made blood products. The need to take whatever steps could reasonably be taken was urgent. Yet the response was delayed.
These delays are almost as nothing when compared to the delay before a revised leaflet was available in England – one should have been decided on by the end of December 1983, if not earlier. It was not until February 1985 that one emerged. The debate had not been about whether or not the original version needed to be strengthened – that was agreed on all fronts – but on the precise wording to be used to provide for this strengthened message. Yet all the time that that message was not “out there” the risks posed to others by donors in high-risk groups were inadequately addressed. Though it cannot be said in the case of any individual that they might have been spared infection with all that followed, it is highly likely that some infections followed which need not have ensued, and should not have done. Moreover, blood was being taken from people who came forward out of a desire to help other people as best they could. They would have been mortified if they learned that there was a real risk that they might have been doing more harm than good, unintentionally, though others had known for some time that they might be, but just hadn’t yet found the right words to tell them this. Such donors were entitled to regard this as a betrayal of their good will.
Lord Glenarthur described the fact that he did not receive a substantive update on the leaflets until nearly a year after their production as “certainly disappointing”.[363] He described the process for producing an amended leaflet as “a protracted and rather bureaucratic process to get it approved and out where it should be, but that seemed to be the system at the time.”[364]
It was more than disappointing. It was, as Lord Glenarthur acknowledged in his evidence to the Inquiry, “an absurdly long period of time … for such an important public health measure”. The “continual toing and froing within the Department and between ministers’ offices, tweaking the leaflet and the statements that go with it, were frustrating … But on the other hand, you know, Mr Clarke had strong views on these things, he was dealing with lots of other things, and it may have been that he didn’t quite perceive the same degree of urgency when he looked at it as those of us who were more immediately involved.”[365] Lord Patten, giving evidence to the Inquiry, could not understand why it had taken so long or why there was no sense of urgency.[366] Even Lord Clarke accepted that the second leaflet “took far too long”,[367] although in terms of his own delay he admitted that it was “unfortunate” only with “the wisdom of hindsight”.[368]
There was no good reason for the failure to review the leaflet and its method of distribution at the end of the agreed three month period; no good reason for the civil servants to be under the illusion that the trial period was six months; no good reason for the failure of civil servants to send a submission to ministers before August 1984; no good reason for the failure of ministers to have raised the matter themselves at an earlier stage, at or towards the end of the three month review period; and no good reason for the delay that then elapsed between August 1984 and January 1985 when the revised leaflet was finally approved.
The result of these multiple failures was that for a year – from January 1984 to January 1985 – a leaflet that was known to be “too lax” in its wording, and which was not being distributed in a way that maximised the prospect of deterring high-risk donors, continued to be used.
As set out in the chapter on Blood Services and Addressing Risk: Response,the first step towards the production of information to discourage high-risk donors was in fact taken in Scotland. The Edinburgh and South East Scotland RTC prepared a draft leaflet in May 1983 which asked various groups to refrain from donating blood.[369] However, by the time the leaflet began to be used in the South East Scotland region in June 1983, the list of “at risk” groups had been amended.[370] Amongst other changes, “Homosexual men” became “Men who have multiple partners of the same sex”[371] and “Anyone who abuses drugs” became “Intravenous drug abusers”. The June 1983 leaflet also included “Haemophiliacs”[372] and recipients of blood transfusion. At an SNBTS meeting on 14 June 1983 Dr Brian McClelland explained that the leaflet was amended following discussion with representatives of the Scottish Homosexual Rights Group.[373]
The first AIDS leaflet that was available across the UK from September 1983 described AIDS as a “new, serious, but rare disease”. It identified three groups as appearing to be “particularly susceptible”: “Homosexual men who have many different partners”,“Drug addicts, male and female, using injections” and “Sexual contacts of people suffering from AIDS”.[374]
In response to the question “How can the risks be reduced?” the leaflet explained that “At present, there is no screening test the Transfusion Service can use to detect people with AIDS. So, until there is and until more is known about this disease, donors are asked not to give blood if they think they may either have the disease or be at risk from it.” The most emphatic part of the leaflet was the response to the question “Will donors be questioned on sexual matters when they attend to give blood?” The answer, in bold and enlarged print, was “Definitely not.”[375]
The wording of this first leaflet was problematic in at least the following five respects. First, those in the risk groups were merely requested not to give blood, rather than being instructed that they should not or must not give blood. Second, the request was contingent upon the donor thinking “they may either have the disease or be at risk from it”, but the leaflet twice described the disease as rare, and in terms of the numbers of cases in the UK indicated that “about a dozen cases have been reported, by the middle of 1983.”[376] Donors might, not unreasonably, have thought it unlikely that they themselves would be at risk of such a rare disease and thus thought that they did not need to self-exclude. Third, the risk group in relation to homosexual men was limited to those “who have many different partners”: this was problematic both in terms of the present tense (“have”) and in terms of the reference to “many different partners” – those who had only one partner or more than one (but not “many” – whatever that meant) would not think to self-exclude; nor would they have thought themselves excluded if they had had only one partner, but that partner had had several others before him.[377] Fourth, the risk group in relation to IV drug use was limited to “Drug addicts”: those who had previously engaged in IV drug use but no longer did so, or who had used drugs but did not consider themselves to be “addicts”, would not necessarily think to self-exclude. Fifth, the risk group in relation to sexual contacts was limited to the sexual contacts of those suffering from AIDS, rather than sexual contacts of people at risk of AIDS.
By February 1984 the DHSS had acknowledged the need to amend the advice within the leaflet, but it should have been evident from the outset that the first leaflet was, as Dr Smithies put it, “too lax.”[378] It was too tentative in merely asking donors not to donate if they thought they had, or might be at risk of, AIDS. Something stronger, making plain in emphatic terms that donors must not give blood if they fell within the at-risk groups, was required from the beginning. It was too narrow in its delineation of the at-risk groups.[379] There was, amongst both ministers (primarily Kenneth Clarke) and regional transfusion directors, a misplaced concern not to offend – whether the concern was one of offending those in the gay community, or offending other donors by raising (even if just in a leaflet) matters of sexual behaviour, or both. Such concerns should not have been allowed either to slow down the process of producing the leaflet, or to water down its content.
The press release which accompanied the publication of the second AIDS leaflet on 1 February 1985 reported the Minister, Kenneth Clarke, as saying “The new leaflet is more explicit than the previous version. It lists those at risk from AIDS – practising homosexual and bisexual men; drug abusers, both men and women, who inject drugs; and the sexual contacts of people in these groups – and stresses that donors in the risk groups must not give blood as they may unknowingly be carriers of the AIDS virus.”[380] The second leaflet had thus been introduced in recognition of the limitations of the first. It was an improvement, not least because of the emphatic “IMPORTANT NEW ADVICE FOR BLOOD DONORS” on the front of the leaflet, and because it stated that “Donors in the risk groups must not give blood”.[381] However, two of the risk groups were still ambiguously and confusingly described.[382] The first was described as “Practising homosexual and bisexual men”. Whilst there was no longer the reference to “many different partners”, the word “practising” was ambiguous[383] and would exclude those who (perhaps because of fear of transmission of AIDS) might have stopped having sexual relations with men. Drug “addicts” had been replaced by “Drug abusers”, but this was qualified by the phrase “who inject drugs”: the present tense thus did not encompass those who had previously injected drugs but no longer did.
By the time the second leaflet was issued, it had already been recognised that it needed further redrafting. At the very first meeting of the Expert Advisory Group on AIDS (“EAGA”) on 29 January 1985 it was recorded that:
“The blood-donor leaflet was not considered sufficiently forceful. It needed some redrafting particularly with regard to its objective of persuading homosexuals not to donate blood. Consideration should be given to the introduction of some means by which the ‘closetted’ homosexual – possibly faced at a visit to a NBTS Centre with advice not to give blood – could unobtrusively withdraw from the system.”[384]
A third AIDS leaflet, produced in September 1985, redefined and simplified the first at-risk group by removing the word “practising”. Thus “homosexual and bisexual men” were now told not to give blood: “People in the high risk groups MUST NOT GIVE BLOOD. They should not attend donor sessions. The test may not pick up early cases of infection.”[385] It is unclear why this amendment was not made until September 1985: it may have been because the third leaflet also explained to donors that donations would now include a test for antibody to the AIDS virus and that its introduction was thus timed to coincide with the introduction of HIV screening in October 1985.[386]
The advice to potential donors became even clearer in September 1986 with the addition of dates: “Men who have had sex with another man at any time since 1978. Drug users, both men and women, who have injected drugs at any time since 1978”, thus making it clear for the first time that a single sexual encounter or use of injected drugs would be sufficient to prevent a person from giving blood.[387] Such wording should have been adopted from the outset.
As set out above, the AIDS leaflet was one of the few, key, measures that could be taken to try to ensure that those donors most likely to transmit the virus did not donate. The delay in producing the first leaflet, the failure to stipulate the most effective method of distribution, the delay in producing a revised second leaflet, and the terms in which both leaflets (particularly the first) were expressed increased the risk that donors from high risk groups might continue to give blood and that the recipients of transfusions (or of blood products made domestically) might be infected. The safety of the blood supply, not a preoccupation with adverse publicity, should have been the central focus.
The potential consequences of the failure to act earlier, more speedily and more decisively in relation to the production and dissemination of the AIDS leaflet are plain. They are starkly illustrated in the case of the Wessex donor: a donor diagnosed with AIDS at Bournemouth Hospital in autumn 1984, who had previously donated blood, including in late March 1984. Transfusions had been given to three recipients all of whom were infected with HIV in consequence.[388] The donor’s plasma was also part of the source material for one batch of Factor 8 concentrate (HL3186) which was used in the treatment of 38 people with bleeding disorders in Wessex and South Wales and which transmitted HIV to a number of recipients.[389]
Professor Bloom appears to have played a central part in shaping the thinking of the DHSS and others. Fuller details of his activities are described elsewhere in this Report. However, he was the principal haemophilia clinician from whom Dr Walford sought advice.[390] He was the only haemophilia expert who participated in the meeting of the CSM(B) on 13 July 1983, having been invited by Dr Joseph Smith. He shaped the views of the Haemophilia Society, who in turn made representations to the DHSS about the correct response to AIDS. He was, amongst other roles, a member of the CBLA and its Committee on Research and Development in Blood Transfusion, the MRC Working Party on AIDS, the Expert Advisory Group on AIDS and the Working Group on AIDS of the Advisory Committee to the NBTS. His was the dominant voice in relation to haemophilia treatment and it is likely that his views influenced the way in which the DHSS viewed the emergence of AIDS and the threat posed to people with bleeding disorders.
Lord Fowler rightly recorded that it would concern him if the DHSS was largely taking its advice about haemophilia care from one clinician – it would not, he said, be good practice.[391] Yet this was undoubtedly the position. There was an over-reliance on Professor Bloom’s input that may have, amongst other matters, influenced the response of the CSM and the approach of the DHSS to the assessment of relative risks. There was an uncritical acceptance of his line of thinking and a failure to challenge or at least probe the advice being provided.
Allied with the over-reliance on a single haemophilia clinician was the failure to establish a body such as the Expert Advisory Group on AIDS until late 1984. As set out earlier in this chapter, the idea of a working group on AIDS was mooted but rejected by the DHSS in May 1983. Dr Walford thought it would have been wonderful to have had an expert group reporting to the CMO with multidisciplinary doctors and scientists to give the best view and that in retrospect it was “a terrible shame that we didn’t”.[392] Sir Donald Acheson, in his later biography, described the decision to establish EAGA in the following terms:
“As far as HIV/Aids was concerned, a few cases of what was already seen as a fatal virus infection associated with infected blood and sexual intercourse had already occurred prior to my appointment. I decided that the implications of the infection were so serious and our knowledge so limited that I should seek expert advice as soon as possible. The expert advisory group on Aids (EAGA) was set up and having met seven times in 1985 and regularly thereafter, it made a series of recommendations which led to more effective control of HIV/Aids within the UK, than in any other country that had links with the African continent.” [393]
However, the dates do not support Sir Donald’s claim to have acted “as soon as possible”: he began work as CMO (overlapping with his predecessor) in around October 1983; EAGA met for the first time in January 1985.[394]
It is not clear why the initiative to establish EAGA was not seized earlier, in 1983: had the DHSS done so, it would have provided a multidisciplinary forum for the proactive discussion of the issues that have been explored earlier in this chapter and might have led to more decisive and earlier action.
The role of CMO is a particularly important one, not least because the vast majority of ministers appointed to positions within the DHSS had no prior health knowledge, experience or expertise,[395] and because of frequent ministerial churn.
The role of the CMO, as described by Lord Michael Forsyth (referring to the CMO for Scotland but equally applicable to other CMOs), was to inform “Ministers and the public of risks to Public Health and advising on policy measures to minimise these risks. He was also responsible for giving guidance to clinicians, health boards and patients where he thought it appropriate.”[396]
However, the CMO was conspicuous by his absence from discussions and decision-making relating to AIDS in the period from mid 1982 to late 1984.
Lord Glenarthur recalled only very occasional dealings with the CMO.[397] Lord Patten never met Sir Henry Yellowlees, as far as he could remember, but did have interactions with Dr Acheson although there was no system of regular meetings with the CMO.[398] Lord Fowler described Sir Henry as a remote figure whom he saw “hardly at all.”[399] Whilst on 9 June 1983 Dr Gunson wrote directly to Sir Henry Yellowlees, raising concerns about AIDS,[400] there is no record of any reply, although the CMO did around this time ask for a briefing on AIDS to be provided to Lord Glenarthur.[401]
It took Dr Acheson some time – too long – to appreciate, and respond to, the gravity of the situation: there is no evidence of any active engagement in late 1983 or for most of 1984. He did write to Dr Gunson early in his appointment to ask for “a brief account of the advances in your specialty that have occurred in the past five years and the problems and opportunities which you can anticipate in the next five years.”[402] However, it was not until late 1984 that there began to be any real involvement by the CMO, and by the Secretary of State, in the response to AIDS. In October 1984 the CMO requested information about “the problems of AIDS and blood donations”, which was provided by Dr Smithies on 19 October 1984.[403] In November 1984 the Secretary of State asked for a note summarising the current situation, which was provided by Dr Smithies on 19 November 1984,[404] and a paper setting out the current position with regard to AIDS was requested by the CMO in December 1984, with a draft being circulated by Dr Smithies for comment on 31 December.[405] Lord Fowler’s recollection, giving evidence to the Inquiry, was that from 1984, going into 1985, “there was a feeling of impending crisis”, and that it was “probably during the early part of 1985 that we became thoroughly engaged in it.”[406]
There is ample evidence of the CMO’s active involvement from this time onwards. By July 1985 the CMO was wanting to be able to give an assurance to the Secretary of State that no people with haemophilia would be infected in the UK from then on.[407] Lord Fowler wanted by this time to become involved with the AIDS issue because it was quite clear that unless a Cabinet minister took charge “we weren’t going to make much progress.”[408] By the end of July the CMO was arranging for a letter to go to all haemophilia centre directors to draw their attention to the availability of heat-treated Factor 8 and the need to avoid using any commercial unheated product that might remain from 1984.[409] What is unclear is why there was no such active engagement at an earlier stage, at least from mid 1982 onwards.[410]
It is apparent that one reason for the absence of guidance or information or advice to doctors from the CMO at an earlier stage was the concept of “clinical freedom”. In 1990 the CMO wrote that “Ministers accord great importance to the principle of clinical freedom.”[411] Dr Roger Moore told the Inquiry that this was a “major … tenet” which “put a limitation on what the Department could do with clinicians … across all policy areas, clinical freedom was a mantra.”[412] Dr Walford described a policy of non-interference with matters of clinical practice; if patients were being treated in a way which exposed them to potentially avoidable risks, she thought that the Department would convene an expert group.[413]
Yet the CMO role had (at least) threefold responsibilities: providing advice to ministers, providing leadership to the medical officers working at the DHSS and, critically, providing public health information to the medical profession and the wider public. Colloquially the role was often described as being “the Nation’s Doctor”. Lord Fowler described the CMO role as including “providing independent advice on public health issues and recommending policy changes to improve public health outcomes. I also considered the CMO to have some responsibility for keeping the public informed on health issues of public concern and explaining the Government’s response.”[414] The CMO, in contrast to most other civil servants, “had the option of making public statements in his own right.”[415] Dr James McKenna recalled that he “was responsible for advising the public on matters of public health … advised Ministers on all health issues and provided the basis for health policy decisions … was frequently in the position of providing health advice to the public at large.”[416]
Furthermore, announcements weremade, when the CMO so chose, by way of “Dear Doctor” letters circulated to the medical profession via local medical officers and GPs. Thus, for example, a Dear Doctor letter was issued on 31 December 1981, relaying advice on Hepatitis B Surface Antigen Carriers among NHS staff.[417] In October 1982, a Dear Doctor letter provided guidance on use of the Hepatitis B vaccine.[418] In May 1985, the first Dear Doctor letter regarding AIDS was issued, providing general information for doctors[419] and advising doctors to bear the diagnosis in mind;[420] possible clinical presentations and precautionary measures were described. In the accompanying press release the CMO said: “This latest initiative is part of a series of public health measures aimed at health professionals and people at risk. I hope it will provide doctors with information which they will find helpful in the diagnosis and treatment of the disease and in counselling those who have worries about it.”[421]
The extent to which the CMO could direct clinicians without infringing on their decision-making autonomy was commented on by various witnesses but misses the point. Lord Clarke’s evidence was that: “it would not have been appropriate for the CMO to provide ‘instruction’ to clinicians about the treatment of their patients. The Department did not then and does not now supervise how patients are treated and clinical freedom was and remains an important and respected principle.”[422] Lord Fowler’s evidence was that: “The CMO’s role – as I understood it – did not extend to giving prescriptive guidance to clinicians of that kind. Clinical decision making was for the practising professionals themselves and that freedom was seen by them as important and was generally respected.”[423] The fact that the CMO might understandably be reticent about directing or instructing clinicians was not, however, a good reason for not providing information, advice or guidance – both for the benefit of clinicians and the benefit of patients.
One function of the CMO role (since the 1859 Public Health Act) was to report annually on the state of the nation’s health.[424] These reports provide an insight into the knowledge and priorities of the CMO and the medical personnel at DHSS. There is little reference to hepatitis in the reports in the first half of the 1980s.[425] The first mention of AIDS appeared in the 1982 annual report with reference to the CDSC surveillance.[426] The 1983 annual report included more detailed information regarding AIDS.[427] The 1985 annual report[428] addressed AIDS but with no section on hepatitis, perhaps reflecting the CMO’s new focus on the AIDS crisis. In the 1986 annual report, Sir Donald Acheson addressed AIDS as the first topic in his introduction, noting that cases of and deaths from AIDS showed exponential growth.[429] Again, there was no section on hepatitis. The 1987 annual report again addressed AIDS in the introduction, but less prominently, with a focus on international cooperation;[430] once more, there was no section on hepatitis. The same was true for the 1988 annual report.[431]
Ministers were very dependent on the civil service advice which they received – “enormous reliance”, in Lord Glenarthur’s words, particularly in scientific and clinical fields.[432] There were no regular meetings with the CMO or with the consultant advisers to the CMO, and the principal sources of information for ministers lay within the DHSS: ministers did not, for example, have any direct dealings with committees or working parties.[433]
As set out earlier in this chapter, ministers did not see everything that was produced by or within the DHSS. A decision would be made by civil servants as to whether to provide information to the minister’s private office, and a second decision would be made by the civil servants within the private office as to whether the information should be seen by the minister.[434]
There was no particular yardstick or criterion for when something had to be brought to a minister’s attention and when it did not. Dr Walford described it as a “rather arcane art”.[435] Lord Glenarthur thought that ministers were very concerned to ensure that any public statements on issues were properly handled and that substantial changes of policy would be brought to the minister’s attention.[436] Lord Patten told the Inquiry that ministerial submissions would be required for a change of policy or significant new spending commitments; he acknowledged also that a concern about media interest or adverse press comment might also lead to a matter being brought to the attention of ministers.[437] Peter Wormald, who was the Under-Secretary in the DHSS from late 1978 to late 1981, said that all senior civil servants “must have continuously in mind the need to keep Ministers sufficiently informed and to seek Ministerial decisions when appropriate.”[438]
There was no training or induction process for ministers – there would be written briefings on some issues, oral briefings on others, “The rest, frankly, was learning on the job as issues arose … You were pitched in, frankly, and got on with it but you could always call for help if necessary.”[439]Ministers had little contact with patients or patient groups and only occasional contact with clinicians.[440] It was and remains the convention not to share with ministers the details of decisions taken by ministers in previous administrations or the official advice on which those decisions were based or grant access to papers of previous administrations (at least those of a different political party).[441] The result in the case of policy on blood and blood products was that ministers would not always be briefed in depth on how policy had been derived or on the history of how a policy had come to be adopted, including how it affected patient safety.
Lord Fowler told the Inquiry that one of the most important qualities of a minister is that they must challenge what is being put in front of them.[442]
According to Lord Clarke “blood products was something that hardly ever came across my desk”.[443] He suggested that the CMO “really, was the person in charge of all the medical things”.[444] It was “complete nonsense” to suggest that the minister would have anything to do with the doctor-patient relationship.[445] There would be “constant interaction” between the medical and other clinical professions and the DHSS and that included public health messages.[446]
The evidence available to the Inquiry demonstrates that many matters which should have come to the attention of ministers did not. There was no particular logic or consistency in what went to ministers and what did not. They were not told of the CSM/CSM(B) decision-making. They were not told of Dr Galbraith’s recommendations. As far as Lord Glenarthur was aware, he was not told in late 1984 that it had been learnt that a number of individuals in Scotland had been infected with HIV through NHS Factor 8 produced at the Protein Fractionation Centre (“PFC”).[447] Yet three ministers became involved – in Kenneth Clarke’s case, particularly closely involved – with the detail of what should appear in the AIDS donor leaflet and how it should be distributed.
It is, of course, not the fault of ministers if civil servants do not bring matters to their attention. It is, however, the responsibility of ministers to demonstrate a degree of proactivity and to challenge, as Lord Fowler and Lord Clarke both acknowledged. The DHSS was a very large department. Its ministers had a wide range of topics and responsibilities with which to deal. They faced considerable pressures. Notwithstanding that, there is little evidence, except to some extent in the case of Lord Clarke, of challenge. Although both Lord Glenarthur and Lord Patten responded promptly to most of the communications they received, demonstrating an appreciation that dealing with AIDS required a swift response, and although there are examples of proactivity on the part of the ministers (such as Lord Glenarthur asking for a briefing from the CMO in June 1983[448] and Lord Patten engaging with the AIDS leaflet, and giving impetus to the evaluation process in respect of HIV screening when it became sluggish) when viewed overall ministers appear to have lacked much curiosity in the early period of the developing public health crisis. No minister, for example, asked officials to investigate what other steps could be taken to protect people with bleeding disorders short of the more radical step of stopping the importation of concentrates.
It did not help that all three ministers most closely concerned with the threat of AIDS in blood and blood products were relatively recent in post. Lord Glenarthur served in the House of Lords as Parliamentary Under-Secretary of State at the DHSS from 14 June 1983 until 26 March 1985; and John Patten in the House of Commons as Parliamentary Under-Secretary of State for Health in the DHSS from 14 June 1983 to 2 September 1985. Neither was thus able to draw on the experience of the other in respect of threats which were already emerging by the time they took office. Kenneth Clarke was in post for a little longer – from 5 March 1982 until September 1985 – and his tenure thus covered the main period of rapid adjustment to the threat of AIDS.
There was evidence or material which they did not see, but should have seen. This did not help.[449]
Both Lord Glenarthur and Lord Patten genuinely endeavoured to assist the Inquiry. By contrast, Lord Clarke was combative: he described his natural style as seeking to challenge, and that extended to his questioning why he should have been asked to give any evidence at all to the Inquiry.[450] He claimed that unless someone pointed out to him that something was going on, he had nothing to do with blood transfusion or products and that “The campaigners attributed everything to me because I later became a well-known figure.”[451] He was at pains to point out his lack of involvement and lack of responsibility. He seemed to argue that any failure on the part of government did not have any effect on anybody’s health, even though he was obviously not in a position to know whether that was the case (indeed he did not even appear to be aware that people were infected with AIDS from the British blood supply, as well as that which was imported, and wondered whether Factor 8 was a pill to be taken at home).[452] He thought it was “daft” that he be asked detailed questions “about events 40 years ago in a busy Government Department where this was a tiny, tiny proportion of my activity.”[453]
He was firmly of the view that if you stopped giving Factor 8 “you were killing some haemophiliacs” and postulated that had the decision to stop imports been taken, whilst lives would have been saved, “we” (the Government) would “have continued to this day to be reviled for condemning haemophiliacs to going back to the kind of life they’d enjoyed before this wonder treatment was devised.”[454] He did not think that there was anything the DHSS did wrong and asserted that if the Inquiry came to the conclusion that the introduction of HIV screening took too long “I would reject the conclusion.”[455]
This chapter is concerned with the response of government to the risks of infection as and when they arose. As has already been made clear, the Terms of Reference cover not just what happened (to cause infections, disease and death from treatment) but the government response to what had happened – its approach to complaints by those infected and affected about what had happened, its reluctance for many years either to contemplate compensation or to hold a public inquiry, and the possibility that it may have been concerned to cover up the true facts. Since the evidence of Lord Clarke relates (so far as facts are concerned) to his involvement in the events of 1983 to 1985, his views now as to the Government’s response to what had happened, after much of it had happened – when it emerged that the worst treatment disaster in the history of the NHS may have occurred – may not fit naturally within the scope of this chapter. However, it is unlikely that anyone who heard him give evidence orally will easily forget it, nor forget the argumentative style in which it was given. It is thus appropriate to deal now with some of what he said about this second aspect, namely his views as to whether there should have been a public inquiry at all, and the motives of those who campaigned for it.
He complained that the Inquiry was engaged in “historical research … with the elderly survivors ... of those who are in the Department at the time” years after the events in question.[456] However, to the extent that this is true, I should state here – first – that much of the value of history lies in learning from the past what mistakes may have been made, so as to help to avoid similar errors in future. Second, the survivors (and many of those who were involved in their treatment) would not have been “elderly” if successive governments, of some of which he was a member, had established an inquiry earlier rather than rejecting calls for one.[457] I agree that this Inquiry has been held far too late – but this is not down to the Inquiry, but successive governments which failed to hold one earlier.
As to the motives of those who complained about their treatment, he referred to what he “had to put up with”because he remained “the best-known person of all those people involved”, claiming that campaigners were “always trying to steer [inquiries] to try to find some celebrity whose fault it was.”[458] I do not accept that this is a fair characterisation of the motives of campaigners. Nor do I accept that the allegations of fault which have been made since infections occurred as they did are centred on him. What he said was unfairly dismissive of, and disparaging towards, many who have suffered physically, mentally, socially and financially from what occurred – in which he played some part, but in which (as this Report shows) many others did too. This will have aggravated the distress and upset of many.
Lord Clarke may hold the view that nothing wrong was done, that a public inquiry serves no purpose, and that therefore those who called for one were wrong to do so. It is regrettable that he could not moderate his natural combative style in expressing these views. It detracts from a dispassionate evaluation of what he had to say about the facts, which it was important to hear. It is right nonetheless to acknowledge that he balanced what he had said at the end of his testimony – in a way which perhaps highlighted that his normal style is to challenge – by saying that:
“it is one of those terrible incidents of my lifetime … despite, you know, my strong feelings, it was a terrible tragedy … this is probably the worst tragedy that’s ever occurred, and … everybody … is acutely aware of the human suffering that was being caused whilst this HIV and then these infections being spreading [sic] to haemophiliacs carried on … And I genuinely feel very great sympathies, to say the least.”[459]
Several other ministers, whether serving in a junior or senior role, may have taken positions or expressed views with which others participating in the Inquiry might disagree. The Inquiry is fortunate that they have done so in a measured, less personalised way, than Lord Clarke did: indeed, adopting the helpful, responsive or responsible approach to the provision of evidence to a public inquiry into the infection and deaths of thousands of people which the public has the right to expect from former government ministers.
There were in the 1970s and 1980s a range of committees/working groups/expert groups which advised the DHSS (and often more widely the whole of the UK) on matters which included hepatitis and HIV. Leaving aside the Committee on Safety of Medicines, which had a specific statutory remit, these committees and groups, some of which are considered below, had varying functions.[460]
Navigating these committees, appreciating the extent to which their remit differed from or overlapped with others, and forming a perspective upon the extent to which any contributed significantly to clinical, regional or central governmental policies is not easy. There may seem at first to be a somewhat confusing list of names.
The list is set out below. However, what is important to recognise at the start of charting a territory through what may seem like an overcrowded landscape is that there was, until 1989, no overarching advisory committee on blood safety. This omission was rectified with the establishment of the Advisory Committee on the Virological Safety of Blood (“ACVSB”) in 1989. It is also important to recognise that each committee or sub-committee or working group had advisory powers only.
The bodies were:
The Maycock Group was appointed as an advisory group in September 1970. It was a joint appointment between the DHSS, the SHHD and the Welsh Office, and its terms of reference were to advise on the organisation of and responsibility for testing blood donations for Hepatitis B Surface Antigen (“HBsAg”) and its antibody and on related matters.[462] In its first report, published in May 1972, its principal recommendation was the introduction of testing of all blood donations for HBsAg and its antibody.[463] The Group reconvened in December 1973[464] and met on five occasions, resulting in the publication of a second report in September 1975. The recommendations in the second report included a change in the method of testing for HBsAg.[465] In November 1979 the group reconvened to consider whether any alterations in the methods used for testing donations was desirable.[466]
At the Group’s meeting in March 1980, members “agreed that the hazard from non-A, non-B hepatitis should now be recognised and brought to the attention of the appropriate Departmental bodies responsible for control of hepatitis.”[467] It is not clear what, if anything, was done in response to that proposal.
In a third report, published in 1981, the Group reviewed the current position regarding HBsAg screening and made various recommendations. It also considered, briefly, non-A non-B Hepatitis (“NANBH”), recommending that research be undertaken in the UK to determine the extent and severity of post-transfusion hepatitis due to NANBH; that regional transfusion directors should encourage hospital haematologists to report all cases of post-transfusion jaundice; and that where such jaundice could be due to NANBH, the facts should be reported to the DHSS or SHHD.[468] A separate recommendation was made for the establishment of a committee of experts to assess the value of any new tests for hepatitis markers which could be used in testing blood donations and preparations of large pool blood products.[469]
At the March 1980 meeting of the Maycock Group, Dr Walford and Dr Sibellas had explained that a new committee was being set up to deal with all aspects of communicable hepatitis and that it was the intention that the Maycock Group should become one of its sub-committees. Members expressed concern at the meeting about the incidence of NANBH.[470] Dr Walford observed that the reason the Deputy CMO had proposed to the CMO that there should be an overarching hepatitis advisory group was “because there was a realisation that this was becoming an issue and that the Department -- there shouldn’t be a whole lot of disparate committees or groups looking at things in isolation”.[471]
At the next meeting of the Maycock Group in September 1980, Dr Sibellas referred to numerous requests the DHSS had received for advice on diverse problems regarding viral hepatitis, with “non-A non-B being particularly problematic” and that it had been decided that it was essential to set up an advisory group to consider and advise on these matters. This group (the Advisory Group on Hepatitis) would meet for the first time in October and its terms of reference were “To provide medical advice to the Chief Medical Officers of the Health Departments of the United Kingdom on all aspects of communicable hepatitis.”[472]
The idea for a new Advisory Group on Hepatitis had been raised over a year earlier. Dr Terry Geffen[473] wrote to Dr John Evans[474] in early July 1979, to the effect that it had been in his mind “for several months” to get together “an outside group of experts to act as an Advisory Group on Hepatitis”.[475] Dr Geffen’s note observed that “This may not be the time to ask about a new advisory group, particularly if we are proposing to be extremely restricted in the amount of advice which we give to the field, but if there is an infectious disease for which such a group is needed, this is it.”[476] Dr Evans responded, “after discussion with CMO and the DCMOs”, that the DHSS should go ahead to take “professional advice on the serious and pressing problems relating to hepatitis particularly those relating to so called carriers of Australia antigen.”[477]
After a meeting on 17 July,[478] Dr Sibellas followed this up on 18 July 1979 with a suggestion that it should be a free-standing committee which would only meet occasionally but would be available to give advice if required; she noted that since the Rosenheim Report had been written in 1972, there was “now at least one new type of viral hepatitis” which had not been discovered at that time (ie non-A non-B Hepatitis), and identified among “the many problems currently facing us” the “hepatitis risks involved in blood transfusion.”[479]
On 24 July 1979 Dr Geffen produced a paper, to go to the CMO, setting out the reasons why an advisory group on viral hepatitis should be established; he noted that “At present hepatitis B presents the majority of problems and is responsible for the majority of enquiries but non-A/non-B hepatitis may well also become a major source of concern”. Current problems in the field included “the possible hazards of the use of blood and blood products”: “Hepatitis B was originally referred to as serum hepatitis and is still often regarded as being in the main associated with the use of contaminated blood and blood products. While other forms of transmission are now known to be important, the risks involved in blood transfusion are still considerable and the subject of many enquiries.”[480]
By November 1979 little progress had been made: according to a further minute from Dr Geffen to Dr Evans on 6 November, other than preliminary discussions with SHHD, the DHSS had “taken no definitive action on this since August”. Reference was made to the “need not to establish new advisory or other bodies without very good reason”. Attaching the new group to the existing Maycock Group would “present real difficulties” because of that Group’s “limited function”, which “in no way touches on the problems with which we are likely to be mainly concerned, and on which we would need advice, in the next few years”. Dr Geffen therefore recommended a new body be established.[481]
In February 1980 Dr Evans and Dr Harris (both Deputy CMOs) discussed the matter with the CMO and it was agreed that the numerous problems arising in relation to hepatitis needed to be brought together into one Advisory Group on Hepatitis “rather than be dealt with in scattered fashion by various ad hoc groups”, and that its terms of reference should be wide enough to encompass “the specialist advice needed by blood transfusion experts.”[482]
The creation of a new advisory group or committee being a matter that required ministerial sign-off, the CMO wrote to the Minister of State for Health, Dr Gerald Vaughan, on 13 June 1980, emphasising that there was “an urgent need to pull together our various sources of advice on hepatitis into one proper professional advisory group capable of giving authoritative and coherent medical advice about these diseases.”[483] The ministerial submission did not refer to non-A non-B Hepatitis by that name, but did record that “Infections resembling those due to hepatitis B are known to be caused by one or more other agents which have not been fully identified.”[484]
By late June 1980 ministerial approval had been forthcoming “with the strict proviso that there should be no other Committees concerned with Hepatitis in operation.”[485] At the request of health departments in Scotland, Wales and Northern Ireland, the Group would advise all the departments in the UK, each of which would have an officer present at meetings.[486]
Thus, despite the need for the expert group having been identified in July 1979, it was not established until the autumn of 1980.
The first meeting of this new Advisory Group on Hepatitis was on 3 October 1980: there was no discussion about non-A non-B Hepatitis (“NANBH”).[487] The second meeting was on 5 December 1980: again no discussion about NANBH.[488] The third was on 11 May 1981: still no discussion of NANBH.[489] The fourth meeting was in October 1981: again nothing on NANBH.[490] A year then elapsed before the fifth meeting in October 1982: Hepatitis A and Hepatitis B were both considered, but not NANBH.[491] The next meeting took place a year later, in October 1983: on this occasion AIDS was discussed as well as Hepatitis B, but not NANBH.[492] Nor was NANBH considered at either of the Advisory Group’s 1984 meetings,[493] nor at its October 1985 meeting,[494] nor its July 1987 meeting.[495]
The February 1989 meeting merely noted that there was a paper on “NANB virus in blood for transfusion” but there was no discussion about the issue.[496] By this time, of course, the ACVSB was being set up.[497] The December 1990 meeting of the Advisory Group on Hepatitis again contained no consideration of NANBH/Hepatitis C, other than recording that the blood transfusion service would be testing donations from 1991.[498]
This Advisory Group took too long to establish, the need for it having been identified by mid 1979. Dr Walford described the Department as “quite monolith”, with “an element of bureaucracy involved” and acknowledged that “one of the issues that should have been of considerable concern, which was non-A, non-B, was not perhaps getting the attention that it should have got.”[499] She was absolutely right.
Furthermore, once established, and despite the fact that it was envisaged at the time of its establishment that the Advisory Group on Hepatitis would provide expert advice on the prevention and management of NANBH, it failed to consider and advise on this question at all. This was symptomatic of a wider problem within government in the 1980s, namely the lack of attention paid to NANBH and its transmission through blood and blood products.
The origins of the MRC’s Blood Transfusion Research Committee dated back to the 1940s, with the Committee being reconstituted from time to time and specific working parties being set up under its auspices.[500] Its terms of reference were to advise the MRC on research within the field of blood transfusion.
The Committee set up a number of working parties. One was a Working Party on Post-Transfusion Hepatitis. Its terms of reference were “To consider the feasibility of carrying out a survey on the incidence of post-transfusion hepatitis and to arrange for any such survey.”[501] It met a number of times between 1967 and 1970. The extent of its meetings in the 1970s is however unclear: a paper from 1978 reported that at that time it had not met for two or three years, but Professor Zuckerman was pressing for it to be reconvened on the basis that “there are no data from the UK or Europe on the importance of so-called non-A, non-B viruses … When a test becomes available, it will be difficult to decide on policy in the UK unless the size of the problem is known.”[502]
The main Committee was reconstituted in 1979, having not met since 1976, and at its first meeting in December 1979 discussed, amongst other matters, the encouragement of the use of red cell concentrates. It noted that the transmission of NANBH “was still a problem with factor VIII concentrates”. Other than agreeing to establish a working party to study the use of red cell concentrates and albumin preparations, and to take proposals for an appropriate clinical trial, no specific decisions or actions were agreed.[503] The Committee did not meet again for 18 months: at its second meeting in June 1981 Dr Gunson, chair of the Committee’s Working Party on Post-Transfusion Hepatitis, reported on its main concern: NANBH. The minutes record his observation that “large-pool blood products were especially likely to cause liver damage in haemophiliacs”. In discussion the Committee noted that:
“MRC, DHSS and the Directors of Transfusion Centres were all interested in the field of post transfusion hepatitis. It was agreed that there was at present no need to screen potential blood donors for non-A non-B hepatitis but the production of a vaccine would be waited with interest, mean-time it would be valuable to follow-up those patients previously found to have a raised serum level of alanine transaminase after blood transfusion to find out their present state.”[504]
This was a somewhat curious statement. The reference to screening potential blood donors was presumably a reference to surrogate testing, but no reasoning was provided for the suggestion that there was no “need” for this; a vaccine was unlikely to be on the horizon given that the virus had not yet been identified; and once it was so identified the first step to take would be screening rather than vaccination. As for the follow-up of patients, no specific action or decision appears to have been taken by the Committee in this regard: the minutes simply record that the exercise would be “valuable”.
The reconvened Committee met for a third (and final) time in March 1982. It was decided to disband the Post-Transfusion Hepatitis Working Party, because it was “in a field in which many other groups, both inside and outside the MRC, were active” and that matters in the field of post-transfusion hepatitis arising in the future should be passed to “an appropriate advisory body.”[505] There was then a discussion about the future of the Committee itself: Dr Gunson thought it needed to “justify its existence”, whilst the DHSS favoured its continuance.[506]
The Committee was disbanded in July 1982, the MRC board having concluded that its work was being duplicated elsewhere.[507]
The ACDP was established in 1981.[508] It provided advice to the health ministers of the UK, the agriculture ministers, the Health and Safety Commission and the Health and Safety Executive (“HSE”).[509] Its meetings were (as was commonplace at the time) private and individual members were required not to disclose its decisions. It would normally be for those whom it advised to determine whether any public statement should be made.[510] Unusually, its inaugural meeting in June 1981 was attended by the Minister of State for Health, Dr Gerard Vaughan.[511] The ACDP’s work related to a wide range of pathogens and viruses, and many of its early meetings focused on questions of categorisation, but of note are its observations in 1983 on NANBH and on AIDS. In relation to NANBH, its September 1983 meeting discussed the categorisation of NANBH viruses, with the Chair explaining that “as these viruses had a more serious effect than Hepatitis A, in fact nearly as serious as Hepatitis B, it was decided to use the same category as for the latter”.[512]
At the same meeting, Dr Walford raised the topic of AIDS, explaining that both the DHSS and the HSE were receiving enquiries on the handling of AIDS cases: “Both Departments would like some guidance from ACDP and hopefully a Working Group set up to look into, and report on this problem.”The ACDP agreed recommendations for the safety of health-care workers, noting that “It appears that blood and secretions may well carry the infection”; it was also agreed that a small working group should be formed to “look into this matter more deeply.”[513] In advance of the meeting, Dr Walford, in a minute to Dr Oliver and John Parker, expressed the view that “we have now reached the stage with AIDS where we are obliged to seek expert advice.” The ACDP was, she said, “by no means the best possible source of advice on AIDS but, because it exists and because of the status it has been accorded, it is currently the most appropriate source of such advice.”[514]
The inaugural meeting of the UK Working Party on Transfusion-Associated Hepatitis took place on 27 September 1982. This Working Party was not established by the DHSS, although it was agreed that a request would be made for a member of the DHSS’s Advisory Group on Hepatitis to nominate a member to attend meetings.[515] Its terms of reference were to promote the investigation of the epidemiology of transfusion-associated hepatitis, to promote research into methods of prevention, and to make recommendations to transfusion directors regarding procedures and screening tests necessary for its prevention. The first meeting decided that the Working Party should collate data which determined the importance of NANBH in the UK and should consider the implications of surrogate markers.[516] The Working Party met on three occasions in 1983[517] and then again in November 1986, having been inactive for some time:[518] its discussions about the undertaking of research relevant to surrogate testing are considered elsewhere in this Report.
The Medical Research Council’s Working Party on AIDS met for the first time in October 1983. Its terms of reference were relatively narrow: to review scientific knowledge and research on AIDS in the UK and abroad; to encourage contact and co-operation between research workers in this field; and to advise the MRC on the current state of knowledge in the field and on topics for research.[519] The minutes of its first meeting include the somewhat opaque sentence “The repercussions of AIDS in respect of blood products received particular comment”.[520] The second meeting in December 1983 included a lengthy discussion with the aim of “identifying important problems which could be usefully tackled in the UK” in terms of research.[521] Following this discussion, a report was prepared setting out possibilities for research: this identified the potential for research involving people with haemophilia.[522] The third meeting in April 1984 discussed contact tracing: “The particular issue of contact tracing of blood donations from AIDS patients was also discussed”.[523] The fourth meeting, on 25 October 1984, revealed knowledge of the seroconversion of patients in Scotland: “there was already evidence from haemophiliacs who had seroconverted that some Scottish factor VIII had been contaminated with HTLV-3.”[524] The source of that information, which was not yet widely known (and, importantly, not yet known by those who had been so infected), is unclear: Dr Richard Tedder was a member of the Working Party and would have been aware of the position, having conducted the tests. There was also a discussion about whether it was unethical to inform patients who were HTLV-3 positive “since no treatment could be offered if AIDS developed subsequently. However haemophiliacs may wish to know so that they can use barrier methods of contraception”.[525]
The CMO’s Annual Report for 1983 referred to the establishment of the MRC’s Working Party on AIDS in October 1983, stating, “The MRC Working Party is the Department’s main source of information concerning European and World Health Organization AIDS research initiatives.”[526]
The CBLA established a Central Committee for Research and Development in Blood Transfusion which met on 21 June 1983. Its membership included Dr Gunson, Professor Bloom, Dr Rizza, Dr Lane and Dr Tedder. It was attended by representatives of the DHSS and SHHD and the MRC. Its role was to advise the CBLA on research and development in blood transfusion and related fields. Discussing AIDS, Dr Gunson, as chair, having “outlined the problems caused by AIDS”, suggested that since AIDS appeared to be transmitted through blood and blood products “then it should be considered by the Committee.” It was agreed that an ad hoc group would be formed to consider the question of the Blood Transfusion Service initiating research and report back at the next meeting.[527]
The first meeting of the Working Group on AIDS in relation to Blood Transfusion took place on 14 October 1983.[528] The Group was described as an ad hoc one set up to consider “the problem of AIDS in relation to the transfusion of blood and blood products.”[529] It was decided at the first meeting that Professor Bloom should be invited to the next meeting, to provide a link with the MRC’s Working Party on AIDS. There was a discussion about the AIDS donor leaflet and agreement that Dr Brian McClelland would submit outline proposals for a prospective study to enable consideration of anti-HBc screening as a form of surrogate testing.[530] The second meeting took place on 27 January 1984, at which the topics under discussion included surrogate testing and the use of small donor pool material. No further meeting date was fixed and it is unclear whether the Group met again.[531]
The ACVSB first met in April 1989.[532] Its terms of reference were “to advise the Health Departments of the UK on measures to ensure the virological safety of blood, whilst maintaining adequate supplies of appropriate quality for both immediate use and for plasma processing”.[533] The expectation was that it would be concerned with “major policy”, rather than detailed implementation, and that other groups with “interests in this field” would bring to the ACVSB any proposals which impacted on the others.[534]
The proposal to establish it followed from an EAGA meeting in June 1988,[535] with Dr Pickles preparing a note for the CMO on 11 July 1988,[536] and Dr Harris, the Deputy CMO, writing to the CMO on 14 July with the proposal for a new advisory group under his chairmanship.[537]
On 2 September 1988 Dr Moore wrote to John Cashman as follows:
“There is growing public awareness, stimulated by the AIDS virus, that many viruses can possibly be transmitted by blood and blood products … From an HS[538] viewpoint the new committee will be invaluable as a source of expert opinion. Over the last 2 years we have had several flaps when ‘new’ viruses have surfaced and policy regarding their testing has needed to be developed on the spot. The new committee should help considerably.”[539]
Meetings took place with the CMO on 6 September and 19 October;[540] there was consultation with Wales, Northern Ireland and Scotland, with the “general agreement of officials in the territorials” having been obtained by 30 September;[541] and a submission then went to ministers on 6 December 1988.[542] The submission – rightly – observed that historically the blood transfusion services had adopted new screening procedures “in an ad-hoc fashion in response to advances in clinical knowledge”, and that concern to maintain the safety of the blood supply had been “heightened by greater public and clinical awareness of the potential for viral contamination and the new developments in product liability legislation.”[543]The approval for a new committee from all UK health ministers had been received by 21 February 1989.[544]
It is surprising, and disappointing, that – the need for such a committee having been identified in June 1988 (a need that should in any event have been identified long before)[545] – it took until April 1989 for it to be in a position to meet. The delay was particularly concerning because the purpose of the group was to provide advice so that the Department of Health could “enable quick reactions to be made to new developments in screening techniques and new epidemiological information.”[546]
Dr Walford rightly said that it would “indubitably” and “obviously” have been a “good thing” to have one overarching body with responsibility for blood safety earlier than there was; she could not recall this being discussed within the DHSS during the time she was involved with blood and blood products (ie from 1976 up to the end of 1983).[547]
Problems were caused by the splintered nature of the structures set up to advise the government (directly, or more usually indirectly) in respect of non-A non-B Hepatitis. Non-A non-B Hepatitis was too often passed over. It was extraordinary that the Advisory Group on Hepatitis was set up in October 1980, less than a month after Dr Walford of the DHSS had described non-A non-B Hepatitis as a form of hepatitis which could “be rapidly fatal … or can lead to progressive liver damage” and could result in a chronic carrier state increasing the pool of non-A non-B Hepatitis in the community,[548] but that the Advisory Group just did not consider non-A non-B Hepatitis at all in any of its meetings, except to mention a paper in 1989 and to mention the date for screening Hepatitis C donations in 1991.
Very little was done before 1991 to address the problems caused by the transmission of non-A non-B Hepatitis.[549] No advice from the main Advisory Group. No decision to undertake surrogate screening except that there should be a study conducted first; and then no funding for a study.[550] No support until the shadow of AIDS began to loom for active research into whether non-A non-B Hepatitis might be inactivated in blood products.[551] No advice to patients as to the risks of non-A non-B Hepatitis.[552] When it came to taking decisions about AIDS, there was a failure to realise that the source which (probably) gave rise to a risk of transmitting AIDS was also a source which (more certainly) gave rise to risks of transmitting non-A non-B Hepatitis. The fact that factor concentrates potentially transmitted both infections at the same time (and thereby not only exposed recipients to all the risks of those infections as separate infections) does not seem to have featured in discussions or advice. There was a real risk arising from this, which was that the combination of non-A non-B Hepatitis and HIV might be all the worse because of the co-infection. This risk actually materialised.[553] The approach taken to non-A non-B Hepatitis thus both weakened the efforts which might otherwise have been made to restrict the use of US-made factor concentrates, and called for research into the effects of co-infection so that patients (and their treating clinicians) might be fully aware of the extent of the risks to which patients with bleeding disorders were being subjected.
Advice in relation to decisions about AIDS from disparate sources was overtaken by the establishment of the EAGA which met for the first time in January 1985. EAGA was formed at the instigation of the CMO, chaired by Dr Abrams (Deputy CMO), and its meetings were attended by representatives of SHHD, the DHSS Northern Ireland, and the Welsh Office.[554] Its purpose was to give advice on all measures required to control the spread of AIDS. As discussed elsewhere in this chapter, it should have been established in 1983. Had it been set up earlier, it is possible that some of the delays and inadequacies in decision-making described in this and other chapters with regards to AIDS would have been avoided. It represented the nearest the UK came to having a single point of reference for expert advice on AIDS as it related to the blood supply until the ACVSB was set up.
Professor Ian Hann (who since his clinical work in Scotland has been concerned with the organisation of blood transfusion services in Ireland), when giving evidence to the Penrose Inquiry, noted that this was a period when they could have done with “a bit less democracy and a bit more guidance”, and that there were many views and many committees but not necessarily many decisions being taken. What was needed, he thought, was “an expert body that comes to the best possible conclusions at the time”: “having a dozen committees doesn’t solve the problem.” In his view, this could only have been co-ordinated by government. The lack of a central government advisory body in 1983 and 1984 indicated that there was a key failure over this important period to recognise the risks. The need was for government, uniquely placed as it was, to rise above the clamour, take informed decisions in the public interest, and take a proactive lead.[555] Professor Hann’s observations have considerable force. Those in government were not well placed to act without the best, reliable, advice, but they were in a position to make sure they had it and did not do so until very late.
There was no single overarching body with responsibility for making recommendations in relation to the virological safety of blood until the establishment of the ACVSB. Had that been established earlier, it is possible that there would have been a central mechanism for decision-making regarding the introduction of surrogate testing and some, at least, of the problems described in the chapter on Surrogate Testing for Hepatitis C would have been avoided.
However, ACVSB did not put an end to the overlapping committees since it was shadowed by a body which advised NBTS, and thus overlapped with much of the discussion being held at ACVSB (though it might be difficult to know, given the secrecy with which ACVSB chose to deliberate): the ACTTI.
This web of committees and groups led to a fragmented and sometimes incoherent system for decision-making, with multiple and to some extent overlapping bodies involved in assessing different aspects and making recommendations on different aspects of risk and risk mitigation. Decision-making on something so fundamental to the health of the nation as blood safety should not have been so “ad hoc”.
The repetition of advice from more than one committee covering the same subject may be reassuring to those who are looking for a reliable star to steer by. However, one of the principal concerns of having so many different bodies, all reporting directly or – more usually – indirectly to government is that both haemophilia care, the blood products fractionation plants, and the blood transfusion service had only a relatively small cohort of leading experts. Some names – for instance that of Professor Bloom – tended to appear on the membership of different bodies. Thus the same voice was being echoed in different sources. Instead of cultivating assurance about the course to steer, this made it difficult to realise that it was essentially the same, one, voice (so far as blood products were concerned), and to look (especially if a minister) to see what if any other views there were which should also be listened to.
The Northern Ireland Department of Health and Social Services (“DHSSNI”) played a very limited role in decision-making regarding blood safety in the 1970s and 1980s. This was in part due to the fact that direct rule from Westminster was introduced in March 1972 following the suspension of devolved government. Thereafter, and until 1998, the mechanism of this governance was by way of a Secretary of State for Northern Ireland, the Northern Ireland Office and a number of junior ministers.[556] The actual delivery of health and social services was, from 1973, by four health boards: the Eastern, Northern, Southern and Western boards.[557]
The role of Secretary of State for Northern Ireland was filled by Merlyn Rees from 1974 to 1976, Roy Mason from 1976 to 1979, Humphrey Atkins from 1979 to 1981, Jim Prior from September 1981 to September 1984, Douglas Hurd from September 1984 to September 1985, and Tom King from September 1985 to July 1989. Junior ministers within the Northern Ireland Office included John Patten from January 1981 to June 1983 and Chris Patten from June 1983 to September 1985. Northern Ireland had its own Chief Medical Officer: Dr Thomas Terence Baird (1973 to 1978); Dr Robert Weir (1978 to 1988); and Dr James McKenna (1988 to 1995).[558]
Although few of those involved at the time in government in Northern Ireland who survive have any direct recollection of decision-making regarding blood and blood products, and there is comparatively little contemporaneous documentation available, it is clear that overall the DHSSNI followed the policy decisions made by the DHSS in London and that the DHSSNI had little observable influence on those decisions. Two particular factors contributed to that state of affairs. The first was that in reality security and political aspects “took up a significant amount of ministerial time”.[559] The second was that the responsibilities of the relatively small number of medical and administrative civil servants in Northern Ireland covered a broad range of matters, with less expertise and (in reality) less time devoted to matters of blood and blood products.[560]
Thus, Lord David Owen’s evidence (in relation to his time as Minister for Health at the DHSS between 1974 and 1976) was that “the Secretary of State for Northern Ireland would take decisions but be hugely influenced by -- they would tend never to go against the grain of decisions that were taken in England.”[561] When he was Parliamentary Under-Secretary of State in the Northern Ireland Office, Lord John Patten’s recollection was: “the liaison with DHSS on health issues was done by officials rather than at Ministerial level.” Indeed he could not recall any meetings with junior health ministers in the DHSS or in the Scottish and Welsh Offices.[562] Likewise when he moved to the DHSS, he could recall little contact with junior ministers in Northern Ireland (or Scotland or Wales).[563] Lord Fowler, as Secretary of State for Health and Social Services between 1981 and 1987, recalled that Northern Ireland closely followed the DHSS.[564]
Dr Morris McClelland, who was the director of the Northern Ireland Blood Transfusion Centre, described the relationship between the DHSSNI and the DHSS as one where: “policies adopted by DHSSNI typically followed those of DoH (London) since NI was under direct rule from London.”[565]
Civil servants from Northern Ireland would be invited to attend some, at least, of the committees and working parties which reported to the DHSS, although the recollection of Dr Pickles (a principal medical officer in the DHSS from 1986 to 1991) was that this could sometimes be as a “regretful late thought”.[566]
Dr Robert McQuiston, the Assistant Secretary in the Health Services Division of the DHSSNI from 1984 to 1998, thought that “On health policy generally, DHSS had an overall coordinating role on issues impacting on the whole of the UK while DHSS (NI) would tailor its approach to take account of particular considerations relevant to Northern Ireland. On other matters, such as prevention of coronary heart disease, DHSS (NI) took its own initiatives, reflecting a higher local priority.”[567]
Examples of the (limited extent of) involvement of Northern Ireland officials include: a December 1980 meeting between the DHSS, SHHD, DHSSNI and Welsh Office to discuss UK self-sufficiency in blood and blood products, attended by Dr J D Acton on behalf of DHSSNI and with express consideration of Northern Ireland’s needs for domestically produced concentrate, following which Dr Acton agreed to discuss with his Department the logistics of sending plasma to Edinburgh;[568] the DHSSNI’s acceptance of the recommendations of the first and second reports of the Maycock Group, followed by the issuing of circulars to the relevant health boards in Northern Ireland in 1973 and 1977;[569]the invitation to Dr Logan of the DHSSNI to attend (as observer rather than member, along with departmental officers from the DHSS and other departments) the meetings of the Advisory Group on Hepatitis in 1980;[570] and attendance of DHSSNI officials as observers at the meetings of the ACVSB.[571]
There appears to have been little or no involvement from Northern Ireland in decision-making on AIDS in the first half of the 1980s. By way of example, the 3 May 1983 letter on the Government’s “line to take” over AIDS had a relatively wide distribution list, including the SHHD and Welsh Office but not Northern Ireland.[572] On the issue of screening of blood for HIV, the DHSSNI followed the approach decided in Westminster.[573] Richard Needham, Parliamentary Private Secretary[574] to Jim Prior, the Secretary of State for Northern Ireland, from 1983 to 1984 (and thus at a key time in relation to AIDS), had a recollection of some discussion on how to handle the treatment of AIDS sufferers and the need to make those vulnerable to risk aware of the dangers of contracting AIDS,[575] but had no recollection of any policy matters relating to blood or blood products ever being raised with him at the time. He suspected that officials in Northern Ireland “would have had little influence when such matters on blood or blood products did arise.”[576] Northern Ireland “essentially mirrored health policy from Great Britain”and he was “certain that most health policies of the Department would have been followed in Northern Ireland, making the relationship one of mirrored subservience. However, the presentation of the policy may have been tailored appropriately to meet the social or cultural norms of the local communities in Northern Ireland.”[577]
The role played by the Welsh Office was, on occasions, a little more active than the Northern Ireland Office, but with Wales still following the lead of the DHSS on matters of health policy regarding blood and blood products.
The role of Secretary of State for Wales was filled by John Morris from 1974 to 1979, Nicholas Edwards from 1979 to 1987, Peter Walker from 1987 to 1990 and David Hunt from 1990 to 1993. Barry Jones was Parliamentary Under-Secretary of State from 1974 to 1979. The first CMO for Wales was Dr Richard Bevan from 1969 to 1977; the post was then held by Dr (later Professor) Gareth Crompton from 1978 to 1989, and Dame Deirdre Hine from 1990 to 1997.
Lord Fowler’s recollection was that the responsibility for healthcare in Wales rested with the Secretary of State for Wales (and that responsibility for Northern Ireland and Scotland rested similarly with the respective “Secretaries of State of the ‘Territorial Departments’.”)However, he pointed out that the three Secretaries of State were Cabinet members in their own right, that they were all ministers in the same Government and as such, had the usual collective responsibility for all government policies. He recalled in practice that “on health issues generally … Scotland tended to be the most independent, whereas Wales and Northern Ireland more closely followed the DHSS.”[578]Lord Fowler remembered interacting with Nicholas Edwards, who would talk to him fairly frequently on health issues.[579]
Barry Jones (now Lord Jones) recalled meetings with the Welsh CMO and his understanding was that it was part of the CMO’s responsibility to issue guidance and advice to clinicians, patients and the public.[580]
As with the DHSSNI, the Welsh Office was significantly smaller than the DHSS and the medical officers responsible for health would have had a much wider role than in the DHSS, which had someone with specific responsibility for blood and blood products.[581]
As with Northern Ireland, civil servants would be invited to attend some, at least, of the committees and working parties which reported to the DHSS.[582] A Welsh Office representative, for example, was invited to attend the meetings of the Advisory Group on Hepatitis, the Working Group on AIDS of the Advisory Committee on the NBTS[583] and the ACVSB (whose establishment the Welsh Office was asked to, and did, agree to).
A letter sent in January 1990 during the HIV haemophilia litigation indicates that there was no independent Welsh Office action concerning the risk of hepatitis from blood and blood products, although it was recognised as a hazard.[584]
Within correspondence that related to the HIV litigation, the Welsh Office described relying on the DHSS to “take the principal lead in determining national policy on matters relating to HIV/AIDS prevention”but that it“contributes to the formulation of policy through membership of Inter-Departmental bodies and their sub-groups … and reserves the right to adapt policies to the local circumstances in Wales.”[585] The Welsh Office also gave advice and information by issuing circulars within Wales “corresponding to those issued by the Department of Health in England.” Examples included the AIDS donor leaflets in September 1983/February 1985 and a CMO letter regarding AIDS in 1986. However, the Welsh Office also issued advice and took action “on its own account”, such as issuing PSM (84)4 in November 1984 asking doctors to inform CDSC of cases of AIDS or Kaposi’s sarcoma;[586] forming an AIDS steering group in September 1985; and issuing a recommendation in December 1985 to all Welsh district health authorities to set up AIDS co-ordinating teams.[587]
There were some discussions within the Welsh Office regarding AIDS, independent of the decision-making being undertaken by the DHSS in the period 1983 to 1984 regarding AIDS. On 3 May 1983, for example, at the same time as Number 10 was being given what was probably its first briefing on AIDS by the DHSS,[588] Dr David Ferguson-Lewis, senior medical officer at the Welsh Office, wrote to the Parliamentary Under-Secretary of State following press reports implicating US blood products in cases of AIDS; those reports included, of course, a report of a person with haemophilia being treated at the University Hospital of Wales. The minute noted that Dr Tony Napier, director of the transfusion centre in Cardiff, had made a statement that had been published in the Western Mail,[589]where it was said that Dr Napier had stressed that “no link between AIDS and blood transfusions have been established … the mechanism of transmission of disease is not yet understood and all present evidence is circumstantial.”Dr Ferguson-Lewis continued by informing the minister “that the Medical Services Health Professional Group are further investigating the local situation and are in contact with DHSS colleagues nationally.”[590]
The following day, 4 May 1983, a meeting was convened by the Welsh Office to discuss the Cardiff patient. It was attended by Dr Crompton, the CMO, along with a number of medical officers, Dr Napier, Professor Bloom, Dr Michael McEvoy (CDSC) and Dr John Skone, chief administrative medical officer of South Glamorgan Health Authority.[591] Kevin Slater’s medical history and clinical condition was discussed in some detail and the assessment was that he presented “a clinical picture which fits within the case definition as set by the CDSC”.There was a discussion of the statement Professor Bloom had made to the Haemophilia Society on 23 April, when he said there was no definite case of AIDS amongst people with haemophilia in the UK. It was asserted that he had spoken from “a typed manuscript”, but that in the discussion that followed he “admitted that a case had been treated in Cardiff which showed some of the features of a mild possible AIDS.” Two journalists – Susan Douglas and a reporter from the South Wales Argus – had made contact with Professor Bloom but he made no comment; the meeting minutes record that he had “provided all relevant information as a precautionary measure to the Medical Protection Society.”[592]
The meeting then considered the impact of publicity on the blood transfusion service in Wales, noting that “it was important to keep the problem in perspective” and that “Given that the reported incidence of AIDS in the UK is very low we might be confident that we are not collecting potentially contaminated blood.” The fact that the current reported incidence (which the meeting recognised probably reflected an underestimate of the problem) was very low was not, of course, a reliable guide.
Consideration was then given to a ban on Factor 8 from the US: this would, it was said, necessitate a reduction in patients treated and the modification of the facility for home treatment.[593] The conclusion (a foreshadow of the decision that would be reached in July 1983 by the CSM(B) – perhaps unsurprisingly given Professor Bloom’s participation in both meetings) was that “There is no justification on the basis of facts so far established to ban the importation of factor 8 though it was thought preferable in the case of children to restrict treatment to the BPL concentrate produced in Britain.”[594]
On the same day Dr Ferguson-Lewis wrote to the Parliamentary Under-Secretary of State notifying him that the patient at the Cardiff Haemophilia Centre did meet the CDSC definition of AIDS but there was “no cause for precipitate action.”[595]
There were further meetings within the Welsh Office in late 1984. On 19 November a meeting was called by the CMO, Dr Crompton, in light of the “considerable media coverage” given to the death of three babies in Australia following transfusion, and to the report of the death of a Newcastle patient with haemophilia from AIDS. The CMO’s intention in calling the meeting was “to establish the known facts as they affected the UK in general and Wales in the particular.”[596] Reference was made to the donor whose donations had been used for whole blood transfusion and for the production of concentrate, some of which had “found its way to Wales”.[597] Consideration was given to the question of donor awareness: although the existing leaflet was said to be liberally distributed at every donor session “it was still thought unsafe to rely upon this as the sole means of weeding out the homosexual population from amongst potential blood donors” and “the matter of a more detailed questionnaire could usefully be pursued.”[598]
On the same date a briefing was provided to the Parliamentary Under-Secretary of State, copied to the Secretary of State and CMO,[599] to bring ministers up to date with the position in South Wales, which was that there had been three cases of AIDS in South Wales to date: two were dead; the third was a person with haemophilia. The briefing stated that there were at present “a very few haemophiliac patients in South Wales,” but that it was “likely that some may have received treatment with Factor 8 which might have been contaminated.”[600]The number at risk was estimated in single figures. Risks to patients from the use of whole blood were said to be negligible, with “no evidence” that any patient has contracted the disease in the UK from this source.[601] There was said to be little the Welsh Office could do to immediately affect the present situation. On 20 November Dr Galbraith of CDSC wrote to Dr Crompton with an update about two important events: the first related to the Wessex donor, the other to a nurse who had seroconverted to HTLV-3 following a needlestick injury.[602] It is of note that none of these communications referred to events in Scotland, and to the fact that it was by now known that a number of patients treated at the Edinburgh Haemophilia Centre had tested positive for HIV.
Scotland had a large degree of independence in matters of health policy and administration at all times relevant to the Inquiry. Over the whole of the period with which the Inquiry is concerned, Scotland had its own, separate health and transfusion services. Health was a matter which was either part of the administrative devolution arrangements (and was hence within the exclusive competence of the Scottish Office) or part of the more formal devolution settlement after the Scotland Act 1998. Responsibility for decision-making and policy in Scotland was vested in a number of entities which were distinctly Scottish, reflecting these facts. Scotland had its own legislation governing health matters.
The fact that Scotland had its own independent National Health Service and own blood transfusion service (SNBTS) meant that it also had its own transfusion directors and haemophilia directors who met as separate groups or together, often along with representatives of government in Scotland to develop blood collection, screening, transfusion and associated treatment policies. It also had its own fractionation facility at the PFC at Liberton, with products made there also used in Northern Ireland and (in times of excess supply) in other parts of the UK.[603]
At government level, the Scottish Home and Health Department (“SHHD”) within the Scottish Office and then, post-1999, the devolved Scottish Executive, had responsibility for health policy and administration.
However, it must be borne in mind that these arrangements and responsibilities for the administration of matters relating to health in Scotland also occurred within a UK context. The apparent freedom and autonomy of the administrative arrangements relating to health thus have to be seen within that context. Several UK bodies had considerable influence over Scottish policy, though they considered matters on a UK-wide basis rather than specifically with Scottish patients in mind. These included the UKHCDO, the DHSS and the MRC as well as advisory bodies and working groups which had a UK-wide bearing.
The constitutional arrangements in place in the 1970s and 1980s were such that “vast swathes of matter relating to Scotland were handled by the Scottish Office as part of ‘administrative devolution’”, with responsibility for all of them being thinly spread amongst a small handful of ministers. The result was that there was little time for ministerial engagement in matters such as the safety of blood or blood products, which had rather to be handled by civil servants, who rested too much on the assumption that blood supply was safe because of the voluntary donor system.[604]
The Scottish Office was headed by the Secretary of State for Scotland (a member of the UK Cabinet). This was a role filled by Willie Ross from 1974 to 1976, Bruce Millan from 1976 to 1979, George Younger from 1979 to 1986, and Malcolm Rifkind from 1986 to 1990. Junior ministers with responsibilities for health in the 1980s included John Mackay from 1982 to 1986, Lord Glenarthur from 1986 to 1987 and Michael Forsyth (now Lord Forsyth) from 1987 to 1990.[605]
The Chief Medical Officer was Sir John Reid from 1977 to 1985, Dr Iain Macdonald from 1985 to 1988 and Professor Kenneth Calman from 1989 to 1991.
Lord Fowler’s recollection was that whilst the DHSS was so big that anything it did tended to be followed in Wales and Northern Ireland, Scotland remained “determinedly independent” on some things.[606] Lord Forsyth, however, described the SHHD’s resources as limited compared to the DHSS’s.[607]
The Scottish Office was made up of a number of constituent departments, including the SHHD which was responsible for home affairs and the health service. It was subdivided into a number of groups, of which Group IV was responsible for the management of the health service,[608] and like the DHSS the civil service comprised an administrative and medical hierarchy. Medical officers involved in decision-making regarding blood and blood products included Dr Iain Macdonald and Dr Graham Scott, both serving as DCMOs, Dr Archibald McIntyre, who was a principal medical officer from 1977 to 1993, overseeing the Scottish National Blood Transfusion Service, and Dr Albert Bell who was the senior medical officer responsible for blood services until 1985, having been in the position since at least 1973.
Advisory committees tended to be administered by the DHSS in Westminster, with Scottish interests being represented by relevant Scottish experts and Scottish civil servants including medical advisers who attended as observers and reported back to SHHD.[609]
SHHD medical officers regularly attended SNBTS meetings and sought the advice of its consultant adviser, Dr John Cash. The SHHD’s involvement in various meetings and direct correspondence with the DHSS included SHHD officials observing meetings of regional transfusion directors in England and Wales[610] and participating in meetings of groups such as the Central Blood Laboratories Authority.
Duncan Macniven, who was Assistant Secretary in the SHHD between 1986 and 1990, explained that most decisions within the SHHD were taken by officials without always consulting the (limited number of) ministers. Only difficult or politically contentious issues were typically brought before ministers.[611] The criteria for referring matters to ministers were not fixed but relied on the judgement of the responsible officials, typically at or above the level of Assistant Secretary, and if necessary, in consultation with more senior officials.[612] Lord Forsyth described the role of officials as administering agreed policies and ensuring that ministers were alerted to any concerning issues. He expected significant matters that required ministerial decision-making to be “drawn to their attention.”[613]
Dr Scott, in evidence to the Penrose Inquiry, described regular liaison with the DHSS at various levels, including attending policy meetings of the DHSS’s Chief Medical Officer and maintaining ongoing communication.[614] However, he recognised that the SHHD did not automatically adopt DHSS policies and, as an example, confirmed that it would have been possible for Scotland to introduce HIV screening ahead of England, with the agreement of Scottish ministers. Duncan Macniven emphasised that health services in Scotland were entirely devolved to the Secretary of State and the SHHD, without any oversight role from the DHSS.[615] He noted that while significant disputes between the departments were rare, any that arose would be resolved through senior-level discussions or ministerial contact. Duncan Macniven spoke of “a great deal of executive devolution to the Scottish Office”prior to the creation of the Scottish Parliament.[616] In an October 1981 minute, Dr Bell emphasised that neither the SHHD nor SNBTS could be committed by policies adopted by the DHSS, suggesting a readiness to follow a uniform UK policy but acknowledging the unpredictability and controversy in the field of blood transfusion.[617]
Though it is reasonable to suppose that similar sources of knowledge about AIDS to those available to the DHSS in London were also available to the SHHD in Scotland, and that those closely involved in policy relating to blood supply and blood products would in general terms be aware of reports in the media about AIDS in America and its possible causes before the end of 1982, there is no documentation which specifically confirms this. The first recorded discussion concerning AIDS which included officials from the SHHD occurred at a meeting held between SNBTS and Scottish haemophilia centre directors on 21 January 1983 chaired by Dr Bell.[618] Before the meeting Dr Cash circulated a briefing paper relating to AIDS.[619] In the meeting he additionally drew attention to recent articles in The Observer[620]and The Lancet[621] and circulated an extract from the December edition of the Morbidity and Mortality Weekly Report (“MMWR”) with his paper.[622] Dr Christopher Ludlam informed members that the UK haemophilia directors had been sent a letter and questionnaire regarding the reporting of possible cases of AIDS.[623] Despite the material provided to the meeting, the minutes do not record that any action to minimise the risks in Scotland of AIDS was to be taken by SHHD (or anyone else).
On 1 May 1983, the Mail on Sunday carried its“Hospitals using Killer Blood” headline to draw attention to the risk of blood transmitting the cause of AIDS. This led to a response from John Parker of the DHSS in London to the private office of the minister (then Geoffrey Finsberg), enclosing a “line to take” and background briefing on AIDS, which had been prepared for the Prime Minister.[624] The response was copied to John Davies, Assistant Secretary at the SHHD.[625]
At this time, the SHHD was also receiving information from international sources. On 5 May 1983, Dr Archibald Prentice forwarded a telex from the WHO to Dr Scott and Dr McIntyre.[626] The telex recorded that a meeting on AIDS would be held in Denmark in November and that as of 1 May 1983 over 120 cases of AIDS had been reported by European countries that were part of the voluntary notification scheme.[627]
In receipt of this information, Dr McIntyre wrote to John Davies on 6 May 1983. He commented on the background briefing provided by the DHSS which he stated “reflects the situation in England and Wales” and that, while some Scottish transfusion directors had been in touch with Dr Gunson, there had not been any formal discussions with regional transfusion directors in England and Wales, contrary to the suggestion in the DHSS’s note. Dr McIntyre recorded that no “proven case” had been notified to date in Scotland and that Dr Prentice was “in close contact with the Communicable Disease (Scotland) Unit at Ruchill to which any case of AIDS arising in Scotland would be notified.”He commented that the signs and symptoms of AIDS were “somewhat vague” and that, as no “specific diagnostic test is available”, it was important that the same diagnostic criteria was being applied. He reminded John Davies that nearly all blood products including Factor 8 used in Scotland were produced at the PFC from blood voluntarily donated within Scotland, although there were a few patients currently being treated with imported Factor 8. He added that the SNBTS directors were very aware of the problem “and have it under constant consideration”, with current thought being given both to the production of a leaflet about AIDS for donors and to avoiding collection in high risk locations such as prisons or where there was known to be a high proportion of homosexuals or drug abusers in the population.[628] In fact, as discussed earlier in this chapter, collection from prisons continued.
Dr McIntyre’s observation was that the situation “does not warrant action until the risks have been more fully evaluated.”[629]
John Davies prepared a ministerial submission for John Mackay on the same date, echoing, and confirming officials’ agreement with the general line in the DHSS’s briefing but incorporating specific Scottish points. These points highlighted Scotland’s near self-sufficiency in Factor 8 and the limited use of imported concentrates. John Davies also outlined the absence of confirmed AIDS cases in Scotland and detailed the matters to which SNBTS was currently giving consideration, as set out in Dr McIntyre’s note.[630]
No specific steps to be taken by the SHHD were identified, nor was the Minister asked to make any decision or take any action.
There is no reason to suppose that decision-makers in Scotland did not know of the risk of AIDS at broadly the same time as did the DHSS in Westminster. The national and mainstream scientific press had speculated that the cause of AIDS might be blood-borne since November 1982.[631] From 21 January 1983 however there is no doubt about their knowledge of a real risk, and ample material to suggest that though cases of manifest infection had not yet been reported in the UK, it was known how quickly it was spreading in the US.[632] It was thus unlikely to be long before blood donors in Scotland, and thus transfused patients, and people with bleeding disorders would become victim to it, unless effective precautions were taken. Despite this, thought was being taken[633] about when they were required. It may have been understandable that Dr McIntyre should think that the situation did “not warrant action until the risks have been more fully evaluated.”[634] He was not alone in needing to know much more than he did about AIDS and its causes. However, the pursuit of full knowledge about a new infection will almost never be completely satisfied, while that infection is in the process of taking hold. Certainty is desirable – but a primary rule in public health is that where there is sufficient information to show that there is a real risk, protective measures must be taken on the basis of the best information then available. It is an understandable, but crucial, mistake to wait for better or further information. It may never come. If the nearby volcano is rumbling in a way it has not done before, it is a mistake to wait until the threatened eruption is underway, and the lava is flowing too fast to escape it. If it turns out, on receipt of further information, to have been a false alarm then no life will have been lost, and comfort may be taken in knowing that the right measures have been taken, and will be taken again when and if necessary.
Dr McIntyre’s attitude thus led to inaction here. Just as in the case of the DHSS in London, the reaction of the SHHD was to do too little, and to do it too late.
As described above, Dr Brian McClelland from the South East Scotland Regional Transfusion Centre initiated work on an AIDS donor leaflet without SHHD involvement (Dr Brian McClelland told Dr Bell that he was going to produce a leaflet, without seeking approval or permission).[635] On 24 May 1983, at a meeting of the SNBTS Co-ordinating Group, which the SHHD did not attend, Dr Brian McClelland presented a draft AIDS leaflet. The South East Scotland RTC subsequently issued this leaflet in June 1983. It highlighted the potential infectious nature of AIDS, suggesting that the disease, thought to be caused by a virus, could be transmitted through blood products like Factor 8, as observed in a few cases in the US.[636]
The topic of AIDS and donor selection leaflets was further discussed at a SNBTS directors’ meeting on 14 June 1983. Attendees included Dr Bell and John Wastle from the SHHD, as well as Dr Gunson and Dr Wagstaff from England. The meeting involved discussions about the approaches taken in England and Wales and the policies of the American Red Cross and the Council of Europe regarding AIDS. The directors further noted that “the DHSS were closely involved in England and Wales and recommended that the SHHD should have a similar involvement in Scotland. There would also be a need for a Government Press Officer to handle enquiries.”[637]
The following day, Dr Bell summarised these discussions and developments in a communication to Dr McIntyre and John Wastle. Dr Bell highlighted the complexity of addressing AIDS in donor centres, including deciding whether the leaflet should be for pick-up or hand-out, and the possibility of needing different leaflets for the general public and specifically for the homosexual community. He commented that there was “no doubt about the desire in the transfusion services to collaborate fully north and south of the Border”, noting that “Dr Gunson has promised to let SNBTS have his latest version ... He will also try to ensure that DHSS consult SHHD in good time before there is ministerial involvement in going public on this subject.” He also noted the increasing public and ministerial attention on AIDS.[638]
In June 1983, the SHHD became aware that the Edinburgh and South East Scotland’s leaflet had started to be circulated with Dr Bell commenting that it “looks as though, de facto, we are about to reach a situation in which there will be two slightly different leaflets.”[639]
Although comfort had initially been drawn from what was seen as an absence of AIDS cases in Scotland, by mid 1983 the press in Scotland began reporting AIDS cases. An article in the July/August 1983 edition of Gay Scotland mentioned two suspected cases in Edinburgh and Tayside, reported a consultant at the Edinburgh Royal Infirmary confirming that “It is only a matter of time before more AIDS cases are confirmed in Edinburgh and Glasgow”, and referred to the leaflet in use by the South East Scotland Blood Transfusion Service.[640]
On 30 June 1983, Dr Anne Smith (the donor consultant at the Edinburgh and South East Scotland Centre) issued internal guidelines for the handling of blood and blood products. This document contained information for, and instructions to, staff on the handling of donors. The note stated that people in high risk groups were asked to refrain from volunteering to give blood but that no blood donor was to be turned away merely on suspicion of being in a high risk group. A policy and procedures for handling those who nevertheless presented was set out.[641]
SHHD officials liaised with their DHSS counterparts over the development of an AIDS donor leaflet in late June and early July 1983. In a handwritten file note, an SHHD official recorded a conversation with Paul Winstanley of the DHSS on 20 June 1983. Paul Winstanley was said to have “confirmed that a revised leaflet – based on Dr McClelland’s – was being prepared. He agreed to let me have copies of the final draft and to keep me in touch with developments, especially on the timing of submission to Ministers.” Dr Bell was said to have had a similar conversation with Dr Walford.[642] In a further note, the official recorded a second conversation with Paul Winstanley on 28 June 1983. His note recorded that Paul Winstanley has said“that progress on preparing a draft leaflet and a draft submission to Ministers was slow, but [he] was well aware of the need to consult SHHD on the leaflet and give adequate warning on the timing of an approval to Ministers.”[643]
On 1 July 1983 a DHSS submission on the publication of an AIDS leaflet was submitted to ministers, with a copy being sent to John Wastle at the SHHD.[644] The submission, prepared by Dr Walford, stated that “Although there is no conclusive evidence, it seems very likely that AIDS is caused by an as yet unidentified virus.”[645] A draft leaflet, dated 24 June 1983, stated that AIDS could “Almost certainly”be transmitted through blood and blood products.[646] Further DHSS internal correspondence was copied to the SHHD, including a 4 July 1983 minute from John Parker confirming that Lord Glenarthur was content with the proposed leaflet.[647]
A 6 July 1983 handwritten note to Dr Bell described a conversation with Steve Green of the DHSS. This recorded that the DHSS “Ministers had mixed reactions and it required a meeting attended by Mr Parker this morning to secure agreement from Ministers who nevertheless wish the terms of the leaflet to be toned down.” DHSS ministers had also asked for a statement to be used when publishing the leaflet to “put the matter in perspective” and to “allay any impression of over-reaction”.[648]
Dr Bell provided Dr Scott with a copy of the DHSS ministerial submission. Dr Bell explained that the submission and proposed leaflet were in line with what had been “tentatively agreed by the English and Scottish RTDs”, although the section requesting high-risk donors not to give blood differed from Dr Gunson’s version, which was based on Dr Brian McClelland’s. The SHHD had been “informed that Mr Fowler’s first reaction” was that “the terms of this leaflet are strong, and that DHSS may therefore be making further amendments.” Dr Cash, however, was in favour of a single UK leaflet, a view shared by Dr Bell.[649]
On 11 July 1983 John Davies briefed the Minister, John Mackay, on the UK AIDS leaflet. He attached the draft leaflet, noting that DHSS ministers had expressed reservations over it and that DHSS officials were “toning down the text somewhat, largely to make clear that, even in the US, only a small number of cases has been reported.”[650] John Davies explained that publication and distribution of a donor leaflet would conform with a draft resolution prepared by the Council of Europe’s Committee of Experts on Blood Transfusion. John Mackay was informed that the SHHD considered that the leaflet should be issued on a UK-wide basis, and that officials were arranging for the text to be adjusted accordingly. John Davies advised that “No separate Scottish announcement would be called for, but an important point for any press inquiries is that Scotland is virtually self sufficient in Factor VIII.”[651]
Alongside the SHHD’s consideration of these issues, it received updates from SNBTS. In a 19 July 1983 letter to Dr Brian McClelland, copied to Dr Bell, Dr Cash enclosed a draft leaflet he had received (presumably from NBTS). He proposed that the SNBTS Co-ordinating Group meeting on 30 August 1983 be updated on the position with regard to a UK leaflet and agree on a method of distribution to donors.[652]
Further updates from the DHSS included a submission dated 29 July 1983, seeking ministers’ approval for the printing and distribution of the proposed AIDS leaflet, a copy of which was sent to John Davies.[653] John Wastle recorded a conversation with Paul Winstanley, confirming the minister’s agreement on the leaflet’s content and the intention to proceed with printing. Paul Winstanley committed to providing 200,000 leaflets for Scotland and updating John Wastle on the timing of the ministerial statement and press release. However, when the DHSS papers arrived on 3 August 1983, it was noted that amendments agreed between John Davies and John Parker had been overlooked. Nonetheless Paul Winstanley was “not inclined to withdraw the leaflet for amendment.”[654]
Dr Cash, in a letter to Dr Brian McClelland on 19 August 1983, mentioned the upcoming statement on AIDS by the English minister and the decision to leave the distribution of leaflets to the discretion of individual RTDs. The Scottish minister was to follow the same approach, with the Scottish Office Information Division issuing a press release based on the English minister’s statement.[655]
Finally, on September 1, 1983, the SHHD issued a press release on the UK AIDS donor leaflet. It stated that there were no confirmed cases of AIDS in Scotland and that “The Scottish Home and Health Department emphasised today that there is no conclusive proof that the disease can be transmitted in blood or in blood products.”The press release highlighted Scotland’s self-sufficiency in whole blood and blood products, with most Factor 8 used for haemophilia treatment being produced from plasma donated to SNBTS by Scottish donors.[656]
The SHHD appears to have been content to sit back and let the DHSS take the lead in respect of decision-making on the AIDS leaflet. Dr Brian McClelland in SNBTS stands out above this. He took the initiative, and was not prepared to wait for Westminster. However, whilst Dr Brian McClelland’s leaflet was circulating in the Edinburgh and South East Transfusion Centre, leaflets were not in universal use in Scotland. The SHHD (in contrast to Dr Brian McClelland) neither sought to urge more decisive and speedier action, nor, when it became apparent that there was delay with the DHSS process, to ensure the issue of its own leaflet, nor to argue for the safest method of distribution (namely the direct provision of the leaflet to all donors).
The decision of the SHHD to adopt and use the “no conclusive proof” line to take was wrong, for the very reasons discussed above in relation to the DHSS. Dr Brian McClelland told the Inquiry that the wording in the press release was quite inconsistent with his own view of the risks and that he thought the wording was “misleading and falsely reassuring”: “by this time, you know, frankly, there was really little shadow of doubt that this was a disease transmissible by blood or in blood products. It is just misleading.”[657] He was right.
In late 1983 and early 1984, officials from the SHHD primarily focused on monitoring developments related to AIDS and blood products. Thus, for example, in his note from the 17 October 1983 meeting of the Advisory Committee on the NBTS, Dr Bell reported a suggestion about concentrating on “small pools of donors”, meaning more intensive plasmapheresis of donors whose health status could be closely monitored.[658] The minutes of this meeting also included an update from Dr Walford on AIDS, highlighting that out of the 24 reported AIDS cases in the UK, two were people with haemophilia, with one deceased.[659] At a meeting on 18 October 1983 of the Advisory Group on Hepatitis, which included Dr Prentice representing the SHHD, Dr Craske reported a doubling of AIDS cases every six months in the US, but emphasised the still very low risk of contracting the disease.[660] An article in The Scotsman on 31 October 1983 noted a 50% increase in British AIDS cases in September, from 16 to 24. This report, which was placed in an SHHD file for John Davies, Dr McIntyre, and Dr Bell, mentioned the death of a patient with haemophilia due to a contaminated blood-clotting agent from an AIDS-infected American donor. A manuscript note beside this report suggested that the SHHD was already aware of this.[661]
Dr Bell participated in the 14 November 1983 meeting of the (Scottish) Haemophilia and Blood Transfusion Working Group, where trials of heat-treated PFC Factor 8 were discussed. The meeting also sought feedback on the effectiveness of the leaflet prepared by SNBTS and the DHSS. The general consensus was that the leaflet had not been particularly useful, despite its wide distribution at donor sessions and other locations, including sexual health clinics.[662]
At the 7 November 1983 meeting of the CBLA Central Committee for Research and Development, Dr Bell mentioned discussions about the AIDS leaflet, with some doubts about its effectiveness and plans by Dr Gunson and Dr Walford to consider revisions. Dr Bell expressed confidence in Scottish interests being represented in these discussions, with Dr Brian McClelland on the AIDS Working Group. Additionally, the meeting discussed surrogate screening for AIDS, centring on anti-HBc testing, and “small pool apheresis” was suggested as a potential strategy within transfusion practice to combat AIDS.[663]
At a meeting of the SNBTS directors on 8 December 1983, attended by Dr Bell and Mr Murray, it was decided to adopt a more proactive approach to the distribution of AIDS leaflets, which had been available at donor sessions for some time. The attendees agreed that each blood donor should receive a copy of the leaflet and that the health questionnaire for donors should include a question about their understanding of the leaflet. Dr Brian McClelland was tasked with producing a revised version of the leaflet.[664] The 2 February 1984 meeting of SNBTS and haemophilia directors, chaired by Dr Bell and attended by Dr McIntyre, again discussed the risk of AIDS transmission through blood and the effectiveness of the current leaflet, with a consensus that modifications might be necessary.[665]
The need to strengthen the message, and the realisation that the effectiveness of the leaflet could be of critical importance, was underlined by the first death of an AIDS patient in Scotland which was reported in the Daily Record on 17 February 1984.[666] The risk was plain that donations might be infected in Scotland despite being provided by volunteers.
The AIDS donor leaflet was again a topic of discussion at a SNBTS directors meeting on 13 March 1984, attended by Dr Bell and Mr Murray. A draft revised leaflet by Dr Brian McClelland was circulated, with directors asked to comment within two weeks. It was reported that Dr Alison Smithies of the DHSS would undertake a similar revision for England and Wales. The Scottish directors believed their approach of making the leaflet available at donor sessions and STD clinics should be strengthened by mailing it to all blood donors.[667]
In March 1984, a local leaflet appealing for blood donors in Edinburgh contained a paragraph on AIDS, which was marked in a manuscript note by John Davies as being more assertive than previously seen.[668]
The trial of the DHSS version of a donor leaflet had been agreed by ministers to run until December 1983. As explained above in relation to the DHSS, some mistakenly thought it was to last for three months longer. At the 10 April 1984 meeting of the Advisory Committee on the NBTS, which Dr Bell attended, the committee discussed amending the DHSS/UK leaflet. Dr Smithies presented an update on the AIDS cases and deaths reported to the CDSC and said that the “6 month trial”[669] of the AIDS leaflet had concluded.[670] In response, the DHSS planned to prepare a revised version for ministerial submission. The committee debated whether a more assertive approach was necessary to discourage high-risk donors and ultimately recommended that the DHSS ministers consider issuing the revised leaflet with donor call-up cards in all regions. Dr Bell noted in his record of the meeting that Dr Smithies had set out the arrangements for revising the leaflet, incorporating suggestions from SNBTS.[671]
Subsequent to these discussions, a revised leaflet was agreed upon at the 12 June 1984 meeting of SNBTS directors, which Dr Bell also attended. The SNBTS secretary was tasked with making the necessary arrangements to provide leaflets for each transfusion centre, tailored to local methods of preparing call-up letters.[672]
The SHHD was not included in the distribution list for the 10 August 1984 DHSS ministerial submission on a revised AIDS leaflet.[673]
Following an SNBTS Co-ordinating Group meeting on 15 February 1984, Professor Cash wrote to Dr Bell suggesting the formation of a single UK group responsible for coordinating AIDS research related to donors, tests and other measures to increase safety of blood and blood products. He proposed a group which included representatives from existing smaller groups, including haematologists, haemophilia centre directors, and SNBTS directors.[674]
At a CBLA Central Committee for Research and Development in Blood Transfusion meeting on 28 February 1984, Dr Bell discussed a proposed study to identify high-risk donors for AIDS through HBc screening. Despite a lack of enthusiasm for the study, the committee felt that some action was needed to identify potential transmitters of AIDS.[675]
In October 1984, the SHHD became aware that a cohort of patients from Edinburgh, treated with PFC Factor 8, had developed antibodies to HTLV-3. The exact date when SHHD officials first learned of this development is unclear,[676] but by 20 November 1984, Hugh Morison, the SHHD Under-Secretary, informed John Mackay of the situation in a minute also copied to the Secretary of State and others. In his communication, Hugh Morison said that 16 Scottish people with haemophilia had been identified with antibodies indicating exposure to the virus, though this did not necessarily mean they would develop AIDS. He explained that a batch of Factor 8 produced at PFC in Liberton was implicated. It was likely to have been contaminated by a Scottish donor. The SHHD was taking steps to identify the source of infection and withdraw the contaminated batch.[677]
Hugh Morison forwarded this information, along with briefing notes, to the Scottish Information Office, Dr Scott, Dr Bell, and Mr Macpherson on the same day.[678] He said that a revised SNBTS leaflet had been prepared that August, and had been sent to all donors receiving mailed reminders, apart from those in the West of Scotland, and that steps were now being urgently taken to issue the leaflet to donors in the West of Scotland and to those throughout Scotland who did not receive mailed reminders. It was said that issuing a statement was not appropriate at this stage, but that “suitable defensive briefing” had been given to the Scottish Information Office. The briefing, mainly in a Q&A format, addressed the discovery of HTLV-3 antibodies in Scottish people with haemophilia, the contamination of Scottish plasma, and the steps being taken by SNBTS, including the withdrawal of the implicated batch of Factor 8 and efforts to trace the donor.[679]
John Mackay, responding, emphasised the need for openness to avoid accusations of a cover-up and inquired about the readiness of the heat-treatment process.[680]
In response to a Parliamentary Question on 28 November 1984, John Mackay addressed the issue of AIDS and the actions taken by SNBTS, including the issuance of a revised AIDS leaflet to blood donors in Scotland. He emphasised that individuals at high risk of contracting AIDS should not donate blood, a stance that was covered in a newspaper article the following day.[681] The response did not make any reference to the fact that it was by now known (by ministers and officials – not by the patients themselves) that there had been infection of recipients of Scottish Factor 8.
On 29 November 1984, a meeting took place involving the SHHD, SNBTS, and haemophilia centre directors to discuss the situation of the Edinburgh patients and other haemophilia patients in Scotland who had tested positive for HTLV-3 antibodies.[682] Dr Charles Forbes presented findings from Glasgow, and Dr Brenda Gibson expressed concerns of parents of children with haemophilia treated in Glasgow, where imported Factor 8 had been used until recently, leading to five out of ten patients testing positive for HTLV-3 antibodies. At this stage, none of those infected had been informed what had happened: as recorded in the chapter on Haemophilia Centres: Policies and Practice, the news was broken to some of them at a group meeting held in Edinburgh on 20 December 1984, though not to all in a way that they understood related to them. As to that, the meeting on 29 November 1984 wrestled with whether, and what, they should be told:
“Views were exchanged on the very difficult ethical problems which had arisen. These included whether patients and patients’ relatives should be informed and perhaps subjected to needless worry – whether publicity additional to that already provided should be given, and how directors should respond to direct enquiries or requests for advice. The chairman advised members that ministers had been informed and that SIO[683] had been briefed. While a press statement wouId not be issued by the Department at present any enquiries would be answered. It was agreed that every effort should be made for patients to have the situation explained to them before the impending publicity.”[684]
On 5 December 1984, John Davies updated John Mackay (and the Secretary of State) on the Edinburgh patients and other individuals who had antibodies having received imported Factor 8.[685] Ministers were advised that “no statement can be made at the moment until the haemophilia directors resolve the very difficult ethical problem of what action to take with regard to their patients about the matter.” This was despite the agreement minuted at the meeting on 29 November 1984.[686] Yet again clinical freedom was being asserted.
This chapter started with a statement which should be uncontroversial – that a first duty of the state is to look after the safety of its population. That duty must extend to the safety of patients receiving blood or blood products.[687] It is one thing to state a duty: it may be another to recognise the principle not just in rhetoric but in action. The opening words thus described how this chapter would examine whether the government discharged that fundamental responsibility.
This chapter has examined key aspects of the government reaction to the threat of blood-borne disease in the late 1970s and early to mid 1980s. Other chapters deal with further matters which involve the government: but what this chapter has shown is that in each of the areas it has examined the government’s response was lacking. Government did not respond appropriately, urgently and proactively to the risks of transmission of Hepatitis C and HIV through blood and blood products.
For ease of reference, the principal failures discussed in this chapter are summarised below.
Despite full knowledge of the practice of blood being collected from prisoners in almost all transfusion centres in the UK, and it being established from at least the beginning of 1975 that there is a much higher incidence of hepatitis amongst prisoners than amongst the rest of the donor population, no action was taken to stop donations from prisons. Nor even to try to discourage this.[688] This inaction increased the risk of transmission of both Hepatitis B and non-A non-B Hepatitis and, in due course, AIDS. The failure lies principally at the door of the DHSS and the SHHD, but action could and should also have been taken by the DHSSNI and the Welsh Office to put a stop to or discourage the practice in Northern Ireland and Wales respectively.
The response, between 1982 and 1984, to the risks posed to the safety of blood and blood products by the emergence of AIDS was inadequate. In particular:
However, despite high-risk groups[701] being known:
The inadequacy of this response was contributed to by the following six factors:
First, the DHSS erroneously formed the view, in early 1983, that the risks of AIDS transmission were far outweighed by the benefits of treatment with factor concentrates: this both understated the risks of AIDS and overstated the advantages of factor concentrates. It was based upon a binary approach – that it was factor concentrates (which would include commercial concentrates) or nothing that could be used to stop serious bleeds. It lacked a proper appreciation of the potential alternatives. Unfortunately, it remained the bedrock of DHSS thinking throughout 1983 and 1984. A contributing factor to that view – or the adherence to it over the next two years – was in all likelihood an uncritical, or insufficiently critical, acceptance of Professor Bloom’s views.
Second, and as described in the course of this chapter, neither civil servants nor ministers discharged their roles as they should have done. Civil servants failed to bring issues to the attention of ministers when they should have done; there is no evidence of a minister taking any interest before the summer of 1983.
Third, there was no proactive involvement or direction from the CMO, and the CMO failed to play the part which he should have done, until the autumn of 1984. The same is essentially true for the CMOs in Scotland, Wales and Northern Ireland.[703]
Fourth, there was no single, overarching multidisciplinary advisory body such as EAGA until late 1984.
Fifth, non-A non-B Hepatitis, and its transmission through blood and blood products, did not receive the attention which it should have done throughout the 1980s. There was no overarching body with responsibility for advice on blood safety until the establishment of the ACVSB in 1989, and the Advisory Group on Hepatitis set up early in the 1980s, despite its name, failed even to address non-A non-B Hepatitis.
Sixth, instead of trusting its citizens with the fullest information it could give, government repeated the “line” that there was no conclusive proof that blood or blood products transmitted the cause of AIDS. As has been pointed out this was misleading – not because it was untrue, because technically it was correct. But it was not “the whole truth”. There may be a natural human desire to reassure others; the phrase “I’m sure it’ll be alright” is an example, often used although the speaker has no idea how true it is. However, government[704] should not expect people to be mature enough to understand the pros and cons of political debate in order to cast a vote, but then act as though they need to be shielded from the whole truth when it comes to threats to their health. If – as here, for a while it was – many of the facts were uncertain, government should not be afraid to admit it. If it is unsure, the truth government should offer is that it does not yet know: it should not be embarrassed by being unable to give exact advice. Government should, instead, be embarrassed by stating less than the whole truth to people who can then take decisions about their lives even with such limited knowledge as government can offer.
Primary responsibility for these several failings rests with the DHSS: on matters of health policy, and in particular public health, those within the SHHD, Welsh Office and DHSSNI at the time usually followed the lead of the DHSS. Nonetheless, the SHHD, Welsh Office and DHSSNI must bear their own share of responsibility as well. Although their resources (particularly in the latter two jurisdictions) were significantly smaller than the DHSS’s, they too should have made it their priority to ensure, as far as possible, the safety of the supply of blood and blood products. They did not do so.
Some of the submissions which the Inquiry received from its core participants submitted that the government failed to act when it should have done on a precautionary basis. The “precautionary principle” as it is now known was not a common currency in much of the discussion about how to deal with risk in the late 1970s and early 1980s.
The essential principles underpinning a response to risk were however well understood. It was easy to understand – then as now – that all begins, as this chapter began, with the recognition that the overriding principle is to seek to ensure safety. If safety is recognised as primary, then where there is a real risk to safety, steps must be taken to reduce that risk. To ask for more details about the risk, or to seek certainty about it, is to let the risk continue unaddressed while greater knowledge is sought. Instead, the risk must be addressed at once – as best it can be – no doubt whilst further studies, or information, or details are being sought, but without waiting for those steps to happen before taking action.
Take an analogy. If a hurricane is approaching, it may well miss landfall. It may be uncertain what its precise course may be. But to wait until the first trees are being shaken violently on the nearby coastline before trying to batten down the hatches and evacuate the region is to wait too long. Further information may show that the risk has been overplayed – but there is no doubt that action should be taken, and if it is to be effective it cannot wait. Here, unfortunately, and wrongly, government waited.
The actions and inactions described in this chapter go beyond what would today be recognised as a failure to act on a precautionary basis, however that is defined.
Sufficient was known about the risks of transmission of both AIDS and non-A non-B Hepatitis during this period to require the Government to act quickly, decisively and proactively, and with the primary objective of reducing the risks of viral transmission. When the failures in this chapter and the preceding ones on Regulation of Commercial Factor Concentrates, Self-Sufficiency, Viral Inactivation, Pool Sizes and the Organisation of the Blood Services are considered, government could not have prevented every infection, but the probability is that timely action would have saved many.
That the government did not act as it should means that the question asked at the start of this chapter has to be answered by saying, clearly, that it failed to discharge its fundamental duty to ensure the safety of the public.
This chapter examines UK haemophilia centres’ transition from treating with cryoprecipitate to treating with factor concentrates during the 1970s and 1980s. It analyses clinicians’ reluctance to adapt treatment despite the emerging hepatitis and HIV risks and considers ethical failings with regard to consent, communication and research.
1 October 1968 First formal meeting of haemophilia centre directors.
November 1974 Dr Craske reports to UKHCDO hepatitis outbreak in Bournemouth linked to commercial Factor 8.
September 1980 Glasgow symposium considers liver disease in haemophilia.
16 July 1982 US Centers for Disease Control reports three confirmed cases of people with haemophilia who had developed AIDS.
13 September 1982 UKHCDO meeting refers to “remote possibility” that commercial blood products were the cause of AIDS in people with haemophilia in the US.
5 November 1982 Dr Craske’s paper on AIDS makes clear that an infectious agent is the most likely cause.
11 January 1983 Letter from Professor Bloom and Dr Rizza regarding administration of factor concentrates to PUPs. (Letter is misdated 1982.)
13 January 1983 The New England Journal of Medicine warns of risks of AIDS to people with haemophilia and advocates a revised approach to treatment.
24 January 1983 Discussion of AIDS at Heathrow hotel meeting of haemophilia centre directors.
26 April 1983 Professor Bloom reports to CDSC a “probable” case of AIDS in one of his patients.
13 May 1983 Special meeting of reference centre directors discusses AIDS.
24 June 1983 Letter from Professor Bloom and Dr Rizza setting out the general recommendations for treatment agreed at the 13 May 1983 special meeting.
17 October 1983 Professor Bloom tells UKHCDO meeting that there was “no proof that commercial concentrates were the cause of AIDS”; meeting agrees that patients “should not be encouraged to go over to cryoprecipitate for home therapy”.
14 December 1984 UKHCDO prepares AIDS Advisory Document.
Dr Rosemary Biggs director, Oxford Haemophilia Centre (until 1977)
Professor Arthur Bloom chairman, UKHCDO and director, Cardiff Haemophilia Centre
Dr John Craske virologist & chairman, UKHCDO’s Hepatitis Working Party (from 1977)
Dr Charles Rizza secretary, UKHCDO and director, Oxford Haemophilia Centre
CDC Centers for Disease Control
CDSC Communicable Disease Surveillance Centre
DDAVP Desmopressin
PUPs previously untreated patients
UKHCDO UK Haemophilia Centre Directors’ Organisation
This chapter looks at the policies and practices of haemophilia centres in the 1970s and 1980s. Because there were so many centres, and so many patients treated in them, it is not practicable to consider the position of each and every centre. However, the evidence relating to each centre, much of which has been set out in a series of written presentations prepared by the Inquiry and published on the Inquiry’s website, has been carefully considered and shapes the findings and conclusions that are set out later in the chapter.
The chapter starts by considering the overall organisation of haemophilia care, and then pays close attention to the role of the UK Haemophilia Centre Directors’ Organisation (“UKHCDO”)[705] before turning to consider individual centres.
Haemophilia centres were first formally designated in the 1950s following discussions involving the Ministry of Health and the establishment by the Medical Research Council (“MRC”) of its Haemophilia Committee. The MRC’s Haemophilia Committee proposed that a number of haemophilia centres should be designated as reference centres with the object of ensuring uniformity of diagnostic standards and co-ordinating the exchange of information.[706]
In 1964 the responsibility for overseeing the organisation of haemophilia care passed to the Ministry of Health and in 1966 the MRC’s Haemophilia Committee was disbanded. In 1968 the Ministry of Health issued a memorandum HM 68(8) “Arrangements for the Care of Persons Suffering from Haemophilia and Related Diseases” with a list of 36 centres that would take responsibility for the care of those with haemophilia and related bleeding disorders.[707] Three centres (Oxford, Manchester, Sheffield) were designated as special treatment centres to undertake major surgical treatment, and it was recommended that close relationships should be developed with the appropriate regional transfusion centre (“RTC”) from which fresh frozen plasma (at that stage just ceasing to be the mainstay of treatment, to be succeeded by cryoprecipitate) would have to be obtained.
Over the next few years there were further discussions about the organisation of haemophilia centres,[708] resulting in the publication of HC 76(4), a memorandum setting out revised arrangements for the care of haemophilia and related bleeding disorders.[709] Centres which had been designated in 1968 but which no longer met fully the new criteria would now be known as “associate centres” and would be linked with a convenient larger haemophilia centre. Thus was introduced a three-tier system: reference centres, designated haemophilia centres and associate centres. Seventy-four centres were listed in the appendix to HC 76(4), of which seven were reference centres: Oxford, Royal Free, St Thomas’, Manchester, Newcastle, Cardiff and Sheffield.[710] In 1980 and 1981 Edinburgh, Glasgow and Belfast were formally recognised as reference centres. The functions of the reference centres included:
The first meeting, in Oxford, of what became the UKHCDO took place on 1 October 1968. It was attended by directors from centres across the UK, as well as representatives from RTCs. It was at that meeting that Dr Rosemary Biggs suggested that the organisation of haemophilia centres in the UK made it possible to carry out collaborative research not easily done elsewhere.[712]
From 1971 UKHCDO meetings took place annually, under the chairmanship of Professor Edward (“Eddie”) Blackburn. All haemophilia centre directors were invited. The majority of UKHCDO meetings in the 1970s and 1980s were attended by a representative of the Department of Health and Social Security (“DHSS”) and (usually) by representatives from the Blood Products Laboratory (“BPL”).[713] Haemophilia Society representatives also often attended. Dr John Craske, a virologist from the Public Health Laboratory Service (“PHLS”), was a regular attendee from 1974. Minutes from the annual meetings were circulated to all directors, as were the reports from working parties which were prepared for the annual meetings.[714]
Professor Christopher Ludlam (the director from 1980 of the reference centre at the Edinburgh Royal Infirmary) described the annual meetings in these terms: “There was always opportunity to ask questions, to raise topics, but there was a quite a full agenda to get through ... they weren’t meetings where there could be a detailed discussion of issues because of the large number of people in the room.”[715] Professor Liakat Parapia (the director from 1982 of the Bradford Haemophilia Centre) offered a slightly different perspective: it was, he said, “very difficult to debate anything”, due to the numbers in attendance, and it would have been “intimidating to try and speak out” for someone relatively junior like himself.[716]
According to Dr Charles Rizza (the director of the Oxford Reference Centre), writing in 1975:
“This conference of haemophilia centre directors has proved useful not only because it provides an opportunity to exchange views on specific problems, but also because within the framework of such meetings it is possible to collect information, not otherwise easily obtained, concerning many aspects of haemophilia and its management. By pooling such information it then becomes possible to make recommendations and plans for the management of haemophilia on a national scale. The haemophilia centre directors of the United Kingdom are now involved in a very active programme of research, including a review of the incidence of hepatitis and factor VIII antibodies in haemophiliacs, a trial of prophylactic treatment, and a survey of home therapy.”[717]
From 1978 it was decided that the annual meeting would be in two parts: a business meeting followed by a scientific session. Professor Arthur Bloom was the chair designate from the autumn of 1978, succeeding Professor Blackburn, and took the chair from the autumn of 1979.[718]
Regular meetings of the reference centre directors began in February 1976.[719] These were not usually attended by a DHSS representative. The minutes of their meetings were circulated only to the reference centre directors themselves.[720] Professor Edward Tuddenham (co-director of the Royal Free Reference Centre) described the reference centre directors as “a group of colleagues who were gathered together under the common objective of organising and improving the management of haemophilia ... to optimise the monitoring of standard of care, gathering data, making representation to the Department of Health for ways to improve.” It was not, he said, hierarchical, but a group of colleagues who respected each other. It was, to some extent, a talking shop and unless a very, very firm line was taken to pursue a particular policy they did not intend to impose views on the rest of their colleagues because they did not have the executive power to do so.[721]
At a January 1977 meeting of the reference centre directors the decision was taken to set up working parties to study problems of particular interest to haemophilia centre directors and patients.[722] There were initially five working parties: the treatment of patients with Factor 8 antibodies; home therapy and prophylaxis; the incidence of hepatitis in patients with haemophilia; the standardisation of assay methods for Factor 8; and methods for the detection of carriers of haemophilia. Over the following years other working parties were set up.
The system for submitting annual returns to Oxford was in operation at least from 1976; from 1977 these returns were to include details of home treatment and treatment of patients with antibodies. Although extensive reference will be made to the annual returns in this chapter – they are, for many centres, the best (and sometimes the only) available guide to treatment practices – it is right to note that they were far from perfect as a record of product usage. Some returns were not fully or legibly completed; there was not a consistent approach to the calculation of the number of international units, in particular in relation to cryoprecipitate; nor was there a consistent approach to the inclusion of desmopressin (“DDAVP”) on the return. Some were simply not returned.
As at 1980 there were, in addition to the reference centres, over 40 other designated haemophilia centres and about 50 associate centres.[723]
The role of reference centres, as described in the Haemophilia Centre Handbook in 1980 included “assisting other Haemophilia Centres to provide a high standard of care for their patients. This is done by giving advice, organising adequate supplies of therapeutic material, and occasionally by taking over the treatment of a difficult patient for a time.”[724] Associate centres were small haemophilia centres “which do not always have the medical or laboratory facilities for comprehensive, full-time care of haemophiliacs ... but which do provide treatment for most of their local patients, most of the time.”[725]
At a meeting of Scottish National Blood Transfusion Service (“SNBTS”) regional transfusion directors and Scottish haemophilia centre directors in January 1981 (which considered the proposed recognition of Edinburgh and Glasgow as official reference centres) the role of the designated reference centres in England and Wales was explained in these terms: “the designated reference centres were charged with a responsibility for co-ordinating the functioning of the haemophilia service. Many centres in England and Wales are relatively small and look to the larger reference centres for guidance and advice.”[726]
Professor Geoffrey Savidge, in written evidence to the Archer Inquiry, described UKHCDO in the 1970s and 1980s in somewhat sceptical terms. It had:
“no formal affiliation with the NHS through the DOH, any Royal College or learned society (eg: BSH[727]) and functioned as an isolated and autonomous advisory body with its own self appointed working parties, essentially to its own members ... Views and opinions involving observations of important health issues in haemophilia patients from members of the executive committee[728] were relayed by informal delegation through the Chairman (or occasionally vice-Chairman) usually to those committees (eg DOH, CSM, CBLA, National Blood Transfusion Organisations, etc) where actual decisions on haemophilia management, blood product production and funding etc would be taken and implemented. Little if any information was reported back on what the chairman actually discussed at these numerous committees although in several matters eg: blood product projected usage, no heed was taken of the UKHCDO data, and deliberations of these committees involving information from the UKHCDO and their decisions were not fed back in a cogent form either to the executive or to the full body of members of the UKHCDO.”[729]
It should be noted that since the 1990s UKHCDO has undergone a number of structural changes. The descriptions above, and the observations within this chapter about the role of UKHCDO in the 1970s and 1980s, are not directed at UKHCDO in its current form.
As set out earlier in this Report,[730] the 1970s saw a gradual shift from the almost exclusive use of cryoprecipitate, largely in hospitals, to the extensive use of factor concentrates for the treatment of Haemophilia A, both in hospitals and in home treatment.[731] The next part of this chapter examines this development, firstly by reference to the discussions which took place within UKHCDO and secondly by consideration of the treatment policies and practices of the reference centres and some of the larger haemophilia centres.
Home treatment was discussed by the haemophilia centre directors at their meeting on 27 October 1972.[732] It was still at a very early stage, but had been commenced in some centres: Oxford was using concentrate for this purpose, whilst the Royal Free used cryoprecipitate.
Over the following years home treatment programmes became more widespread. There appears still to have been some ambivalence and uncertainty about home treatment by the time of the first meeting of reference centre directors in February 1976, the minutes of which recorded that Professor Ilsley Ingram:
“said that he had taken advice from the Medical Defence Union about home therapy and the ruling was that if a policy taken by a doctor (e.g. to institute home therapy) were one which he honestly thought to be best for his patient then the Medical Defence Union would defend him. Another organisation thought that the patient introduced to home therapy should have the risks and advantages of home therapy carefully explained to him.”[733]
Home treatment continued to be the subject of discussion from time to time amongst the haemophilia centre directors and reference centre directors. A joint meeting of haemophilia centre directors and blood transfusion directors in January 1974 “stressed that home therapy was becoming more accepted and widespread and was improving patients’ lives.” The minutes record that some directors were buying commercial concentrates for use in home therapy.[734]
At the September 1975 annual meeting of haemophilia centre directors, it was reported that a study of home therapy in patients with haemophilia was being organised at St Thomas’ and the Oxford Centre, and that, of those centres represented at the meeting, 25 centres were using home therapy, 20 centres were using commercial concentrate for some part of the home therapy programme, and at 2 centres NHS concentrate was used. 12 centres reported using some cryoprecipitate for this purpose.[735]
1977 saw the establishment of UKHCDO’s Home Treatment Working Party, which identified four projects to be undertaken: a study of minimum dosage required for the control of haemorrhage, a study of prophylaxis, a study of employment, and a study of the long-term side-effects of replacement therapy. Replies from a questionnaire that had been sent to haemophilia centres during 1976 showed that there were at that stage some 729 patients on home treatment.[736]
At the reference centre directors’ January 1978 meeting, Dr Katharine Dormandy (director of the Royal Free) explained that she had patients on home treatment with cryoprecipitate and wished to know if the reference centre directors thought such patients should now be treated with commercial concentrate. The minutes record that it “was unanimously agreed that freeze dried concentrates were the material of choice for home treatment and the Reference Centre Directors recommend that all patients on home treatment should have freeze dried concentrates.”[737] No discussion about the relative safety of cryoprecipitate versus concentrate, or of the increased risk of viral transmission in consequence of such a change, is apparent in the minutes.
It does not appear that the Royal Free immediately ceased using cryoprecipitate for home treatment. The Haemophilia Centre Handbook, produced by the Royal Free and published (by Immuno) sometime after May 1978, contained an explanation of the arrangements for the collection of supplies of cryoprecipitate for home treatment.[738] The same handbook recorded that “All Haemophilia Centres now teach most of their severely affected patients to treat themselves at home.”[739]
A more mixed picture emerges in relation to the provision of treatment on a prophylactic basis.
At the haemophilia centre directors’ first meeting in October 1968 the mood of the meeting was that “at present the treatment of patients with bleeding episodes should have precedence over prophylaxis.” “Experiments in the prophylactic treatment of haemophilic patients” were, however, anticipated.[740] There had been some use of prophylaxis by the time of the April 1971 meeting of haemophilia centre directors, at least in relation to the treatment of Haemophilia B: the conclusion of the meeting was that regular administration of Factor 9 to severely affected Haemophilia B patients was beneficial, regimes of weekly, fortnightly and monthly administration having been tried with success. Prophylactic treatment for Haemophilia A was regarded as more difficult, in part because of the inadequacy of supplies. Some centres were said to be treating a limited number of patients in this way. The minutes recorded that it was felt that a controlled trial of regular weekly treatment for six months and on demand treatment for six months could be useful; Dr Biggs agreed to prepare a draft protocol to test the feasibility of such a trial.[741]
At the October 1972 meeting there was further discussion about a trial: Dr Biggs had had a great deal of trouble preparing a protocol. She concluded that it would be very difficult to organise a prophylactic trial from a haemophilia centre and that Treloar’s might be the only place where it could be done. Dr Biggs had sent her draft protocol to Drs Peter Arblaster, Anthony Aronstam and Seymour Rainsford, and they were planning to organise a trial along the lines of the protocol. Dr Biggs thought it “very important” for a trial to be undertaken, because they really needed to know whether patients were better having prophylactic therapy or just receiving treatment on demand.[742]
The trials that were undertaken are described in the Treloar’s chapter of this Report. In January 1977 Dr Peter Kirk reported to the haemophilia centre directors on the third trial of prophylactic treatment of patients at Treloar’s.[743] Professor James Stewart’s view was that prophylactic treatment should not be entered into until there was sufficient evidence that it was beneficial to patients.[744]
Home therapy figures for 1978 showed that 719 Haemophilia A patients and 87 Haemophilia B patients were on home therapy, and that approximately 77% of those with clinically severe classical haemophilia were now on home treatment in the UK. Cryoprecipitate was still being used but this use was waning. 65 Haemophilia A patients reported receiving prophylaxis in 1978; this was said to be about double the number in 1977.[745]
Discussions about the availability of Factor 8 concentrates, and concerns about there being insufficient supplies of NHS Factor 8, were a feature of the meetings of the haemophilia centre directors throughout the 1970s.[746] The October 1972 meeting recorded that many directors were pressing for permission to purchase the “good commercial products” manufactured overseas.[747] At a joint meeting of directors of haemophilia centres and blood transfusion directors in January 1974 there was “a wide ranging discussion about the relative merits of cryoprecipitate and freeze dried concentrates with regard to ease of manufacture, recovery from the original plasma, ease of administration and recovery of activity in the patients”. Notably, the discussion did not include relative safety. The minutes recorded the general feeling that “larger supplies of concentrated preparations were required now and urgently” and that none of those present would prefer cryoprecipitate if freeze-dried concentrates were freely available.[748]
The first meeting of reference centre directors in February 1976 discussed difficulties concerning the supply of Factor 8.[749]
Hepatitis was a constant feature of discussion at UKHCDO meetings in the 1970s. A report tabled for the meeting of haemophilia centre directors in 1971 described transfusion hepatitis as one of the “most alarming complications of treatment of patients with coagulation defects” (the other being inhibitors) and acknowledged that the danger of infection was related to the number of donors used, which “will increase with the use of dried concentrates made from large pools of donors”. The conclusion of the report was, however, “that the increased risk of clinical illness is not so great as to overbalance the advantages of the use of concentrates”.[750] The greater reliability, ease of administration, and economy of manufacture were said to be in favour of concentrated materials.[751]
This was the mindset that prevailed amongst the majority of haemophilia centre directors throughout the 1970s. The increasing awareness of the risks of hepatitis, in particular of non-A non-B Hepatitis (“NANBH”), did not influence the approach to treatment, as it should have done.
As has been described elsewhere in this Report,[752] November 1974 saw Dr Craske of the Public Health Laboratory reporting to the haemophilia centre directors meeting that there had been an “epidemic” of Hepatitis A and Hepatitis B in patients with haemophilia in Bournemouth who had received one particular batch of commercial Factor 8.[753] Dr Rizza reported to the same meeting 11 episodes of hepatitis in Oxford patients since January 1974. Dr Biggs’ recorded contribution to the discussion that ensued included the statement that “it was not yet proved[754] that commercial factor VIII was much more dangerous from the point of view of causing hepatitis than other preparations”; she expressed the hope that commercial concentrate “would not get an unnecessarily bad name” as it was clinically invaluable while the NHS supply was so limited. Dr Craske agreed but felt that a wholly NHS concentrate was likely to be safer when available. He undertook to draw up a plan to study the incidence of various types of hepatitis at different centres and the relationship of infection to the various types of material used.[755]
At the haemophilia centre directors’ meeting the following year, in September 1975, there was, according to the minutes, a “full discussion about the incidence of hepatitis and the problem of anicteric cases.” The significance of pool sizes was recognised, with Professor Ingram observing that “NHS factor VIII was derived from pools of 500-750 donations whereas the commercial factor VIII was often derived from pools of 2,000 to 6,000 litres of plasma and that the probability of including an infected donation was greater with commercial factor VIII.” This meeting was significant also for its recognition that screening would not exclude all infected batches, both because the tests would not pick up all cases of Hepatitis B and because some hepatitis was caused “by viruses not detected by the test”.[756]
Also in September 1975 a symposium took place in Glasgow at which Dr Craske gave a talk entitled Virus hepatitis complicating replacement therapy. Professor Gordon Lowe recalled Dr Craske discussing at the symposium one of the first outbreaks following the early use of concentrate; it was, he thought, the first time he heard about NANBH.[757]
As has been discussed elsewhere in this Report, 8 and 15 December 1975 saw the screening of the World In Action documentary Blood Money.[758] The reference centre directors held their first formal meeting some two months later. Surprisingly the minutes contain no express reference to the documentary or even to hepatitis, and no discussion of the issues and concerns to which that documentary should inevitably have given rise – and so far as many of their more regular patients were concerned, would have done. Instead there was a discussion about taking part in TV programmes which could “distort the facts and present biased views which were embarrassing to doctors and could be alarming to patients”.[759] The subject of participation in such programmes was to be discussed at the meeting of all directors in autumn 1976.[760]
1977 saw the establishment of UKHCDO’s Hepatitis Working Party, under the chairmanship of Dr Craske. Dr Craske prepared a report for its first meeting entitled Hepatitis Associated Commercial Factor VIII 1976, which was a continuation of a study of Hemofil begun in 1974: the 1976 study looked at the incidence of hepatitis after transfusions of Kryobulin in 1976 and compared it with hepatitis caused by Hemofil. The report proposed that such studies continue in order to consider the number of types and incidence of NANBH and the incidence of sequelae after acute hepatitis.[761] Dr Craske recommended in the report that there be a collection of sera, so that retrospective studies could be undertaken should tests for NANBH become available. A discussion took place at the haemophilia centre directors’ meeting in October 1977 about the advisability of liver biopsy in people with haemophilia, with the consensus being that “each case must be considered individually”.[762]
The very establishment of a working party to study “knowledge of transfusion hepatitis in British haemophiliacs and its sequelae”[763] (and, indeed, the contemplation of biopsy) reinforces the conclusion that it was, rightly, understood that hepatitis (including NANBH) was something serious, requiring further investigation, rather than, as some clinicians have claimed, something believed at the time to be benign and mild. At the very least it shows that clinicians did not truly know what the consequences were, and that if they thought despite that lack of knowledge that the disease was benign, it was in the words of Dr Brian Colvin “wishful thinking”.[764]
The first meeting of the Hepatitis Working Party took place in December 1977 and opened with discussion of the results of the prospective survey on hepatitis carried out at Edinburgh and Treloar’s. The latter’s results showed a higher proportion of patients treated with concentrates with consistently abnormal liver enzyme tests than in boys treated with cryoprecipitate.[765] Further investigations were planned in Oxford and Edinburgh.[766]
The issue of keeping patients on one type of concentrate for as long as possible was raised by Dr Rizza at the reference centre directors’ meeting in September 1978. Dr Rizza referred to patients being kept on a type of concentrate “which they were used to handling and had found satisfactory” rather than as a risk reduction measure.[767] Analysis of data from the 1977 annual returns was reported as showing “a further increase in the average amount of factor VIII required to treat haemophilic patients”. There was no discussion as to the implications of this in terms of risk. The Hepatitis Working Party wanted to look into the incidence of chronic hepatitis in people with haemophilia “as they felt that the problem might be more widely encountered than was at present realised.” Dr Craske requested haemophilia centre directors to send in details of cases of chronic hepatitis on a new form which the Working Party would draw up and distribute to centres.[768]
The 1978 report of the Hepatitis Working Party explained that the DHSS was providing financial support for the surveillance programme for hepatitis at the Oxford Haemophilia Centre and for a project investigating the incidence of chronic liver disease in patients treated with Hemofil in 1974-75; Dr Susanta Ghosh, a research fellow, had been appointed to run the clinical side of the project. As part of the hepatitis surveillance study there had been, since the original work on hepatitis associated with Hemofil and Kryobulin, a review of cases of hepatitis reported as part of the study since 1974. The report noted that “Apart from the increase in the cases associated with the introduction of commercial concentrates, the incidence of jaundice has remained fairly constant since 1974.”[769] Dr Craske’s view at that time was that there was evidence in favour of two types of non-B Hepatitis: “A crucial question yet to be answered is the relative role of each of these agents as a cause of chronic liver disease in haemophiliacs.” In the last few months the Working Party had received reports of patients in several haemophilia centres who were thought to have evidence of chronic liver disease and the Working Party regarded it as important to collect as much information as possible about them. Liver biopsy was a matter for each director to make up their own mind. Dr Craske’s report continued:
“I have recently visited the Department of Medicine at the University of North Carolina at Chapel Hill during a visit to the U.S.A., and had the opportunity to discuss the problem with Dr Roberts and his colleagues. They have carried out almost 100 liver biopsies on patients with chronically elevated serum transaminases in a collaborative survey, and nearly 50% of these have histological changes compatible with cirrhosis, chronic active or chronic persistent hepatitis. These patients have had up to ten years of treatment with freeze dried factor VIII concentrates of different brands. There is controversy as to whether these changes are the sequel to acute viral hepatitis, or are due to some other cause, but Dr Roberts and many other physicians are of the opinion the viral hepatitis is the main factor.”[770]
Dr Craske’s conclusion was that “there remains much work to be done to devise methods to prevent the threat of chronic liver disease clouding the undoubted benefits that large pool concentrates have brought.”[771]
When the haemophilia centre directors met again in November 1978, it was reported that the 1976 and 1977 annual returns from haemophilia centres demonstrated that an increasingly large amount of commercial Factor 8 concentrate was being used by centres. In response to a query from Dr Rizza as to whether the DHSS had any views and whether the DHSS was making any progress towards self-sufficiency, Dr Mary Collins on behalf of the DHSS “said that there was no limit on the amount of commercial material which Haemophilia Centres could receive.”[772]
Dr Craske’s Hepatitis Working Party report was presented at the scientific session of the directors’ meeting but the minutes do not describe any discussion about its significance.
The fifth meeting of the Hepatitis Working Party in August 1979 considered the results of the studies on “the Oxford Haemophiliacs”. 70 out of 174 patients for whom detailed records of liver function tests were available had persistently abnormal liver function tests, of whom 20 had clinical features of significant chronic liver disease. It was agreed to continue the study and to obtain additional evidence of the relationship of transaminitis and overt chronic liver disease to the mortality in these patients and other factors.[773]
There was little discussion of issues relating to hepatitis at the reference centre directors’ meeting on 15 October 1979. Dr Craske presented a pre-circulated report from the Hepatitis Working Party but the only minuted discussion related to the collection of patient data and the kind of information that should be submitted to the Working Party.[774] When the haemophilia centre directors met the following month, the minutes recorded that “There was much discussion regarding the incidence of chronic hepatitis in haemophilic patients, the possible value of liver biopsies and the type of information which Directors would be willing to give to the Working Party.”[775]
The 1979 report of the Hepatitis Working Party explained that the first year of the surveillance programme financed by the DHSS was complete and that the investigation for evidence of chronic liver disease in people with haemophilia undergoing long-term Factor 8 therapy was ongoing at Oxford. There had been an increase in the proportion of NANBH in people with mild haemophilia. “Only 20 ... so far” of the 70 patients with persistent transaminitis had clinical evidence suggestive of chronic liver disease.[776]
At the Hepatitis Working Party’s sixth meeting in February 1980 Dr (later Professor) Howard Thomas and Dr Peter Kernoff (both of the Royal Free) described a prospective study they had carried out on patients receiving concentrate for the first time. Eleven patients were followed for up to four years. All had evidence of chronic hepatitis as judged by persistently abnormal serum transaminases unrelated to Hepatitis B. Most Royal Free patients had received commercial concentrate. Dr Ghosh said similar results at Oxford had been seen in patients receiving mostly NHS concentrate for the first time. It was agreed that more information was needed on the risk to patients of developing chronic NANBH, by prospectively following patients first exposed to concentrate or other products, such as people with mild haemophilia undergoing non-emergency surgery.[777]
The suggestion of an autumn symposium on hepatitis with experts in liver disease emerged from the reference centre directors’ meeting in February 1980. The significance of this symposium is discussed later in this chapter.
The evidence is clear that haemophilia clinicians in the 1970s regarded hepatitis as being of huge significance, and knew that it might well have serious long-term consequences, that there was much yet to be learned about it, and that it was a real threat: hence the Working Party, the ongoing studies, and the contemplation of biopsies. At the start of the decade it was seen as one of the most alarming consequences of treatment. By the middle, in 1975, it was recognised that anicteric cases were a real problem, known that there had been an epidemic in Bournemouth, and that the pool sizes from which commercial concentrates were made meant that they were more likely to cause infection. Indeed, the study (of Hemofil on the one hand and Kryobulin on the other) was aimed at seeing which was worse when it came to infectivity.
What is concerning is that while the problem of hepatitis was very real for those patients who became infected with it, no sense of what was happening to them, or the impact the disease was having on them, or might in the future have, is apparent from the minutes. The problem was rather one to be studied, to be kept under surveillance, but not such as to cause any modification of the treatments being given, or even hesitation about pressing on with more of them. Instead, the minutes show the centres marching on inexorably with the ever-increasing use of concentrates, including developing home treatment, which inevitably increased the volume of concentrate used, and to some extent prophylaxis, which used more again.
There is no point at which the minutes suggest that as a group the haemophilia centre directors stopped, reflected, said such as “Perhaps we should not be continuing with ever more product from even larger donor pools of uncertain origin; should we not stop and think about what we might be doing to patients, and offer them alternatives?”
Safety was not the paramount consideration that it should have been.
In the next part of this chapter, the focus is on the approach to treatment of the reference centres and some of the larger non-reference centres in the 1970s. Associate centres, and the smaller designated haemophilia centres, tended to treat rather fewer patients, who would in any event be registered with a reference centre, and it was usually to the reference centres that the associate centres looked for advice.[778] For that reason product usage in the associate centres is not separately addressed here; however, the position at each and every centre has been considered in the course of formulating the conclusions that appear towards the end of this chapter.[779]
The Newcastle Haemophilia Centre was one of the original centres set up by the MRC in the 1950s. In the early 1970s Dr Peter Jones became its director, succeeding Dr Tom Boon;[780] he was joined in 1978 as co-director by Dr Peter Hamilton.[781] Newcastle was the central reference centre for the Northern Regional Haemophilia Service and Dr Jones considered that “the major part of my responsibility was a regional commitment to the care of children and adults with haemophilia”.[782] Dr Jones’ “Guidelines for the Organisation of a Haemophilia Centre” recorded that “within our geographical region, which has a population of 3.3 million, the home therapy programme is run from the Newcastle Centre and all patients are followed up there by the core team.”[783]
Newcastle was an early proponent of home treatment and commercial concentrates were an established part of its treatment practices by or soon after 1973.[784] Dr Jones’ written statement to the Inquiry suggested that cryoprecipitate was the treatment of choice until 1973 “when sufficient factor VIII concentrate became available”.[785] According to a 1974 paper co-authored by Dr Jones and entitled “Optimum Use of Factor VIII Preparations at Present Available in the United Kingdom”, cryoprecipitate was not considered to be suitable for home therapy at Newcastle and Hemofil was used instead for that purpose. Cryoprecipitate would be used for most other purposes: for patients with bleeds, patients undergoing surgery or dental extraction, and patients receiving physiotherapy and mobilisation following bleeds; whilst Hemofil would be used (in addition to home treatment) for the management of severe bleeds when insufficient cryoprecipitate was available, and for patients with antibodies or who had experienced severe reactions to cryoprecipitate or fresh frozen plasma.[786]
Dr Jones’ policy from the 1970s was to treat children under six[787] with “locally produced” cryoprecipitate rather than factor concentrates but from the age of six, depending on their veins and parental expertise, home therapy could be commenced, and this involved factor concentrates.[788] Thus at Newcastle and from the early 1970s onwards children from six upwards were routinely treated with concentrates, including substantial amounts of commercial concentrates. Prophylaxis was also a feature of treatment policy at Newcastle, with, by 1979, “an effect on the average number of factor VIII units per patient per year”,[789] and the Centre’s policy was to encourage both home treatment and prophylaxis.[790]
According to a 1988 letter to the regional medical officer at the Northern Regional Health Authority, which set out statistics on the use of blood products in the region,[791] in 1969, 270,000 units of cryoprecipitate were used and just 280 units of NHS concentrate; in 1973, commercial concentrate was used for the first time (133,000 units compared to 100,000 units of plasma and 917,000 units of cryoprecipitate); by 1975, the use of commercial concentrate had rapidly increased to 972,000 units; and by 1976, a great deal more commercial concentrate (1,649,240 units) was used than cryoprecipitate (676,050 units) and NHS concentrate (82,800 units) put together.[792] The annual returns from 1976 to 1979 show substantial use of a range of different commercial concentrates (as well as the use of NHS concentrate) and the diminishing use of cryoprecipitate over that period.[793]
In his written statements to the Inquiry Dr Jones asserted that clinicians were only reliant on commercial concentrates because there was insufficient NHS product.[794] Whilst the insufficiency of NHS product no doubt played a part in shaping treatment practices at Newcastle, it is clear that commercial concentrates were considered to be preferable for home therapy for reasons including “size of bottle, volume of fluid required for reconstitution, time of reconstitution, viscosity”.[795] It was apparent to Dr Anne Collins, the regional transfusion director at the Newcastle RTC, that there was “a preference at the Haemophilia Centre for commercially produced Factor VIII blood product, for the following reasons: (a) commercial Factor VIII was more easily soluble. (b) Some patients tended to have allergic reactions to NHS produced Factor VIII ... (c) The presentation of commercial Factor VIII was more attractive to the Haemophilia Centre.”[796] These factors of convenience were not, however, balanced against the risks of infection as they should have been.
The risks of hepatitis from the use of concentrates (and in particular commercial concentrates) were well known to Dr Jones.[797] For example:
Yet some of the information which Dr Jones produced for dissemination to people with haemophilia contained more reassuring messages. Following the World in Action documentary screened in December 1975, Dr Jones wrote in the spring 1976 newsletter of the Haemophilia Society Northumbrian Branch that:
“the programmes screened presented a dramatised account of the danger of hepatitis which, by being taken out of context, was both biased and frightening. As you know the interview filmed in Newcastle was totally cut presumably because in it we tried to present the true picture without condemning a lot of hard working and conscientious people who, through both the National Blood Transfusion Service and the commercial companies, are responsible for allowing us to implement the advances in haemophilia care of which you are all aware.”[801]
Dr Jones went on to set out “the facts”, including an explanation of the “theoretical risk of virus transmission”increasing from 3 to 1 in fresh frozen plasma to between 500 to 1 and 3000 to 1 for AHG concentrate, and to state that “Of course the actual risk will be much lower than these figures suggest as only a very small proportion of donors may carry the virus.”[802] A further article in the autumn 1980 Haemophilia Society Northern Branch newsletter stated:
“As everybody who receives blood products for treatment knows one of the possible side effects is yellow jaundice (hepatitis) ... As a result [of screening] we hardly ever see hepatitis B now. However, there is no way of measuring non A non B hepatitis and the risk of infection, which is almost always a very mild one, is therefore still present ... These [liver biopsy] tests [at other centres] have shown abnormalities but we do not think that these are as serious as was at first believed and there has been no reported increase in severe liver disorders in patients treated with far higher doses of blood product than we use.”[803]
This might be thought to contrast with, in the same newsletter, the inclusion of the introduction to Dr Jones’ talk at the twelfth Congress of the World Federation of Haemophilia:
“Thanks to his colleagues engaged in research and in blood collection and fractionation the clinician has powerful tools with which to manage a chronic and painful disorder. But at what price? Is quality being bought at the expense of longevity? Is chronic hepatic damage really one of the expected side effects of intensive, multi-donor transfusion, or do we play with fears based on serological and histological findings with little relevance to clinical fact? If we are harming our patients, at what stage and by what means should we recognise this harm, and most important of all, can we treat (if we cannot prevent) liver damage in haemophiliacs? ... It is evident, that although the safeguards imposed since the outbreaks of hepatitis B six years ago were welcome, the dangers of viral disease transmission inherent in intensive transfusion are far from over, and that these dangers are compounded by the use of large plasma pools from commercial sources.”[804]
Dr Jones’ anonymous editorial in The Lancet on 14 July 1979 stated “The substantial improvements in the quality of life ... may be bought at the expense of shorter survival.”[805] Writing at a later date, Dr Jones reported that “by the end of the decade [ie the 1970s] we were in no doubt that haemophiliacs exposed to multi donor concentrates were inevitably infected with non A non B hepatitis, and that a substantial proportion of them could go on to develop chronic liver disease.”[806] In Newcastle, as in so many other centres, that knowledge of almost inevitable infection with NANBH and risk of chronic liver disease was not shared with patients as it should have been.[807]
The haemophilia centre at Cardiff moved in 1971 from Cardiff Royal Infirmary to University Hospital Wales.[808] Professor Arthur Bloom was the director of the centre from 1966. He played a very significant part in many of the events with which this Report is concerned.[809]
There is limited contemporary information available about Professor Bloom’s approach to treatment in the early 1970s. In a letter to Dr William d’A Maycock in late 1972 he described the local supply of cryoprecipitate as “quite good” but in anticipation of BPL producing a higher potency concentrate, he explained to Dr Maycock that he would “optimally like to use freeze-dried concentrate if available.”[810] At a meeting of haemophilia centre directors and regional transfusion directors in October 1976 he was recorded as stating that Cardiff used cryoprecipitate for ordinary bleeds, such as into joints, but that they needed freeze-dried material for the treatment of inhibitors and home treatment.[811]
A 31 August 1978 file note by David Williams of Speywood Laboratories Ltd, which described a recent meeting with Professor Bloom, recorded that, until recently, Factor 8 purchases at Cardiff had been split three ways between Hemofil, Factorate and “Elstree”.[812] Professor Bloom had stopped using Armour product “following the hepatitis problem”and no longer bought Immuno because of its high price. David Williams was reasonably confident of getting Cardiff’s business, noting that “Bloom always likes to keep two suppliers, but is reluctant to make frequent changes.”[813]
The annual return for 1976 shows, for the treatment of Haemophilia A, the use of substantial quantities of cryoprecipitate, but a very modest amount of NHS concentrate. Significant amounts of Kryobulin and Hemofil were also in use, together with comparatively small amounts of Factorate, Profilate and Koate.[814] A home treatment programme had been established by this time. The 1977 return shows cryoprecipitate still being extensively used; over double the amount of commercial concentrate (primarily Hemofil) than NHS concentrate was used.[815] Individual patient records provided with the return show no consistent attempt to keep patients on one type of concentrate only. 1978 saw continued substantial use of cryoprecipitate but again over double the amount of commercial concentrates were used than NHS, with Factorate being the largest in volume, although substantial quantities of Koate and Hemofil were also used. The individual records again show some patients receiving multiple concentrates.[816] The annual returns for 1979 continue to show significant quantities of cryoprecipitate in use but over a million units of commercial concentrate compared with 328,538 units of NHS concentrate.[817]
On 10 February 1975 Professor Bloom wrote to another clinician regarding a patient with haemophilia who had “been selected for home treatment” with Factor 8 concentrate, stating that the “risks from the use of this preparation, especially allergic reactions and hepatitis have been explained.” He expanded upon the hepatitis risks as follows: “A small percentage of these freeze dried preparations contain, unavoidably, the virus of serum hepatitis and therefore potentially dangerous to the patient, his relatives etc.”[818]
Professor Ludlam, who worked as a senior registrar in Cardiff from 1975 to 1979, recalled Professor Bloom talking to him on a number of occasions about the “very important event” that was the Bournemouth hepatitis outbreak of 1974 and suggested that the Cardiff director was “cautious” about US concentrates.[819] Dr Saad Al-Ismail, who worked at Cardiff before taking up a consultant haematologist post in Swansea, recalled Professor Bloom’s advice on NANBH as being that for “the vast majority of patients” it was “probably not going to be a big issue.”[820]
In the course of the HIV Haemophilia Litigation Professor Bloom prepared a report for some of the defendants. The report does not detail his own approach to treatment at Cardiff but insofar as hepatitis was concerned, he wrote that it “has always been appreciated by doctors who cared for patients” that most patients with haemophilia were infected with both Hepatitis B and NANBH, but that “patients did not, in the main, seem to suffer from clinical liver disease and mortality from this cause during the 1970’s was low.”[821] By 1980 “most haemophilia specialists recognised the risk of hepatitis in haemophiliacs after treatment with concentrates and the fact that biopsy changes could occur.” The impact of this recognition on treatment practice was, however, marginal: “The general recommendation however was that bleeding was still the main cause of morbidity and mortality and that treatment with concentrates should continue except perhaps that treatment with cryoprecipitate may have been more circumspect in general in young children and that DDAVP should be used, within its constraints, in mildly affected patients with haemophilia A”.[822]
Given the terms in which Professor Bloom expressed himself in this report, it is reasonable to assume that in treating patients at Cardiff in the 1970s he was content to use concentrates (including large amounts of different commercial concentrates) notwithstanding the risk of transmission of hepatitis. That assumption is reinforced by comments on an individual statement of claim in the HIV Haemophilia Litigation made by Professor Bloom in September 1991:
“The existence of the viruses causing serum hepatitis was well known to doctors caring for haemophiliacs during the 1960’s, 1970’s and later. It was appreciated in the early 1970’s that concentrates made from pooled plasma carried a greater risk of hepatitis than blood products made from single donors. It was also thought that products made from commercial paid donors could present a greater risk of hepatitis than products made from UK domestic voluntary donors although this assumption later proved to be incorrect. However, tests for screening for hepatitis B improved and commercial firms improved their rules of donor selection in the mid 1970’s. Close monitoring of jaundice and deaths from hepatitis carried out by the UK Haemophilia Centre Directors ... indicated a low incidence of jaundice in haemophilia and few, if any, deaths from hepatitis. Even when the occurrence of chronic non A non B hepatitis was recognised in haemophilia in the late 1970’s and early 1980’s there was published evidence from reputable physicians that it was considered to be a benign non-progressive disorder. It was not until the mid 1980’s that the potentially serious nature of chronic hepatitis in haemophilia was fully recognised”.[823]
The reference centre at the Manchester Royal Infirmary was part of a regional haemophilia service in North West England, which included Manchester Children’s Hospital and the Lancaster Haemophilia Centre.[824] Dr Irvine Delamore was its director throughout the 1970s and was joined by Dr Richard Wensley in 1974. Somewhat unusually Dr Wensley worked in both haemophilia care and transfusion, being a joint appointment between the regional transfusion centre in Manchester and the Manchester Royal Infirmary. One of the aims of the appointment was a better understanding with the RTC and “a greater availability of cryoprecipitate and better treatment for all haemophiliacs.”[825]
A January 1970 article from the Manchester Evening News described what were said to be recent improvements in the lives of those with haemophilia and in particular Manchester Royal Infirmary’s role: “today with modern methods of treatment and patient assessment, much of which has been pioneered over the past 20 years at the Manchester Royal Infirmary, haemophiliacs are for the most part able to lead a near-normal, albeit hazardous, life. Their great salvation comes in small plastic bags containing what is known as the cryoprecipitate.”[826]
As at December 1972, Dr Delamore, completing a questionnaire for Dr Maycock on treatment preferences, and treating around 200 patients regularly, preferred to administer cryoprecipitate but observed that if freeze-dried concentrate could be altered to be dissolved more easily and in smaller volume, “we would probably choose that preparation in preference to cryoprecipitate.” He also noted that concentrates were “much more suitable for home treatment”, which the Centre hoped to institute in selected cases.[827]
Manchester was slower than some other large centres to institute home treatment and appears to have used cryoprecipitate for home treatment at least until 1978.[828] Dr Douglas Lee, who was the director of the Lancaster Haemophilia Centre from 1977 to 1989, recalled that Dr Wensley was a “powerful advocate of cryoprecipitate”whose “thoughts were that yields of cryoprecipitate over those of concentrate are roughly 70% compared to 20%, and the risks of transfused virus are certainly less.” Dr Wensley “would advise this constantly at haemophilia directors’ meetings, and I remember that he was very much alone on this point at one time.”[829]
The annual return for 1976 shows substantial use of cryoprecipitate, NHS concentrate and Kryobulin, with some use of Hemofil. Both FEIBA and porcine Factor 8 were also used.[830] 1977 saw an increase in the volume of NHS concentrate used, but a greater volume of commercial as well. Cryoprecipitate was still in substantial use but the volume had decreased since the previous year.[831] In 1978, NHS concentrate was used in greatest measure, but significant quantities of commercial concentrates and cryoprecipitate were also used.[832] A similar pattern appeared in 1979, with NHS concentrate used in greatest measure, but with large quantities of commercial concentrates and cryoprecipitate all used as well.[833]
A note of a November 1978 meeting between David Williams of Speywood and Dr Wensley records the latter suggesting that the NHS concentrate now compared well with commercial and that he was gradually changing his home treatment patients from commercial to NHS concentrate, with the plan that commercial concentrate would then be used only in operations.[834]
Writing in 1986 Dr Harold Gunson explained that Dr Wensley’s job when appointed in 1974 was “to treat patients with haemophilia at the Manchester Royal Infirmary and to be responsible for the production of cryoprecipitate which was at that time the product of choice for the treatment of these patients.” Dr Gunson said that Dr Wensley “worked very hard and devised a semi-automated method for producing high quality cryoprecipitate from which the patients in the region derived considerable benefit.” However, since 1980 there had been a decline in the use of cryoprecipitate in favour of Factor 8 concentrate.[835]
It would appear that certainly by 1978 the transmission of hepatitis was a matter of concern to Dr Delamore. Having been asked to identify three topics he considered most worthy of study by UKHCDO working parties, he identified the incidence of hepatitis in haemophilia as being the highest priority in a March 1977 letter to Dr Rizza,[836] and at the November 1978 “Haemophilia Today”seminar, held at Manchester Royal Infirmary, Dr Delamore was recorded as noting that: “a very high percentage of patients being treated for haemophilia and Christmas disease are proving after all to be infected by one type of hepatitis or another. A great deal more work in assessing the severity of hepatitis needs to be undertaken, possibly to develop an immunisation against hepatitis or in developing ways of making blood products safer.”[837]
Conversely, however, Dr Delamore and Dr Wensley were both contributors to the 1983 article “Liver disease in haemophiliacs: an overstated problem?” 12 multi-transfused patients with haemophilia were biopsied and described in that paper, which reported that “only” 1 showed evidence of progression to active cirrhosis, although a further 4 patients showed some evidence of mild chronic active hepatitis. The study was acknowledged to be small but said to represent “a much lower incidence of severe histological liver damage than many previous reports.”[838]
The haemophilia centre at St Thomas’ Hospital was under the directorship of Professor Ingram until 1979, when he was succeeded by Dr (later Professor) Geoffrey Savidge.[839] Professor Ingram was an early advocate of home treatment, writing to Dr Maycock in 1972 that he was “pressing on with training as many severe haemophiliacs as possible to give themselves their own treatment.”[840] In 1974 he wrote a letter to the editor of The Lancet in support of Dr Biggs’ request for a realistic supply in terms which suggested that St Thomas’ was using commercial concentrates: “We know that treatment material is being provided within the Health Service in increasing amounts, but it is still far short of what we need. Until the N.H.S. provision is adequate, it is cruel not to make good the shortfall from the large supplies of good commercial material which, as Dr Biggs says, are now available.”[841] By 1976 St Thomas’ was “well in our stride with the Home Treatment Study, and have taken in as many patients as the supplies of factor VIII concentrate allow.”[842]
On 9 February 1978 Professor Ingram, in correspondence to Dr Maycock, set out the shortfalls that the region (for which St Thomas’ was the reference centre) was continuing to experience:
“Since we already distribute nearly all our monthly allocation from the BPL, it looks as though more and more commercial material will have to be bought to satisfy our demands for home treatment alone, let alone our needs for surgery and patients with antibodies. In fact, our own monthly allocation is only sufficient for 75% of our Home Treatment needs at this Centre as it is. We are of course also using considerable quantities of commercial material for surgical cover ... Can anything further be done to increase NHS production?”[843]
At the reference centre directors’ meeting in September 1980, Dr (later Professor) Geoffrey Savidge asked what the policy of the haemophilia reference centre directors was regarding the use of cryoprecipitate, both for treatment generally and for home therapy. Professor Bloom, responding, said that it was “a matter for the individual Directors to decide”, but then referred to the 1978 reference centre directors’ meeting at which they had agreed that Factor 8 concentrates were preferred for home therapy.[844]
In his oral evidence to the Archer Inquiry, Professor Savidge, when asked about the timescales about knowledge of NANBH, described two schools of thought:
“One school of thought was: this causes problems, and it was backed up by a lot of tissue work biopsies, liver biopsies, which showed progressive liver disease, and then you had another group of individuals, who are quite happy to say that, you know: we just measure it with blood tests and the blood tests stay the same, so we just think it is a little bit of inflammation of blood tests from the liver. So-called transaminitis, which has no clinical connotation and which is merely a figment of a few people’s imagination. So, by the time the histology data started coming through and by the time children started developing cirrhosis of the liver, perhaps it was a little bit more than inflammation of blood tests.
So I think the majority of responsible physicians and people treating these patients knew by the end of the 70s -- in fact pretty closely about 78 I think tipped it -- that large donor pool concentrates, whether it be for Factor 8 or Factor 9 were the cause of non-A/non-B hepatitis. Nobody knew what the agent was but they assumed it was an infective disorder; it came from an infection. And as time moved on, it became proven that was the case.” [845]
In his written statement to the Archer Inquiry, Professor Savidge gave his perspective on the broad nature of haemophilia treatment in the 1970s and 1980s:
“extra money when found was spent on the purchase of commercial imported factor VIII concentrate, usually from the US, in preference to the safer cryoprecipitate that was the recommend [sic] treatment of children and mild haemophilia patients (assuming failure with DDAVP) generally available (in some regions in excess). The US commercial concentrate was considered to be more user friendly, it could be stored at room temperature and was eminently more suitable for patients on home care programmes.”[846]
There is no reason to think that this description did not encompass treatment practice at St Thomas’. Whilst the annual returns for 1976 and 1977 show NHS Factor 8 concentrate and cryoprecipitate as the most used products,[847] a different picture emerges from both the 1978[848] and the 1979 return:[849] commercial concentrates were then the products most in use.
The Haemophilia Centre at the Royal Free Hospital was the largest in London. Its director from 1968 to 1978 was Dr Dormandy. Dr Kernoff and Dr (later Professor) Tuddenham were co-directors between 1978 and 1986.[850]
The Royal Free began to use commercial concentrates in 1973.[851] Its annual return for 1976 indicates that at that stage Haemophilia A patients were treated primarily with cryoprecipitate, followed by commercial concentrate and then NHS.[852] The pattern was similar in 1977.[853]
In January 1978 Dr Dormandy described in a letter to Dr Richard Lane the Royal Free’s treatment policy in relation to NHS concentrate: “It is our policy to use NHS-concentrate for patients on home treatment and for those who are allergic to cryoprecipitate. This material is used for the treatment of patients who attend hospital with uncomplicated bleeds and for minor operations, and commercial factor VIII for major operations, some inhibitor patients and a backlog of patients on home treatment.”[854]
In May 1978 Dr Dormandy died. She had been known as an early and keen advocate of cryoprecipitate for home treatment.[855]
The annual return for 1978 shows that over the course of that year, for the first time, more units of commercial concentrates were used than cryoprecipitate.[856] In 1979 the volume of commercial concentrates was almost double that of NHS Factor 8 and cryoprecipitate.[857] As described in Professor Christine Lee’s evidence to the Lindsay Tribunal, Drs Kernoff and Tuddenham “came in in 1978 and very rapidly changed everybody to concentrate.”[858]
This was a conscious decision; as recorded at a meeting on 1 September 1978 “it was the intention to switch home treatment patients from cryoprecipitate to concentrate. Half the home treatment patients at the Royal Free were still using cryoprecipitate and this was felt to be an unacceptable state of affairs. If NHS concentrate was not available then commercial concentrate would have to be bought.”[859] Professor Tuddenham, in his evidence to the Inquiry, explained that concentrates had practical advantages and that they were more reliable in elevating the factor level in cases of head injury or life-threatening bleeding; he acknowledged in hindsight that the relative risks were not sufficiently appreciated.[860] The switch to concentrates encompassed those with moderate haemophilia, and patients with mild haemophilia may well have been given concentrates as well.[861] Children were prioritised for NHS concentrate.[862]
This was at a time when Dr Kernoff was well aware of the risks from commercial concentrates. Writing in April 1979 in his capacity as chairman of the Haemophilia Working Party of the North East Thames Region Association of Haematologists, he recorded the “growing awareness of the probability that commercial concentrates have a higher risk of transmitting non-A non-B hepatitis than NHS material”, NANBH being a “serious disease with long-term consequences” and therefore there were“both clinical and moral reasons for preferring the NHS material”. He suggested that cryoprecipitate, although relatively cheap to produce, had “serious clinical disadvantages”and that the shortfall in NHS concentrates “has to be met by buying commercial concentrate”.[863]
The NANBH risks associated with Factor 8 concentrates were the subject of discussion at the Haemophilia Working Party’s meeting on 4 April 1979, at which Dr Kernoff reported “the increased recognition of Non A/Non B Hepatitis as a risk of Factor VIII concentrates”. There was no discussion about any change of approach to treatment, nor about the provision of information to patients. Instead what was agreed was regular testing for Hepatitis B and liver function tests, and the storage of sera for a retrospective study for NANBH.[864]
At an August 1979 meeting of the Haemophilia Working Party, Dr Kernoff reported on his and Dr Colvin’s “recent experience of post-treatment hepatitis”. It was agreed that all registered haemophiliacs on regular treatment should be fully screened for hepatitis at their regular three-month visits to the major haemophilia centres.[865] That Dr Kernoff was not a fan of cryoprecipitate was clear: he was recorded as stating in relation to the Royal Free that “25% of all Factor VIII used was in the form of cryoprecipitate which was far from satisfactory.”[866]
DDAVP was not in use at the Royal Free until some time after 1980.[867] However, between 1981 and 1985 usage increased substantially.[868]
Professor Lee, who did not at this time work at the Royal Free, expressed the firm view that the Royal Free’s haemophilia centre directors could not be criticised for the complete change from cryoprecipitate to concentrate.[869] I disagree. Though she deferred to Professor Tuddenham on the reasons for the change, I consider she was right nonetheless to identify them as “probably the convenience and the efficiency”.[870] These reasons persuaded them to change despite the fact, as Professor Lee understood it, that the previous director, Dr Dormandy, had been particularly keen on the use of cryoprecipitate because of a study she had done with US counterparts who had treated exclusively with the new concentrates. It had shown her that they suffered raised transaminases more commonly than her own patients who were treated with cryoprecipitate.[871] The change was despite the fact that Dr Kernoff knew that NANBH was a serious disease with significant long-term consequences, and had made a point of this to other clinicians.[872] It was despite the fact that at the time he believed (as had Dr Dormandy) that factor concentrates exposed recipients to a greater risk of infection because of the large sizes of the pools from which they were made.[873] Professor Tuddenham recognised in his evidence that it was known there was risk, but volunteered that “the extent to which that was a risk in numerical terms wasn’t sufficiently appreciated, in hindsight”.[874] I agree with this, save for the reference to hindsight, since the risks were there to be, and were, seen at the time, and patient safety should have required a more cautious approach. After all, Dr Craske had finished his recent report on the hepatitis outbreak in Bournemouth by suggesting that “Commercial factor VIII concentrates should be reserved for the treatment of life-threatening bleeds in all haemophiliacs and for covering major operations.”[875]
The Oxford Reference Centre became the largest haemophilia centre in the country, treating both adults and children. A large proportion of patients came from outside the area for treatment. The Centre built on earlier work conducted at the Blood Coagulation Research Unit at the Churchill Hospital under the leadership of Dr Gwyn Macfarlane. Dr Biggs served as director until 1977 when she was succeeded by Dr Rizza.[876]
Due in part to its co-location with the Plasma Fractionation Laboratory (“PFL”), the Centre made the switch from cryoprecipitate to factor concentrates relatively early. In a 1977 article, Dr Biggs wrote that:
“It will be seen that at Centres other than Oxford the amount of cryoprecipitate used has increased steadily over the years ... This increase has been due to the efforts made by Regional Transfusion Centres. In 1974 cryoprecipitate still accounted for nearly 80% of all material used (at Centres other than Oxford). By contrast, at the Oxford Centre cryoprecipitate has never constituted more than 43% of material used and since 1971 the proportion of cryoprecipitate has fallen steadily ... In Oxford, plasma previously used to make cryoprecipitate is now fractionated to make NHS concentrate. The amount of NHS concentrate used in Oxford reflects close proximity and the good co-operation between the Oxford Regional Transfusion Service and the Plasma Fractionation Laboratory which has enabled plasma to be fractionated to make all valuable components rather than used for cryoprecipitate and red cells alone.”[877]
During the period 1969 to 1974, the use of cryoprecipitate at the Centre dropped from 21.99% to 3.86% of total Factor 8 material used, while the use of NHS concentrate rose from 45.93% to 60.89% of the total. Commercial Factor 8 was introduced in 1973, when it made up 17.74% of product used, rising to 35.25% the following year.[878]
By 1976, 42.6% of the material used at the Centre was NHS Factor 8 concentrate, just 1.54% was cryoprecipitate, and the rest was commercial concentrate produced by Hyland Laboratories and Immuno Ltd.[879]
In July 1977 Dr Rizza wrote that there had been since April 1977 a greatly increased supply of plasma to the PFL and the Centre was now beginning to receive nearly twice as much locally made NHS Factor 8 compared to the previous year. As a consequence the Centre was able to transfer several patients from commercial to NHS concentrate. This was described as a “bright light on the horizon”.[880]
Dr James Matthews, who worked alongside Dr Rizza, recollected at a later (1998) Wellcome Institute seminar that home treatment was not introduced for some time.[881] However, it appears that home treatment had commenced in 1971 for a very small number of patients. By 1975 there were 54 patients on home therapy (representing about 25% of Haemophilia A patients).[882]
The use of commercial concentrates was well established at the Centre, with Dr Rizza giving a colleague at another hospital an order of preference for Hemofil, followed by Factorate, and then Kryobulin. The Centre had also used Profilate and Koate: Dr Rizza said “we find them all equally effective clinically ... we tend to use Hemofil”.[883]
The 1977 annual return recorded no use of cryoprecipitate at all and greater use of commercial concentrates than NHS.[884] The overall figures for 1978 are unclear.[885] The 1979 return recorded figures for home therapy: no cryoprecipitate; a small amount of Elstree Factor 8; 1,078,110 units of Oxford Factor 8; and 906,830 units of commercial (Factorate, Koate, Hemofil).[886] NHS Factor 8 was (according to Dr Rizza writing in 1984) always in very short supply and reserved “as far as possible” for young children and adolescents: “Ultimately most severely affected patients are changed from NHS to commercial factor VIII especially those who use larger amounts of factor VIII.”[887]
Like Professor Bloom, Dr Rizza produced a report for the HIV Haemophilia Litigation. This suggested that during the first half of the 1970s “hepatitis was probably not perceived as a long term problem in haemophiliacs” but that more detailed follow-up of people with haemophilia during the late 1970s showed that a significant number who were clinically well had persistently abnormal tests of liver function and that liver biopsy studies revealed a significant number with abnormal liver histology consistent with chronic liver disease.[888]
Belfast, Edinburgh and Glasgow were not formally recognised as reference centres in the 1970s but were large and important centres.
The haemophilia centre in Edinburgh Royal Infirmary served a large geographical area, encompassing patients in the south of Fife, Kirkcaldy, Dunfermline and most of the Borders.[889] It received NHS concentrates directly from the Protein Fractionation Centre (“PFC”) in Liberton via the hospital blood bank. Cryoprecipitate was received from the blood transfusion centre in Edinburgh. In the course of the 1970s cryoprecipitate was the preferred treatment of Dr Howard Davies, the then director, with no commercial concentrates being used.[890]
Dr Davies’ preference for locally sourced materials centred on the risks associated with hepatitis viruses as well as a reluctance to introduce novel viruses to the local population.[891]
The annual returns from 1976 to 1979 confirm no use of commercial concentrates. In each of the years 1976, 1977, 1978 and 1979 the principal product used was cryoprecipitate.[892] No commercial concentrates were recorded, even for the treatment of inhibitors. As discussed later in this chapter, the position changed in 1980, following Dr (later Professor) Ludlam’s arrival in place of Dr Davies, when the volume of NHS concentrates used exceeded the volume of cryoprecipitate for the first time, and a (relatively) small amount of commercial concentrate (Factorate) was purchased, which was used for both inhibitor and non-inhibitor patients.[893] Perhaps the most striking feature of the 1980 return is the overall volume of products used in comparison with previous years, for a broadly similar number of patients.
In the 1970s the directors of the haemophilia centre in Glasgow Royal Infirmary were Dr (later Professor) Charles Forbes and Dr Colin Prentice. It served effectively as the reference centre for the whole of the West of Scotland (although was not formally designated as a reference centre until 1980/1981). Although it was an adult centre, with children treated at the Royal Hospital for Sick Children in Glasgow, children might transfer from the latter at around the age of 12 or 13 but it was, according to Professor Gordon Lowe (who succeeded Dr Forbes as director in 1988, with Dr George McDonald as his co-director), very much up to the director at the children’s hospital to decide.[894]
Commercial concentrates were in use in Glasgow in 1974 and 1975, although cryoprecipitate was the predominant product in both years.[895] In 1976, according to the annual return, the use of concentrates (more NHS than commercial, although Profilate, Factorate, Koate and Hemofil were all used) exceeded the use of cryoprecipitate;[896] the picture was similar in 1977[897] and 1978.[898] 1979 saw a reduction in the use of cryoprecipitate and an increase in the use of concentrates, both NHS and (in particular) commercial.[899]
According to Professor Forbes’ evidence to the Penrose Inquiry, he did not see the World In Action programme in December 1975 but “It was the talk of the haemophilia part of the hospital. Very much so.” He described a “gasp of disbelief when they showed the types of donors that were being used to give plasma in commercial centres”, adding that he thought “that was the dominant thing in the discussions at that time”.[900] However, he later suggested that “at the end of the day the risk of dying of bleeding was always much greater and that was what drove all of us to use these products despite the possible downside”.[901] Asked about Dr John Cash’s 24 January 1976 letter to The British Medical Journal (in which he observed that “the import into the United Kingdom of Factor VIII concentrates derived from external sources, however well screened for hepatitis viruses, represents an unequivocal pathway by which the level of a potentially lethal virus into the whole community is being deliberately increased”), Dr Forbes indicated that he would not agree with the words “deliberately increased”, but did agree that undoubtedly the importation of concentrates was “bringing with it a potentially lethal virus into the whole community”.[902] Discussing home treatment, of which he was a strong advocate, and the increased numbers on home treatment by around 1978, Dr Forbes described this as “the golden age, in which we actually seemed to be doing something valuable for these patients”, and “before all the horrendous complications came on stream”.[903] By 1979, the issue of chronic hepatitis “dominated everyone’s lives”.[904]
The Belfast Haemophilia Centre was established in 1958 but until 1981 it was included in the Oxford supra-region.[905] In 1980/1981 the Centre, which was based at the Royal Victoria Hospital (“RVI”), was designated as a reference centre.[906] It was the only centre in Northern Ireland and served patients drawn from all over the region. Dr Elizabeth Mayne became a consultant haematologist at the RVI in 1972 and director of the Centre from 1978.[907]
In 1988, Dr Mayne, referring to the history of haemophilia care in Northern Ireland, described patients as being “ecstatic”with the advent of cryoprecipitate which was “revolutionary”.[908] However, in a report prepared for the HIV Haemophilia Litigation in May 1991, she described difficulties in the use of cryoprecipitate: “A major disadvantage was the unpredictability of infused dosage ... A further disadvantage was the necessity of storage of the product within a deep freeze unit. Advantages were efficacy, low donor exposure and simplicity of manufacture.” Dr Mayne suggested that the development of factor concentrates “had an estimated dose content. They enabled accurate calculated doses of Factor VIII to be given in small volume, associated with a decreased chance of clinical side effects. They represented manifest advantages over cryoprecipitate.”[909]
Dr Mayne recalled the first use of concentrate in Belfast as being in 1971.[910] Thereafter Hemofil was the commercial concentrate used for the next three years.[911]
In January 1974 Dr Mayne reported to a joint meeting of haemophilia centre directors and regional transfusion directors that Belfast was using material prepared from approximately 10,000 donors.[912]
In the mid 1970s Dr Mayne instituted a home treatment programme using commercial concentrate. Her policy was that all home treatment patients would be treated with Kryobulin and all hospital treatment would be with Hemofil. Children would continue to be treated with cryoprecipitate.[913] She chose Kryobulin because the company was straightforward and their packaging ideal; Hemofil because she had been familiar with it since 1971.[914]
Following a meeting with Dr Mayne in October 1978, David Williams of Speywood wrote that:
“Dr Mayne is not prepared to change her present policy concerning human factor VIII. She uses Hemofil for operations and Immuno for home treatment (22 patients). She realises this is an expensive policy, but feels that treatment changes are something best avoided with Haemophiliacs. She is very concerned about liver enzyme changes, but at least she knows what to expect with products which have been used for some years. There is also loyalty to Hemofil, because Baxter obviously gave her considerable financial help in the early days.”[915]
In early 1979 Dr Mayne placed an order for Koate with David Williams. The home treatment programme was likely to expand and it was likely that “our needs for commercial Factor VIII may expand further due to increasing orthopaedic operations, etc. being carried out on the site”.[916]
The 1976 annual return records the use of cryoprecipitate (376,190 units) and commercial concentrates (423,656) (Hemofil and Kryobulin). No NHS concentrate was used.[917] A similar picture emerged in 1977[918] and 1978.[919] The returns do not suggest any formal system of batch dedication existed.
In 1979 the vast bulk of treatment was with commercial concentrates (Hemofil: 557,655 units, Kryobulin: 440,051).[920]
Throughout the 1970s liver function tests were performed on patients at Belfast “because of my apprehension about the adverse effect of prolonged IV treatment”;[921] the tests showed persistent abnormal liver function.[922] Dr Mayne’s various descriptions of her evolving knowledge of NANBH are not entirely consistent. In her sixth statement to the Inquiry she said that between “the late-1970s and the mid-1980s, there was increasing evidence that NANB hepatitis was not as benign as had been thought but could progress from chronic persistent hepatitis to cirrhosis.”[923] However, in her 1991 HIV Litigation report it was claimed that the “possible significance of asymptomatic hepatitis became apparent by 1978 ... when structural abnormalities of the liver were described in patients”(citing the paper by Spero et al in the New England Journal of Medicine).[924] In another litigation report she suggested that “the risk that non-A non-B hepatitis could progress to chronic hepatitis was known in 1977 but the full significance of its effects was not appreciated, elaborated and investigated until the mid- to late-1980s” .[925]
The haemophilia centre at Sheffield was first based at the Royal Infirmary before moving to Royal Hallamshire Hospital. It was a reference centre but not one of the larger reference centres.[926] Its first director was Professor Eddie Blackburn.[927] He was succeeded in 1981 by Dr (later Professor) Eric Preston.
At Sheffield there was a particular focus upon hepatitis and liver disease. Significant research into hepatitis was undertaken there and Dr Preston was part of the UKHCDO’s Hepatitis Working Party for many years. Unusually for a haemophilia centre at that time Dr Preston worked closely with a hepatologist, Dr David Triger, as well as a consultant histopathologist with a special interest in liver disease, Dr James Underwood.[928] The importance of the study reported in The Lancet in 1978 has been discussed elsewhere in this Report[929] but Dr Preston told the Lindsay Tribunal that the broad spectrum of chronic liver disease which it revealed “surprised us and concerned us”.[930] The results of a collaborative survey between Sheffield and the Royal Free were presented to the Hepatitis Working Party in December 1980 and showed that approximately one third of the patients studied had the appearance of chronic active (aggressive) hepatitis.[931] A letter to The Lancet in 1982 reported that “we have previously shown that there is a high incidence of chronic liver disease among patients receiving blood product concentrates even in the absence of any symptoms” and described a further case in which significant progression of liver disease was shown over two and a half years in the absence of any symptoms.[932]
The annual return for 1976 showed the centre treating its patients with cryoprecipitate, NHS Factor 8 and commercial concentrates.[933] 1977 saw increased use of concentrates (both NHS and commercial) but a substantially reduced use of cryoprecipitate.[934] In 1979 the centre’s return recorded no cryoprecipitate use at all for people with Haemophilia A.[935] In 1980 a small amount of cryoprecipitate was used, but the mainstay of treatment was commercial concentrate (with some NHS concentrate).[936]
The limited use that was made of cryoprecipitate may reflect Professor Preston’s view (as expressed in his statement to the Inquiry) that cryoprecipitate was “not an option for the treatment of sever [sic] haemophiliacs”.[937] Professor Preston also indicated that whilst the hepatitis risk from commercial products was substantially greater than from NHS products, “there were insufficient NHS products for the treatment of Royal Hallamshire Hospital patients”.[938] His policy was to treat people with mild haemophilia with DDAVP as soon as it became available.[939]
Two aspects of Professor Preston’s approach were: to purchase a number of different commercial concentrates (this was described as “not putting all the eggs in one basket in case something happened with the supply chain and so a number of different products would be used rather than just one product”) but to “keep individual patients on the same concentrate, and the same ‘batch’ for as long as possible to minimise exposure to different blood donations”.[940] According to Professor Preston’s evidence both to the Lindsay Tribunal and to this Inquiry, the amount of Factor 8 (and Factor 9) given to patients was very much less than the majority of other reference centres, although he did not think this reflected a deliberate decision to take a conservative approach.[941]
Birmingham was not a reference centre but it was one of the largest centres in the country. Haemophilia care was split between the Children’s Hospital and the Queen Elizabeth Hospital (“QEH”) and they were jointly designated as a haemophilia centre in the 1970s.[942] In 1976 Dr (later Professor) Frank Hill succeeded Dr Jillian Mann as director at the Children’s Hospital; Dr (later Professor) John Stuart was director at QEH until 1983 when he was succeeded by Dr (later Professor) Ian Franklin.[943]
By 1974 a home treatment programme had begun.
The West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs met regularly throughout the 1970s to discuss issues relating to supply.[944] At a meeting of the Working Party in December 1975 difficulties in producing sufficient plasma were recorded and it was agreed that commercial Factor 8 (Kryobulin) would need to be purchased at an annual cost to the region of £350,000.[945] A meeting of the Working Party in May 1977 noted that the demand for cryoprecipitate was going down and that NHS concentrates were not being used at the rate that had been predicted.[946]
The 1976 return for QEH showed cryoprecipitate, NHS concentrate, Factorate and Kryobulin all being used in substantial quantities.[947] At a Working Party meeting in November 1977 Dr Stuart stated that during 1976 QEH had used 500,000 units of commercial Factor 8 for home treatment, with all the NHS product having been used for treatment in hospital and for dental cases. He stated that his preference was to have all his Factor 8 from the same source (ie either NHS or commercial), and that he was minded to discontinue cryoprecipitate as a home treatment and use NHS product instead.[948] During 1977 QEH used significant amounts of commercial Factor 8 (almost double the amount from the previous year) as well as NHS Factor 8 (at a similar level to the previous year).[949]
During 1978 little cryoprecipitate was used and the NHS and commercial Factor 8 levels broadly remained similar to the year before.[950] In 1979 almost no cryoprecipitate was used and the amount of commercial concentrate (Factorate and Hemofil) was well over double the amount of NHS concentrate.[951]
Whilst Professor Hill told the Inquiry that he believed in the late 1970s that non-A non-B Hepatitis was a minor self limiting condition with no serious long-term consequences[952] (an assessment which, if actually held, was wrong for the reasons described elsewhere in this Report), it appears from the minutes of the November 1976 Working Party meeting that both Dr Hill and Dr Stuart were concerned about the risks of hepatitis: referring to “the hepatitis risk in respect of freeze dried Factor VIII concentrate obtained from commercial sources”, Dr Hill asked whether it might be advantageous to reserve the NHS Factor 8 for children, “leaving the concentrate obtained from commercial sources, largely of foreign origin, for adults”. Dr Stuart agreed with Dr Hill as to the hepatitis risk, and said that “in case of doubt”he would prefer to use cryoprecipitate for children.[953] Following Dr Hill’s attendance at the UKHCDO annual meeting in November 1979, where Dr Craske gave a presentation on the work of the Hepatitis Working Party,[954] he reported back to the December 1979 meeting of the West Midlands Working Party that: “the Hepatitis Working Party had reported that Commercial Factor VIII carried the risk of hepatitis, and he was concerned that some children at the Childrens Hospital had become hepatitis carriers”.[955]
Dr Brian Colvin was the director of the haemophilia centre at The London (later Royal London) Hospital from 1977. By 1975 he “was aware that there was at least a possibility of chronic liver disease in haemophilia.”[956] In relation to NANBH “there was the hope that this wouldn’t be a big problem, and that hope clearly was misplaced ... there was an unjustified but justifiable, if you like, feeling that it would be all right.”[957] Dr Craske’s August 1975 paper was very important: “a watershed moment, after which it was known that there was quite a significant problem for the future, at least in terms of numbers ... We didn’t know what was going to happen next but I think we knew that it was going to happen to a lot of people.”[958]
Dr Colvin remembered reading the 1978 Sheffield/Preston paper and accepted that this would suggest clinicians could no longer work on the assumption that the absence of overt or acute signs was a reliable indicator that a person would not develop NANBH.[959] Dr Kernoff’s April 1979 letter in which he described NANBH as a “serious disease with long-term consequences” represented Dr Colvin’s understanding by that time.[960]
Dr Colvin attended (as did Dr Kernoff) meetings of the North East Thames Region (“NETR”) Association of Haematologists’ Haemophilia Working Party – a group of consultants from different hospitals who met regularly and discussed a range of issues. In May 1979 Drs Colvin and Kernoff authored guidelines on “the screening and investigation of hepatic disease in patient [sic] with congenital coagulation disorders”, advocating “closer monitoring of patients than has hitherto been the case”.[961] The guidelines advised regular liver function tests and Hepatitis B surface antigen (“HBsAg”) checks and outlined proposals for research. The Haemophilia Working Party met in December 1979 and discussed the preliminary findings from the Regional Study of Hepatitis. Up to 70% of patients with severe haemophilia had abnormal liver function tests, with a wide spectrum of histological abnormalities. All types of concentrate were said to constitute a risk with “as yet, no evidence that imported Concentrates are more dangerous”.[962] Notwithstanding the recognition of risk, the minutes of the meeting recorded no consideration of how that risk might be reduced, or whether different treatment policies should be adopted.
The home treatment programme at The Royal London started with cryoprecipitate but changed to Factor 8 concentrates – NHS if available but otherwise commercial. Dr Colvin would try to keep very small children on cryoprecipitate but otherwise children would be treated with concentrates.[963]
Dr Colvin accepted that by 1979 the view within the NETR was that cryoprecipitate was the past, concentrates the present and future: “we did give up on cryoprecipitate”.[964] No analysis of the relative risks of cryoprecipitate and factor concentrates was undertaken and they did not expressly consider the possibility of returning to cryoprecipitate use in a big way. Cryoprecipitate was “old hat”. Other than through the continuation of the policy of using mostly cryoprecipitate for young children, the approach to treating patients did not change at all in the period 1977-1983 to reflect the risk of hepatitis.[965]
The haemophilia centre at Leeds was based at St James’s University Hospital. The director from around 1970 was Dr Layinka Swinburne; she was joined by Dr Bernard McVerry in 1985.[966] Leeds was a relatively large centre and by 1977 was using a substantial volume of commercial concentrates.[967] By 1978 little cryoprecipitate was in use[968] and the 1979 return recorded the use of no cryoprecipitate at all.[969] There does not appear to have been any system of batch dedication, nor any other evidence of a risk reduction or minimisation strategy.[970] Dr Swinburne was a regular attender of UKHCDO meetings, including the 1971 and 1972 meetings at which Dr Biggs’ work on jaundice was discussed,[971] the 1974 meeting at which Dr Craske reported on the hepatitis outbreak in Bournemouth,[972] the 1975 meeting at which there was a discussion about hepatitis, liver function tests and pool sizes,[973] the 1977 meeting at which Dr Craske reported on his study of hepatitis in patients receiving Hemofil,[974] and the 1979 meeting at which Dr Craske presented the report of the Hepatitis Working Party.[975]
Six features emerge from examination of the treatment policies and practices towards patients with Haemophilia A in the 1970s. The first is the increasing use of concentrates (particularly commercial). The second is the insufficiency of NHS concentrates outside Scotland: many clinicians complained of a “shortfall” in what was available from BPL.[976] The third is the decreasing use of cryoprecipitate. The fourth is the fact that there was no or little express consideration given to safety. Rather the approach was treatment with the latest, most convenient product, with no self-reflection as to whether that was the right course. The fifth is the growth in using greater quantities of Factor 8 therapies, especially for home treatment, associated in particular with commercial concentrates, but also for some prophylaxis. The sixth is the limited deployment of risk mitigation or reduction measures: for example, DDAVP should have been widely used from 1978 but was not; some centres attempted batch dedication policies, but others did not. There is no record of doctors choosing one concentrate over another because the pool size from which it was manufactured was said to be smaller. Underpinning it all was an assumption that hepatitis was “an inconvenience, but essentially harmless”: an assumption “of the kind that doctors should not make”.[977] This was despite the considerable evidence, arising in respect of serum hepatitis from the end of the Second World War, that it could not only be dangerous in its acute phase[978] but in a number of cases could become chronic and lead to cirrhosis, liver failure, and liver cancer. Though Hepatitis B had been identified by the start of the 1970s, clinicians knew it continued to be transmitted through concentrates; once it became clear that a large part of serum hepatitis was NANBH, treating clinicians should not have assumed NANBH to be a harmless part. They knew that was not the case with Hepatitis B; they also had a number of warnings from leading experts that the long-term consequences of NANBH could not be assumed to be benign. Yet that was the assumption most made.
An elementary principle is that if a certain process or procedure carries risks with it then reasonable steps should be taken to eliminate those risks or, if they cannot be eliminated, to reduce them. Scant regard is paid to this principle if no attempt is made to take any such step.
In September 1980 a symposium entitled Unresolved Problems in Haemophilia was held at the Royal College of Physicians and Surgeons in Glasgow.[979] The symposium immediately followed the annual meeting of haemophilia centre directors on 30 September 1980 and it is reasonable to assume that most directors attending the annual meeting would also have attended the symposium.
At the reference centre directors’ meeting a week or so before, on 22 September, hepatitis had, yet again, been a subject for discussion. Dr Craske had reported a poor response from directors to his request for information about patients thought to have developed chronic hepatitis and he proposed to ask directors at the annual meeting in Glasgow to send in as soon as possible information about all patients who had shown abnormal liver function test results for six months or more. Dr Craske explained that he was awaiting the results of biopsy studies being undertaken in Sheffield and at the Royal Free, and it was recorded that there were other studies underway or anticipated in Oxford and Manchester.[980] There was also a discussion on freeze-dried cryoprecipitate, which led to a query from Dr Savidge as to what the policy was for the use of cryoprecipitate for home therapy: Professor Bloom said that it was a matter for individual directors to decide whilst also referring to the minutes of a meeting in January 1978 where the reference centre directors had agreed that Factor 8 concentrates were preferred for home therapy.[981]
The haemophilia centre directors’ annual meeting on 30 September 1980 included a discussion about “the increasingly inadequate supplies of NHS factor VIII concentrate”[982] and included an update from Dr Craske on behalf of the Hepatitis Working Party. The minutes include the following discussion:
“Large pool concentrates appeared to give a higher risk of hepatitis than small pooled concentrates and Dr Craske felt that increased usage of small pooled concentrates would help to reduce the incidence of hepatitis in the haemophilic population. First-time exposure to large pooled factor VIII concentrate resulted in many cases of hepatitis, especially in von Willebrand’s disease patients. Professor Bloom wondered whether cryoprecipitate would be a better product to use for mild haemophiliacs and von Willebrand’s disease but pointed out that there was a problem over the amount of factor VIII in these materials. Dr Creaske [sic] agreed and he said that the NHS product was certainly better than the Commercial products because of the screening of the blood donors and the regular donor panels which were used in the UK. The screening procedure used for donors of plasma used to make Commercial factor VIII is radioimmunoassay but because of the unstable population and the poor social background, it is more likely that there will be a higher incidence of carriers of the hepatitis virus than in the U.K. volunteer blood donors.”[983]
The one and a half day symposium organised by Dr Forbes and the Royal College of Physicians and Surgeons of Glasgow and sponsored by Travenol followed.[984] The first part of the symposium was devoted to the subject of Liver Disease in Haemophilia and in their foreword to the subsequent publication of the proceedings Drs Forbes and Lowe observed that “a major section of these proceedings is devoted to the investigation of liver disease in haemophilia – an area which offers unique opportunities for both basic, applied and clinical research”.[985]
The opening remarks, from Professor Roddy MacSween,[986] included the following:
“It was anticipated that the screening of blood donors for HBsAg would substantially reduce the incidence of post-transfusion hepatitis. However, this was not the course of events and, while some reduction did occur, post-transfusion hepatitis remained and remains a significant clinical hazard. It is now established that there are other transmissible agents capable of causing post-transfusion hepatitis, and there is good evidence that more than one virus is involved in what has become defined as non-A, non-B hepatitis ... Of particular interest has been the discovery that non-A, non-B hepatitis is a hazard in haemophilia patients and, as you will hear this afternoon, has been particularly associated with the use of the various concentrates with which these patients are now managed. Thus, while the use of these concentrates has represented a major advance in the therapy of haemophilia, it is unfortunate for the patients that this may be accompanied by an increased risk of acute and, possibly, chronic liver disease.”[987]
Dr Craske gave the first presentation, on The epidemiology of Factor VIII and IX associated hepatitis in the UK, in which he noted that despite the introduction of radioimmunoassay (“RIA”) screening in 1975, a significant amount of both symptomatic and symptomless Hepatitis B “still occurs associated with commercial and NHS Factor VIII transfusions”. Whilst stating that most cases of non-A non-B Hepatitis were mild illnesses, Dr Craske also observed that:
“About 25%-40% of haemophiliacs on regular Factor VIII therapy have persistently elevated serum aminotransferase levels for periods of at least one year. Most of these patients are symptomless. However, a few have clinical features suggestive of chronic liver disease, but the ethical problems associated with the indications for liver biopsy have meant that few patients have so far undergone this procedure. About 40 patients have undergone biopsy in the UK and approximately 50% of these have histological evidence of chronic persistent hepatitis ... Other patients showed evidence of chronic liver disease or cirrhosis ... Most of the patients in this group are children or young adults, though the age range at Oxford is 6-70 years. It seems likely that some patients will develop severe chronic liver disease over the next 10 years.”
Dr Craske’s presentation ended:“There is, therefore, a high risk from the use of Factor VIII or IX concentrate that the patient will contract non-A, non-B hepatitis, and a 20-30% chance of resultant chronic hepatitis, together with a smaller risk of hepatitis B.”[988]
A further presentation on Clinical, immunological and histological aspects of non-A, non-B hepatitis in haemophiliacs by Dr Thomas, Dr May Bamber and Dr Kernoff[989] summarised data from a study undertaken at the Royal Free Hospital:
“The data from our prospective study suggests that patients receiving Factor VIII concentrates (commercial and NHS) for the first time run a high risk of developing acute NANB hepatitis. The incidence of chronicity in our study was higher than that observed by others. Six of our patients had persistently elevated transaminases at 6 months ... The high attack rate with a high incidence of chronicity suggests that the majority of the haemophiliac population exposed to Factor VIII concentrates will develop chronic hepatitis, at least as regards the definition of transaminase abnormalities persisting for longer than 6 months ... In a larger series of biopsies in this patient group we found 5 of 17 patients (42%) biopsied during the chronic phase to have chronic active hepatitis. Although the prognosis of this lesion following NANB hepatitis is unknown, it should be noted that a similar lesion associated with chronic hepatitis B virus infection is progressive and, in a proportion of patients, ultimately results in the development of cirrhosis and its attendant complications.”
In the discussion which followed Dr Thomas explained that none of their patients had cirrhosis:
“but then, if we are to believe that this illness at the most has been going on since 1974 when the commercial concentrates were first introduced, then this period is short in the course of the disease. There are some indications that these patients may have lesions which will turn to fibrosis or cirrhosis ... It is really now a question of how long it takes. Just because we have not seen it in this six-year period, it does not mean that it will not happen. I think the thinking is that it takes ten or twenty years, or even thirty years for these lesions to progress. I think we have to realise that these are young patients, with many years ahead, when we are considering the significance of these lesions.”[990]
Professor Peter Scheuer[991] provided the symposium with a short account of biopsies that had been undertaken: two showed acute hepatitis; a third showed an excessive portal and periportal inflammatory reaction suggesting possible transition to chronicity; two more showed chronic active hepatitis; and the last showed chronic persistent hepatitis.
A talk by Dr Preston, Dr Triger and Dr Underwood[992] explained that they had now examined liver biopsies from 19 patients with haemophilia, including 5 children whose ages ranged from two to ten years, and 1 patient with von Willebrand disorder. “The biopsy findings ranged from chronic persistent hepatitis, present in the majority of our cases, to severe chronic active (aggressive) hepatitis with evolving or established cirrhosis.”[993] Dr Thomas, responding to a question from Professor Bloom about treatments for hepatitis, observed that “One can predict that there will be problems in the future” and added later, by reference to patients with haemophilia, that “The prediction is that it will be a more significant progressive illness, and I think they will develop fibrosis. Indeed, Dr Triger’s studies have shown that a significant proportion have cirrhosis.” Dr Jones (presumably Dr Peter Jones) asked the speakers to “try to put this into perspective”, stating that“Patients in the UK have now been chronically transfused with commercial concentrate for over 7 years, and in the US and Germany for considerably longer at considerably higher doses. What we do not seem to have seen is chronic morbidity or increasing mortality from liver disease.” In responding, Dr Triger emphasised that “We are dealing with chronic liver disease, in which 5 to 7 years is a very short time – as we all know. 10 to 20 years may be a long time, but we have been looking at liver biopsies of children under the age of 10 years, and what we are concerned with is what is likely to happen to them when they should be fit, healthy 25 year olds ... I think we are just building up trouble.” Dr Thomas agreed: “it is in 10 years time that we shall see the problems. Bearing in mind the proportion of the patients that are infected, or have persistent abnormal liver function tests, anything from 60 to 80 per cent, it will be an enormous problem when it happens.”[994]
Sadly, Dr Triger and Dr Thomas were absolutely right.
Professor Thomas in his oral evidence to the Inquiry agreed with this description of his message to the symposium: that the expectation was that “there would be problems with chronic active hepatitis, fibrosis and cirrhosis in the future for this cohort of patients ... the presence of chronic active hepatitis was a bad prognostic sign ... as with hepatitis B, this develops over decades rather than months or years or small numbers of years”.[995]
Dr Mark Winter, in his oral evidence to the Inquiry, rightly described the 1978 Sheffield study as showing NANBH to be a “really serious evolving clinical problem”.[996] There had been, as he suggested, “a sort of unwillingness to think it might be a problem because this new treatment had brought such spectacular benefits and because the patients were so enthusiastic about it ... people were reluctant ... to say this is a serious problem”.[997] The Preston paper was indeed an “absolutely key moment, where any haemophilia doctor should have switched from a viewpoint [from] ‘they have probably got a mild form of the virus’ to ‘I’m very concerned’”;[998] it was “one of the great sea change moments”.[999] But for any haemophilia clinician working in that capacity in 1980 who had not picked up on the significance of the Sheffield study, the Glasgow symposium in September 1980 was another “absolutely key moment” and should have driven home the message that NANBH could not be dismissed as “benign” or “mild” or as a risk that did not need to be taken seriously.
Yet treatment with factor concentrates continued unabated throughout the early 1980s. The Hepatitis Working Party continued to meet and discuss its various studies;[1000] the reference centre directors turned their attention to concerns about the new concentrates said to be hepatitis-free or hepatitis-reduced[1001] and noted that the annual returns for 1980 showed that the amount of Factor 8 concentrates used had again increased, especially commercial materials;[1002] the haemophilia centre directors met again in the autumn of 1981 and received Dr Craske’s report on behalf of the Hepatitis Working Party for 1980-81 with its recommendations that the surveillance should continue, as should further studies.[1003] But for most centres little or nothing changed.
The tables below show, from the annual returns for 1980-1982, the use of concentrates and cryoprecipitate in the reference centres and in some of the other sizeable centres.[1004] The figures shown relate to treatment for Haemophilia A.
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 4,138,918 | 616,785 | 3,522,133 | 3,629 |
| 1981 | 4,653,526 | 1,422,075 | 3,231,451 | 136,820 |
| 1982 | 4,582,052 | 977,610 | 3,604,442 | 0 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 3,996,453 | 602,430 | 3,394,023 | 247,900 |
| 1981 | 3,973,175 | 1,358,905 | 2,614,270 | 177,525 |
| 1982 | 5,897,835 | 1,374,996 | 4,522,839 | 142,240 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 1,278,571 | 245,271 | 1,033,300 | 399,210 |
| 1981 | 1,632,468 | 500,201 | 1,132,267 | 330,870 |
| 1982 | 1,919,645 | 602,930 | 1,316,715 | 178,640 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 1,396,451 | 120,672 | 1,275,779 | 71,370 |
| 1981 | 2,278,476 | 122,049 | 2,156,427 | 160,100 |
| 1982 | 2,190,252 | 12,960 | 2,177,292 | 77,122 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
| 1980 | 1,602,158 | 1,490,449 | 111,709 | 108,550 |
| 1981 | 1,396,324 | 1,246,155 | 150,169 | 20,300 |
| 1982 | 2,002,544 | 1,977,048 | 25,496 | 17,350 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 1,808,730 | 1,644,730 | 164,000 | 1,190,000 |
| 1981 | 1,282,148 | 840,130 | 442,018 | 680,470 |
| 1982 | 1,581,300 | 1,574,000 | 7,300 | 528,000 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 942,627 | 141,775 | 800,852 | 4,690 |
| 1981 | 850,076 | 419,213 | 430,863 | 219 bags |
| 1982 | 964,010 | 413,220 | 550,790 | 5,250 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 2,033,137 | 204,982 | 1,828,155 | 17,200 |
| 1981 | 2,653,655 | 335,712 | 2,317,943 | 1,800 |
| 1982 | 3,107,716 | 181,875 | 2,925,841 | 2,300 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 1,510,834 | 644,356 | 866,478 | 725,040 |
| 1981 | 2,558,945 | 1,368,345 | 1,190,600 | 407,760 |
| 1982 | 2,922,861 | 850,475 | 2,072,386 | 479,762 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 4,979,538 | 1,652,045 | 3,327,493 | 0 |
| 1981 | 4,920,216 | 1,616,573 | 3,303,643 | 0 |
| 1982 | 6,188,662 | 1,591,620 | 4,597,042 | 0 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 1,503,969 | 334,669 | 1,169,300 | 14,640 |
| 1981 | 2,317,441 | 1,184,305 | 1,133,136 | 44,720 |
| 1982 | 2,338,715 | 868,910 | 1,469,805 | 100,560 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
| 1980 | 723,873 | 293,200 | 430,673 | 250,400 |
| 1981 | 997,387 | 473,020 | 524,367 | 261,800 |
| 1982 | 992,535 | 650,750 | 341,785 | 239,000 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 2,203,590 | 356,635 | 1,846,955 | 0 |
| 1981 | 2,437,273 | 644,820 | 1,792,453 | 0 |
| 1982 | 2,762,230 | 404,955 | 2,357,275 | 0 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 1,790,691 | 80,605 | 1,710,086 | 1,010,000 |
| 1981 | 2,579,240 | 368,820 | 2,210,420 | 331,100 |
| 1982 | 3,860,474 | 1,156,340 | 2,704,134 | 29,260 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 1,000,683 | 366,177 | 634,506 | 375,000 |
| 1981 | 1,407,370 | 731,382 | 675,988 | 1,774 packs |
| 1982 | 1,298,545 | 776,947 | 521,598 | 84,350 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 914,356 | 193,553 | 720,803 | 13,435 bags |
| 1981 | 884,854 | 320,966 | 563,888 | 925,330 |
| 1982 | 1,003,198 | 263,608 | 739,590 | 570,290 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 374,928 | 175,937 | 198,991 | 1,332 bags |
| 1981 | 414,227 | 273,846 | 140,381 | 990 packs |
| 1982 | 356,730 | 319,540 | 37,190 | 36,050 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 548,145 | 292,790 | 255,355 | 0 |
| 1981 | 604,603 | 463,450 | 141,153 | 630 |
| 1982 | 946,921 | 424,000 | 522,921 | 0 |
| Year | Total NHS and Commercial F8 | NHS F8 | Commercial F8 | Cryoprecipitate |
|---|---|---|---|---|
| 1980 | 165,033 | 63,305 | 101,728 | 0 |
| 1981 | 243,004 | 109,900 | 133,104 | 0 |
| 1982 | 177,700 | 60,100 | 117,600 | 0 |
The charts below show the use of cryoprecipitate, NHS Factor 8 and commercial Factor 8 as proportions of total treatment in 1980, 1981 and 1982 for the centres in the tables.
The Glasgow symposium, and what ought on any view to have been understood to be the risks of transmission of NANBH and the potentially serious nature of NANBH, did not lead to any noticeable difference of approach to treatment, or even of any consideration of whether a changed approach was warranted. Nor was there any consideration or discussion about the position of patients and the information that should be provided to them about the risks of treatment.
In October 1986 Dr Colvin wrote to David Watters at the Haemophilia Society in the following terms:
“in 1976 it was widely believed that commercial factor VIII concentrate was more unsafe with respect to hepatitis than British concentrate although later studies showed this was not necessarily the case ... It was also realised that while importation of factor VIII concentrate continued the potential for the introduction of even more serious infections in the UK haemophilia population existed and that a disaster might occur. That fear was eventually realised when Human Immunodeficiency Virus (HIV) infection, which is the cause of AIDS, was transmitted to patients with haemophilia.” [1024]
A similar idea was expressed by Dr Mark Winter in his oral evidence:
“A central mantra for all the time that I was working was, it wasn’t the virus you knew about; it was the virus that you didn’t know about. If you looked at the history of blood products, every few years ... there would be a new virus apparent and, most importantly, it would then become apparent ... that it had been there for some time ... all blood and blood products are risky because, you know, how do you know what we’re about to discover in three years?”[1025]
It might be thought, therefore, that haemophilia clinicians would and should be in a position to recognise and react promptly to the threat of a new virus. That was not to be the case.
The first mention of AIDS in the meetings of haemophilia centre directors came in early autumn 1982 when it was raised, almost as an afterthought, by Professor Bloom at the reference centre directors’ meeting on 6 September.[1026] Following discussion of the 1981 annual returns[1027] and estimated requirements for Factor 8,[1028] the meeting turned to consider hepatitis, with Dr Craske updating those present about the study being conducted in collaboration with the Oxford Haemophilia Centre on the use of commercial and NHS concentrate for first time or seldom treated patients (9 out of 28 patients who had been entered into the study had developed NANBH). Dr Wensley felt it important to point out that Hepatitis B had not disappeared (there had been two new cases in Manchester that year), and the Hepatitis Working Party was invited to give priority for the drawing up of guidelines for the use of “hepatitis-free” concentrates. Following discussion about the Hepatitis B vaccine, Professor Bloom wondered what value the giving of the vaccine was “when Non-A, Non-B hepatitis seemed to be the larger problem for the haemophilic patients”.[1029]
The minutes then record that: “Professor Bloom asked Dr Craske if he had any information about the acquired immune-deficiency syndrome following reports in the United States and the possible relationship with this syndrome of blood products and hepatitis. Dr Craske said that he would find out more about this and agreed to try to have some information available to the Haemophilia Centre Directors at the Manchester meeting.”[1030]
A week later, at the annual meeting of haemophilia centre directors on 13 September 1982, the minutes record that the reference centre directors had asked Dr Craske to look into the report from the US “mainly in homosexuals but including three haemophiliacs. It appeared that there was a remote possibility that commercial blood products had been involved.” Dr Craske asked directors to let him know if they had any cases of the syndrome and the Hepatitis Working Party was said to be considering the implications of the reports from the US.[1031]
The next meeting of the Hepatitis Working Party took place that same day. It was dominated by discussions about research projects.[1032] However, towards the end of their meeting the Working Party agreed that, as AIDS had similarities in its epidemiology to Hepatitis B, enquiries would be made by members of the Working Party to ascertain the likelihood of transmission of the disease by blood or blood products and a further meeting would be held when more information became available.[1033]
As set out elsewhere in this Report,[1034] possibly by March 1982, and certainly from July 1982 onward, it was known in the UK to both some clinicians and some within government that there was a real risk that blood, and blood products in particular, would transmit the cause of AIDS. That the reference centre directors and UKHCDO were, as at September 1982, only at the beginning of enquiries into this risk – enquiries that were effectively being delegated to Dr Craske – and that the minutes of the 13 September 1982 meeting could characterise the nature of the risk as being “a remote possibility” amounts to an inadequate response. No sense of urgency arose, as it should have done and on any reasonable view at that stage the risk of commercial blood products was more than a “remote possibility”.
No doubt as part of the process of enquiry that had been delegated to him, Dr Craske wrote to the Centers for Disease Control and Prevention (“CDC”) on 4 October 1982; he seems also to have received information from Dr Kernoff.[1035] On 8 October Dr Rizza wrote to Dr Craske explaining that he had spoken to a physician in the US: “Apparently the whole problem has caused quite a stir in the haemophilia world in the States so much so that one very senior physician has withdrawn his factor VIII concentrates from the accident room and insists on vetting the patients himself before any dose is given.” Dr Rizza felt that “the whole thing should be looked at urgently if only to clear the air and dispel some of the apprehension that has been stirred up”.[1036]
On 5 November 1982 Dr Craske prepared a paper about AIDS which described how between June 1981 and January 1982 the CDC had become aware of an increase in the occurrence of Kaposi’s sarcoma, pneumocystis pneumonia and other opportunistic infections. He reported that a considerable delay was noted between the occurrence of initial symptoms and diagnosis, that the signs and symptoms were in most cases insidious and non-specific in nature, and that the overall mortality rate was high. Recently seven cases had been reported in people with haemophilia, three of whom had no association with drugs or sexual promiscuity. Dr Craske described three theories that had been advanced. The first – the effect of drugs such as amyl nitrate – was swiftly discounted by him “as the disease has been described in patients who do not use the drug”. The second – the immunosuppressive effect of cytomegalovirus infection – was also said by Dr Craske to seem unlikely. The third theory was that “The association with sexual promiscuity, intravenous drug abuse and possibly the transfusion of commercial blood concentrates, together with evidence of clustering and a prodromal phase suggest an infectious agent with a similar epidemiology to that of hepatitis B, possibly specific for human T. cell populations.” It is abundantly clear that this was regarded as the most likely cause by Dr Craske.[1037]
Whilst the paper itself had been prepared for a meeting of the MRC Hepatitis Vaccine Working Group, Dr Craske sent a copy of it on 11 November 1982 to Dr Rizza and to Dr Ludlam, both members of the Hepatitis Working Party.[1038] Dr Craske’s letter to Drs Rizza and Ludlam explained that he had spoken to the CDC the previous week. The latest information was that five people with haemophilia had been identified with this syndrome, two of whom recently died. All the cases were without any of the factors that had been found in other patients (drug addiction, homosexual practices, treatment with immunosuppressive drugs). The hypothesis was said to be that one or two patients in the incubation period of the disease had donated plasma which had since been used to prepare concentrates. “The likelihood is, therefore, that other cases will be identified amongst severe haemophiliacs, though probably at a low prevalence.” The basis for the assertion that there would be a low prevalence of other cases is unclear. Dr Craske thought it necessary to have a meeting of the Hepatitis Working Party “to decide what further investigations need to be undertaken in the British haemophiliac population”.[1039]
On 22 November 1982 Dr Craske received further information by way of a letter from Dr Dale Lawrence of the CDC, which explained that “We are increasingly concerned that involvement of US Hemophilia - A patients with AIDS is based on (infected) plasma donorship by certain US residents who may have been experiencing subclinical or prodomal states of AIDS illness, but unaware of this state. However, we have no evidence as yet to indicate association among the 8 US hemophilia AIDS cases through common exposure to a Brand or lot.”[1040]
On 15 December 1982 a meeting took place at BPL, attended by, amongst others, Professor Bloom, Dr Rizza, Dr Gunson, Dr Craske, Dr Cash and Dr Lane. The purpose of the meeting was to discuss the implications for the haemophilia and blood transfusion services of the commercial introduction of “hepatitis-safe” factor concentrates. AIDS does not appear to have been discussed.[1041]
By 22 December 1982 the “latest information” from CDC, according to Dr Craske and communicated to Dr Lane, was that eight cases had occurred in Haemophilia A patients, all of whom had severe coagulation defects requiring regular treatment with Factor 8, and that two cases had occurred in people without haemophilia which might be related to whole blood transfusions between a year and eighteen months prior to the onset of the syndrome.[1042]
In December 1982, the Royal Free Hospital began to measure the ratio of T4 to T8 cells in patients with haemophilia. This was plainly a reaction to a perceived threat of AIDS taking hold, and implies a belief that whatever the cause of AIDS was it might be transmissible by blood or blood products.[1043]
On 7 January 1983 Alpha Pharmaceuticals issued a press release which said “The evidence suggests, although it does not absolutely prove, that a virus or other disease agent was transmitted to them [patients with haemophilia who had contracted AIDS] in the Factor VIII concentrate ... Surveys now being conducted by NHF [the National Hemophilia Foundation in the US] are producing other disquieting findings: AIDS has jumped from the seventh to the second most common cause of death in hemophiliacs within a year”.[1044]
The Hepatitis Working Party duly met on 19 January 1983. The focus of discussions was, again, the proposed prospective study of Factors 8 and 9 associated hepatitis. It was recorded that Professor Savidge was contemplating taking part in a trial of Travenol’s “hepatitis-reduced” Factor 8. However, Dr Craske also reviewed “developments in the field” relating to AIDS. So far ten cases of AIDS had occurred in Haemophilia A patients, of whom five had died. It “seemed possible that factor VIII or other blood products administered to these patients might be implicated”.[1045] The CDC’s AIDS Task Force was working on the hypothesis that there was an infective agent, which was supported by reports of three cases associated with whole blood or platelet transfusions. According to Dr Craske, US clinicians were keen for UK clinicians to collaborate in the reporting of cases of AIDS possibly associated with transfusions of US Factor 8. No cases so far had been found in Haemophilia B patients. Dr Craske suggested a retrospective survey where haemophilia centre directors would be asked to report patients with clinical features of AIDS-like disease. He agreed to draw up a form for the reporting of AIDS cases and to consider what further information would be needed in a retrospective study.[1046]
There was no suggestion in the Working Party’s meeting of any change of approach in relation to treatment, or any action to ensure the provision of information and advice to patients: rather the emphasis was, as had been trailed in Dr Craske’s 11 November letters to Drs Rizza and Ludlam, on “what further investigations need to be undertaken in the British haemophiliac population.”[1047] The unspoken assumption was that treatment would continue unchanged and unchecked. That the role of blood products was still described as something that “seemed possible”[1048] rather than being, by this stage, acknowledged as probable, may explain – but does not justify – this approach.
Three further events of significance took place in January 1983.[1049] The first, on 13 January, was the editorial in The New England Journal of Medicine, a publication that was widely read amongst clinicians in the UK, which stated that “The fact that haemophiliacs are at risk from AIDS is becoming clear”and advocated a revised approach to treatment.[1050] The second was the meeting at a Heathrow hotel on 24 January 1983, attended by a number of leading haemophilia centre directors,[1051] at which no one questioned that AIDS was likely to result from the transmission of an infectious agent and at which Dr Craske informed those present that the disease was intractable, had a high mortality rate and appeared to have a lengthy incubation period. Attention was expressly drawn to the recent New England Journal of Medicine, as well as to cases involving platelet transfusion including the San Francisco baby case.[1052] No one present at that meeting could have been left in any doubt as to the seriousness of the position.
The third significant event was the issue, on 11 January 1983,[1053] of a letter from Professor Bloom and Dr Rizza to all haemophilia centre directors which discussed the attempts that had been made by commercial companies to reduce the risk of hepatitis transmission through heat treatment. It emphasised the importance of finding out “by studies in human beings to what extent the infectivity of the various concentrates has been reduced”. Professor Bloom and Dr Rizza suggested that“The most clear cut way of doing this is by administering those concentrates to patients requiring treatment who have not been previously exposed to large pool concentrates,” and encouraged directors to avoid the use of such concentrates on a named patient basis, because this “might seriously hinder controlled studies in the future”.[1054] The importance of this letter is three-fold. First, what is remarkable about this letter is the complete absence of any reference to AIDS. There was no update, even though more was now known, or at least suspected, than had been shared at the last haemophilia centre directors’ meeting four months previously. Second, the letter illustrates that UKHCDO – through its chair and secretary – could give advice and information to haemophilia centre directors where it thought that was warranted. Third, this letter contemplated the administration of large pool concentrates to patients who had not previously received them at the very time when the emergence of AIDS should have led to the avoidance of treatment with concentrates for those who were previously untreated.
The reference centre directors met again on 14 February 1983.[1055] The minutes record a discussion about “The AIDS syndrome” in the following terms:
“Professor Bloom said that the Syndrome would be discussed at the Stockholm meeting of the World Federation of Haemophilia. Reports from the United States indicated that the incidence of AIDS was higher than at first thought and there was some concern that the haemophilic population of the U.K. who had received American concentrates might be at risk. Dr. Craske summarised the latest information from the United States and said that approximately 10 cases of AIDS were thought to have occurred in non-haemophiliacs in London, one in Glasgow and one in Manchester. Dr. Craske had drawn up a draft form for reporting of the cases. There was a lengthy discussion regarding the report form and which of the various documents which Dr. Craske had obtained with the United States should be circulated to the Haemophilia Centre Directors. It was agreed that Dr. Craske should draw up a new form for the reporting of cases and to arrange for this to be circulated to all Haemophilia Centre Directors with appropriate notes regarding the criteria on which the diagnosis should be based. It was suggested that Dr. Craske should invite an Immunologist to join the Hepatitis Working Party in view of the Working Party’s involvement with the AIDS Syndrome.”[1056]
There may have been a “lengthy discussion” about the form which would be circulated to haemophilia centre directors for the reporting of cases, but there was a complete absence of discussion about whether there should now be a different approach to treatment, or about what information should be provided to patients. This showed an unacceptably casual and blasé approach to the risk which treatment with blood products posed to patients.[1057]
Early March saw a meeting of the Haemostasis Club, a gathering at which clinicians were invited to present on topics of interest.[1058] On 8 March it was Professor Jeanne Luscher who talked about AIDS.[1059] She explained that the CDC postulated that AIDS was caused by a transmissible agent and that it shared some common properties with Hepatitis B (a long incubation period). She drew attention to the possibility of altered T4/T8 cell ratios. Recommendations from the US were set out: use cryoprecipitate or fresh frozen plasma for children under four, DDAVP wherever possible, avoid elective surgery, no longer obtain concentrate donations from high-risk areas and attempt to screen out high-risk groups, for example by the use of questionnaires. Dr John Lilleyman (Sheffield Children’s Hospital) was said to be looking at T4 and T8 cell ratios in children.[1060]
On 22 March 1983 Dr Craske wrote to all haemophilia centre directors inviting them to report possible cases of AIDS.[1061] A revised and updated version of his 5 November 1982 report was enclosed with the letter. An infectious agent being the most likely cause, the report still used the language of possibility rather than probability, suggesting that “it is possible that such an agent might be present in the plasma pools used to prepare commercial factor VIII and IX concentrate manufactured from donor plasma collected in the U.S.A.”[1062] Directors were provided with guidance in identifying possible cases of AIDS[1063] and a form for the reporting of such cases,[1064] but no advice or guidance about the approach to treatment or the provision of information to patients.
The reference centre directors did not meet again until 13 May 1983, when there was a “special meeting” to discuss AIDS.[1065] But in the meantime, whilst treatment continued as normal, a young man with haemophilia in Wales developed symptoms of AIDS.
Kevin Slater was 20 years old when his AIDS symptoms were first identified and just 22 years old when he died in 1985.[1066] He was suspected of suffering from AIDS in March 1983, following a visit to University Hospital Wales. Professor Bloom was aware of his case and told the audience at a 22 April 1983 Haemophilia Society meeting that one of his patients “may have a mild form”of the syndrome.[1067] The factual basis for Professor Bloom’s conclusion that Kevin had a “mild form” of AIDS is unclear.
Kevin returned to the hospital on 25 April 1983, when he was admitted as an in-patient. The following day, Professor Bloom completed a UKHCDO AIDS surveillance form in relation to Kevin.[1068] Having identified which diagnostic criteria were met and when symptoms first emerged, he wrote that Kevin’s was a “probable”case of AIDS.[1069]
Around 6 May 1983, the Communicable Disease Surveillance Centre (“CDSC”) published a weekly report identifying Kevin’s case (without naming him) and observing that “This is the first report of AIDS in a patient with haemophilia in the United Kingdom known to CDSC.”[1070] Dr Spence Galbraith, director of the CDSC, notified the DHSS by telephone of this development on 6 May.[1071]
A week later the reference centre directors held their special meeting. Unusually, Dr Diana Walford of the DHSS was invited to attend: ordinarily she only attended the annual meetings. It was chaired by Professor Bloom and attended by Dr Craske, Dr Hamilton, Dr Kernoff, Dr Ludlam, Dr Savidge, Dr Preston, Dr Delamore and Dr Rizza.
The minutes are short and worth setting out in full:
“Professor Bloom briefly outlined the background to the meeting and its purpose. The recent publicity in the press, radio and television about the problem of acquired immuno deficiency syndrome (AIDS) had caused considerable anxiety to haemophiliacs and their medical attendants as well as to the Department of Health. There was clearly a need for Haemophilia Centre Directors to discuss what should be done with regard to the surveillance and reporting of suspected cases and management of patients. To date in the United Kingdom one haemophiliac is suspected of suffering from AIDS. In London there are reported to be 10 cases of confirmed AIDS in homosexual males. Concern was expressed about the definition of AIDS. It was felt that there might be many individuals with evidence of impaired cell-mediated immunity but only a very small number of these might progress to a full blown picture of the condition. It is important that such individuals are not classified as suffering from AIDS. It was accepted that because of our lack of knowledge of the nature of AIDS, decisions about diagnosis and reporting of suspected cases would prove difficult. Nevertheless the criteria laid down by the Centres for Disease Control, Atlanta, Georgia, and in the form prepared by Dr. J. Craske for use at U.K. Haemophilia Centres, should be followed for diagnostic purposes. The importance of opportunistic infection as a diagnostic criterion was stressed. It was agreed that any patient who was suspected of suffering from AIDS should be reported immediately on the form provided and thereafter the clinical course of the patient would be followed and a definitive diagnosis attached if the patient developed intractable disease.
The steps to be taken should a patient develop the features of the full-blown condition were then discussed. It was agreed that there was insufficient information available from the U.S. experience to warrant changing the type of concentrate used in any particular patient. Moreover once the condition is fully developed it seems to be irreversible so that there would seem to be no clinical benefit to be gained by changing to another type of factor VIII.
With regard to general policy to be followed in the use of factor VIII concentrates, it was noted that many directors have up until now reserved a supply of National Health Service concentrates for children and mildly affected haemophiliacs[1072] and it was considered that it would be circumspect to continue with that policy. It was also agreed that there was, as yet, insufficient evidence to warrant restriction of the use of imported concentrates in other patients in view of the immense benefits of therapy. The situation shall be kept under constant review.” [1073]
The meeting concluded by noting that blood transfusion centre directors were due to meet to discuss the problem of donor screening in relation to AIDS.
There are a number of points to be made about the decisions taken – and not taken – at this meeting.
First, what was set out represented no change at all to existing treatment practices. There was no discussion about any measures such as: reverting to cryoprecipitate (even if only on a temporary basis); batch dedication; more conservative treatment; a cessation of or reduction in home treatment; a cessation of prophylactic treatment for those centres whose approach to treatment included an element of prophylaxis; or cancelling or postponing elective surgery.
Second, the evidence was said to be insufficient in view of the immense benefits of therapy. Underpinning that conclusion was an all-or-nothing assumption: the sense that a restriction on imports would lead to a complete (and long-term) cessation of therapy. That was by no means the only outcome.
Third, the decisions in the meeting were taken in ignorance of the paper which Dr Galbraith had sent to the DHSS on 9 May 1983.[1074] That paper should have been provided by the DHSS to the reference centre directors, whether in advance of the meeting or as soon as practicable thereafter.[1075] It was not. Nor did Professor Bloom tell the meeting that he had sought information about the present situation in the US from Dr Bruce Evatt of the CDC, who described to him how “The evolution of the epidemic is occurring with a frightening pace” and that there were now 13 confirmed cases in people with haemophilia in the US, 1 of whom had Haemophilia B, with 5 more highly suspect cases under investigation, and all of whom had received factor concentrates.[1076]
Fourth, there was no discussion at all about advising patients of the risks.
Finally, the minutes firmly state that the situation “shall be kept under constant review.” Yet there is no evidence of there being any such review, let alone constant review: as set out below, there was little if any reconsideration by the reference centre directors until December 1984.
The meeting was followed, six weeks later, by a letter of 24 June 1983 to all haemophilia centre directors from Professor Bloom and Dr Rizza.[1077] That it took six weeks for such a letter to be produced is redolent of the lack of urgency with which UKHCDO/the reference centre directors acted up until December 1984. The letter contained a material inaccuracy in its opening paragraph: it stated that “So far one possible case has been reported to our organisation.” That could only be a reference to Kevin Slater and Professor Bloom certainly knew by this time that it was not a possible case but a probable one: he himself had reported it in those terms to Dr Craske.
The letter continued:
“At the above mentioned meeting on May 13th the following general recommendations were agreed.
It was agreed that there is as yet insufficient evidence to warrant restriction of the use of imported concentrates in other patients in view of the immense benefits of therapy but the situation will be constantly reviewed.” [1078]
The letter then stated that following the meeting on 13 May, “the Licensing Authority was asked to consider any implications for us of the revised recommendations of the American Food and Drug Administration which were made on March 24th, 1983 to American plasma collecting agencies”.[1079] It is not entirely clear what this refers to, but it is likely to be a reference to the reference centre directors raising misgivings at their meeting about the potential “dumping” of US product in the UK after the Food and Drug Administration (“FDA”) in the US had recommended that products made from plasma from “high-risk” groups should no longer be produced. Professor Bloom is likely to have assumed that Dr Walford was taking the issue forward with the Medicines Division[1080] (as indeed this Report concludes she did, even though, in the result, nothing was done to stop “dumping” happening). The letter did not, however, refer to the prospect of “dumping” in any clearer way, but as Dr Colvin pointed out in his oral evidence to the Inquiry the letter “also implies ... that if patients on home treatment were on imported concentrates, they should remain on imported concentrates”[1081] and does not suggest that some of these may create a greater risk than others because of the date of manufacture or the practices of the manufacturer.
The letter continued by referring to two additional points drawn to the authors’ attention since the 13 May meeting. The first related to treatment for Haemophilia B, where it was said that the evidence to incriminate Factor 9 concentrates “is even less than with factor VIII and it seems logical to continue to use our normal supplies of NHS concentrate.”[1082] The phrase “even less than with factor VIII” can only be designed to cast doubt on the view that AIDS could be transmitted through use of Factor 8 – yet by mid 1983 no one could reasonably have been under any illusion. The second point concerned proposed trials of “hepatitis-reduced” Factor 8 concentrate: it was, the letter said, still important that the effectiveness of these concentrates vis-à-vis hepatitis “is subjected to formal clinical trials in mild haemophiliacs notwithstanding our general recommendations above”. Directors were urged not to use these concentrates “randomly on a ‘named patient’ basis”. Thus, the reference centre directors were simultaneously suggesting that it was circumspect to treat people with mild haemophilia with DDAVP or NHS concentrate, whilst happily contemplating the enrolment of such patients in clinical trials in which they would be exposed to imported concentrates. Furthermore, whilst recommendations 1 and 2 were plainly drafted with “clinical freedom” in mind, with everything being left to the discretion and judgement of directors, the reference centre directors at the same time urged directors not to use the “hepatitis-reduced” concentrates. Ironically the reference centre directors were willing to urge directors not to use products that might well be safer (at least in relation to hepatitis),[1083] but were unwilling to urge directors not to use products that were very likely if not certain to be unsafe.
The 24 June letter was, remarkably, the only advice issued by the reference centre directors/UKHCDO until December 1984. It was poor advice. It was also too little too late.[1084]
Viewed broadly, it suggested that treatment should continue as before, despite the risks of AIDS on top of those of hepatitis. The complacency which this suggests, and the absence of any practical advice to reduce the risk of these diseases being transmitted by the choice of therapy, represent a failure of leadership and a missed opportunity.
June 1983 was also the month in which the Council of Europe issued its recommendation to member states, recommendations which included avoiding, wherever possible, the use of coagulation factor concentrates prepared from large plasma pools and informing people with haemophilia of the potential health hazards of haemotherapy and the possibilities of minimising these risks.[1085] Professor Ludlam was unaware of the existence of this recommendation, and it appears that it did not come to the attention of the reference centre directors.[1086] As with Dr Galbraith’s letter, those who were aware of the Council of Europe recommendations – which would include the DHSS and Dr Gunson – ought to have ensured that they were shared with UKHCDO/the reference centre directors.
The Hepatitis Working Party’s next meeting was 14 September 1983,[1087] followed by a meeting of the reference centre directors on 19 September, with Dr Walford in attendance again “in view of the Department’s interest in AIDS.” It was now known that a patient with haemophilia had died from AIDS. A paper was presented by Dr Craske, updating the situation regarding AIDS. It was agreed that the patients who had received the same batches of NHS or commercial Factor 8 as the patient who died in Bristol should be followed up. Professor Bloom reported that Dr Galbraith, director of CDSC, had not heard about the Bristol case until after the patient’s death, and it was agreed that reporting to CDSC should be through Dr Craske after discussion with the director involved in patient management.[1088] There were, as Professor Tuddenham (who was one of the reference centre directors at the meeting) accepted, no substantive recommendations at all made about changes in policy or different ways of treating patients or providing information to patients.[1089]
The annual meeting of haemophilia centre directors took place on 17 October 1983. Dr Chisholm, the director of the haemophilia centre at Southampton, raised the problem of patients refusing to take up commercial Factor 8 concentrate because of the AIDS scare. She wondered in view of patients’ worry whether directors could revert to using cryoprecipitate for home therapy. Professor Bloom replied that “he felt that there was no need for patients to stop using the commercial concentrates because at present there was no proof that the commercial concentrates were the cause of AIDS”. Dr Chisholm pointed out a further problem in her region in getting large amounts of commercial concentrates whereas she could get unlimited amounts of cryoprecipitate, and other directors reported the same problem. After discussion it was “agreed that patients should not be encouraged to go over to cryoprecipitate for home therapy but should continue to receive the NHS or commercial concentrates in their usual way”.[1090]
Dr Craske presented the paper which had been pre-circulated to directors.[1091] He outlined his proposals for investigating UK cases of AIDS in people with haemophilia and proposed follow-up for three years of patients who had received “suspect batches of factor VIII”. There was some discussion of the two cases of AIDS in people with haemophilia in the UK and Dr Geoffrey Scott, director of the Bristol Centre, gave details about the case of the patient who had died. Dr Craske urged directors not to put the word AIDS on pathology request forms and said he could supply directors with a copy of the US recommendations about the handling of samples. It was agreed that he would send out details of his proposals as soon as possible.[1092]
It might be thought that the death of a patient from AIDS would have focused minds on the need for a change of approach to treatment, but it is apparent from the minutes that was not the case. It is astonishing that as at October 1983 Professor Bloom felt able to say in response to Dr Chisholm that there was “no proof”[1093] that commercial concentrates were the cause of AIDS,[1094] and astonishing that the directors as a whole agreed that patients should not be encouraged to switch to a treatment which was on any view substantially safer. Dr Colvin, in his oral evidence to the Inquiry, described Professor Bloom’s statement as “more wishful thinking”.[1095] It was that and more. It was an unsustainable and misleading position to promulgate in the autumn of 1983. It was tantamount to telling clinicians that they did not need to do anything. It is highly surprising that Professor Bloom was not challenged on this by his peers at the meeting.
Thus the position as at the end of 1983 was that far too little had been done by UKHCDO or the reference centre directors in response to the emergence of AIDS. The focus was on surveillance and research rather than on taking urgent steps to reduce the risk of transmission. The only guidance that had been provided – the 24 June letter – was woefully inadequate. The reference centre directors were apparently unaware of key pieces of information – Dr Galbraith’s paper and the Council of Europe recommendations – and thus their advice (such as it was) was issued in ignorance of them. The risks were assessed on the basis of the number of cases which had emerged, when the focus should have been on what might be already on the way. And the risks to people with bleeding disorders were consistently, and unjustifiably, downplayed.
1984 saw little by way of positive action by the reference centre directors or UKHCDO. Reference centre directors held their first meeting of the year on 13 February 1984. Dr Craske informed the meeting that there had been 21 cases of AIDS in patients with haemophilia, including 2 with Haemophilia B, and there was discussion about methods for reporting on possible AIDS cases and about Dr Craske’s draft protocol for a study. Professor Bloom reported to the meeting about a survey he had undertaken regarding the possible incidence of AIDS cases in Europe. He had sent out a questionnaire and received 132 replies from all over Europe; 11 cases of AIDS had been reported.[1096]
Despite the increase in the number of cases of AIDS, both in patients with haemophilia and generally,[1097] and despite being told that “One-third of the Centres [ie in Europe] had changed their treatment regimes for patients following the onset of the AIDS problem”,[1098] regrettably the reference centre directors gave no further thought to treatment policy or any risk reduction measures or to the issue of any further advice. If they did not consider it their role to do so, they should have asked the DHSS or the Chief Medical Officer to act.
Likewise, at their next meeting on 10 September 1984 the reference centre directors listened to a presentation from Dr Craske regarding the current situation: he referred to the article in The Lancet on 1 September and stated that a further 20 patients with AIDS-related symptoms had been notified to him.[1099] There was still no consideration of any need for a change to treatment.
The haemophilia centre directors’ annual meeting took place on 27 September 1984. Notably, a substantial part of the meeting focused on discussions about the designation of haemophilia centres (a subject on which the reference centre directors had apparently held several meetings specifically for the purpose of discussing the criteria for designation). A note of self-congratulation may be thought to appear in the minuted assertion that “The UK was recognised throughout the World as having the best organisation for the treatment of haemophilic patients.”[1100] AIDS, by contrast, appears to have merited a short discussion in which Dr Craske referred directors to his report on the current AIDS situation and invited them to give special attention to the work on HTLV-3, testing for which had been available since August.[1101] Yet again there was no recorded consideration or discussion of any change to treatment or practice. Yet by now it was generally accepted that Dr Robert Gallo had identified a virus causative of AIDS, which therefore made it as good as certain that blood products could transmit it.
It was not until 10 December 1984 – some two or more years after the risks of transmission of AIDS should have been apparent to all haemophilia clinicians – that the reference centre directors and others finally addressed the implications of, and for, treatment choices. A meeting took place at Elstree on that date, chaired by Professor Bloom and attended by the majority of reference centre directors, representatives from BPL (including Dr Lane, Dr Terence Snape and Dr James Smith), Dr Gunson, Dr Cash, Dr Craske, Dr Philip Mortimer (PHLS), Dr Richard Tedder and Dr Alison Smithies from the DHSS.[1102] The meeting was said by Professor Bloom to have been “precipitated” by “the resulting publicity surrounding the events in Newcastle and Australia, and the continuing work on HTLV III”.[1103]
Following discussions on the arrangements for testing patients and whether patients should be told of their test results,[1104] the meeting considered the use of heat-treated Factor 8 versus non-heat-treated product.[1105] A particular concern was cost, with Dr Cash urging that “the financial considerations be looked at seriously. The implications for the cost of treatment to Haemophilia were enormous for the small number of patients involved”, and Dr Lane adding that “the cost considerations spread to the NBTS, which was not just concerned with Haemophilia management”.[1106] Following discussion of the progress with heat treatment of NHS Factor 8, there was a debate about the best options for treatment, with the chair advising that he would issue guidelines following the meeting: “In summary, the first choice would be HT material followed by the judgement of the individual clinician.” Professor Bloom also suggested that “peripheral treatment centres”should return all unheated commercial material to the reference centres “for transfer back to the Company involved”, most companies having undertaken (according to the note) in writing to accept such material back.[1107]
Following the conclusion of the discussion, it was suggested by Dr Lane that the haemophilia directors present “be allowed to have a private meeting with only themselves present”.[1108] No record of this “private” meeting exists.
The “AIDS Advisory Document” dated 14 December 1984 which was prepared in light of the meeting noted that there were in the US over 6,000 cases of AIDS including 52 people with haemophilia and 102 cases in the UK with 3 reported in people with haemophilia, and recorded that“No doubt other cases are developing in the haemophiliac population.”[1109] The document gave options in “probable decreasing order of safety from AIDS for Haemophilia A”:
The recommendations were:
The Advisory Document suggested that in individual patients “there may need to be a choice. In general heated concentrate appears to be the recommendation of virologists consulted but individual Directors may wish to make up their own minds.” From 30 January 1985 a limited supply of BPL heated product was expected to be available, with preference being given to previously untreated patients and children and possibly to those willing to participate in clinical trials.[1112]
This was the first guidance issued by UKHCDO since the 24 June 1983 letter (which, as observed earlier, in reality contained little by way of actual guidance); as Dr Rizza acknowledged in his report for the HIV litigation, up to December 1984 “the recommendations set out in the letter of 24th June, 1983 were still being promoted”.[1113] The failure to hold such a meeting earlier, and to provide advice to haemophilia clinicians earlier, was both inexcusable and inexplicable.
It is not clear precisely when the AIDS Advisory Document was sent to haemophilia centre directors, but the minutes of the first meeting of the UKHCDO’s AIDS Group on 11 January 1985 recorded that it had been sent to all centres.[1114]
Professor Savidge, in his written evidence to the Archer Inquiry, suggested that in the period 1983 to 1985 UKHCDO received “little if any information concerning haemophilia treatment from the representative Professor Bloom regarding information from other more influential committees”.[1115] Professor Bloom’s role on other committees, and his relationship with the DHSS, is discussed elsewhere in the Report,[1116] but the criticism is a well-founded one. Professor Savidge was also – and rightly – critical of the lack of timeliness of the December 1984 advice.
One does not have to look far to see the dreadful consequences of this delayed advice. Dr Janet Shirley was the consultant haematologist at Frimley Park Hospital, an associate haemophilia centre with a small number of patients. She had been appointed to her post in February 1980, at which point her experience of bleeding disorders was two years as a senior registrar at St Thomas’.[1117] Dr Shirley was one of a number of haemophilia centre directors to be appointed as such with relatively little experience of treatment for bleeding disorders. Moreover, Frimley Park was an associate haemophilia centre (it was designated as such between 1980 and 1981), with a small number of patients,[1118] and much of Dr Shirley’s time was taken up with other haematology services, unrelated to treatment for haemophilia or von Willebrand disorder. These two factors – a relative lack of experience in treating haemophilia and other bleeding disorders and a small number of patients seen annually – were not uncommon and should have reinforced the importance of there being clear and up-to-date guidance from UKHCDO to all doctors who might be treating patients with bleeding disorders.[1119] Dr Shirley acknowledged the need to keep up-to-date with developments relating to bleeding disorders and their treatment, but emphasised that “you need to understand that we had to keep up-to-date with an awful lot of other haematological diseases. So our ability to be really up-to-date would not be as great as the clinicians at the main centres.”[1120]
Dr Shirley thought it unlikely that she would have seen the AIDS Advisory Document before Christmas 1984 and that the likelihood was that she would have read it in January 1985.[1121] She was not aware, as far as she could recall, of the Edinburgh infections which were reported in the press on 20 December.[1122] The fact that a cohort of patients in Scotland had been infected apparently as a result of treatment with the Scottish NHS product – which had been known at least since late October 1984 – should have been immediately notified to all directors but was not.
There was one patient infected with HIV in likelihood as a result of treatment administered at Frimley Park on 17 December 1984.[1123] He had mild haemophilia.[1124] He was treated with unheated NHS concentrates on several occasions; available records suggest that he received a Scottish product as well as BPL. Dr Shirley did not tell the patient of the possible risk of AIDS from concentrates and in hindsight accepted that she should have done.[1125] If she had been in receipt of the AIDS Advisory Document (ie of advice from UKHCDO) at the time of his treatment, the treatment would probably have been different: she would have attempted to obtain heated concentrate. Dr Shirley agreed that the reference centre directors should have done more to ensure that directors such as herself were better informed:
“I think, as far as I can remember, that December 1984 document was the first time that we were given any guidance on what product we should use in what type of patient, and I think if we had had that sort of guidance issued through the 1980s, it would have been – it would have been easier for consultants to know that they were giving the right treatment, and also, I think, it would have enabled consultants like myself to put pressure on the regional Blood Transfusion Services to give us certain types of product.”[1126]
Other clinicians spoke also of the lack of guidance.
“We were desperate for guidance ... for leadership, which I don’t think we ever got properly, either from the Government or UKHCDO or whatever”.[1127]
It is difficult to understand why UKHCDO and the reference centre directors were so painfully and dangerously slow to recognise and react to the risks of AIDS being transmitted to their patients. The reflection of Dr David Bevan,[1128] referring to the generation of clinicians who had experienced periods when treatment for haemophilia was of limited availability and effectiveness, was that “Their attitude and reactions were dominated by determination never to withhold treatment and never to run short – let alone out – of treatment.” He added that “The UKHCDO also took a position in many ways typical of British public health governance: Not to risk over-reaction, not to act prematurely, not to alarm the public, ‘the evidence is not yet conclusive’, ‘we don’t yet have proof.’” Taking all these things into account he thought that UKHCDO continued to hold a line well into 1983 that the evidence of an infectious cause of AIDS was inconclusive and that action would be premature “long after that position became obviously untenable.”[1129] It was “a kind of denial of the reality.”[1130]
It was wrong.
Haemophilia centre directors knew, or should have known, no later than the end of 1982 (and probably earlier), of the risks of transmission of AIDS by blood and blood products.[1131]
Those who gave oral evidence to the Inquiry largely accepted that.
Dr Stanley Dempsey, consultant haematologist at the Royal Belfast Hospital for Sick Children, told the Inquiry that from late 1982 he had “no major doubt” or “no real doubt” that AIDS was transmissible by blood or blood products “because any alternative theory didn’t really seem to hold water”[1132] but haemophilia clinicians “were not prepared to commit themselves totally and utterly to AIDS being – the idea of AIDS being related to transmission by blood products.” He described UKHCDO as not having come round fully to the idea that commercial concentrates were responsible for the emerging AIDS problem – there was “resistance among the haemophilia treaters about the significance of concentrate and the emerging AIDS problem”, some of which he absorbed.[1133]
Professor Ian Franklin, consultant haematologist at the Queen Elizabeth Hospital in Birmingham from September 1982, said that certainly by the time the San Francisco baby case was reported, it was “pretty clear” that AIDS was probably transmitted by blood and blood products.[1134]
Dr Colvin, consultant haematologist at the London Hospital since 1977, said that he would have read the Dr Jane Desforges editorial in The New England Journal of Medicine and attended the January meeting at the Heathrow hotel, and would therefore have by January 1983 been aware that there was a risk to people with haemophilia of AIDS and that the most likely route of transmission for them was blood products.[1135]
Dr Winter, a lecturer and honorary senior registrar at Guy’s Hospital until he took up a consultant and director post in Margate in December 1983, would have seen the Morbidity and Mortality Weekly Reports (“MMWR”) including that of 16 July 1982.[1136] All doctors would, he said, have been aware of the 1981 reports of gay patients with a new disease but initially it was not suggested that it was to do with blood or anything transmissible.[1137] Then came the reports of three patients with haemophilia with pneumocystis, followed by the report of the San Francisco baby who had a platelet transfusion from a donor who subsequently developed AIDS. “So in this period of six months, say, from July ‘82 to December ‘82, by the end of that period, as a haemophilia doctor, you would have to look at that data and say ... This is something which is in the blood. This must be a virus or something like that”.[1138] As Dr Winter stated to the Penrose Inquiry, by December other theories are no longer tenable and “Any clinician looking at this data would have to believe that AIDS was a transmissible disorder and that it could be transmitted by blood and by blood products. It was the only clinical interpretation of the data that was available.”[1139] Importantly, Dr Winter’s evidence recognised that by this point in time “there are two major problems with concentrate therapy”: non-A non-B Hepatitis (“the liver disease is much more significant than we thought”) and AIDS: “set against the extraordinary benefits of concentrate therapy, it’s really stressing the dangers of concentrate therapy.”[1140]
Put more colloquially by Dr Winter, “however many alarm bells a human being has, they should all have been ringing at this stage.”[1141] Yet as set out below it is clear that those alarm bells were not ringing for many, indeed most, haemophilia clinicians – or if they were, they did not lead to any substantial changes in treatment policies and practices.
They rang in June 1982 for Professor Ian Hann, haemophilia centre director of Yorkhill Children’s Hospital in Glasgow between January 1983 and August 1987. As, then, a junior doctor he attended an international symposium On Infections in the Immunocompromised Host held in Stirling. A paper presented to the conference spoke of “an alarming epidemic of an acquired immunodeficiency syndrome, AIDS, in certain cities in the US ... Nationwide, half of the patients have died ... Blood or body secretions would appear to be potential vehicles of infection”.[1142] To him, this was a bombshell, and he thought it might be relevant to people with haemophilia. He called it “part of the burgeoning knowledge that began to explode at that time”.[1143]
It is a pity it did not ring as clearly for more.
Some examples will serve to illustrate this but the picture is a broader one.
It is unclear when Dr Jones first gave active consideration to the risks to his patients at the Newcastle Haemophilia Centre. In a document which he produced in around 1990 he suggested that AIDS in haemophilia patients “was brought to our attention by Professor Bloom at a meeting of the Haemophilia Reference Centre Directors in September 1982 when Dr. John Craske was to look at the question of British haemophiliacs being involved.”[1144] It is unclear whether he undertook any further enquiries himself or passively awaited the outcome of Dr Craske’s investigations.[1145] Newcastle was represented at the Heathrow hotel meeting in January 1983 by Dr Hamilton, Dr Jones’ co-director, who no doubt shared what was discussed with Dr Jones.[1146] However, two documents suggest that Dr Jones did not take the risk of AIDS as seriously as he should have done at this stage.[1147] First, in his letter of complaint to the Press Council in early May 1983, criticising The Mail on Sunday’s coverage of the AIDS crisis under the headline “Hospitals using killer blood”, Dr Jones said that“there is no proof that a virus even exists as a cause of the acquired immune deficiency syndrome” and no proof that any transmissible agent had been imported from the US.[1148] Secondly, in late May 1983, Dr Jones sent a circular letter to doctors in the Northern Region regarding “AIDS and Haemophilia” which substantially downplayed the risks.[1149]
In an editorial in The Lancet in April 1983 Dr Jones rejected the need for a change in treatment policy partly because the emergence of HIV/AIDS “in a few haemophiliacs does not necessarily reflect the tip of an iceberg”.[1150] There is nothing to suggest that his position subsequently changed. He did not make any switch to cryoprecipitate (even on a temporary basis or for children older than four or six who had graduated to factor products).[1151] Dr Jones was perceived by his peers to be committed to continuing to use factor concentrates at this time.[1152] In a memo written by Dr Frank Boulton to Dr Brian McClelland on 30 May 1983, Dr Boulton described a recent conversation with Dr Jones in which the latter “claimed that there is a lot of doubt about the diagnosis of all the AIDS cases in the UK, and in particular the haemophiliacs”; Dr Boulton felt that Dr Jones was “still being somewhat less than cautious” with regard to his attitude towards the risk of AIDS.[1153] Dr Collins, at the regional transfusion centre, had to write to Dr Jones in August 1983 to remind him that there was a large supply of BPL concentrate awaiting use at the regional transfusion centre.[1154] Commercial concentrates continued to be the mainstay of treatment in 1983 and 1984.[1155]
In short, there were no significant changes in approach to treatment at the Newcastle Centre in response to the risk of AIDS until the introduction of heat-treated concentrates in December 1984.[1156]
Dr Jones formed the view in the course of November 1984 that there should be a change to heat-treated Factor 8 (in other words in advance of the meeting at BPL on 10 December 1984) and took steps to secure the regional health authority’s agreement to that change.[1157] However, he did not take steps to recall existing unheated product from patients: instead they were told to use up their present stocks and that the switch would be made when they came back for new supplies for their home therapy.[1158] This was despite the fact that he had checked with representatives of the three companies supplying concentrates to the Centre who had all agreed to take back present stocks of non-heat-treated material without any financial consequences to the Health Authority.[1159]
The number of patients of the Newcastle Centre infected with HIV was high. Terence McStay, the second person with haemophilia to die of AIDS in the UK, was a patient at the Newcastle Centre, although he returned to his home in Glasgow shortly after he was diagnosed, and died on 3 November 1984.[1160] A paper published in The British Medical Journal in 1985 stated that out of 99 Newcastle patients with severe Haemophilia A, 76 were HIV positive.[1161] All except one of them had received commercial Factor 8 products at some time. Of the 76 infected patients, 30 were suffering from AIDS-related complex or lymphadenopathy. Three had died from AIDS. Three partners of seropositive patients also tested positive.[1162]
There were no changes in approach to treatment at the QEH[1163] in response to the risk of AIDS prior to December 1984.[1164] Having regard to the May 1983 Haemophilia Society publication[1165] and the October 1983 UKHCDO meeting,[1166] the advice was essentially to “carry on” and that was what Professor Franklin was guided by.[1167]
In March 1984 Professor Franklin wrote to Dr Fereydoun Ala at the regional transfusion centre outlining prescribing policy at the time. The Inquiry does not have that letter, but has a description of it in a later letter from April 1991:
“there had been a meeting of the Haemophilia Centre Directors in which it was considered advisable that patients remain on the Factor VIII product that they had been regularly using. Therefore it did not appear unreasonable at that time to propose that patients who had been using Armour for several years should continue to do so. There was never at any time sufficient NHS Factor VIII available to treat all patients and the decision of Dr Hill and myself was that patients should receive a regular supply of one or other product and not a mixture of both.”[1168]
At a meeting on 27 June 1983 of the West Midlands Working Party the regional transfusion centre advised the meeting through a letter from Dr Ala that cryoprecipitate was “probably a safer product than Factor VIII concentrate in respect of transmission of”AIDS.[1169] No action appears to have been taken in response to this. Professor Franklin’s evidence was that “I think ... in Birmingham the feeling was to carry on, but probably to carry on in the hope that we would eventually get more NHS material”; to switch from factor concentrate to cryoprecipitate“would have really needed some sort of national push to say that’s what needs to be done”.[1170]
A further Working Party meeting in December 1983 did not result in any change of
approach.[1171]
The QEH return for 1983 showed some treatment with cryoprecipitate in hospital but predominantly treatment with NHS concentrate and Factorate in both hospital and home settings.[1172] A similar picture emerged from the 1984 return.[1173]
A further meeting of the Working Party in May 1984 noted that there was a shortfall of 3.5 million units of Factor 8 which it was agreed should be made up by commercial Factor 8.[1174] On 24 May 1984 Dr Franklin wrote to Dr Lane registering his concern about the shortfall, which meant that the Centre might have to treat patients with commercial product who had never been exposed to it in the past.[1175]
Professor Franklin suggested that it would have been beneficial to have something more forthright from UKHCDO as to what to do: he expressed himself as feeling “a bit sad on behalf of the patients of the Queen Elizabeth Hospital that we didn’t get enough advice. You know, there was more to be had, I think ... Mark Winter mentioned the CMO – pretty silent in all this. I don’t think it necessarily had to be the CMO but something definitive as to what we should do.”[1176]
It was only after the Elstree meeting on 10 December 1984 that measures were taken. The West Midlands Working Party held an extraordinary meeting on 17 December to discuss the implications of the use of Factor 8 concentrates in light of the death of two people with haemophilia from AIDS and a treatment policy was agreed: DDAVP or cryoprecipitate for mildly affected patients and von Willebrand disorder; newly diagnosed people with severe haemophilia to be managed wholly on cryoprecipitate; NHS Factor 8 for patients with no previous exposure to commercial concentrate; patients with previous exposure to be treated with NHS Factor 8 if available and heat-treated commercial concentrate if not.[1177]
Professor Tuddenham became aware of the reports of an association between haemophilia, factor concentrates and AIDS as soon as it was reported by the CDC in July 1982.[1178] Dr Kernoff attended the Heathrow airport hotel meeting in January 1983. Professor Tuddenham delivered a talk at the World Federation of Hemophilia meeting in Stockholm in late June 1983, describing the “deplorable situation the results of which are being discussed in the seminars on hepatitis and AIDS.”[1179] He was using “colourful language to emphasise the inherent risks of pooling blood from thousands of donors.”[1180] There was, however, no change in the Royal Free’s treatment policies until heat-treated products became available at the end of 1984, as both Professor Tuddenham and Professor Lee accepted.[1181] December 1984 was the first time that the Royal Free effectively responded to the risks of AIDS by changing its approach to treatment, which it sought to do in two ways: introducing heat-treated products and delaying elective surgery.[1182]
The Royal Free’s annual return for 1983 showed that commercial concentrates remained the principal treatment for Haemophilia A.[1183] The same was the case in 1984 although the volume of NHS concentrates increased.[1184]
Following the decision to use heat-treated products in December 1984, in January 1985 Dr Kernoff wrote to patients explaining that it would not be possible to change everybody to heat-treated products immediately. The overall objective of the Royal Free’s policy was said to be to give the safest possible treatment to an individual. There are two remarkable features about this letter. The first is that the letter makes no reference to AIDS whatsoever: the change is said to be to “reduce the risk of virus transmission” but does not explain which viruses had triggered this change of approach. The second is that home treatment patients (who would be receiving commercial concentrates) were told to continue to use their current stocks until they were almost finished and then call in personally to collect new supplies.[1185]
When Dr Ludlam became director in 1980, his approach to treatment had three principal features. First, he moved from a system based on cryoprecipitate as the main treatment for Haemophilia A to a system of predominantly PFC Factor 8 concentrates. Secondly, he substantially increased the number of patients on home treatment: when he arrived in Edinburgh there were 6 patients on home therapy; by 1983 there were about 40 or 45. And thirdly, he increased usage of factor concentrates as a whole substantially.[1186]
One effect of Dr Ludlam’s reversal of his predecessor’s policy (which had been based on cryoprecipitate) was that the local blood transfusion service redirected donor blood plasma from cryoprecipitate production to concentrate manufacture.[1187] By May 1982 Dr Boulton, the deputy director of the South East Scotland Blood Transfusion Centre, was writing to Dr Ludlam stating that “your home therapy programme alone has accounted for about 80 per cent of our allocation from PFC” and warning that “we are now very definitely at the limits of our production for home therapy and therefore you may consider the necessity for buying some commercial product.”[1188] Dr Boulton wrote again with similar concerns in August 1982.[1189] Minutes of a meeting in August 1982 recorded agreement that Dr Ludlam would “make additional efforts to keep within the monthly allocation from PFC” and a warning from Dr Boulton that there would almost certainly be a need to buy more commercial Factor 8 if the current usage pattern continued.[1190] Similar concerns continued to be expressed at the end of 1982.[1191]
The figures in the annual return for 1981 are not legible.[1192] However, the 1982 return records an increased use of NHS concentrate over cryoprecipitate and the use of small amounts of Factorate and Koate; the use of DDAVP was also recorded.[1193] 1983 showed a further reduction in the use of cryoprecipitate and increase in the use of NHS concentrate, with both Factorate and Koate being used in larger quantities than previously.[1194] 1984 saw a repetition of that pattern, with a further reduction in cryoprecipitate use and increase in NHS concentrate; some commercial concentrate (Factorate) was also used.[1195]
Children with severe Haemophilia A would be treated initially with cryoprecipitate, but might move to concentrate at a youngish age. By 1983 there were around four to six children on home treatment.[1196]
A form of batch dedication was introduced in late 1984. Professor Ludlam was not clear why this was not introduced earlier.[1197]
Professor Ludlam described his perception of non-A non-B Hepatitis as being that it was seen as a “mild non-progressive condition, the first serious study on liver biopsy having been undertaken in 1985.”[1198] During questioning by Counsel to the Inquiry he suggested that this was the perception in the mid-1980s.[1199] He said he had been well aware of the Sheffield study of 1978, and of later papers questioning whether it was progressive, but it was “clear” by the mid 1980s. When he came into post in 1980 he said his view “and I think a widely held view was that we were very uncertain about its seriousness ... I think it was more a lack of evidence about its progressiveness that led us to believe that it’s possible it might not be progressive and it became clear that there was a wide range of ways in which it – rates at which it did progress between different people.” He went on to describe the view of Dr Colvin and Dr Kernoff in 1979 that it was a “serious disease with long-term consequences” as being a reasonable view to have held at the time.[1200]
As a comment, where a doctor is uncertain about whether an infection leads to serious long-term consequences, but recognises that there is significant evidence to show that it may do so, and it is reasonable to think that it might, he should not be drawing comfort from a lack of evidence that it does. He should not be looking for and placing importance on it becoming “clear” until he considers taking action: for there is at the very least a real risk from the start that it might do so. To draw comfort from there appearing to be few cases is to confuse incidence with risk, especially where it is believed that the consequences of being infected may emerge only later. The sense of Professor Ludlam’s evidence was that he chose to be reassured by the absence of many cases of serious liver disease (where there was no reliable evidence that he should have been, and it might have been expected that such disease would inevitably take some time to emerge) rather than choosing to take active steps to reduce the potential for the risk to become reality. Professor Ludlam was not alone in this: the criticism in this paragraph applies to most, including his mentor Professor Bloom. However, it is a real pity that he, of all people, someone who came across as painstaking, adopting something of an academic approach to research in haematology, and plainly given to detail, should adopt it, especially since his appointment as director of the Edinburgh Centre led to it largely abandoning cryoprecipitate in favour of concentrate. Though he was justified in placing faith in the voluntary donor system, and local sourcing of blood and plasma in Scotland as protective against the much larger risks from imported commercially sourced products, it was not a complete panacea as events would show.
Professor Ludlam thought that he first became aware of cases of AIDS in people with haemophilia in August to October 1982.[1201] He was, however, in his oral evidence to the Inquiry, at pains to emphasise – and over-emphasise – “the uncertainty that there was at the time about the cause of AIDS.”[1202] He was dismissive about the value of the Desforges article in The New England Journal of Medicine, suggesting that she was “a staff writer” for the journal (she was in fact a haematologist with over three decades of clinical experience by 1983 and had been appointed a professor of medicine in 1972; that she was also an associate editor of The New England Journal of Medicine did not undermine that). He accepted that he was by 19 January 1983 (when the Hepatitis Working Party, of which he was a member, received an update from Dr Craske)[1203] aware of the San Francisco baby case, but suggested that this was “circumstantial evidence. It didn’t, in any way, begin to fulfil Koch’s postulates for demonstrating that an agent causes a disease.”[1204]
Dr Ludlam attended a meeting on 21 January 1983 of SNBTS directors and haemophilia directors which recorded that purchases of commercial material in Edinburgh had increased; he told the meeting that the reasons were partially clinical and partially a policy of conserving a “cushion” of NHS Factor 8 against an anticipated shortage when production at the PFC would be suspended to carry out alterations required by the Medicines Inspectorate. There was surprisingly little discussion of AIDS; the minutes merely record Dr Cash drawing attention to recent articles and Dr Ludlam informing members that in the UK a letter and questionnaire had been sent out to haemophilia directors. There was no discussion about any change of approach to treatment or any other expression of concern by those present.[1205] Dr Ludlam was also present at the Heathrow hotel meeting on 24 January 1983.[1206] He had no recollection of the contents of the meeting. When asked by Counsel to the Inquiry if he agreed that there was no suggestion in the notes of the meeting that the cause of AIDS in either patients with haemophilia or patients who had had transfusions was anything other than the receipt of blood products or blood, he said “I agree that is as set out by Dr Craske, but of course, Dr Craske is a virologist and would see things from a virological perspective.”[1207]
In his testimony there was the following exchange:
“Q. what you are describing is 1983, early 1983, you realised that factor concentrates not only gave rise to a potential risk of non-A, non-B infection and a real risk of HIV infection, but there was a third problem, which was neither hepatitis or HIV, but that was the problem that it might, in any event, separately, give rise to a deterioration in the immune system which, in general, would not be a good thing. Have I understood correctly?
A. Absolutely correctly, yes.
Q. So there were now three reasons why factor concentrates were potentially undesirable if there were any proper alternative?
A. Yes.” [1208]
It would follow if this were well-founded that although PFC-produced concentrate was less likely than commercially produced concentrate to have contributions from donors with a virus which might lead to AIDS,[1209] all factor concentrates – whether domestic or commercial – were as likely as each other to cause people with haemophilia who had been heavily treated with them in the past to have deteriorating immune systems and be more vulnerable to AIDS.
There was no significant change of approach to treatment in 1983 and 1984 at Edinburgh in response to the risk of AIDS, or the threefold risk identified in this exchange, because Professor Ludlam thought the PFC concentrates were reasonably safe and made the assumption that the likelihood of there being a transmissible agent was low in Scotland: “we felt it reasonable to go on with using cryoprecipitate in decreasing amounts and using local concentrate for treating the patients.”[1210]
In February 1984, a meeting of SNBTS directors and haemophilia directors recorded Dr Ludlam as saying that “cryoprecipitate was preferred in the treatment of children at present, because of the new danger of AIDS.” Dr Hann was recorded as concurring. The minutes continued “A policy seemed to be emerging however to use less cryo for haemophilia A patients.”[1211] Dr Ludlam’s practice in Edinburgh was not, however, now to use cryoprecipitate for the treatment of children. It was unclear from his oral evidence why that was the case and he found it difficult to explain what, in February 1984, his views were as to the relative risks of cryoprecipitate and NHS concentrate.[1212]
In the autumn of 1984, Dr Ludlam sent a number of stored samples to Dr Tedder for testing. He did so without the knowledge or agreement of the patients involved.[1213] It is unclear what prompted that action. Dr Tedder’s evidence, to the Lindsay Tribunal, was that Dr Ludlam “already had a clinical suspicion that something had occurred.”[1214] Dr Ludlam told this Inquiry that he had “no prior inkling that any of our patients had been infected” and that he was “pretty confident that they would be negative.” His reasoning was that he sent them because, having read the paper in The Lancet in September describing the testing of different groups, “I thought, well, I should at least find out whether the patients who got commercial concentrate were antibody positive or not and, along the way, why not send some people who had only received Scottish Factor VIII, as I say, expecting them to be negative.”[1215]
By 26 October 1984, when Dr Ludlam telephoned Dr McClelland, he had learned that six patients with haemophilia had developed antibody to HTLV-3. By 2 November Dr Ludlam had received further test results relating to sixteen patients.[1216] On 7 November 1984, a meeting was held regarding the “Laboratory and clinical management of patients with evidence of HTLV-3 infection and from groups known to be at risk” following which, on 16 November, Dr Ludlam wrote to a colleague at the Royal Infirmary that “It has recently become apparent to me that some of our patients with haemophilia have antibody to HTLVIII virus.”[1217] And on 29 November, a meeting was convened to discuss the implications of the recent findings, at which Dr Ludlam explained the circumstances in which it had been discovered that 16 patients treated exclusively with SNBTS Factor 8 had been infected. Dr Forbes described findings relating to seroconversion in a comparative study of patients in Glasgow and Denmark and Dr Brenda Gibson reported that five out of ten patients tested at the Royal Hospital for Sick Children (Yorkhill) were HIV positive.[1218] The meeting continued:
“Views were exchanged on the very difficult ethical problems which had arisen. These included whether patients and patients’ relatives should be informed and perhaps subjected to needless worry; whether publicity additional to that already provided should be given, and how directors should respond to direct enquiries or requests for advice. The chairman advised members that ministers had been informed and that SIO had been briefed. While a press statement would not be issued by the Department at present any enquiries would be answered. It was agreed that every effort should be made for patients to have the situation explained to them before the impending publicity.”[1219]
Thus by 29 November, over a month after the first results had been communicated to Dr Ludlam, a number of organisations and individuals, including ministers, were aware of what had happened, but patients were still in the dark. Some were known to be infected with HIV but through their own lack of knowledge of that fact were not aware of the importance of taking precautions to avoid infecting others; others continued to treat themselves with concentrates in the erroneous belief that PFC concentrates were entirely safe. As detailed later in this chapter, it was not until 19 December 1984 (by which time Dr Ludlam had known the results for 16 patients, as well as a larger number of negative results, for nearly two months but had not told a single patient) that a group meeting took place to alert patients to what had happened. It was not until 1985 that the process of informing individual patients of their test results commenced.[1220]
According to information provided by Professor Ludlam both to the Penrose Inquiry and to this Inquiry, 23 patients (all with severe Haemophilia A) were infected with HIV as a result of treatment in Edinburgh (2 of them children); 18 of those 23 had received treatment with material from a single batch of SNBTS product; 5 had received treatment with other SNBTS and commercial products.[1221]
In 1982, the usage of cryoprecipitate diminished markedly: only 17,350 units in contrast with nearly 2 million units of NHS concentrates (and modest amounts of commercial: 25,496).[1222] 1983 saw an increase in the use of commercial concentrates (200,000 units of Factorate for home treatment), although NHS concentrates remained the mainstay of treatment.[1223] The use of commercial concentrates dropped again in 1984.[1224]
Professor Forbes told the Penrose Inquiry that by March 1983 “already we were starting to look rather differently at our patients to see if they had any of the features that might be an early warning of AIDS.”[1225] He also acknowledged that in 1983 there was a potential for contamination of blood products “even from local, home-grown sources ... that was always the concern, that HIV would come into the donor population of the UK.”[1226] Whilst accepting that this was a “concern”, there is no indication of any alteration in practice in Glasgow, save that a batch dedication system may have started in around 1983/1984.[1227] The reference to “starting to look rather differently at our patients” may be a reference to the work initiated by Dr Forbes in around late 1982 or early 1983 – a study of immune abnormalities in patients with severe haemophilia, which resulted in the publication in The British Medical Journal on 15 October 1983 of a paper entitled Immunological abnormalities in haemophilia: are they caused by American factor VIII concentrate? The conclusion of the study was that Scottish patients had immunological abnormalities similar to those in their US counterparts.[1228]
In December 1984, a second article emanating from Glasgow was published, this time in The Lancet. This revealed that 77 Scottish people with haemophilia and 22 Danish people with haemophilia were tested for antibodies to HTLV-3. 15.6% of the Scottish people with haemophilia (11 with Haemophilia A, 1 with Haemophilia B) were positive. All but 2 were known to have received commercial factor concentrates in the period 1979-1984. By contrast, 59.1% of the Danish cohort were positive: all but 2 of the cohort had received commercially produced concentrates. The study showed that infection was directly correlated with taking commercial concentrates.[1229]
Blood had been taken from the 77 patients between December 1983 and July 1984. They were not told that their blood was being tested for HIV.[1230]
Dr Mayne’s recollection of when she first became aware of AIDS was that it was raised during an informal lunchtime conversation with Professor Bloom, Dr Kernoff and Dr Craske, in which the latter described a recently published paper referring to an immune condition in homosexual males in San Francisco. Dr Mayne could not recall when this discussion took place, but the paper referred to may be the article published in The Lancet on 12 December 1981.[1231] She attended the reference centre directors’ meeting in September 1982 referred to earlier in this chapter, as well as the January 1983 meeting at the Heathrow hotel. She was not in attendance at the 13 May 1983 special meeting of reference centre directors.[1232]
Some years later, in 1993, following the prosecution of Professor Jean-Pierre Allain in France, Dr Mayne wrote to the editor of The Lancet stating that “The evolvement of the HIV problem within the haemophilia population has caused immeasurable distress to patients and to all physicians treating them. The Doctors concerned were guilty of one fault, namely that of ignorance.”[1233] That is an inaccurate characterisation of the position. Sufficient evidence and information were available to clinicians, especially in the second half of 1982, to put them on notice that action was required in order to minimise the risk of AIDS being transmitted to their patients. Unfortunately, no such action was taken in Belfast.
In 1982, 1983 and 1984 patients with Haemophilia A continued to be extensively treated with commercial concentrates.[1234] In 1985 Dr Mayne listed the following volumes of product usage:
Dr Mayne suggested that “It is clear from these figures that the increased use of N.H.S. material should have produced an economy in the purchase of commercial material but, due to extensive orthopaedic surgery being necessary following a series of road traffic accidents and bone fractures, the increase in N.H.S. material was inadequate for needs.”[1236]
In a report which Dr Mayne prepared for defendants in the HIV Haemophilia Litigation, she commented on measures which might have reduced the risks of hepatitis and AIDS, suggesting that some of them would have denied “the goal of haemophilia treatment, namely to minimise pain and disability and to prolong life.” She objected to restriction of:
“the choice of treatment available to the physicians in charge of the patient: the person in possession of all the information regarding the patient’s needs. The alternative treatments; cryoprecipitate, Desmopressin and animal concentrates have already been discussed and found wanting for the universal treatment of severe haemophilia ... The risk/benefit ratio of non treatment versus treatment could not be upheld in the light of the plight of haemophiliacs in the era before infusion treatment became available.”[1237]
There are four obvious problems with this perspective. The first lies in the characterisation of the physician as being “in charge of” the patient, the physician being the person “in possession of all the information regarding the patient’s needs.” This is paternalism writ large. The person in charge of the patient is the patient. The person in possession of all the information regarding the patient’s needs is, in the broad sense, the patient. The second problem is the sense that only a universal answer would have been satisfactory, whereas in reality what could and should have been implemented was not a single “universal treatment” in place of factor concentrates, but a range of different and time-limited measures: a suspension of home treatment for some, the replacement of concentrates with cryoprecipitate for others, bed rest for those who did not want to run the risks of any treatment. That this was her approach at the time is apparent from her written evidence to the Inquiry, in which she stated that “In reality, the choice was stark – stop treatment with concentrates with all the risks and disruption that would entail for patients or continue with treatment in light of the information then available.”[1238] The third problem is her characterisation of the “plight” of people with haemophilia in the pre-concentrate era, which overlooks the role of cryoprecipitate. And the fourth, linked to the first, is the unspoken assumption that it was for the physician to determine the risk/benefit ratio, when that should have been a choice left to the patient.
Dr Mayne’s evidence, and data provided to the Inquiry by UKHCDO, suggests that 16 people were infected with HIV following treatment at the Belfast Centre.[1239]
Professor Bloom was, as the chair of UKHCDO, privy to the information regarding AIDS that is discussed earlier in this chapter. He was aware as at September 1982 that three patients with haemophilia in the US were reported to have AIDS. By, or in, January 1983 he was sent, probably by Dr Cash, the December 1982 MMWR. This reported that all three of the patients identified in the July MMWR had died and more cases had been identified, including two patients aged ten or under, leading to the observation that “children with hemophilia must now be considered at risk for the disease.”[1240] He attended the Hepatitis Working Party meeting on 19 January 1983 at which Dr Craske provided a detailed update about the cases in the US, including the San Francisco baby case and the papers in The New England Journal of Medicine.[1241] He attended the Heathrow hotel meeting on 24 January 1983.[1242] Yet, as discussed elsewhere in this Report, he materially downplayed the risks of transmission at this critical time. His stance throughout this time is exemplified by the letter he sent to David Watters on 20 January 1983, in which he wrote:
“Clearly at the present time the cause is quite unknown and neither has it been proven that it is transmitted through contaminated blood products. The incidence of the condition in America is not known but seems to be about one per thousand of the severely affected treated patients. On this basis if the disease exists in the U.K. we could reasonably expect two or three cases amongst British haemophiliacs. So far none have been reported ... As the full blown condition has not yet been reported amongst British haemophiliacs it is not possible to state if the coagulation concentrates produced in this country are safer in this respect than the concentrates produced in the U.S.A. Indeed there is no evidence yet in fact to implicate the latter ... In the meanwhile there is certainly no need for the haemophilic community to be unduly concerned about this ‘new’ syndrome. They can rest assured that every effort is being made to monitor the situation in this country and to collaborate with the Centre for Disease Control in the U.S.A. ... coagulation factor therapy is so essential for the safety and well being of patients that there is no doubt whatsoever that their advantages outweigh this disadvantage which at the moment seems to be potential rather than real in the U.K. at any rate.”[1243]
In early March 1983, Professor Bloom received a letter from Dr Evatt from the CDC who informed him that AIDS was having a major impact on the treatment of people with haemophilia in the US: “The evolution of the epidemic is occurring with a frightening pace ... The incidence rate has been increasing in hemophiliacs and the epidemic curve paralays that of the total epidemic curve.”[1244] He was also at around the same time sent Alpha’s press release which reported that the evidence suggested (although did not absolutely prove) that a virus or other disease agent was transmitted through Factor 8 concentrates to those people with haemophilia who had developed AIDS.[1245]
There can be no doubt, therefore, that in early 1983 Professor Bloom had not only all the information about the risks of transmission of AIDS available to him that other haemophilia clinicians had, but he also had additional sources of information that ought on any view to have led him to appreciate that transmission to people with haemophilia in the UK was inevitable unless steps were taken. By April he also had the knowledge that one of his own patients had AIDS. Yet he continued to minimise the risk, as seen by the advice which he provided to the Haemophilia Society, discussed elsewhere in this Report.[1246]
There is, however, evidence to suggest that following the special meeting of reference centre directors on 13 May 1983, Cardiff may have produced written guidelines for haemophilia treatment. These guidelines, dated 18 May 1983, suggested that: for people with mild haemophilia and von Willebrand disorder DDAVP should be used for minor lesions, or cryoprecipitate or NHS concentrate for other lesions; for children with severe haemophilia cryoprecipitate or NHS concentrate should be used; for adults with severe haemophilia cryoprecipitate should be used for in-patient treatment where feasible; those who had never received imported concentrates should where possible only receive NHS concentrate, and other patients should continue to receive imported concentrate; and patients with Haemophilia B should continue to receive NHS Factor 9. There were also some “General Points”, which included:
There are four observations to make regarding these guidelines.
The first is that their production in May 1983 suggests that no steps were taken prior to that date in response to the risk of AIDS.
The second is that the picture revealed by the annual returns is not entirely consistent with the implementation of these guidelines. 1983 saw a reduction in the use of cryoprecipitate for the treatment of patients with Haemophilia A, with the main treatment product being NHS concentrates (809,972 units) and commercial concentrates (1,051,422 units).[1248] Whilst Profilate was the main commercial product used (both for home and hospital treatment), Factorate, Koate, Hemofil and Kryobulin were all used in varying degrees. The individual patient data filed with the return shows some people being treated with multiple products during the year. The 1984 return showed a modest increase in the use of cryoprecipitate, a greater increase in the amount of NHS concentrates used (1,704,313 units), and a reduction in the amount of commercial concentrates (861,677 units), although, as the figures show, treatment with commercial concentrates was still a substantial part of the approach at Cardiff. The principal commercial concentrate in use in 1984 was Koate.[1249] DDAVP featured on the return for the first time: there is no record of its use to any significant extent in 1983.[1250]
The third is that the guidelines drew little distinction between the use of NHS concentrate and the use of cryoprecipitate (and indeed Professor Bloom wrote to Dr Boulton on 23 May stating that “at the moment we are not rigidly differentiating between cryoprecipitate and N.H.S. concentrate as far as severely affected patients are concerned at any rate”[1251]), yet NHS concentrates were made from large donor pools and on any view carried a substantially greater risk of transmitting both NANBH and the agent causing AIDS than cryoprecipitate. This absence of any clear distinction between cryoprecipitate and NHS concentrate is apparent from the inconsistent treatment of children at the Centre in 1984. The individual patient data filed with the 1984 return shows:
The fourth point is that the Cardiff guidelines may relate only to treatment in hospital. In relation to home treatment, Professor Bloom’s view, as expressed by him at the UKHCDO meeting in October 1983, was that there was no need for patients to stop using commercial concentrates and that patients should not be encouraged to go over to cryoprecipitate for home therapy but should “continue to receive the NHS or commercial concentrates in their usual way.”[1254] It is, moreover, clear from both the returns and the statements which the Inquiry has received from those treated in Cardiff, that home treatment continued unabated.
The data provided by UKHCDO to the Inquiry indicates that 45 people treated at the Cardiff Haemophilia Centre were infected with HIV.[1255]
In common with Professor Bloom, Dr Rizza, director of the Oxford Haemophilia Centre, and secretary to UKHCDO, knew at least as at September 1982 that three US patients with haemophilia were reported to have AIDS. On 8 October 1982 he wrote to Dr Craske referring to information he had received from the US: “Apparently the whole problem has caused quite a stir in the haemophilia world in the States so much so that one very senior physician has withdrawn his factor VIII concentrates from the accident room and insists on vetting the patients himself before any dose is given.”[1256] In November 1983, Dr Rizza was provided with a copy of Dr Craske’s paper on AIDS. He attended the Hepatitis Working Party meeting on 19 January and the Heathrow hotel meeting on 24 January 1983.
In May 1983, Dr Rizza wrote to the Oxford Regional Health Authority’s regional medical officer in support of plans to set up an AIDS screening programme. The terms in which he wrote are instructive:
“I think it is important that we act quickly to set up screening tests to detect the patients who might be at risk of developing the full blown condition.
Apart from their value in helping us manage our patients better, I think it is particularly important to set up tests in Oxford for the following reason. The Oxford Haemophilia Centre is the largest in the country and in addition to using American factor VIII concentrates which are said to carry a risk of transmitting AIDS, we also use large amounts of NHS factor VIII. Our system of treatment is such that many patients have received only NHS factor VIII and others only U.S. concentrates. It should therefore be possible to find out if patients on NHS concentrates are immuno-suppressed to the same degree as those on U.S. concentrates ... The matter is one of great urgency.” [1257]
The letter indicates a clear awareness that people treated at Oxford were and would continue to be at risk. There is, however, no evidence of any change of direction in terms of treatment. The 1983 annual return shows that there was almost no cryoprecipitate used for the treatment of Haemophilia A. 1,636,580 units of NHS Factor 8 were used; over 4.5 million units of commercial concentrates were used.[1258] The return made no mention of DDAVP. The individual patient data filed with the return shows patients being treated with more than one type of concentrate (sometimes treatment with NHS concentrate and with two types of commercial concentrate), suggesting that there was no batch dedication system in place.[1259] The picture in 1984 is similar (save that DDAVP was mentioned for the first time): almost no cryoprecipitate; 1,919,162 units of NHS Factor 8; and 3,907,595 units of commercial concentrates.[1260] The individual patient data shows people being treated with NHS and commercial concentrate and with more than one type of commercial concentrate.[1261]
It was not until December 1984, when the Centre placed its first order for heat-treated concentrates, that there was any significant change of approach.[1262]
Data from UKHCDO records that 128 patients tested positive for HIV at Oxford.[1263]
In Bradford, where Dr Parapia took up an appointment as a consultant in 1981 and then became director in 1982,[1264] cryoprecipitate had been used almost exclusively.[1265] The 1982 annual return showed a move away from cryoprecipitate to factor concentrates and the introduction of home treatment,[1266] with a similar pattern in 1983.[1267] It appeared from Professor Parapia’s evidence that this reflected a perceived need to “keep up with the times” and not appear “inferior”. Professor Robert Turner had been “quite old fashioned and he believed cryoprecipitate was okay.” The commercial home treatment packs were “far better” than the NHS packs, being “all ready in a nice little box with the needle and everything” and were more soluble.[1268] In relation to the relative safety of commercial products, Professor Parapia would ask questions of commercial companies about where they were getting their donations from, would be told that they conformed to the appropriate US standards, and had to accept their answers “because [the products] were licensed.”[1269] He said “we were desperate for guidance ... for leadership, which I don’t think we ever got properly, either from the Government or UKHCDO or whatever.”[1270]
Professor Parapia read The New England Journal of Medicine but following the January 1983 editorial[1271] he did not recall having discussions within the region about what to do: “We were waiting, again, for instruction or guidance.”[1272] A reversion to cryoprecipitate for patients with haemophilia was not considered.[1273]
No changes to treatment practice took place in Bradford before December 1984. A meeting of local haemophilia centre directors and transfusion directors took place on 4 December 1984. The note of the meeting recorded agreement that “on theoretical grounds heat-treated material was likely to be safer than non-treated material”: Dr Parapia and Dr Michael McEvoy felt that NHS material was preferable, whilst Dr Swinburne and Dr David Barnard were in favour of heat-treated material (whether NHS or from the US).[1274] In February 1985, Dr Swinburne wrote to Dr Derrick Tovey at the RTC explaining that local directors, having discussed the Elstree protocols (a reference to the AIDS Advisory Document produced following the 10 December meeting at BPL), were not interested in the offer of an interim heat-treated product likely to be available for only two or three months and preferred to wait until April when “a better product is promised”; in the interim they would use untreated BPL Factor 8.[1275] Professor Parapia expressed surprise at the decision (which he could not recall) to turn down the interim heat-treated product and use an unheated product.[1276]
UKHCDO data suggests that 18 patients were infected with HIV at Bradford.[1277] To put that figure in context, 22 patients with Haemophilia A were treated during 1982 and in 1983.
St George’s Hospital had around 25 severely affected patients, including about 8 children, in the late 1970s and early 1980s. Like many haemophilia centres, it had shifted away from cryoprecipitate and towards concentrate, predominantly commercial.[1278] As described by Dr Bevan (who joined St George’s in 1977 as a registrar, then as lecturer and honorary senior registrar, before his appointment as the consultant haematologist in 1984), “this was the pattern all across the haemophilia world.”[1279] He recalled the growing use of home treatment, mostly on demand but with some prophylaxis, mostly in children and young people.[1280] Professor Peter Flute, who was until 1985 the director of the Centre, preferred to give NHS concentrate to children and younger adults with severe Haemophilia A because of the risk of transmission of NANBH, but adults were usually given commercial concentrate. So too were younger adults, despite the preference of Professor Flute for NHS product, because there were insufficient supplies of NHS concentrate. It was probably inevitable that children too ended up receiving commercial (Armour) concentrate.
There was no change of treatment policy at St George’s in response to the risk of AIDS until a switch to heat-treated products in early 1985.[1281] Dr Bevan recalled a meeting with Professor Flute at which the issue of AIDS was raised and the risk to people with haemophilia. Professor Flute “in his usual way, kind of gruffly, jovially said he didn’t regard this as in any way a proven infection.”[1282] Professor Flute explained that in no way would he take any action in terms of changing infusion practice in haemophilia, unless there was official firm guidance from UKHCDO to do so.[1283] There was, of course, no such guidance until the December 1984 AIDS Advisory Document.[1284]
Dr Bevan’s recollection was that there were between 15 and 18 patients infected with HIV, of whom one had moderate Haemophilia A, one had Haemophilia B and the remainder were people with severe haemophilia (of whom three or four were children).[1285]
Guy’s Hospital, in London, was a relatively small haemophilia centre, with about 30-40 registered patients, of whom about 10-15 were severely affected. The director was Dr Percy Barkham, whose interest lay outside haemophilia, and in practice the haemophilia patients were managed by senior registrars. Dr Winter, who worked at Guy’s between 1979 and 1983 as one of the senior registrars, explained that there was “never enough” NHS concentrate.[1286] The RTC at Tooting had to cover both the South East and the South West Thames regional health authority areas and was as a result under a great deal of pressure.[1287] Shortfalls were covered by the use of commercial concentrate, and cryoprecipitate was in limited use only: for mild haemophilia or von Willebrand disorder, or occasionally for a child or rarely treated adult.[1288] Some people with moderate haemophilia would have received commercial concentrate because of the shortfall.[1289] It was possible that a patient with mild haemophilia might also have received commercial concentrates, if DDAVP was not going to work.[1290] Children were prioritised for the NHS product: Dr Winter could not recall giving a child commercial concentrate but could not be absolutely sure that he had not.[1291] There was prophylactic treatment for children.[1292]
Dr Winter could not recall what (if any) changes were made to the treatment practices at Guy’s in response to the risks of AIDS: children would have continued to be prioritised for the BPL product; it was possible (but he could not recall) that prophylaxis programmes might have been suspended; but the key message for him and his colleagues was “do not give concentrate unless the patient absolutely needs it.”[1293] There was no reversion to cryoprecipitate; Dr Winter thought that Tooting would not have been able to provide sufficient supplies, but accepted that no one from Guy’s, to his knowledge, approached Tooting to explore the possibility of more cryoprecipitate being supplied.[1294]
In December 1983, Dr Winter moved to take up the post of director at the Haemophilia Centre in Margate.[1295] This Centre had not been operating in the same way as centres elsewhere: patients on home treatment got Factor 8 on prescription from their GP and then collected it from their local pharmacy.[1296] This system appeared to have resulted from a serious lack of local funding in previous years. The result was that there were no records as to what patients had received or as to the type or amount of Factor 8 they had been using for home treatment. Neither the GP nor the pharmacist would have been likely to know anything about Factor 8 or alternative treatments, and patients would have been receiving exclusively commercial concentrates because the pharmacist would not have access to the supply of NHS concentrate from the RTC.[1297]
Following discussions with Dr Savidge, Dr Winter decided to start using heat-treated concentrates (from Alpha) on a named patient basis; this was, he said, a very difficult decision.[1298] Dr Winter recalled Professor Bloom saying to them “You are mad to switch. There will never be HIV in BPL Factor VIII.”[1299]
The heat-treated concentrates began to be available in May 1984 and from June 1984 the only concentrates being used were heat-treated Factor 8 and 9 both for hospital treatment and home treatment and prophylactically for children.[1300] Dr Winter’s initiative was, however, too late. When he sent sera to Dr Tedder for testing in October 1984, all but one was positive for HIV, a consequence of the system that had prevailed under his predecessor. About half of those were children and some would have been people with moderate haemophilia.[1301]
Dr Winter was, rightly, critical of the lack of “what you might call powerful, influential, centralised advice ... there was no central body that had published very clear, firm guidance or protocol, or call it what you will, to haemophilia doctors saying, this is what we think you should do in this situation.” When HIV broke, “we were blood specialists, haemophilia doctors, not virologists dealing [on a] day-to-day basis with the problems caused by a virus of which we were not specialists ... We very much lacked firm, central guidance from whatever body ... a body set up for national virological advice, or the Chief Medical Officer or whatever.”[1302]
Dr Winter told the Inquiry of two patients who were treated at William Harvey Hospital in Ashford, Kent, a general hospital which did not have a haemophilia centre. A four-year-old boy with mild haemophilia was given commercial Factor 8 in April 1984, was infected with HIV, and subsequently died. A man with mild haemophilia who cut his arm and was taken to the same hospital in June 1984 was given commercial Factor 8, was infected with HIV, and subsequently died.[1303] These starkly illustrate the consequences of the lack of clear central advice and guidance.
Dr Colvin, the director of the haemophilia centre at The London Hospital, attended, like many of his colleagues, the 24 January 1983 meeting at the Heathrow hotel.[1304] He would have read the Desforges article in The New England Journal of Medicine.[1305] He acknowledged that by January 1983 he would have been aware that there was a risk to people with haemophilia of AIDS and that the most likely route of transmission for them was blood or blood products.[1306] He accepted also that AIDS was known to have a very high mortality rate and that there might be a significant lapse of time before symptoms presented, such that the fact that there were only a few cases so far identified would not be a reliable guide to the true extent of the risk.[1307] Yet when the Haemophilia Working Party of the North East Thames Region Association of Haematologists met on 9 February 1983, there was no discussion whatsoever about AIDS and the risks it posed.[1308] There was no significant change of approach to treatment instituted at The London, although Dr Colvin thought that they would have tried “to minimise the risk where it was sensible and possible to do so.”[1309]
It is striking that when in August 1983 Dr Colvin and Dr Kernoff co-authored a paper on haemophilia services in the NETR there was only passing reference to the risks of AIDS: a description of the complications of treatment as including “Plasma product-transmitted disease, particularly hepatitis and (possibly) the acquired immune deficiency syndrome (AIDS)” and a sentence that read “Clinical problems related to impaired immunity seem to be rare at present, but conceivably could become a major clinical problem.” No measures or steps to address or attempt to reduce or minimise those problems were considered in the paper.[1310]
Writing to David Watters of the Haemophilia Society in February 1984, Dr Colvin suggested that “we know little about AIDS at present. In my opinion there is no reason to spurn commercial concentrate and we have to keep an open mind on the risk associated with NHS material.”[1311] When the NETR Haemophilia Working Party met again in May 1984, the minutes record a suggestion that “until a positive test for AIDS and/or a vaccine is developed it should be policy to avoid use of blood products except for essential treatments and to use cryoprecipitate or plasma instead of FVIII Concentrate whenever possible.”[1312] That suggestion did not lead to any change of policy at The London.[1313] It was not until 13 December 1984 (ie following the meeting at Elstree on 10 December) that the NETR Haemophilia Working Party agreed a change of approach, namely to use heat-treated material whenever possible and to treat all new patients and those with mild haemophilia with heat-treated NHS concentrate or small pool Factor 8 concentrate if treatment with cryoprecipitate or DDAVP was not possible.[1314]
Dr Colvin’s evidence was that there were 41 patients infected with HIV, of whom 31 had severe Haemophilia A, 9 had moderate/mild Haemophilia A and 1 had Haemophilia B. He could recall three children who were infected with HIV from their treatment and one partner of a patient who was infected.[1315]
Of particular interest were Dr Colvin’s views that:
Also of interest are his reflections on how the service could have managed if importation of commercial concentrates had been suspended in July 1983.[1318]
The haemophilia centre at Leeds continued to use substantial amounts of commercial concentrate and no cryoprecipitate for the treatment of Haemophilia A patients between 1982 and 1984. Thus in 1982 the annual return shows somewhere between four and five times as much commercial concentrate being used as NHS.[1319] Although the volume of NHS concentrate increased in 1983, a very substantial amount of Factorate continued to be used.[1320] 1985 showed the use of a tiny amount of cryoprecipitate, with NHS concentrate and commercial concentrates being used in substantial amounts.[1321] There is no evidence from the returns or any other material of any risk reduction or minimisation strategy being pursued. The data received from UKHCDO suggests that 53 patients were infected with HIV.
Liverpool was another large non-reference centre. Dr Bernard McVerry was (in practice) the director between 1980 and 1985. A meeting of regional haematologists at the Mersey RTC in November 1983, attended by Dr McVerry and Professor Alastair Bellingham, was notable for the absence of any discussion at all about the issue of AIDS.[1322] From 1981 commercial concentrates predominated,[1323] with a marked decline in the use of cryoprecipitate from 1982,[1324] although the use of NHS concentrate increased in 1983 and 1984.[1325] The individual patient data filed with returns showed patients being treated with more than one type of concentrate.
Dr McVerry recalled consulting Dr Jones, the director of the Newcastle Haemophilia Centre, before choosing what products to prescribe: “Based on Dr Jones’s experience I was encouraged to switch to commercial F8 for two reasons, the first related [to] availability and reliability of supply, and second there was a mood at that time to continue using a particular product in an individual patient as this may reduce the prevalence of factor antibodies arising (although this later proved not to be the case).”[1326] Dr McVerry could not recall giving cryoprecipitate to a patient in Liverpool.[1327]
A document prepared by Dr Charles Hay (who became the director at Liverpool in 1987) for the HIV Haemophilia Litigation set out his understanding that “All patients were treated with whichever material was available. No cohorts were treated with any specific product ... Patients were treated with whatever was available and were not reserved particular products or batches (as was the practice in some centres). There was no pattern of use, and this did not change. All factor VIII used prior to mid 1985 was untreated and after that all was heat treated.” His view was that “insufficient use of cryo was made in this centre. Children and mild haemophiliacs should have been treated preferentially with cryo and possibly domestic concentrate.” He also confirmed that DDAVP was used less in Liverpool than in other centres.[1328] Other documentation arising in the context of litigation suggests that “no specific priority was given to mild haemophiliacs for treatment with NHS product at the time.”[1329]
Dr McVerry’s statement indicates that he had no awareness of AIDS until the September 1982 UKHCDO meeting. He referred to Professor Bloom saying even up to mid 1984 that there was no proven association with blood products, although he said it was reasonably clear there was a real risk at the end of 1983 or beginning of 1984. He would have read the Desforges article (having worked with her in Boston) and did not recall any reversion to cryoprecipitate in Liverpool (as is borne out by the annual returns).[1330]
1981 saw substantially increased use of NHS concentrate, although commercial concentrates remained the most used product (however, the usage for commercial concentrates was significantly less than the previous year); a relatively small amount of cryoprecipitate was used.[1331] In 1982, the picture was broadly similar to 1981.[1332] 1983 showed no particular change of approach. The Centre treated its patients with a mix of NHS concentrates and commercial.[1333] 1984, however, saw a rather greater use of NHS concentrates than commercial, although a substantial amount of the latter (and a small amount of cryoprecipitate) was still used.[1334] It is likely that some of the commercial concentrates would have been heat-treated, although that is not apparent from the return itself.[1335] In 1985, the vast majority of treatment was with commercial concentrates, with very little NHS concentrate used: this is likely to reflect the use of heat-treated concentrates.[1336]
Dr Preston was present at the January 1983 Heathrow hotel meeting and as a reference centre director was party to the special meeting on 13 May 1983. He could not remember the detail of the meeting, although his general recollection was that nobody amongst the reference centre directors disagreed “with the concept of continuing with treatment, with the concentrates.”[1337] Treatment with concentrates “had to continue” because otherwise patients “would be severely incapacitated or even die.”[1338] The advent of AIDS did not lead to any reversion to cryoprecipitate for the Royal Hallamshire: it appears to have remained Dr Preston’s view that it was not particularly easy to use, there was no guarantee of the amount of Factor 8 in each bag, and it was not a particularly useful therapeutic option for major surgery or major bleeds.[1339]
The numbers of patients infected with HIV in consequence of treatment at the Royal Hallamshire Hospital is not entirely clear. Data from UKHCDO suggests 24 patients[1340] and Professor Preston’s recollection when he gave evidence to the Lindsay Tribunal was that the percentage of patients infected with HIV in Sheffield was lower than many other centres.[1341]
It will be clear from the above narrative that little was done by haemophilia centres in response to the risks of AIDS. Few centres implemented, or even contemplated, a reversion to cryoprecipitate. But cryoprecipitate could successfully be used for the treatment of both adults and children.
Dr Vivian Mitchell became the director at Leicester Haemophilia Centre in November 1979. When he arrived home treatment was established, with patients mostly using commercial concentrates. There was not a great deal of NHS Factor 8 being used. Dr Mitchell had worked as a senior registrar in Sheffield, under Professor Blackburn and Dr Preston. He understood from the 1978 Sheffield study that at least in some patients liver disease was significant and progressive.[1342] Dr Mitchell decided to adopt an approach to treatment that was explicitly based on the reduction of risk, restricting the use of large donor pool concentrates whenever possible. He was “convinced by the Sheffield work and the Sheffield report that there was a connection between the use of multi-donor factor concentrates and the development of liver disease” which could be progressive.[1343] Dr Mitchell described professional isolation. There was no national or regional guidance and he was some 70 miles from the reference centre in Sheffield. He therefore devised his own policy. For mild and moderate haemophilia and for von Willebrand disorder, he used DDAVP and tranexamic acid wherever possible and largely successfully, although it was not always sufficient for moderate patients.[1344] If he could not use DDAVP/tranexamic acid, he would use cryoprecipitate where feasible. For children with severe haemophilia, they would be treated with cryoprecipitate until they went onto home treatment (probably around the age of ten).[1345] Dr Mitchell did not experience difficulties in obtaining sufficient quantities of cryoprecipitate or with adverse reactions to cryoprecipitate.[1346] For adults with severe Haemophilia A, the approach was to treat them with NHS concentrates as much as possible,[1347] although there were insufficient supplies so commercial concentrates were used. He would have used more NHS product if it had been available.[1348] When he arrived, the majority of patients on home treatment were receiving commercial concentrate and he did not have the ability to switch them all over to NHS concentrates given the amount received.[1349] The second element of Dr Mitchell’s policy in relation to adults with severe Haemophilia A was to adhere to one batch of one concentrate as much as possible. He would buy as much as he could of a batch from a single commercial supplier. It took a year or so to implement this approach.[1350]
Dr Mitchell wrote to The British Medical Journal in July 1985 in response to Professor Bloom’s letter suggesting that cryoprecipitate should no longer be used. It is an important letter, because it shows that haemophilia centre directors could, using their initiative, reduce (although not eliminate)[1351] the risks of viral transmission:
“Initially because of concern about chronic liver disease in haemophiliacs, and, more recently, with HTLV-III also in mind, we have for the past five years tried to restrict the exposure of our patients to large donor pool concentrates. Cryoprecipitate has played a major part in this policy, being used in the treatment of patients with von Willebrand’s disease and those with mild to moderate haemophilia. Children with severe haemophilia are also treated with cryoprecipitate until they go on to home treatment. Even so, we used 1 million units of factor VIII concentrate in 1984, 60% in the form of commercial concentrate. This exposure is limited by buying as much as possible of a batch from a single commercial supplier. In this way patients have been treated for as long as 18 months using 100 000 units or more of the same batch.
This policy has resulted in a low prevalence of HTLV-III antibody in our patients. We recently tested 76 patients (including 27 children) who have received blood products at this centre during the past five years. Seven of the 28 who had received commercial concentrate were HTLV-III antibody positive (25%). There were no positive results from patients treated with NHS factor VIII concentrate only (5), NHS factor IX concentrate (12), cryoprecipitate (28), or fresh frozen plasma (3). The seven positive patients all have severe haemophilia A ... and constitute 37% (7 of 19) of this most at risk group. All are adults, aged 23 to 54 years ...
Recurrent treatment with blood products is hazardous ... The best approach seems to us to be a treatment policy which is designed to reduce, as much as possible, all the risks associated with blood products and which is tailored to the needs of each individual patient.” [1352]
An eighth patient later tested positive, who also had severe haemophilia. Dr Mitchell’s recollection was that no patient at Leicester with mild or moderate Haemophilia A or with Haemophilia B or with von Willebrand disorder tested positive, nor any child.[1353]
Professor Tuddenham rightly said in his evidence to this Inquiry that“Everything that we give to a patient has to be subjected to the most intense scrutiny.”[1354]
Blood products above all should be given the closest scrutiny to ensure they are as safe as can reasonably be: for it is given that one person’s blood or plasma may contain something that is harmful to a recipient just as it may also be beneficial. That should have been the guiding principle when dealing with blood products in the 1970s and 1980s. It is clear from earlier sections of this Report that blood was not always as safe as could reasonably be, and that making products from pools of blood from different sources made them less safe still.
Haematologists treating patients needed to be alert to newly emerging risks, and be prepared to modify the treatment offered to patients so as to minimise the prospect of those risks becoming reality for them.
The evidence shows that clinicians should all have been alert to a risk of AIDS by the end of 1982, if not earlier. It was by then already a substantial concern in the US, the likeliest candidates for transmitting its cause were blood or sex, and thus whether AIDS was caused by a virus, an overload of foreign proteins, or a combination of the two, large pool factor concentrates were likely carriers of them.
In the light of this awareness, what were the steps that could and should have been taken by haemophilia centres? They could and should have:
Above all, it was important to discuss the risks and alternatives (and be straightforward about the gaps in knowledge) with each patient individually, as fully as reasonably possible, and be guided by their view of what mattered to them.
It is important to appreciate that these measures did not have to provide a satisfactory permanent or even long-term solution: they needed to be implemented only until such time as the risk of transmission was eradicated, through viral inactivation, vaccination (until it could be discounted as being a possibility) and donor screening, or until knowledge expanded to a state where it could be shown that taking factor concentrates was safe. If, for instance, there had been a policy to use only NHS concentrate or cryoprecipitate, it would have reduced risks. It would not have eliminated them, as the Edinburgh experience demonstrates, but it would have taken steps in the right direction. What should not have happened was waiting for proof (rather than reacting to the risk, which was already established) that concentrates were unsafe before acting, for this is a recipe for inaction, delay, and the growth in numbers of infections and those carrying them which turns a public health problem into a public health crisis.
It is clear from what has been said about the individual centres that they each responded (if they responded at all) to different extents but, with notable exceptions such as Leicester, did not sufficiently respond as they might have done. Though knowledge of the extent to which patients with Haemophilia A became infected is inevitably retrospective, the policies which led to differences in result were made prospectively. What was applied in one centre with a view to keeping risk low could have been applied elsewhere, unless there was some compelling reason why it could not have been. None is obvious.
These failures lie with the haemophilia centres and their directors, in particular the reference centre directors, who failed to provide guidance when it was required. It is important to recognise, of course, that as set out elsewhere in this Report the blame for them goes well beyond clinicians, who in some respects were dealt a difficult hand[1355] – products were licensed, as they should not have been; NHS concentrates, undoubtedly safer, were not produced in sufficient quantities as they should have been; pool sizes from which products were made were allowed to grow and grow, and with them the risks they posed; research into viral inactivation was inadequately resourced and not sufficiently encouraged; domestic products were made from pools containing plasma donated by prisoners and other high risk groups, and insufficient was done to avoid this; the official rhetoric was that of reassurance rather than realism; decisions as to continued importation of factor concentrates were deeply flawed in the manner they were taken and the logic applied to take them; there was no review of these decisions as had been promised; dumping of riskier commercial products was permitted. It is clear that clinicians such as Dr Parapia (Bradford) and Dr Chisholm (Southampton) would have welcomed guidance and were not given it. Individual directors – in particular reference centre directors – contributed to some of these failings, quite apart from failures in their own treatment of patients, for they influenced a number of those decisions. They influenced the rhetoric. They influenced the fierce dismissal of messengers of bad news such as Susan Douglas writing in The Mail on Sunday. They contributed to a climate in which other treating clinicians understood the guidance to be simply to carry on as before.
The complex web of shortcomings described in brief above which led to infections occurring when they should not have done is addressed elsewhere in this Report. It means that others share some responsibility for what occurred. Nonetheless, the “front line” of treatment was the haemophilia clinician. Difficult hand though they might have been dealt, most fell short. They failed to adjust treatment policies as should have occurred; failed to tell patients adequately of the risks to them as individuals; and when infections were known, frequently failed to tell the patient concerned as soon as they reasonably could, or appropriately.
Much of what has been set out in this chapter so far has focused on the treatment of Haemophilia A, not least because of the extensive use of imported commercial factor concentrates in the treatment of people with Haemophilia A. Imported concentrates were not usually a feature of the treatment of people with Haemophilia B in the 1970s and 1980s because the UK was largely self-sufficient in its supply of Factor 9.
Haemophilia B, originally referred to as “Christmas disease”,[1356] is a bleeding disorder caused by a deficiency of Factor 9. “The biological roles of Factors 8 and 9 are closely related ... and so the clinical picture that is caused by these deficiencies is near identical.”[1357] Prior to 1952 patients were categorised under a generic diagnosis of haemophilia, but by 1952 it was possible to identify Haemophilia B as separate from Haemophilia A. Haemophilia B is, however, less common than Haemophilia A.[1358] As with Haemophilia A, Haemophilia B can be classed as severe (<1% Factor 9), moderate (levels of 1-5%) and mild (>5%): there are roughly six times as many people with severe Haemophilia A as suffer from severe Haemophilia B.
Prior to the availability of Factor 9 concentrates, treatment of Haemophilia B was with fresh frozen plasma (“FFP”).[1359] Tranexamic acid (but not DDAVP)[1360] could also be used in the treatment of Haemophilia B.
Factor 9 concentrates were first used in the UK in 1960. They were prepared by Dr Biggs, Dr Ethel Bidwell and colleagues at the Blood Coagulation Research Unit in Oxford using residual material derived from the plasma fractionation process at BPL.[1361]
According to Dr Rizza in his report for the HIV Haemophilia Litigation:
“Throughout the 1960’s supplies of NHS Factor IX were limited and were reserved mainly for patients undergoing surgery. From 1969 onwards there was a slow increase in the availability and use of NHS Factor IX in the UK from approximately 0.5M units in 1969 to 18M in 1988. The United Kingdom has been self sufficient in Factor IX since about 1970 and there has been little usage of commercial Factor IX except for a short period in 1985 when some Directors of Haemophilia Centres purchased commercial Factor IX in preference to NHS Factor IX because the commercial material had undergone heat treatment.” [1362]
As availability of NHS Factor 9 increased, its regular administration became a possibility. At the haemophilia centre directors’ annual meeting in April 1971, there was a general feeling among directors “that regular administration of factor IX to severely affected Christmas disease patients was beneficial.” Regimes of “weekly, fortnightly or even monthly administration had been tried with success”and such treatment “was to be recommended for the very severely affected Christmas disease patient whenever this was possible.”[1363]
As the 1970s progressed, home therapy with Factor 9 concentrates became a feature of the treatment of people with Haemophilia B.[1364] So too, to an extent, was prophylaxis.[1365] The usage per person increased year by year.
In January 1977, Dr Bidwell of PFL reported that whilst she had in 1972 estimated the Factor 9 requirements to be about 5,000 bottles a year, by 1976 nearly 10,000 bottles were used. She explained to those directors whose Factor 9 requirements had increased substantially that “present arrangements for production of factor IX and level of funding did not allow for prophylactic treatment except for occasional short periods of time.” However, “prophylaxis for severely affected patients may not be excluded if it were shown not to result in substantial increased usage.”[1366]
By 1976 Factor 9 concentrate was the dominant treatment with comparatively little use of FFP.[1367] By October 1977 the amount of Factor 9 concentrates being issued from the PFL at Oxford was said still to be rising although showing signs of levelling off,[1368] and in 1978 and 1979 there were increases in total usage, though at a much smaller rate. The average amount used per patient stabilised at 20,300 units (compared to just under 19,000 in 1976).[1369] The increase in overall usage was possibly due to the number of children who were growing and therefore requiring more treatment “but in general there was no clear-cut reason for the increase in usage.”[1370] By 1978 there were approximately 87 Haemophilia B patients on home therapy.[1371]
There was then an increase in 1980 both of the overall amount used and the average per patient. 367 patients were treated (including 12 carriers of Haemophilia B), with a total of 8,387,000 units of Factor 9: mostly with NHS Factor 9 (8,307,000 units), with a tiny amount of FFP (3,000 units) and an increase in commercial Factor 9 concentrates (77,000 units), though the usage of this remained less than 1% of the total. The average used per Haemophilia B patient was now 22,853 units.[1372] Patients on home treatment (of whom there were 143 during the year – an increase of over 60% from 1978, a significant increase over two years) received an average of 29,685 units.
1981 saw a further increase. 378 patients (including 10 carriers) were treated with 9,899,000 units of Factor 9: again mostly with NHS Factor 9 (9,874,000), with a tiny amount of FFP (2,000 units) and 23,000 units of commercial concentrates (less than one quarter of 1% of the total). The average amount used per Haemophilia B patient was 26,188 units – representing an increased use of Factor 9 concentrates[1373] despite this being the year following the Glasgow symposium (which should, as described earlier in this chapter, have reinforced to clinicians the risks of hepatitis transmission). Patients on home treatment (of whom there were 157 during the year) received an average of 33,210 units. This upward trend continued in 1982-84, as detailed in the next three paragraphs.
In 1982, 379 patients (including 9 carriers) were treated with 9,281,000 units of Factor 9, all of which was NHS concentrate apart from 5,000 units of plasma used to treat carriers. The average used per patient with Haemophilia B was 24,488 units, a slight decrease from the previous year. There were 164 patients on home treatment, who received an average of 32,927 units.[1374]
In 1983, 382 patients (including 12 carriers) were treated with 10,895,000 units of Factor 9, all of which was NHS concentrate apart from 9,000 units of FFP. The average used per patient with Haemophilia B was 29,241 – an increase on the previous year. There were 167 patients on home treatment, who received an average of 37,569 units.[1375]
In 1984, 403 patients (including 12 carriers) were treated with 12,114,000 units of Factor 9, all of which was NHS concentrate apart from 17,000 units of FFP. 7,000 units of Autoplex were also used. The average used per patient with Haemophilia B was 30,060 units, an increase on the previous year. There were 186 patients on home treatment, who received an average of 36,392 units.[1376]
The picture changed markedly in 1985, no doubt in consequence of the AIDS Advisory Document. 401 patients (including 15 carriers) were treated with 10,675,000 units of Factor 9. The amount of FFP used remained low (27,000 units). Most patients were still treated with NHS Factor 9 – much of which would not have been heat treated – totalling 7,750,000 units but a substantial quantity of treatment (2,898,000 units) was with commercial concentrates, presumably those which had been heat treated. The average used per patient with Haemophilia B was 26,621 units. 193 patients were on home treatment, receiving an average of 32,119 units of Factor 9.[1377]
In summary, the average usage of Factor 9 per patient rose from 21,000 units in 1978 to 30,060 units in 1984 (a figure almost half as much again). The numbers on home therapy rose from 87 to 186. Almost all of the treatment during that period was provided by NHS concentrate. What followed in 1985 might suggest that treatment at that level was more than was thought strictly necessary, for the average amount per patient dropped by 12% overall and for those on home treatment. The largest criticism, however, is that the figures show that the heightened awareness of serious long-term consequences caused by hepatitis as a result of using pooled concentrates demonstrated in the Glasgow symposium had had no obvious effect on practice. To the contrary, as the risk of long-term disease grew greater, so did prescription of the amount of product causing it.
| Year | Patients treated | |||
|---|---|---|---|---|
| Total patients | Patients with Haemophilia B | Carriers | Patients on home therapy | |
| 1978 | 337 | 330 | 7 | 87 |
| 1979 | 342 | 331 | 11 | 125 |
| 1980 | 367 | 355 | 12 | 143 |
| 1981 | 378 | 368 | 10 | 157 |
| 1982 | 379 | 370 | 9 | 164 |
| 1983 | 382 | 370 | 12 | 167 |
| 1984 | 403 | 391 | 12 | 186 |
| 1985 | 401 | 386 | 15 | 193 |
| Year | Average number of units per patient | ||||
|---|---|---|---|---|---|
| Total units | NHS Factor 9 | Fresh frozen plasma | Commercial Factor 9 | For patients on home treatment | |
| 1978 | 20,300 | 20,175 | 92 | 33 | Data not available |
| 1979 | 20,273 | 20,269 | 4 | 0 | |
| 1980 | 22,853 | 22,635 | 8 | 210 | 29,685 |
| 1981 | 30,060 | 26,122 | 5 | 61 | 33,210 |
| 1982 | 28,521 | 24,475 | 13 | 0 | 32,927 |
| 1983 | 28,521 | 28,497 | 24 | 0 | 37,569 |
| 1984 | 30,060 | 30,017 | 42 | 0 | 36,392 |
| 1985 | 26,621 | 19,327 | 67 | 7,227 | 32,119 |
In Scotland, the supply of Factor 9 concentrates from the PFC was, according to a January 1981 report from Dr Cash, “always more than adequate”.[1378] The amount of PFC Factor 9 (DEFIX) supplied doubled from 500,000 international units in 1975 to 1,000,000 international units in 1980. Dr Cash continued: “Several reports have implied that the risks of transmitting agents likely to cause hepatitis is higher for factor IX than VIII concentrates. The evidence is not firm but may relate to differences in pool size (the former usually being larger). Nevertheless, continuing efforts are being made to improve matters and a stage has been reached at P.F.C. when clinical studies will soon be required.” Haemophilia B patients were described as “a high risk group for hepatitis”.[1379]
The report also recorded that a new Factor 9 product – Supernine – was at an advanced stage of development: “Further purification of DEFIX has led to a product which we believe may be both safer with regard to virus transmission and thrombogenicity.”[1380]
The Scottish Haemophilia and Blood Transfusion Working Group discussed, at its meeting on 4 March 1981, the setting up of clinical studies of Supernine. The West and South East Regions were reported to have access to a limited amount of Supernine and a licence had been given for clinical trials. The “main aim was to obtain a product licence.” A discussion also took place about ways of determining quantities of Factor 9 concentrates used in Haemophilia B and non-Haemophilia B patients on an annual basis, Dr Cash expressing concern about the inadequate tracing of patients and lack of available data. It was agreed that “there should be an effective method of monitoring blood products, recording what product is given to a patient and how the products are used.”[1381]
The minutes of the meeting of SNBTS directors and haemophilia directors on 21 January 1983 reported that the supply position of DEFIX over the last five years “had remained strong and the demand reasonably stable.” The clinical studies on Supernine “had produced excellent results” and it was not thought necessary to obtain a separate product licence, as a variation of the DEFIX licence on a named patient basis was considered sufficient. It was also reported that studies of heat treatment, to reduce hepatitis risk, were currently underway using Supernine, but the rate of progress would be slower than with Factor 8 because of the need to submit the heated Factor 9 concentrate to intensive animal studies to assess thrombogenicity.[1382]
Hepatitis (both B and non-A non-B) was transmissible by Factor 9 concentrates in the same way as Factor 8 concentrates. This is illustrated by a study undertaken at Oxford on the epidemiology and chronic sequelae of Factor 8 and Factor 9 associated hepatitis in the UK.[1383] The second annual report on this study explained that, in addition to the follow up of 148 patients at Oxford receiving long-term Factor 8, Haemophilia B patients on NHS Factor 9 therapy had also been assessed. A table in Appendix II to the report provided details of changes in liver function tests in Oxford patients on regular treatment with Factor 9 concentrate in 1980: of 16 patients, 7 (44%) had persistently abnormal Aspartate Aminotransferase (“AST”) levels. Two of those (12.5% of the total cohort) had a persistently abnormal AST level of more than 70 international units per litre, double the upper range of normal for the study.[1384]
Three features emerge from the above narrative. The first is that as the 1970s progressed treatment for patients with Haemophilia B was increasingly with Factor 9 concentrates rather than FFP, ie with a product made from large donor pools rather than from single donations. The second is that the pools used for the production of Factor 9 were at times larger than the pools used for the domestic production of Factor 8.[1385] Thus, Dr Rainsford (at Treloar’s), writing in 1975 to a consultant at Great Ormond Street about the increased incidence of jaundice amongst boys with Haemophilia B, remarked that: “We have always assumed that this is due to the fact that the Christmas boys are almost invariably transfused with high potency factor IX prepared with material from large donor pools. However, I think this is a debt we shall have to continue to pay, since this high potency concentrate is so effective and no case of hepatitis that we have experienced can be regarded as even moderately severe”[1386] and in 1976 Dr Maycock gave Dr Bidwell authorisation to increase the pool size for Factor 9 beyond that for Factor 8 so that one batch reached the capacity of the freeze dryer.[1387] The third is that the increasing use of home therapy and, to some extent at least, therapy on a prophylactic basis, meant that Haemophilia B patients were being treated with progressively greater amounts of concentrates than was previously the case – with, inevitably, a progressively increasing risk of hepatitis.[1388]
As discussed earlier in this chapter, the risk of hepatitis was well known and by the late 1970s, if not earlier, the potential for non-A non-B Hepatitis to have serious effects should have been appreciated in relation to Factor 9 concentrates just as much as in relation to Factor 8. It may be that, as a consequence of the combination of two elements, infections were less visible. First, the numbers of those who had Haemophilia B were significantly fewer than those who had Haemophilia A, and those whose condition was classed as severe only one-sixth as many. Second, though, and possibly most significant of all, the UK was self-sufficient in Factor 9 almost throughout the entire period. Though some commercial concentrate was procured, the percentage of it was so small that it can confidently be said that 99% or more of the product used was NHS (until heat treatment led to commercial concentrates filling the gap for a while).
Less visible though cases of infection in those with Haemophilia B may have been in comparison with Haemophilia A, many similar issues contributed to infections continuing to arise, and the numbers in which they did. Viral inactivation was as necessary; so too was giving thought to the size of the pool from which Factor 9 concentrates were made. Pool sizes increased for both Factor 8 and Factor 9 during the 1970s, to the extent that the pool sizes in the late 1970s were at least seven times, and often more, than they had been at the start of the decade, and well in excess of the figures regarded from 1952[1389] as the highest to secure reasonable safety. There is one point to note here though: whereas with Factor 8 pursuing a goal of self-sufficiency led to a desire to have larger pools, in the case of Factor 9 production this reason could not apply. This is because self-sufficiency was effectively secured. Pool sizes nonetheless were increased relentlessly.[1390]
Notwithstanding the growing knowledge, in the second half of the 1970s and into the early 1980s, of the potential seriousness of non-A non-B Hepatitis, there was no appreciable change in the approach to treatment of patients with Haemophilia B.
The minutes of the special meeting of haemophilia reference centre directors on 13 May 1983 contain no reference to the use of Factor 9 concentrates or the treatment of patients with Haemophilia B at all.[1391] However, the recommendations subsequently circulated on 24 June 1983 by Professor Bloom and Dr Rizza referred to two matters having been drawn to their attention since the 13 May meeting: “The first concerns the treatment of patients with haemophilia B. The evidence to incriminate factor IX concentrates in AIDS is even less than with factor VIII and it seems logical to continue to use our normal supplies of NHS concentrate.”[1392]
This is both a revealing and disappointing comment. There was no logical reason for thinking that Factor 8 could transmit the virus responsible for AIDS but that Factor 9 could not: the route of transmission was identical. There was reason, knowing that Factor 9 concentrates were made domestically from plasma which had been voluntarily donated, to think that it might be safer for that reason though it would not necessarily make the products entirely free of virus: but the words used combine a “continue as before” approach for Factor 9 with an emphatic dismissal of the idea that there was any substantial evidence to implicate Factor 9, which was irresponsible at the time.
In other words, “no change”: clinicians should go on treating patients with Haemophilia B with Factor 9 concentrates, even though careful and conscientious consideration of the position should have led to the conclusion that Factor 9 was capable of infecting patients with the cause of AIDS.
No further advice at all was issued by UKHCDO until the production of the AIDS Advisory Document, following the meeting at Elstree on 10 December 1984.[1393]The AIDS Advisory Document recorded that various commercial heat-treated Factor 9 concentrates were available:“Profilnine (heated) (Alpha), heated Konyne (Cutter) and Immuno (heated Prothromplex) are available at prices up to 20p a unit but the effects on efficacy and thrombogenicity are unpublished. Since AIDS and laboratory changes seem (controversially) to be less common in Christmas disease than haemophilia A no firm recommendation can be given on heated factor IX.”[1394]
The following treatments for Haemophilia B were recommended:
It was further generally advised that “In individual patients there may need to be a choice. In general heated concentrate appears to be the recommendation of virologists consulted but individual Directors may wish to make up their own minds. This is particularly true of unheated NHS material.”[1395]
Some clinicians began to switch from unheated NHS Factor 9 to commercial heat-treated Factor 9. The AIDS Group of haemophilia centre directors, at their first meeting on 11 January 1985, recorded “some difference of opinion with regard to factor IX. Some Centres had stopped using NHS factor IX and were now using heated commercial factor IX while others intended to continue for the meantime with the unheated NHS factor IX.”[1396]
By the time the AIDS Group held its fifth meeting on 17 June 1985, it was reported that most reference centres had transitioned to using commercial heat-treated Factor 9, and at this meeting the Group agreed that a recommendation should be made to haemophilia centre directors to use only heat-treated products.[1397] Professor Bloom switched at this time to heat-treated Factor 9.[1398]
The annual returns data which the Inquiry has examined confirm that heated commercial Factor 9 concentrates began to be used on a named patient basis in centres in the course of 1985, but that centres also continued to use unheated NHS Factor 9.[1399]
It was not until October 1985 that all Factor 9 issued by BPL had undergone heat treatment. Dr Snape explained that:
“BPL was more cautious in the evaluation of heat treatment on our Factor IX concentrate (the unheated concentrate was coded ‘9D’, the heated product ‘9A’). Although the programme of work began at the end of 1982, the heated product 9A was only released for clinical trial in selected centres in July 1985, three months after the first trial batches of 8Y. We were especially concerned to rule out the potential for thromboembolic sequelae that might be caused by activated factors produced on heat treatment of the 9D product. Prothrombin complex concentrates in general had a history of association with problems of this sort and we were concerned that the risk might be increased by heating the concentrate.”[1400]
He confirmed that heated Factor 9 (9A) was first issued by BPL in July 1985 (for a limited clinical trial of safety and efficacy only), and that all Factor 9 issued after 2 October 1985 was heat treated. Dr Snape’s understanding was that during the first nine months of 1985 most treatment centres continued to use the BPL unheated product, although heat-treated commercial Factor 9 products were available.[1401]
28 people with Haemophilia B were infected with HIV, 18 of them with severe Haemophilia B, 9 with moderate Haemophilia B and 1 with mild Haemophilia B.[1402] Many more were infected with Hepatitis C.[1403]
Given that the ratio of people with Haemophilia B to Haemophilia A in the UK is, and was, roughly 1:6, this indicates that commercial concentrates were more dangerous than NHS products: the ratio of those who were infected was 1:9, meaning that people with severe Haemophilia A, who as a group were treated with a mix of commercial and NHS products, were nine times more likely to be infected than people treated predominately with NHS products for severe Haemophilia B.[1404] There is a noticeable echo here of observations made by Professor Joseph Garrott Allen in his writings and letters in the late 1960s and 1970s. In 1966, he compared the rates of hepatitis of those receiving blood from people who had sold it with those receiving it from people who had freely donated. He concluded that it was around ten times more likely that the first group would suffer hepatitis than the second.[1405] Of course, this related to the US. Of course, it related to blood, not to blood products manufactured from plasma. Of course, since then some testing had been required by the FDA, which required radioimmunoassay screening of plasma. And of course, this was a different virus. But the essential message remained the same: buyer beware. A product made from pools which had been contributed to by people who had sold their blood was inherently less safe.[1406]
The consequences in terms of the numbers of infections that occurred may have been known only in retrospect. However, the purpose of referring here to Professor Garrott Allen’s work is to show that it was entirely predictable. It supports the importance of seeking self-sufficiency.
It is also worth noting that although there was much less to be said in favour of fresh frozen plasma as a form of alternative treatment than there is to be said for considering cryoprecipitate as an alternative to Factor 8 concentrate (it had to be administered in large volumes to be effective, and that created its own risks), nonetheless in the guidelines circulated after 10 December 1984 it was recommended as the treatment of choice for mild cases of Haemophilia B, previously untreated patients, and children. There was plainly some role for it, even if relatively limited.
A step that could and should have been taken, but was not, would have been to limit home treatment and suspend prophylaxis using unheated Factor 9 concentrates at least until it either became clear that there was in truth no real risk that unheated NHS Factor 9 concentrates could transmit the cause of AIDS (although as we now know, that moment never arrived) or until (as happened in 1985) it became possible to provide a reliably safe heat-treated product. Other steps that, as with Haemophilia A, could and should have been taken included adopting a conservative approach to treatment, deferring elective/non-essential surgery, and most importantly discussing the risks and alternatives with each patient individually so that they could take an informed decision as to whether or not to accept the risks of treatment.
By the time heat-treated Factor 9 concentrates became widely available, it was too late
for some.
Von Willebrand disorder (“VWD”) is the most common inherited bleeding disorder and affects people who have a deficiency of functional von Willebrand Factor (“VWF”). VWF is a protein. Its job is both to carry Factor 8, and to enable it to take effect when a clot is needed. Without sufficient VWF, the Factor 8 in the bloodstream cannot play an effective part in the clotting process. People affected by von Willebrand disorder thus have most of the symptoms of a shortage of Factor 8. Their blood will not clot, or if it does, will take longer to do so. Symptoms include easy bruising and mucous membrane bleeding (mouth, nose, gastrointestinal tract, menstrual bleeding).
Because VWF is responsible for carrying Factor 8, some people also have low Factor 8 levels, which also hinders clotting. Von Willebrand disorder affects thousands of people in the UK.[1407] Whereas haemophilia is inherited (caused by a defective X chromosome, and thus much more prevalent in males) VWF disorder affects males and females equally, though women may experience a greater number of problems linked to periods, pregnancy and childbirth.[1408]
There are three main classifications of VWD:
Prior to the 1970s, treatment of patients with von Willebrand disorder was mainly with FFP or cryoprecipitate.
In January 1977, haemophilia centre directors agreed, following a suggestion from Professor Bloom, that their annual returns to the haemophilia database would include data relating to patients with von Willebrand disorder.[1410] The annual returns for 1976, which were the first to be supplied in respect of VWD, show that cryoprecipitate was at that stage the dominant treatment, with some use of concentrates (including commercial ones) and comparatively little use of FFP.[1411]
In 1977 it was reported, following a trial, that desmopressin (“DDAVP”)[1412] infusion caused a marked increase in Factor-8-related properties in patients with moderate and mild haemophilia and von Willebrand disorder. The administration of DDAVP before dental surgery and in the early postoperative period was followed by a two- to threefold rise in Factor 8 coagulant activity and led Professor Pier Manucci to write in The Lancet that DDAVP could be “a promising pharmacological alternative to plasma concentrates in the management of some patients with haemophilia and vWd.”[1413] Professor Hay, who in 1977 was working as a senior house physician in Sheffield, recalled “administering probably the first dose of DDAVP we had used in Sheffield for this indication in 1977 to correct von Willebrand’s disease prior to a minor procedure.”[1414]
By the end of 1978 the total number of patients with von Willebrand recorded on the annual returns had increased to 240. Cryoprecipitate was still the most common treatment, although there had been a significant increase in the use of NHS factor concentrates from 41,025 units in 1976 to 171,000 units. The average amount used per patient increased from 4,282 to 6,000 Factor 8 units.[1415] By the end of 1979, although the average amount of Factor 8 units used per patient had decreased slightly to 5,250 (for 233 patients treated), the number of units of cryoprecipitate had decreased markedly (673,500 in 1979 compared with 1,030,000 units in 1978) and there was a considerable increase (fourfold) in the number of units of commercial concentrates used (334,000 units in 1979 compared with 79,000 units in 1978).[1416]
At the haemophilia centre directors’ meeting on 20-21 November 1979, it was unanimously agreed that a working party on von Willebrand disorder should be set up. It was noted that the first problem for the working party “would be to define what von Willebrand’s disease was” due to difficulties in diagnosing people with the disorder and the variants of the disorder which had been reported. Centre directors were also reminded that the computer file at Oxford contained only the details of people with von Willebrand disorder who had been treated, but the number of those with the disorder who had not received treatment was unknown.[1417]
In 1980 data on home treatment for patients with von Willebrand disorder was collected for the first time from haemophilia centres. The annual returns for that year show that 271,000 units were used for home treatment, out of a total of 1,427,000. Cryoprecipitate was still the most common treatment and the number of units had increased again to 1,052,000 – a level similar to the amount used in 1978. However, the amount of commercial concentrates used (258,000 units) was more than twice the amount of NHS Factor 8 (113,000) and the amount of FFP continued to reduce (4,000 units).[1418] This trend continued into 1981, where the annual returns show that FFP usage was down to 3,000 units, cryoprecipitate accounted for 1,327,000 of the total of 2,193,000 units used to treat 282 patients with VWD, and commercial concentrate continued to be the next treatment preference (601,000 units) whereas NHS concentrate accounted for 262,000 units. This overall increase in the amount of product used meant the average amount used per patient rose to 7,776 units.[1419]
In a letter to Stanley Godfrey of the DHSS in October 1981, Professor Bloom outlined that cryoprecipitate (either frozen or freeze-dried) “is still the treatment of choice in most patients with von Willebrands disease.” The letter sought to correct a set of meeting minutes which seemed “to imply that intermediate-purity concentrate would be generally acceptable to treat von Willebrands disease rather than cryoprecipitate.” Professor Bloom thought the minutes ought to be amended to reflect that concentrate should be viewed as an “acceptable substitute”.[1420]
In 1982, 258 patients were treated with 2,329,000 units of Factor 8, which consisted of 1,254,000 units of cryoprecipitate, an increase to 45,000 units of FFP, 650,000 units of commercial concentrate and 380,00 units of NHS concentrate. The average amount used per patient rose to 9,027 units – an increase on the previous years. There were 14 patients on home treatment who received an average of 43,286 units (26% of the total units used).[1421]
The annual returns for 1983 reported for the first time the number of patients with VWD known to haemophilia centres in the UK. This was also the first year that data relating to the patient’s age and Factor 8 level were included within the annual returns. Patients were treated with 1,373,000 units of cryoprecipitate, 49,000 units of FFP, 408,000 units of NHS concentrate and almost the same number of units of commercial concentrate (428,000 units) – a decrease from the previous year. 1,570 patients were registered with haemophilia centres, of whom 314 were treated. 17 were on home treatment and received a total of 691,000 units which accounted for 30% of the total number of units used. The average amount used per patient decreased to 7,260 units.[1422]
DDAVP was licensed for the treatment of haemophilia and VWD in 1982, but was available to be used (and was used in some centres) on a “named patient” basis prior to that.[1423] Professor Hay recalled that during the late 1970s and early 1980s, centres explored and learned how to use DDAVP and learned its strengths and limitations: “Its use was well established in Sheffield when I joined in 1983 and it was used wherever the response was considered adequate.”[1424]
In the haemophilia centre directors’ meeting on 30 September 1980, Dr Craske reported that “Large pool concentrates appeared to give a higher risk of hepatitis than small pooled concentrates”. He felt that increased usage of small pooled concentrates would help reduce the incidence of hepatitis in the haemophilic population and reported that “First-time exposure to large pooled factor VIII concentrate resulted in many cases of hepatitis, especially in von Willebrand’s disease patients.” In response, Professor Bloom “wondered whether cryoprecipitate would be a better product to use for mild haemophiliacs and von Willebrand’s disease but pointed out that there was a problem over the amount of factor VIII in these materials.” Dr Craske agreed and said that the NHS material was “certainly better” than commercial products “because of the screening of the blood donors and the regular donor panels which were used in the UK.”[1425]
At the haemophilia centre directors’ annual meeting in September 1982, at which AIDS was mentioned for the first time, there was a discussion about the treatment of von Willebrand disorder with commercial Factor 8. Professor Bloom commented that much of the commercial concentrate used in such treatment had been for a patient with inhibitors in Cardiff. He felt that the figures for the usage of commercial concentrate in von Willebrand disorder in the annual returns were heavily biased by the treatment for this one patient. At the same meeting Dr Tuddenham presented the Working Party’s report which involved a survey of the condition in the UK. Clinical and laboratory information had been received so far on 557 patients with von Willebrand disorder.[1426]
The recommendation in the letter (discussed earlier in this chapter) from Professor Bloom and Dr Rizza to all haemophilia centre directors on 24 June 1983 was that “For mildly affected patients with haemophilia A or von Willebrand’s disease and minor lesions, treatment with DDAVP should be considered.” The letter suggested that this was the usual practice of many directors, because of the “increased risk of transmitting hepatitis by means of large pool concentrates in such patients.”[1427]
The treatment guidelines produced in Cardiff in May 1983 recommended that patients with von Willebrand disorder should be treated with DDAVP for minor lesions (such as teeth extractions), and cryoprecipitate or NHS Factor 8 “for other lesions as rational e.g. cryo for vWd and for in-patients; NHS FVIII conc. for outpatient mild haemophiliacs.”[1428]
At the annual meeting of haemophilia centre directors on 17 October 1983, Dr Rizza presented a report on the 1982 annual returns, following which “The materials used for the treatment of von Willebrand’s disease patients was discussed and it was suggested that it would be useful for information on the use of DDAVP in von Willebrand’s disease patients to be included in the next report.” It was recorded that “There was a clear bias towards the use of cryoprecipitate for the treatment of Von Willebrand’s disease patients”and that “The majority of Directors limited the use of concentrate in von Willebrand’s disease patients to reduce the risk of hepatitis.”[1429]
The AIDS Advisory Document produced following the meeting at Elstree on 10 December 1984 recommended directors to “Use DDAVP in mild Haemophilia A and vWd if possible.”[1430]
The annual returns reveal a mixed picture. Some centres did not routinely record DDAVP usage on their return, and it is therefore difficult to gauge with precision the extent of its usage. It was noted in Dr Rizza’s annual returns report for 1983 that only some centres had used “other products” and that “Doubtless, this table does not reflect the full use of these products at Centres.” Centre directors were asked to ensure that all the products given to their patients were noted in the annual returns for 1984 onwards.[1431] The data for 1983 recorded 45 VWD patients as having been treated with DDAVP.
In 1984, 1,725 patients with VWD were registered with centres, 302 of whom were treated with 16 patients on home treatment. There was a significant decrease in the use of FFP (3,000 units) and the amount of cryoprecipitate used almost doubled (2,273,000). NHS concentrates accounted for 244,000 units and there was a further decrease in the amount of commercial concentrate used (137,000 units). The total number of units used was 2,657,000, which put the average amount used per patient at 8,857 units.[1432] The use of DDAVP was not included in Dr Rizza’s report for 1984.
In 1985, 1,877 patients with VWD were registered with centres, 273 of whom were treated, with 15 patients on home treatment. FFP accounted for 5,000 units and there was a significant decrease in the use of cryoprecipitate compared with the previous year, with 1,062,000 units being used. NHS concentrates accounted for 248,000 units (a slight increase on the year before). However, the amount of commercial concentrate used trebled (465,000 units). The total number of units used was 1,78,000 which put the average amount used per patient at 6,667 units.[1433] Again the use of DDAVP was not included in the annual returns report for 1985.
| Year | Number of patients | Proportion of patients treated with DDAVP when recorded | Average number of units per patient | ||||
|---|---|---|---|---|---|---|---|
| Total Units | Fresh frozen plasma | Cryo-precipitate | NHS Factor 8 | Commercial Factor 8 | |||
| 1978 | 240 | Not recorded | 5,400 | 67 | 4,292 | 713 | 329 |
| 1979 | 233 | Not recorded | 5,249 | 28 | 2,891 | 897 | 1,433 |
| 1980 | 238 | Not recorded | 5,996 | 17 | 4,420 | 475 | 1,084 |
| 1981 | 282 | Not recorded | 7,777 | 11 | 4,706 | 929 | 2,131 |
| 1982 | 258 | Not recorded | 9,027 | 174 | 4,860 | 1,473 | 2,519 |
| 1983 | 311 | 14% | 7,260 | 158 | 4,415 | 1,312 | 1,376 |
| 1984 | 300 | Not recorded | 8,857 | 10 | 7,577 | 813 | 457 |
| 1985 | 267 | Not recorded | 6,667 | 19 | 3,978 | 929 | 1,742 |
| 1986 | 271 | Not recorded | 7,229 | 18 | 5,812 | 768 | 631 |
This data can be seen in Figure 1.
DDAVP gave rise to no risk of viral transmission: it was not a biological product. It was available from 1977 onwards, licensed in 1982 and was one of a number of alternative treatments which ethically required to be discussed with a patient in advance of treatment, together with the other possibilities. The meetings of haemophilia clinicians in 1980, 1982 and the advice given in June 1983 all show that haemophilia clinicians were alive to the risk that using concentrates, especially commercial concentrates, risked transmitting viral infection and should best be avoided if possible. Yet people with von Willebrand disorder were (like people with Haemophilia A or B) typically not given advice or information about the risks of treatment (insofar as those risks related to transmission of hepatitis or HIV) and were not given information about safer alternatives. The evidence available to the Inquiry indicates that DDAVP was not used to the extent that it should have been, given the risks of viral transmission, and that concentrates (including commercial concentrates) were used more frequently than they should have been for the treatment of people with von Willebrand disorder, particularly after the risks of AIDS had become apparent from mid 1982 onwards.
By way of example:
Pauline Nicholson received Factor 8 concentrate in November 1983: she was not aware of the time what treatment she was receiving: “I was given an injection, not being told what it was or what it was for.”[1434]
One woman treated from the 1970s recalls first receiving snake venom, then cryoprecipitate. A letter in 1979 had recommended a trial use of tranexamic acid, which would avoid “the necessity of repeated injections of cryoprecipitate with the slight risk of hepatitis or plasma reactions”.[1435] However, she was treated in 1981-82 with Factor 8 concentrates as a result of which she was infected with Hepatitis C.[1436]
Catherine Slater was infected with HIV, Hepatitis B and Hepatitis C following treatment with cryoprecipitate from the late 1970s; she began home treatment in 1980: “No information or advice was provided to me, my parents or my sister before treatment about the risk of being exposed to infections”.[1437]
Beryl Partington’s son Nick Anderton was treated with Factor 8 concentrates from the age of 4: “During the time that Nick was being treated with Factor VIII, I was never told about the risk of infection”. Nick was infected with HIV.[1438]
Ian Joy (who had “a diagnosis of von Willebrand’s disease, although he does not have any obvious bleeding tendency”) received prophylactic Factor 8 and cryoprecipitate during an operation in autumn 1984.[1439] His mother “had no idea that one treatment was a batch comprised of hundreds of donations ... He was just a child in 1984 and as his parents, we should have been fully informed of all possibilities and risks.”[1440]
One woman with mild von Willebrand disorder was treated with prophylactic cryoprecipitate over a period of days in 1987 “just in case” and with no advice or information regarding safety. She was infected with Hepatitis C.[1441]
Melanie Richmond was treated with Factor 8 concentrate for the first time in 1989, having previously been given cryoprecipitate or DDAVP. In 1992 she was told casually, whilst admitted to hospital, having been “taken into an isolated cubicle which had contamination labels everywhere”, that she had been infected with Hepatitis C.[1442]
14 people with von Willebrand disorder were infected with HIV according to the National Haemophilia Database records.[1443] Many more were infected with Hepatitis C.
Heat-treated Factor 8 concentrate produced by PFC (known as NY) was available from December 1984. It was believed to (and did) inactivate HIV; it did not, however, prevent the transmission of non-A non-B Hepatitis. It was not until April 1987 that PFC produced a Factor 8 concentrate (Z8) that was effective against non-A non-B Hepatitis. By contrast the heat-treated concentrate produced by BPL (8Y) over the same period transmitted neither HIV nor non-A non-B Hepatitis.
Thus there was in Scotland a continuing need for particular care to be taken by clinicians in relation to people with bleeding disorders who were untreated or minimally treated and who thus had not been, or were unlikely to have been, previously exposed. Haemophilia clinicians should have been alert to this, so as to avoid such patients receiving NY unless absolutely necessary. Appropriate systems should have been in place to address this. If such a patient were to be offered NY, they needed to be told in advance of their treatment what the options were (including the possibility of alternative treatment eg with DDAVP or cryoprecipitate), what the risks and benefits were, and in particular they should have had explained to them what by now was on any view abundantly clear – that non-A non-B Hepatitis was a serious illness which could cause long term (and potentially fatal) liver disease and that treatment with NY would in all probability infect them with it.
In May 1986 Bill Wright, who had mild haemophilia and had not previously been treated with blood products, was treated at the Edinburgh Royal Infirmary with NY. He was not offered any alternative treatment. He was not provided with any information about the risks of the treatment. He was infected with non-A non-B Hepatitis in consequence of that treatment.[1444] That should never have happened.[1445] As recorded in a letter from Dr Frank Boulton to Dr Robert Perry in June 1986, “A young haemophiliac who previously had minimal[1446] therapy with factor VIII received an infusion of the current heat-treated product a month ago. He now shows signs of liver enzyme rises indicating non-A, non-B hepatitis. Christopher [Ludlam] is a bit ruthful with his own staff about this because he feels that this patient should have received VIIIY or an equivalent product.”[1447]
8Y, the product developed at BPL, was heat-treated at a higher temperature and for longer than the PFC product, and there was evidence available by 1986 to suggest that it was showing itself to be effective against non-A non-B Hepatitis. There had been an initial report of encouraging signs in July 1985[1448] and an information sheet was sent to haemophilia centre directors and to regional transfusion directors in England and Wales (but not Scotland – although Dr Perry’s evidence to the Penrose Inquiry was that haemophilia centre directors in Scotland would have had access to it through their network of contacts and would have been aware of it).[1449] This information sheet explained that clinical trials at six centres were in progress to gain evidence of reduction or elimination of viral transmission “and several patients have safely passed the point at which first evidence of NANBH virus transmission would normally occur with unheated Factor VIII.” Haemophilia centre directors were asked to compile lists of their patients considered at risk; most centres had already done so. It was “the considered view at BPL” that if possible there should be liaison between haemophilia services and the blood services aiming to direct the supplies of 8Y to those patients considered to be “at risk”.[1450] Professor Ludlam told the Inquiry that he was unaware of this report.[1451]
In December 1985, at a meeting of the CBLA’s Central Committee for Research and Development in Blood Transfusion (attended by Dr Brian McClelland of SNBTS as well as by Dr Forrester on behalf of the SHHD) Dr Rizza reported on the progress of trials using 8Y which had been in use for some nine months: “none of his patients, including children, had become clinically ill and, therefore, the immediate signs were encouraging.”[1452] There is no evidence of this information being shared more widely within Scotland. It should have been, probably by the SHHD.
On 10 January 1986 Dr Perry produced a report, intended for the March meeting of the SNBTS directors and Scottish haemophilia centre directors, which noted that “Directors will be aware that the Blood Products Laboratory are currently issuing a FVIII product which has been heated at 80°/72 hours and preliminary clinical data indicates that this material is non-infective with respect to HTLV III, NANB and Hepatitis B.”[1453] The current PFC product could not, it was explained, be successfully treated under these conditions.
On 17 March 1986 a meeting between representatives of BPL and of SNBTS took place at the PFC. Dr Perry’s note of the meeting records that Dr Smith “outlined clinical trial results of the 8Y F VIII product so far. While results cannot be considered conclusive at this stage, he indicated that no cases of virus infection have occurred (attributable to 8Y material) after 12 months experience of 8Y in virgin haemophiliacs.”[1454] Dr Perry told the Inquiry that it was at this stage that he thought it “likely” that 8Y was successful in terms of not transmitting non-A non-B Hepatitis; his view of the reports was “more optimistic than Dr Smith’s actually. He was always very cautious not to overestimate or be too optimistic about outcomes before the data was confirming it.”[1455] SNBTS, which was aware that its own product continued to transmit non-A non-B Hepatitis, thus now knew that 8Y probably did not. They should have let haemophilia clinicians know this, and not assume (if they did) that they would find out by some other route.
Professor Ludlam did not attend the March 1986 meeting and did not think that he had read Dr Perry’s report.[1456] At some stage before 27 June 1986,[1457] he had a discussion in a corridor with Dr McClelland at which the latter told him he had been at a meeting recently when the preliminary encouraging results with the use of 8Y had been spoken about. Professor Ludlam said this led him to discuss it with other people in SNBTS, resulting in Dr Perry obtaining a small supply of 8Y from BPL.[1458] Professor Ludlam himself obtained a modest amount of 8Y from the Newcastle Haemophilia Centre.[1459] Dr Boulton and Dr Perry appear to have discussed the matter in early July and to have agreed that, whilst the PFC worked on producing a product equivalent to 8Y, “In the meantime, any Edinburgh ‘virgin’ h’philiacs requiring therapy could be given BPL 8Y.”[1460]
All this was too late, however, for Bill Wright.
There was a culpable failure to ensure that haemophilia clinicians were kept informed of the progress of 8Y, and of the increasing confidence in the inactivation of non-A non-B Hepatitis, and to institute a system which would have enabled a small amount of 8Y to be made available to SNBTS or to the Scottish reference centres.[1461] This would have satisfied the requests for 8Y which would inevitably follow information that 8Y might well not transmit non-A non-B Hepatitis, such that if treatment with a Factor 8 concentrate were absolutely necessary for an individual who had received little or no previous concentrate therapy, that treatment could be provided using the product least likely to transmit it.[1462] There is no reason why such a system could not have been in place from July 1985, and there was no justification whatsoever for its absence after March 1986.[1463] Dr Perry reminded the Inquiry that Dr Forbes was then the chair of UKHCDO, an organisation which covered the whole of the UK, and he was a Glasgow clinician: so he would be aware of both the increasingly promising reports of treatment by 8Y, and that BPL could probably be prevailed upon to supply some to Scotland despite issues of finance and supply created by the border. UKHCDO should therefore have raised the issue; had it been raised, the DHSS and the other health departments should then have ensured that some supply of 8Y was provided for the sake of minimally treated children and adults in Scotland and Northern Ireland. Dr Perry (who rightly thought the failure to obtain a small supply of 8Y earlier than was achieved was a lost opportunity)[1464] considered that the primary responsibility for this rested on clinicians rather than manufacturers, because they had the choice of which products to use in treatment – and, in this case, had the information necessary to make this choice assuming a supply could be arranged, as Dr Perry (rightly) thought it could be.
Northern Ireland is mentioned because Belfast Haemophilia Centre used both commercial and domestic factor concentrates during this same period. Its domestic Factor 8 concentrate was NY, supplied by PFC;[1465] the first supplies of Z8 were received in Belfast in July 1987.[1466] Any such system ought therefore to have also involved Dr Mayne and Dr Dempsey. There is contemporaneous evidence which demonstrates that a child with mild haemophilia who was treated with NY was infected with non-A non-B Hepatitis as a consequence.[1467] It appears, furthermore, that this individual was treated with NY at a time (autumn 1987) when Z8 was available, suggesting that this was a case in which the “old generation product” was being used.[1468] This should never have happened. The action taken in response to the case was to “set aside product heated at 80° for future therapy of virgin/mild haemophiliacs.”[1469] This was action that should have already been taken; had it been, this child would not have been put at risk of infection with Hepatitis C. Dr Perry recognised that the exposure at Belfast should not have happened – he recorded to Dr Boulton, once investigations had concluded that Z8 had not been involved, that it was “unfortunate that the boy was unnecessarily exposed to 68° material (NY).”[1470] “Unfortunate” was entirely the wrong word to use to describe a failure of treatment which was wholly avoidable.
It is worth noting that on the basis of such material as is available, there were at least 18 patients in the East of Scotland, 13 in the West, and probably a number attending Dundee centre, who were treated for the first time with a blood product between 1 September 1985 and 30 June 1987.[1471] Of those, a number were infected with non-A non-B Hepatitis.
In the 1970s and 1980s there were regular, and often cordial, interactions between representatives of pharmaceutical companies and haemophilia centre clinicians. Sales representatives visited haemophilia centres, in particular the reference centres and other larger centres.[1472] As Dr Colvin described: “I, like many others, had commercial representatives knocking on my door, speaking to me trying to persuade me to use their products ... they had all sorts of argument for telling me that their products were better than anybody else’s”.[1473]
Sometimes gifts were provided.[1474] Sometimes the pharmaceutical companies provided sponsorship or monies for research.[1475] More commonly funding was provided to cover the costs of attendance at international conferences. There are many instances of a close relationship between haemophilia centre directors and pharmaceutical companies recorded in contemporaneous documents. Some illustrative examples are set out below.
Armour, in 1980, provided funding to the Newcastle Haemophilia Centre in respect of research being undertaken in conjunction with Treloar’s. Armour would reimburse Newcastle for certain costs incurred, as well as supplying some of the concentrates to be used.[1476] In 1981 Armour offered, in a letter to Dr Rizza, to “help in any way we can” regarding the preparation of a paper on inhibitor treatment.[1477] In 1983 Dr Kernoff, of the Royal Free, sent a proposal to Armour “requesting support for our AIDS-related project in haemophiliacs.”[1478] Also in 1983 Armour provided funding to Sheffield Haemophilia Centre for research into AIDS.[1479] Donations were made by Armour to Dr Hill’s research fund at the Central Birmingham Health Authority in 1985.[1480]
Cutter, putting together a marketing strategy for 1981 with regard to Koate with the objective of establishing Cutter “as a major supplier with a good definable market image”, identified various “Supporting Activities” which included the provision of booklets and home care packs, and also “Support of/attendance at/involvement in ... a) Hospital meetings, staff and patient training. b) Haemophilia Society Meetings. c) National and International Meetings. d) Haemophilia Nurses Association.”[1481] At a December 1980 board meeting, reference was made to “the promises ... to the Alton Centre where Doctor Aronstam had been promised some form of financial support for a research fellowship and had put in a great deal of time and effort in putting forward a representation to the Company. However, nothing materialised and it seems that this was causing the Alton Centre to have nothing to do with Cutter whatsoever.” It was agreed to look into this “with a view to the Company being in a position to offer some form of financial support for such a fellowship.”[1482] A December 1984 sales report described that: “By far the most important happening this month is a very successful meeting with Dr. Wensley (MANCHESTER), when he promised me all of his business for the next contract. This is the period between January and April, 1985, depending on finances being available ... Dr. Wensley was promised a £10,000 sponsorship programme for research to be carried out over two years.”[1483] In April 1985 Cutter invited Dr Kernoff “to visit Cutter in San Francisco around the San Diego meeting. I hope to arrange the visit after San Diego, staying in San Francisco over the weekend and visiting Cutter Monday and possibly Tuesday morning depending on flights home. Cutter would of course arrange your hotel and look after you during your stay in San Francisco.” Professor Bloom and Dr Wensley “will also be in the party.”[1484] A Situation Report for April 1986 suggests that haemophilia centre staff were invited to attend concerts in the UK of the Bayer Philharmonic Orchestra.[1485]
An internal Cutter memo in May 1985 describes how the author “sought out and visited briefly with Prof. Bloom during the AIDS Conference in Atlanta. He asked if he could visit with Cutter the week following the San Diego meeting ... He will need room reservations in the city for Saturday, Sunday and Monday, plane reservations from San Diego. He will be accompanied by his wife.”[1486]
Alpha provided funding for the 1986 annual meeting of haemophilia centre directors.[1487] Lothian Health Board records suggest that donations were received from Alpha and other pharmaceutical companies in the second half of the 1980s.[1488]
Writing in June 1980 to the area health authority, Dr Kernoff explained that:
“In common with the Directors of most other large Haemophilia Centres in the UK., I have in the past both sought and accepted financial support for research and educational purposes from all the companies now making tenders. We are currently receiving support from Immuno, who paid the publication costs of a Royal Free ‘Haemophilia Centre Handbook’ which we are now selling to augment our research funds. The maintenance of our academic programme has always depended to some extent on assistance from commercial companies and it is my intention to continue to seek such support and, if funds are offered, to accept them.”[1489]
Dr Kernoff added that it was inappropriate for a person in his position to make decisions on the way in which large sums of public money should be dispersed and that this was a responsibility he was pleased to relinquish. He nonetheless expressed the views of the medical members of the adjudication panel (himself and Dr Colvin) on the tenders that had been submitted, recommending a continuation for the remainder of the financial year the present buying policy, which was to share purchases between Immuno and Armour, whilst acknowledging that he could not be considered to be unbiased as regards choice of companies.[1490]
Two particular recollections from clinicians who gave evidence to the Inquiry stand out.
Professor Tuddenham, who had been a co-director at the Royal Free with Dr Kernoff, recalled hospitality from pharmaceutical companies that was:
“overwhelmingly lavish ... at various stages ... you would be going to the best -- to a conference on haemophilia, there would be the very best restaurants, the river cruises, the -- all the paraphernalia of marketing products. It didn’t go quite to the heights that it got in some areas with a bigger turnover like the, let’s say, cardiology and gastrointestinal diseases where people would go on cruises for so called -- for educational purposes, and make hundreds of thousands of pounds out of it, but it was -- it was remarkably lavish.”[1491]
Posing the question “why were they[1492] spending that money?”, the answer was “Because they could gain influence with it.”[1493]
Professor Parapia, who had been director of the haemophilia centre in Bradford, described “Extravagant hospitality” being available “for Centres using large amounts of their products”,[1494] adding: “When we went to conferences, meetings and so on ... the directors that were most closely associated with companies would stay in the conference hotels and have five-star, et cetera, et cetera ... then there were gradations and you could see that as you went lower down the usage of Factor VIII in numbers or type of centre you were, then you may have to go into three-star and four-star hotels”.[1495] He added that for attendance at scientific meetings support from pharmaceutical companies was the only way for clinical staff to attend: “There was no money in the NHS”.[1496]
Professor Tuddenham also identified the conflict of interest that might be involved in being a paid consultant to a particular drug company: it was, he said, very difficult to “still keep completely independent in your thought ... there can be conscious and unconscious bias.” He considered that the standards now for declaring interests were much better than they used to be, with a requirement for complete transparency.[1497] One example of a haemophilia centre director providing consultancy services to pharmaceutical companies is Dr Jones. In November 1976, Dr Biggs wrote to Dr Jones regarding the “delicate and difficult” situation that arose at a haemophilia centre directors’ meeting, “representing the Newcastle Haemophilia Reference Centre while you are working for Hyland.” She wondered whether Dr Jones would consider “the Parliamentary procedure of ‘Declaring an Interest’ and possibly withdrawing from the meeting” when certain items were discussed.[1498] Dr Jones, in response, explained that this was “why I have gone out of my way to make it known to everybody concerned ... that I am at present acting as a Consultant to Hyland.” Whilst expressing a willingness to declare an interest and withdraw from meetings if necessary, he pointed out that “I could always argue that not a little of research and travel conducted by our colleagues is sponsored by commercial firms!”[1499]
Professor Michael Rawlins,[1500] giving evidence in October 1984 to the Royal College of Physicians Working Party on the Ethics of the Relationship between Physicians and the Pharmaceutical Industry, described the “fundamental ethical issue” as being based on the fact that “doctors spent very large sums of public money each year, and that the public could reasonably expect doctors to prescribe drugs with deference to their efficacy, safety and economy.” He felt strongly that “consultancies and their financial details” should be disclosed, that money should “not go to one person but to a department”, that the General Medical Council should give doctors “positive advice concerning their relationships with the Industry”, and that hospitality should be “totally divorced from promotion”.[1501] Professor Rawlins considered that guidance should be issued which included the following features: that physicians should be aware of the pressures that were placed upon them; that they should avoid placing themselves under an obligation to a particular company to promote its product or its image; and that they should act, and appear to act, impartially when discussing and prescribing the products of individual companies. He also thought that physicians should not accept any form of hospitality that accompanied drug promotion, and should not seek financial support from pharmaceutical companies for their expenses to attend scientific meetings.[1502]
In its report, published in March 1986, the Working Party acknowledged that a close relationship between doctors and the pharmaceutical industry was important for the treatment of patients and the future development and assessment of new drugs: because of the importance of this relationship, physicians should “ensure that their behaviour in relation to the pharmaceutical industry is always seen to be scrupulously impartial and honest.” The “overriding principle”was that “any benefit in cash or kind, any gift, any hospitality or any subsidy received from a pharmaceutical company must leave the doctor’s independence of judgement manifestly unimpaired.” It suggested that a useful criterion of acceptability was to ask “would you be willing to have these arrangements generally known?”[1503]
The General Medical Council’s 1985 publication Professional Conduct and Discipline: Fitness to Practise advised that doctors should avoid accepting any pecuniary or material inducement which might compromise the independent exercise of their professional judgement in prescribing, and that the acceptance of “unreasonable sums of” money or gifts from pharmaceutical companies “may be regarded as improper.”[1504]
The Medical Ethics Expert Group reported to the Inquiry, in response to a question regarding disclosure by clinicians of any commercial relationship with, or receipt of remuneration or assistance from pharmaceutical companies, that: “While there is an ethical obligation to declare, the way in which declarations are made has changed over 30 years. Previously declarations were not made to patients but to institutional bodies, committees, journals, colleges, grant awarding bodies, etc. In recent years there has been professional debate about the necessity of public declarations of interests, however, there is not yet consensus on this.”[1505]
In light of all of the above, it is not surprising that many core participants expressed in their submissions to the Inquiry serious concerns about the relationship between haemophilia centre directors and pharmaceutical companies. Thus, for example, the submissions on behalf of the core participants represented by Saunders Solicitors suggested that there was “an unhealthy – and some might say, improper – relationship between clinicians (by no means all) and the pharmaceutical industry ... pharmaceutical companies afforded ‘lavish entertainment’ and the like on doctors because of an expectation that they might gain influence. The same is true of research funded by the pharmaceutical industry that might be affected by ‘conscious and unconscious bias’.”[1506] The submissions on behalf of the core participants represented by Watkins & Gunn Solicitors spoke of a “conflict of interest at the epicentre” and of the “cosy relationships with pharmaceutical companies”.[1507]
It is clear, as set out in the submissions on behalf of the core participants represented by Collins Solicitors, that:
“there were close associations between prescribing physicians and pharmaceutical companies. These associations took many forms. They included hospitality, funded research (including free treatment to patients of the concentrate on trial), honorariums (whether paid directly to the researcher or to the hospital trust), and remunerated or non-remunerated roles as consultants or advisers to the companies. As Dr Geoffrey Savidge put it in his evidence to the Archer Inquiry, ‘such incentives could be recommendations for this [product] or recommendations for that [product].’ More subtly, clinicians may have been beguiled into thinking that free treatment to patients in trials would benefit both patients and the greater good.”[1508]
By way of comment, the value to the UK of public funding for UK attendees at international conferences is self-evident – healthcare is in many respects international, and UK clinicians can benefit from exchanging ideas and information with clinicians and academics from other parts of the world, just as those others may in turn benefit from association with UK clinicians. It is also true that pharmaceutical developments often help to advance the quality of care across the globe. It is that which essentially keeps pharmaceutical companies in business, for it is their efficacy in treatment which leads to their use, and their use leads to payment for it from which many such companies make their profit.
There was however a balance to be struck between the good to come from the use of “pharmaceutical money”, and the danger that it was used to influence the minds of those who had a role to play in purchasing.[1509] A simple answer would have been to make public funding available, at least for travel to conferences, for example, within a settled budget. If that was unavailable, because of other calls on the NHS for funding treatment, then the best answer would have been, and remains, publicity about the nature and extent of funding which is accepted to support clinicians. The passing of money to institutions such as hospital trusts or boards or charitable funds, where the proper use of it comes under the scrutiny of a number of people, and is more likely to come to public attention, is preferable to any payment – whether in cash or in kind – to an individual clinician or health administrator.
It is always difficult to ascertain the presence and, if present at all, the extent of bias – whether conscious or subconscious. At this distance of time, and in circumstances where those clinicians most prominently associated with pharmaceutical companies (such as Professor Bloom, Dr Kernoff, Dr Aronstam, and Professor Savidge) are dead, it is no longer possible to determine what impact these relationships and these offers of funding had on clinical decision-making. Acceptance of cash, or hospitality, by a clinician or hospital from a pharmaceutical manufacturer is likely to fuel distrust if use of their product later leads to results which were not highlighted beforehand by the clinician in discussions about risk, and the use of the product. Clinicians (and hospital boards or trusts) should be aware that this can do damage of a kind which makes their acceptance of the “benefit” look like a very poor deal indeed. A good mantra to have in mind is that if an individual healthcare professional is satisfied that they have no actual bias, they should then ask “might it, nonetheless, appear to others that I might have?” If so, steps need to be taken to change the appearance – and certainly, never, to try to hide what gives rise to it.
What can on any view be said, however, is that if clinicians accepted funding (whether it be for hospitality, for attending conferences, or for research) it was all the more incumbent upon them to ensure that their clinical recommendations and the risks and benefits of treatment were fully explained to those being treated. As described later in this chapter, the failure to do so was widespread and profound.
The organisation of haemophilia centres in the United Kingdom “made it possible to carry out collaborative research which was not so easily done elsewhere.” So said Dr Rosemary Biggs, of the Oxford Haemophilia Centre, at the first meeting of haemophilia centre directors in October 1968.[1510]
The “collection of 49 haemophilic patients at the Alton School makes this a unique opportunity to study the disease.”[1511] That was the view expressed by Dr Biggs in December 1970, referring to the boys with haemophilia attending Treloar’s.
They – the “almost unique group of haemophiliacs we have in Edinburgh because they have never received commercial concentrate” – “are, therefore ... useful material for a variety of studies in relation to liver disease.”[1512] So said Dr Christopher Ludlam – newly appointed consultant haematologist in Edinburgh – to Dr John Craske of the Public Health Laboratory Service on 28 April 1980.
“Although initial production batches may have been tested for infectivity by injecting them into chimpanzees it is unlikely that the manufacturers will be able to guarantee this form of quality control for all future batches. It is therefore very important to find out by studies in human beings to what extent the infectivity of the various concentrates has been reduced. The most clear cut way of doing this, is by administering those concentrates to patients requiring treatment who have not been previously exposed to large pool concentrates.”[1513]
So said Professor Arthur Bloom and Dr Charles Rizza in a letter to all haemophilia centre directors on 11 January 1983.
“So what are we? Are we human beings or are we just material?”[1514]That rhetorical question, posed by campaigner Bruce Norval in his oral evidence to the Inquiry, conveys the understandable – and in many respects well-founded – feelings of many people with bleeding disorders who were infected in consequence of their treatment with concentrates: that they were, often without their knowledge or consent, objects of research.
Medical research is, of course, in general terms “a good thing”: as the Inquiry’s expert panel of medical ethicists noted in their report “Scientifically robust research is essential to maintaining global health and wellbeing.”[1515]However, the value of such research to society is enhanced rather than undermined by undertaking research in an ethical and moral way.[1516]
As one clinician told the Inquiry, “The first ethical principle of research involving humans is the one we inherit from Hippocrates ‘First do no harm’. The second principle is that consent to take part in research must be a voluntary choice of the participant after a full explanation of the risks.”[1517] The expert panel expressed the position in a similar way: “there are two basic ethical principles which protect participants even where direct benefit is not anticipated: reasonable risk and consent.”[1518]
The requirement for informed consent to participation in research is fundamental. It was reflected in the terms of the Nuremberg Code in 1947:[1519] the Code’s first principle was that “The voluntary consent of the human subject is absolutely essential.”[1520] Similar stipulations were set out in the 1964 Declaration of Helsinki. In cases where there is a therapeutic benefit to the participant arising from the research, the doctor should “obtain the patient’s freely given consent after the patient has been given a full explanation”; in cases where there is no therapeutic benefit to the participant, “The nature, the purpose and the risk of clinical research must be explained to the subject by the doctor” and clinical research “on a human being cannot be undertaken without his free consent after he has been informed.”[1521]Over subsequent years guidance was issued by bodies including the Medical Research Council (“MRC”), the Royal College of Physicians, and the British Medical Association (“BMA”), emphasising the centrality of voluntary participation and informed consent.[1522] These principles also find their expression in the 1997 Oviedo Convention.[1523]
The reason why this is so important should be obvious but, not least because this principle was plainly not adhered to in relation to bleeding disorder patients in the 1970s and 1980s, it is re-stated here:
“Research brings the risk of causing harm, in the practical sense of possibly damaging or disadvantaging a patient, and of doing wrong, in the moral sense of ignoring the autonomy of that individual. People are wronged if they are deprived of choice or their values are transgressed on the assumption that the best clinical outcome is necessarily what is best for them. The possibility of harm cannot be entirely eliminated from research but by insisting that patients have adequate information and choice about participation, we minimise the possibility of wronging them.”[1524]
In practice, what this required was that the person undertaking the research should inform the patient about the potential benefits and risks of the proposed treatment, why it was proposed, the significance in terms of advancing knowledge and the researcher’s own stake in proposing the procedure. Further,
“Where patients are offered choices, they need information about the alternatives to the treatment recommended by their doctor. When a clinical study is proposed patients need to know about the advantages and shortcomings of conventional treatments as well as the options in the trial. In any situation, the more risky or invasive the procedure, the greater attention must be paid to the patient’s understanding of it and consent to it.”[1525]
Research can take different forms. In much of the contemporaneous documentation research was categorised as prospective or retrospective.[1526] Another distinction that was sometimes drawn in the evidence was between interventional and observational studies. Professor Charles Hay told the Inquiry that this distinction is not always clear cut and may be a matter of opinion. He suggested that in an observational study the intervention would have occurred anyway and that the intervention was not done for the purpose of research. An interventional study might, he said, involve a patient being given a concentrate that they would not have been given if they were not participating in the study.[1527] However, that distinction is often not easy to identify. Moreover, if there is to be study of this type, it becomes all the more important that care is taken when seeking the consent of the patient: for it may be exposing them to harm without there being any expectation they will benefit personally, whatever the benefit may be to medical science more generally. Where the research subject is a child, as a general rule they should not be exposed to research when there is no realistic prospect that this will benefit them in their present treatment. The ethics experts told the Inquiry that, in general, if the clinician is thinking of publishing the results, it is usually considered to be research – “if it’s been published in a journal, it’s original knowledge.”[1528]
Much of the research undertaken in the 1970s involved the Oxford Haemophilia Centre. In 1967 the work in Oxford of the MRC’s Blood Coagulation Research Unit under Professor Gwyn Macfarlane had been reorganised:[1529] a new building housed the clinical work of the haemophilia centre and the fractionation work of the Plasma Fractionation Laboratory; the original building where the Blood Coagulation Research Unit had been based now housed a Research Laboratory, “concerned with developing research in all aspects of haemostasis and blood coagulation” which worked “in close cooperation with the Clinical and Fractionation departments.” The official opening of the new haemophilia centre “was celebrated by inviting the Directors of the 36 Haemophilia Centres of Great Britain and holding a meeting at which research projects were planned in conjunction with the M.R.C. Cryoprecipitate Working Party.” A progress report covering the period 1967-70 summarised a range of clinical and other studies that had been undertaken or were in progress.[1530]
Much of the research undertaken at Oxford was purely laboratory based. But clinical studies were a regular feature. Much of what was undertaken involved “surveillance” – studying data that was available about patients and their treatment. A document from around 1972 described that there were “124 items coded on the O.H.C. punch cards for each patient”– including name, age, severity of bleeding disorder, family history of bleeding, treatment, history of jaundice, and complications – most of which would be “useful for comparison”.[1531]
Where that research involved hepatitis, it was often, from the mid 1970s onwards, coordinated or organised by Dr Craske, a virologist from the Public Health Laboratory Service. As detailed below a number of research projects involved other centres, such as Newcastle and Treloar’s.
Following an outbreak of hepatitis associated with the first use of Hemofil at the Bournemouth Haemophilia Centre in 1974, a retrospective survey of the use of this product was undertaken.[1532] The study was proposed at a 22 May 1975 meeting at Oxford, when Dr Craske explained that its purpose was to obtain “the most complete information possible about the incidence of hepatitis in patients who had received certain specific batches of Hemofil.” Dr Craske had already obtained data about the incidence of hepatitis in patients at Newcastle, Bournemouth and Alton,[1533] and his “impression” was that hepatitis had occurred most often in people who had been treated relatively little in the past. Haemophilia centre directors whose returns recorded that they had treated patients with Hemofil in 1974 were asked to report clinical details of hepatitis cases possibly associated with treatment with the product to the Oxford Centre. Haemophilia centre directors were told in September 1975 that henceforth they should make a specific return notifying each case of jaundice, and for those centres which used Hemofil there was a form which “should be completed for all Centres using Hemofil and will be forwarded to Dr. Craske so that he can complete his study.”[1534]
Dr Craske reported the results of the retrospective study at the 13 January 1977 meeting of haemophilia centre directors, when he explained that he would like to continue with this study for the next two years to study the incidence of chronic sequelae as well as a comparison of jaundice associated with NHS Factor 8 and commercial products.[1535] Further detail was set out in a written report, authored by Dr Craske and Dr Peter Kirk. This explained that returns had been received from 24 haemophilia centres, and that 374 patients had received transfusions of one or more batches of Hemofil over this period.[1536] A total of 78 cases of hepatitis affecting 66 patients (17.7%) were considered to have been associated with transfusions of Hemofil, of which 48 were non-B Hepatitis and 30 Hepatitis B. The paper concluded that “the first introduction of Hemofil as Factor VIII replacement therapy in the U.K. was associated with an overall incidence of 17.7% of transfusion hepatitis.” It added, with considerable understatement, that since “this disease was commoner in patients with mild haemophilia it is possible that with hindsight alternative products might have been used to treat some patients and this might have reduced the incidence of hepatitis.”[1537]
A paper with the results of the survey, in which Hemofil was referred to as “Brand ‘L’”, was published in 1978.[1538]
This study was retrospective – it looked back at treatment which had already been given – but it remains ethically problematic in two respects: firstly, it is clear that not only were patients being studied[1539] without their knowledge but the results of those studies were not shared with the patients themselves;[1540] secondly, it fuelled a desire to undertake more and more surveillance, including the proposal to study over the next two years the incidence of hepatitis due to Hemofil, Kryobulin and NHS Factor 8, with the potential to influence treatment choices and have an impact on clinical decision-making.[1541]
As a continuation of the Hemofil survey, Dr Craske subsequently carried out a study of the incidence of hepatitis after treatment with Kryobulin in 1976 to compare it with that due to Hemofil.[1542] In a January 1977 protocol, Dr Craske proposed that the study last for two years, with hepatitis cases again to be reported to the Oxford Centre.[1543]
Results from the survey were subsequently presented to haemophilia centre directors at their 24 October 1977 meeting.[1544] The report containing the results, prepared by Dr Craske, recorded that the methods used were the same as in the first Hemofil survey. Six batches of Hemofil were studied and transfusion records were available for 16 batches of Kryobulin. Returns were received from 24 haemophilia centres. There was epidemiological evidence that 2/6 batches of Hemofil and 2/16 batches of Kryobulin contained Hepatitis B virus. 4/6 batches of Hemofil and 3/17 batches of Kryobulin were associated with cases of non-B Hepatitis. Of 371 patients transfused with Hemofil in 1974-75, 111 received further transfusions in 1976, and 77 patients received Hemofil for the first time. A total of 101 patients were transfused with Kryobulin of whom 31 had previously received Hemofil in 1974-75. It was noted that cases of non-A non-B Hepatitis associated with Hemofil had continued to occur, all in patients receiving Hemofil for the first time.[1545]
Whilst the original Hemofil study was retrospective, it is not clear whether this study was entirely so. The January 1977 protocol envisaged the reporting of cases of hepatitis associated with use of the products throughout the two year period 1976-77, although the report prepared in September 1977 for haemophilia centre directors studied Kryobulin given in 1976 only. Furthermore, the Kryobulin study involved some people being treated with Hemofil, and it is conceivable that those treatment choices may have been influenced by the knowledge of the first Hemofil study.
It was said to be essential to continue these studies. This would help to determine the incidence of further problems following acute hepatitis, and several more projects were proposed. These included a study of hepatitis following NHS concentrate and the compilation of a register of carriers of Hepatitis B surface antigen to be kept with the other patient data at Oxford. During a discussion of the paper at the directors’ meeting in October 1977, some directors “expressed concern about this data being included in the National Register as they were worried that the information might become available to unauthorised persons and be used in a manner detrimental to the interests of the patients.”[1546]
Some of those infected have discovered only on receipt of their National Haemophilia Database (“NHD”) records that they were part of “Dr Craske’s research work”. Each entry in the database was assigned to a centre, and in some cases this was “Dr Craske’s research work” rather than a physical centre. Individual records extracted from the NHD included a list of the centres where the individual received care and this could include “Dr Craske’s research work” if treatment or testing was linked in the database to his research but his work went wider than the entries with that code.
Lee Stay described his “complete shock” on reading this entry in his records. He was not aware of his participation in this, which related to treatment by the Hammersmith Hospital. Lee’s treatment with two different commercial concentrates – Kryobulin and Hemofil – in 1975 (when he was around 6 years old) and again in 1976 was recorded as part of “Dr Craske’s research work”.[1547]
Neil Weller told the Inquiry “It would appear that I was part of Dr Craske’s research work. I was not aware of this. I do not know who Dr Craske is.” His NHD records show treatment under the auspices of “Dr Craske’s research work” with Hemofil in 1974 – when he would have been only 3 years old – and with Kryobulin, BPL Factor 8 concentrate and Oxford Factor 8 concentrate in 1976.[1548]
Ruth Major described several entries in her late husband Peter’s database records referring to Dr Craske’s research:
“I was not familiar with this person and in fact had never heard mention of him. My Husband had also never mentioned him therefore I conclude that he had never heard of him. I decided to do some research into this person and discovered that he was a virologist who had been conducting research into Hepatitis Non-A and Non-B in the 1970’s and 1980’s. I also found an entry in my Husband’s medical notes dated 27th February 1979 which states ‘Blood taken for hepatitis project.’ As far as I know my Husband was never informed or consented for this research project.”
Peter’s NHD records show treatment with Hemofil in the category of “Dr Craske’s research work” in 1974 and 1975. Peter was a young man in his twenties at that time. A later entry in his medical records from the University Hospital of Wales refers, in 1979, to a “Hepatitis Project”.[1549]
Robert Hodgkins’ NHD records show treatment with Hemofil in 1974 (when he was around 6 years old) for “Dr Craske’s research work”.[1550]
Similar entries appear for Patricia Crowe’s father, David Gill. She told the Inquiry that “My father had no knowledge of this and was therefore unable to consent to it.”[1551]
Rosamund Cooper’s NHD record similarly refers to Dr Craske’s research work. Neither she nor her mother had any recollection of being informed about this.[1552]
Haydn Lewis’ NHD records show treatment with Hemofil in 1974 again under the heading “Dr Craske’s research work.”[1553] He queried this (and other entries) in 2006 and received a response from Dr Hay on behalf of the UK Haemophilia Centre Doctors’ Organisation (“UKHCDO”) which stated that “We believe that in the late 1970’s the UKHCDO Liver Disease Working Party conducted a retrospective survey of non-A, non-B hepatitis and that the data from this survey was kept in a file labelled treatment centre code 39 Dr Craske for the sake of convenience. Understandable [sic], this has caused quite a lot of confusion since.”[1554]
Jonathan Evans’ son Jason told the Inquiry that “on my father’s [NHD] extract, there was an entry that said, ‘Dr Craske’s research work’ and I know, because having spoken to people and having seen it, that it appears on that of many others as well. It’s by no means unique to my father’s schedule.”In his written evidence, Jason Evans raised the question “what consent Dr Craske had or should have had to carry out such research work.”[1555] Professor Hay suggested in response that the research was published in 1983 in the British Medical Journal and that it was “a retrospective study looking at the risk of developing non-A, non-B hepartitis [sic] after administration of concentrate.” He described it as a “non-interventional observational study.”[1556] This was incorrect: the study published in 1983 related to patients attending the Oxford Haemophilia Centre and was clearly a prospective study: it is discussed further below.
However, in a written statement to the Inquiry Professor Hay pointed to “Commercial factor VIII associated hepatitis 1974-1975 in the United Kingdom: a retrospective survey”[1557]as the only publication relating to:
“Dr Craske’s surveys conducted collaboratively with UKHCDO and the NHD. This was a retrospective survey of 371 people from 24 haemophilia centres who had been transfused with the same commercial factor VIII product (Hyland) thought to have been responsible for the hepatitis outbreak at Bournemouth Haemophilia Centre. New cases of hepatitis associated with this brand of factor concentrate were reported through the NHD. This was a non-interventional retrospective observational study, which at that time was not thought by the people undertaking this work to require individual patient consent.”
He contrasted this with the 1983 publication “Non-A non-B hepatitis after transfusion of factor VIII in infrequently treated patients”, which he correctly described as “interventional clinical trial, conducted in Oxford”.[1558]
The reference to “Dr Craske’s research work” in individual records on the National Haemophilia Database would indeed have referred to the studies relating to Hemofil and Kryobulin discussed above.[1559] It went wider than that. Though it seems clear that a major focus was on research into Hemofil, especially after the Bournemouth outbreak in 1974, and separate returns were sought from centres using it which were specific to that product, “Dr Craske’s Research Work” covered reports to him from 1973/74 onwards in respect of all the concentrates then licensed and in use, cryoprecipitate and plasma.[1560]
Nonetheless, once Dr Craske had decided in mid 1975 to gather and study data relating to such treatment and its effects, subsequent treatment decisions, in the second half of 1975 and in 1976, could have been influenced (consciously or otherwise) by the knowledge that research into the effects of the treatment was being undertaken. There is some support for this, though it stops short of declaring it clearly to be the case, in that Lee Stay, Neil Weller and Robert Hodgkins were all very young when given commercial factor concentrate at a time when for young children cryoprecipitate should have been the product of first resort, and NHS concentrate the second.[1561] Furthermore, it remains the position that the personal medical data of individuals was shared by haemophilia centres with Dr Craske; the patients so studied knew nothing about that; and the association with hepatitis which was revealed was not shared or discussed with them so that they could make an informed decision for themselves whether or not to continue with such treatment. This was wrong.
In 1975 a prospective study on hepatitis in Haemophilia A patients was proposed, involving three centres: Treloar’s, Newcastle and Oxford. The study was discussed at a meeting at the Oxford Centre on 22 May 1975, attended by Drs Biggs, Rizza, Craske and others. It was noted that there were difficulties in planning a formal controlled study of various therapeutic materials: for example, “in Oxford material made from large pools was not given to patients who had received relatively little previous treatment or to small children (Dr Biggs and Dr Rizza). Thus patients could not be allocated to treatment in a random manner and patients thought to be most likely to develop hepatitis would not receive the commercial factor VIII.” It was said that the existing system of “using first one type of preparation and then another in the same patient could make it virtually impossible to attribute infectivity to any particular material.” A trial on a large scale would require to be sponsored by the DHSS, the MRC or by the haemophilia centre directors, and it was “felt that perhaps the best thing that could be done at present would be to arrange a pilot study at Oxford and at the Treloar College.” It was further “felt that restriction of materials to particular patients would greatly improve the definition of the cause of Hepatitis.”[1562]
A protocol for the study – which would involve each patient being treated with one type of material – was subsequently introduced by Dr Kirk of Treloar’s at the 18 September 1975 meeting of haemophilia centre directors. It was proposed that those who were to participate should be 25 patients at the Oxford Centre (15 receiving Oxford Factor 8 and 10 receiving Hemofil), 35 at Alton/Treloar’s (20 receiving cryoprecipitate, 10 Kryobulin and 5 Elstree Factor 8), and 40 at Newcastle (all receiving Hemofil).[1563] The protocol recognised that treatment with Factor 8 concentrates exposed patients to a much larger risk of contracting transfusion hepatitis “since the fractionated product is processed from donor pools”; it was recognised too that commercial concentrates were made from “very large pools”. The protocol recorded that the study was intended to answer the following question: “Does the administration of factor VIII concentrates to haemophiliacs on regular replacement therapy, significantly increase the incidence of transfusion hepatitis?” It was also hoped that it would address a number of other points, including any difference in the attack rates between commercial Factor 8 concentrates and those produced at Oxford and Elstree, and further information on hepatitis “due to unknown viruses or agents other than hepatitis ‘A’, ‘B’, EB or cytomegalo virus.” It was preferable that on entry patients had normal liver function measurements (though abnormal results would not exclude a patient from admission). Each patient would be required to remain on the allotted therapeutic material for a minimum of 18 months.[1564]
Patients would be categorised as mild or severe in relation to their bleeding frequency[1565] and would, as far as possible, “be allocated evenly over the various treatment groups.” It was noted that in practice this would “not be feasible since there will be a tendency to use concentrates for patients having HBsAb or HBsAg and cryoprecipitate for those who are antibody negative”. Each patient would be treated with the same type of material throughout the study and, where possible, it was intended that batches be arranged sequentially in order that the patient receive the same batch of their particular brand over a three-month period.[1566]
Another eligibility criterion concerned consent:
“All patients or their parents/guardians must give their informed consent. The following points will be made clear:
Even if this information were provided to patients – and the Inquiry has uncovered no evidence to suggest that it was – this would be patently insufficient to enable the giving of informed consent. While it described an anticipated benefit of the trial – namely, reducing the degree of donor exposure by limiting the transfused material to one type – it failed to address the risks involved, including the risk that commercial concentrate would be more likely to transmit hepatitis than NHS Factor 8 or cryoprecipitate. The express endpoint for the study (to see if giving Factor 8 concentrates significantly increased the risk of hepatitis) shows that the study began with a proposition that giving them would cause recipients to be infected more than they would otherwise have been.[1569] It did not explain that one of the reasons for undertaking the study was to determine the relative likelihood of hepatitis infection from commercial and NHS concentrates, or that information was sought on hepatitis other than Hepatitis B. In other words, it did not even begin to discharge the obligation to ensure voluntary and fully informed participation and was plainly unethical.
On 1 April 1977, Dr Kirk wrote to the National Institute of Biological Standards and Control with an update on the study. In the 19 months or so in which it had taken place, “All the cases of clinical hepatitis and almost all the cases of asymptomatic hepatitis were confined to the patients restricted to commercial concentrates. There were no significant differences between the cases restricted to Hemofil and Kryobulin.” Dr Kirk proposed to continue the study and at the next stage it would restrict patients to either commercial concentrates as a group, or to cryoprecipitate, or to BPL Factor 8.[1570] This leads to the further comment that it was proposing restricting some patients to a product which he, Dr Kirk, had already identified as causing harm which the other two choices probably did not. This was unethical.
In a letter in October of that year, Dr Craske described the study as involving – at least with respect to Treloar’s pupils – “the prospective study of the incidence of hepatitis, and abnormal liver function tests associated with different forms of Factor VIII therapy.”[1571]
The study appears to have continued (or been extended): Dr Kirk described the results of “the prospective survey on hepatitis carried out at Edinburgh and Alton” at the 14 December 1977 meeting of the Haemophilia Centre Directors’ Hepatitis Working Party,[1572] and the meetings of the Working Party on 14 March 1978[1573] and 7 November 1978 included further discussion of the prospective study.[1574]
In April 1978 Dr Craske applied to the DHSS for funding to cover two research projects, both involving the Oxford Centre and described as a joint project between the Hepatitis Working Party and the PHLS.[1575]
The first, described as “Hepatitis Surveillance”, would involve haemophilia centre directors notifying hepatitis cases thought to be associated with Factor 8 or 9 therapy to the Oxford Centre. The application explained that this had previously been done annually, but that centres were now being encouraged to notify cases immediately. It was proposed that the project take place over a three year period: “With the large number of brands of Factor VIII in use, it is anticipated that the most useful information about the incidence and types of hepatitis will be obtained over the next 3 years.” In cases of doubt as to the presence of hepatitis, queries would be clarified by correspondence with the centre: “If necessary, the patients notes are consulted, and, if necessary, Miss Spooner visits the Centre, with the agreement of the Director, and assists in obtaining any further information required.”[1576] (This plainly involves the communication of personal, confidential, medical information, with no indication either of that fact being communicated to the patient, or the concerns about hepatitis being shared with the patient.)
The second project concerned the follow-up of “chronic sequelae of Factor VIII associated hepatitis”, which it was proposed would be carried out over two years at the Oxford Centre. In the first instance, it was intended to study 116 patients at the Oxford Centre who had received 6 infected batches of Hemofil in 1974/75, 4 of which were found to be positive for Hepatitis B. Each of these patients would be matched with a second group of patients receiving treatment with cryoprecipitate.[1577] The patient’s GP would be contacted “and invited to furnish details of the patient’s general health.” Patients would be visited at home or seen when they attended at the Centre: “A medical history will be taken, and, physical examination will be carried out with particular reference to liver disease.” It was also proposed to study the incidence of hepatitis in the patients’ close household contacts.[1578]
By the time of the 7 November 1978 meeting of the Haemophilia Centre Directors’ Hepatitis Working Party, the DHSS had agreed to provide the grant and work on both studies was underway.[1579]
An update was provided at the 29 January 1979 meeting of the Hepatitis Working Party. So far, 25% of the Oxford haemophilia patients who had been examined had been found to have persistent transaminitis.[1580]
These two studies were both retrospective. However, at the same meeting two protocols were discussed for the studies relating to ongoing study of chronic liver disease in Oxford patients: one concerning the effect of intravenous infusions of Factor 8 on serum enzyme levels in haemophilia patients; the other concerning the value of serum bile acid measurements in the investigation of haemophilia patients thought to have chronic hepatitis.[1581] The first of these protocols proposed that up to 20 Haemophilia A patients at the Oxford and Edinburgh Centres would be selected. An attempt would be made to include patients on home treatment, those receiving only cryoprecipitate and patients with a mild coagulation defect. Only patients over the age of 18 would be included. As for consent: “The object of the study will be explained to each patient before he is included in the study, and his informed consent obtained.”[1582] The evidence does not confirm the extent (if any) to which this was done: and the extent in any event of what was to be said seems to be limited to telling the patient what the purpose of the study was, and not to require going further to tell them of other relevant matters such as the risks involved. The protocol for the second study explained that “As part of the investigation of patients in the chronic hepatitis study, it is proposed to measure the fasting blood bile acid levels in 40 patients attending the Oxford Haemophilia Centre”, as well as a similar group of patients from the Edinburgh Centre.[1583]
A further update was provided at a meeting of the Working Party on 20 August 1979. In relation to the chronic liver disease study, Dr Susanta Ghosh explained that, so far, 179 patients with severe haemophilia had been studied. 70 out of 174 patients for whom detailed records of liver function tests were available had persistently abnormal liver function tests. 32 of these had been seen at the liver clinic, and “20 of these had significant chronic liver disease, as judged by their clinical features.”[1584]
Dr Craske also provided an update on the Hepatitis Surveillance study. He explained that the prevalence of hepatitis appeared to be about the same as the previous two years. Compared with 1974, “most of the overt Hepatitis occurred in mild Haemophiliacs many of whom had been transfused with concentrate for the first time to cover operations.” Two thirds of the reported cases were non-B Hepatitis, and over thirty of these had been confirmed as non-A non-B Hepatitis.[1585]
Dr Craske provided the DHSS with an annual report on the two studies – known together as “Project Number J/S240/78/7” – in late 1979. This explained that the Hepatitis Surveillance study included, in addition to reported hepatitis cases from 1977, a review of cases reported to the Oxford Centre since 1974. The “two most obvious results of the 1977 returns” were said to be: a “high association of Factorate with cases of hepatitis B compared with other brands of commercial concentrate”; and the “continued association of Hemofil and other brands of commercial concentrate with cases of non-B hepatitis”.[1586]
As for the second study, 179 haemophilia patients on long term Factor 8 and Factor 9 therapy at the Oxford Centre had been studied. The study was summarised as involving the examination of patients for clinical and laboratory evidence of chronic liver disease and their comparison with matched controls. The incidence of the “secondary spread of hepatitis B to household contacts of haemophiliacs” was also being assessed. Further detail was provided in an appended progress report.[1587]
Further progress reports were provided to the DHSS in the second and third (and final) years of the project.[1588]
Results were also shared with the UKHCDO Hepatitis Working Party at its 3 September 1980 meeting.[1589] Further results from the Hepatitis Surveillance study were presented by Dr Craske at the 11 September 1981 meeting of the Hepatitis Working Party. A total of 283 episodes involving 253 patients reported to Oxford since 1974 had been identified as probable cases of transfusion hepatitis, of which 197 were non-A non-B Hepatitis and 86 Hepatitis B.[1590]
Dr Craske presented a report on the final year of the study at the 9 October 1981 meeting of haemophilia centre directors.[1591] A total of 283 episodes of hepatitis related to Factor 8 or Factor 9 therapy had been reported by haemophilia centre directors, involving 253 patients. 197 were “non-B hepatitis and therefore probably non-A, non-B, and 86 incidents were hepatitis B.” It was suggested that the differing proportions of incidents related to each brand did not “reflect the relative incidence of hepatitis due to each product. Hemofil and Kryobulin were used in the U.K. 2 to 3 years before the other commercial products, and the relative amounts of other products have varied since due to market forces.” However, it was also noted that there was a 4-20 times higher incidence of overt non-A non-B Hepatitis associated with US commercial concentrate compared with NHS product. Further, 70-80% of cases of non-A non-B Hepatitis were associated with the first dose of concentrate the patient received.[1592]
A number of further research projects were outlined, including: the continuation of the Hepatitis Surveillance scheme; a prospective study comparing different products in relation to the incidence of sub-clinical hepatitis;[1593] and continuing efforts to assess the types and severity of chronic hepatitis resulting from Factor 8 or 9 replacement therapy.[1594]
During the late 1970s and early 1980s, patients treated with concentrate for the first time (sometimes referred to as PUPs – previously untreated patients) were the subject of study. At the 20 February 1980 meeting of the UKHCDO Hepatitis Working Party, Dr Howard Thomas and Dr Peter Kernoff of the Royal Free Hospital described a prospective study they had carried out on patients receiving concentrate for the first time. 11 patients, most of whom had received commercial concentrate and who had been followed for periods of up to 4 years, had evidence of chronic hepatitis as judged by persistently abnormal serum transaminases. Dr Ghosh of the Oxford Centre reported that similar results had been seen in Oxford patients receiving mainly NHS concentrate for the first time. The meeting agreed that more information was needed “on the risk to patients of developing chronic non-A, non-B hepatitis by prospectively following patients first exposed to concentrate or other products, e.g., mild haemophiliacs undergoing non-emergency surgery. The value of other methods of treatment to cover operations needed reassessing.”[1595]
This appears to have led to Dr Craske preparing a protocol, dated 2 July 1980, for a prospective study of the incidence of acute and chronic hepatitis in patients with bleeding disorders as a result of first exposure to Factor 8 concentrate or cryoprecipitate. This noted that Oxford’s hepatitis surveillance programme had shown that the group of haemophilia patients with the highest incidence of acute hepatitis were those exposed to concentrate for the first time. Most of these patients had mild haemophilia and “usually require few transfusions, usually of cryoprecipitate only.” The protocol added: “Since the risk of chronic hepatitis following an acute attack of non-A, non-B hepatitis after a transfusion of factor VIII concentrate is between 20 and 40%, it is important that an accurate estimation should be made of the incidence of transfusion hepatitis in this group.” It was noted that some of the operative or treatment procedures covered by concentrate transfusion were minor, and it seemed “possible that some could be carried out with the use of alternative methods of treatment.” Patients would be considered for the study if they had received less than two transfusions of Factor 8 in the previous year, and came within the following groups: newly diagnosed patients with Haemophilia A, Haemophilia B and von Willebrand disorder; and Haemophilia A patients, Haemophilia gene carriers, Haemophilia B patients and those with von Willebrand disorder who were “about to undergo an elective treatment procedure which will require cover with concentrate.” As for consent for patients admitted to the study: “The objects of the project will be explained to them, and their consent, or that of their parents if under 18 years of age obtained.” Patients would be followed for 12 months after their operation, with regular liver function and Hepatitis B tests during that period. The study was to last for 12 months and would involve, if possible, 40-50 patients.[1596]
At the 3 September 1980 meeting of the Hepatitis Working Party, Dr Craske circulated data “which suggested that NHS Factor VIII made at Oxford might be associated with a lower risk of non-A, non-B hepatitis than other batches of NHS factor VIII, e.g., Elstree or commercial factor VIII.” It was noted that Oxford Factor 8 had a pool size of 500 donations, whereas the Elstree product had a pool size of 3,500 donations, and it was “proposed to carry out a prospective study to evaluate the value of such a preparation for the treatment of mild haemophiliacs at operation, etc.”[1597]
In February 1981, Dr Craske submitted a grant application for a prospective study of the incidence of acute and chronic hepatitis in haemophilia patients after treatment with Factor 8 or Factor 9 for the first time. It was proposed to carry out the survey over a period of 30 months on patients undergoing elective surgery “or other treatment requiring cover with concentrate”. It was estimated that around 15 patients would be suitable for study in any 1 year; overall it was hoped to include 30 to 40 patients. Patients receiving cryoprecipitate only would be studied as a control where possible. The purpose of the study was “to compare the incidence of acute hepatitis and chronic sequelae in patients transfused with both commercial and NHS freeze dried concentrate for the first time by means of a prospective study of patients treated at the Oxford Haemophilia Centre.” It was said to be important to undertake this investigation because it was possible that “a significant proportion of haemophiliacs on regular factor VIII therapy may become severely ill with chronic hepatitis in 10-20 years’ time.”[1598]
Patients at the Oxford Centre who had received fewer than two transfusions of Factor 8 or 9 in the previous year would be considered for the study. Rather than newly diagnosed patients (of which there were very few), or infrequently treated patients with inhibitors, it was proposed to select patients with mild coagulation disorders who did not “usually require factor VIII or IX concentrate, but who are about to undergo an elective procedure which will require cover with concentrate.” Patients from this category who attended the Oxford Centre during the course of the study would be selected. The “objects of this study will be explained to them and their consent, or that of their parents if under 18 years of age obtained.” A clinical examination and blood tests would be carried out before the operation and patients would be followed up for 12 months.[1599]
At the 11 September 1981 meeting of the Haemophilia Centre Directors’ Hepatitis Working Party, it was recorded that the grant application had been made to the MRC “with a view to undertaking a prospective study of patients with mild coagulation defects undergoing treatment requiring concentrate cover.” The aim was to assess “the risk of contracting hepatitis on first exposure to concentrate and to provide a collection of sera from well documented cases of NANB hepatitis for the evaluation of new tests for this disease.” It was recorded that a preliminary study had been started at the Oxford Centre in March 1981 and so far 8 patients had enrolled.[1600] At the haemophilia centre directors’ meeting on 9 October 1981, Dr Craske reported that a multicentre prospective study of hepatitis in first time treated/seldom treated patients was planned, noting that this group of patients “seem to be running a higher risk of contracting Non-A Non-B hepatitis whatever type of material was used for their treatment.”[1601]
Dr Craske provided an update at the 6 September 1982 meeting of Haemophilia Reference Centre Directors. 28 patients at the Oxford Centre had been entered into the study to date and followed for a period of 6 months or more after treatment. 9 of these patients had developed non-A non-B Hepatitis. It appeared that there was a “100% attack rate for first time treated patients who received NHS factor VIII concentrate and more than 80% chance of contracting hepatitis following treatment with any type of concentrate.” Dr Craske proposed that further trials of the type conducted at the Oxford Centre should be undertaken at other centres. He had also discussed with Dr Lane “the possibility of concentrates being made from pools of ‘accredited donors’ for the treatment of first time or seldom treated patients.”[1602]
A further update was provided by Dr Craske at the 13 September 1982 meeting of the Hepatitis Working Party. He explained that the application to the MRC for funding had been refused and that the DHSS no longer had any funds available.[1603] Nonetheless, the preliminary study had been carried out at the Oxford Centre with the help of funds from the Haemophilia Society. 32 patients had so far been enrolled and 28 of these had been followed for at least six months. These were patients with mild coagulation defects who had fewer than two transfusions of Factor 8 or 9 concentrate during the previous year. 9 out of 9 patients treated with one batch of concentrate who had had no previous transfusions of Factor 8 or 9 developed non-A non-B Hepatitis with incubation periods of between 24 and 111 days. Some of these patients had received NHS Factor 8, one US commercial Factor 8 and the last patient NHS Factor 9. The pool sizes for NHS Factor 8 contained 1,536 - 2,504 donations.[1604] The study “implied that there was more than a 90% chance of contracting non-A, non-B hepatitis after first treatment with NHS or US commercial factor VIII concentrate.”[1605]
Dr Craske explained that it was proposed to extend this project to other centres to compare the attack rates of non-A non-B Hepatitis after transfusion with different brands of Factor 8 concentrate, “and to prospectively follow-up patients with a view to determining the long-term sequelae.” The meeting also discussed the possibility of using the prospective study to assess the effectiveness of evaluating new hepatitis reduced products. Dr Lane suggested that the “only way to evaluate the preparations for freedom from non-A, non-B hepatitis viruses was by chimpanzee inoculation, or in a prospective study of susceptible human subjects.” Dr Craske agreed to revise the prospective study protocol and circulate it for comment. It would then be open to any haemophilia centre director to use the protocol when evaluating any of the new concentrate products. They would be invited to report the results to the Working Party and “would be asked to retain serial samples of each patient’s serum so that a collection would be available to evaluate any new marker tests for non-A, non-B hepatitis viruses.”[1606]
Dr Craske subsequently prepared an updated protocol, dated 23 September 1982, which proposed that other haemophilia centres undertake a similar study to that carried out in Oxford. As well as comparing the incidence of hepatitis after first exposure to Factor 8 or Factor 9 concentrate of different brands, it was recorded that there were also “several commercial products under development where attempts have been made to inactivate viruses present in the concentrate” using a variety of methods. It was said that the “only way of determining whether any of these methods is effective in inactivating hepatitis viruses in these products is by chimpanzee inoculation or a prospective study in haemophiliacs who have had no previous exposure to concentrate.” The protocol continued: “Chimpanzees are in short supply, so in the absence of laboratory tests for non-A, non-B, hepatitis trials in patients likely to be susceptible to non-A, non-B, hepatitis present the only possible way of evaluating this risk.”[1607]
Two aims were described. First, to assess the risk of contracting non-A non-B Hepatitis and Hepatitis B after first exposure to Factor 8 or 9, both NHS and commercial, and to “compare this with the risk after treatment with cryoprecipitate or any other product which may have a reduced risk of transfusion hepatitis.” The second was to assess the risk of chronic sequelae after both Hepatitis B and non-A non-B Hepatitis. The selection of patients, study method and references to consent were otherwise similar to those described in Dr Craske’s February 1981 funding application.[1608]
However, it appears that, insofar as it was to be used by other haemophilia centre directors, Dr Craske’s protocol was to be amended further. The approach to be taken to trials of “hepatitis reduced” Factor 8 and 9 was discussed in detail at the 19 January 1983 meeting of the Hepatitis Working Party. The meeting was concerned in particular with the use of such products – which had not yet been licensed – on a named patient basis in the absence of coordinated trials by centre directors. It was agreed the Working Party would attempt to obtain the collaboration of haemophilia centre directors in organising a trial.[1609] The questions to be addressed included the “risk of non-A, non-B hepatitis when given to susceptible patients. In view of the results of the Oxford prospective study, these should be patients with no prior exposure to factor VIII or IX concentrate.” Dr Craske agreed to modify the prospective study protocol to include this and other points.[1610]
In September 1983 Dr Craske produced the Hepatitis Working Party’s 1982-83 annual report and appended a paper explaining that manufacturers would shortly be offering trial batches of hepatitis reduced products and referring to the risk of AIDS. The paper explained that, since the only way of ensuring the susceptibility to non-A, non-B viruses was by using patients who had not previously received concentrates, a choice would have to be made between using heat-treated products from commercial sources, which might carry a small risk of AIDS transmission, or using NHS concentrate which appeared to carry a 100% chance of transmitting non-A, non-B Hepatitis.[1611]
In December 1983 the results (relating to the first 30 patients in the study) of the prospective study on the incidence of hepatitis in infrequently treated patients was published in the British Medical Journal. The article asserted that all of the patients gave their informed consent.[1612] The Inquiry has found no evidence to support that, nor any evidence of ethics committee approval.[1613]
Malcolm and Violet Slater gave evidence to the Inquiry in October 2019. Malcolm Slater recalled being given Factor 8 concentrate pre- and post-operatively in November 1981,[1614] and that subsequently lab staff from the haemophilia centre (Oxford) would come to his home, take samples of his and his wife’s blood, and ask questions about their health. Disconcertingly, he said, the staff wore protective clothing and glasses. When he and his wife asked the reason for taking blood samples, “they would only tell us that it was for important research and they really would appreciate it if we would participate.” He had not been told about the risks of infection – had he been told, he would not have gone ahead with the operation because it was not essential.[1615] In their oral evidence, they confirmed that the staff who visited at home “wouldn’t say why, other than they were taking blood” – they said they were doing “some important research” but said “nothing about the research. It was all a bit of a mystery.” Violet Slater explained that “we never got a satisfactory answer apart from sort of a pat on the back and, ‘This would be really helpful for haemophiliacs in the future.’”[1616]
What Malcolm and Violet Slater were describing to the Inquiry was their involvement in the prospective study of infrequently treated patients discussed above – Malcolm as an individual with haemophilia who had not been treated for a number of years and who was then given Factor 8 concentrate for the elective surgery in November 1981, and infected with Hepatitis C in consequence, and Violet as part of the associated study of household contacts.[1617] It is plain from their evidence that, contrary to the assertion made in the British Medical Journal publication, Malcolm Slater had not given informed consent to participation in that research. It also appears from his description of staff wearing biohazard protection that it was thought that giving him, and thereby exposing her, to the product being researched might involve a considerable transmissible health risk.
The evolution of this particular prospective study from its genesis in 1980 to its publication in 1983 has been set out in some detail above because the ethical implications of this research are so disturbing. It straddled the period from the Glasgow Symposium, where the risks of non-A non-B Hepatitis were starkly discussed, to the emergence of AIDS – a period when above all the focus should have been on a precautionary approach to the safety of each individual patient. The study involved the conscious decision to treat with concentrates those who, because they had received no or minimal previous treatment, were almost certainly not at that stage infected with Hepatitis B or C (or any other blood borne virus). The implication of the research was that participants would be exposed to the risks of infection, risks that were known to be high, as were the risks that this would progress to chronic liver disease. Evidence of ethical oversight is lacking. So too is the evidence of fully informed consent being sought, with all the implications being fully explained and explored in advance.
The objective of clinicians during this critical period should have been to take every conceivable step to avoid treating such patients with concentrates (still less with commercial concentrates). Instead this research did the opposite.
The minutes of UKHCDO meetings throughout the 1970s and early 1980s reveal that there was a powerful interest in research being undertaken.[1618] It was a regular topic of discussion – but with little or no emphasis on informed consent and patient involvement. Even where research was genuinely retrospective, the culture which it created, and the enthusiasm with which it was pursued, may well have had an impact on clinicians’ decision making and inclined them towards the greater use of factor concentrates, notwithstanding the greater risks associated with that use. Put another way, where there is a possibility that information which is being gathered will be used for a purpose other than the care of the patient, there is a risk that the care of that patient will be “compromised by measures taken more in the interest of the research objective (even sub-consciously) than the pure interests of the patient.”[1619]
An example which illustrates the approach came as early as 1973. It relates to Newcastle and Dr Peter Jones. In April 1973 Dr Jones wrote to Pete Longstaff’s parents, who, he said, would have received a letter from Treloar’s asking for permission for Pete to participate in “the special trial of regular factor VIII injections.” Dr Jones was “in complete agreement with the trial, and that it could do nothing but good for the boys and other patients. It has been most carefully worked out, was discussed at the last meeting of the Haemophilia Directors in Oxford, and has the support of the Medical Research Council.”[1620] Far from doing “nothing but good”, Pete Longstaff was infected with Hepatitis C and with HIV and died “a very painful death”, as a result of those infections, in 2005.[1621]
At the meeting of haemophilia centre directors on 20-21 November 1979, Dr Craske emphasised the view of the Hepatitis Working Party that it was “important for the incidence of chronic hepatitis in haemophilic patients to be assessed.” There was “much discussion regarding the incidence of chronic hepatitis in haemophilic patients, the possible value of liver biopsies and the type of information which Directors would be willing to give to the Working Party.”[1622]
Did this engender a culture in which the focus on science, on research, rather than on the potential impacts of hepatitis on patients and securing the safest treatment for them as individuals shaped the decision making of clinicians?
The submissions made on behalf of those represented by Milners Solicitors point to the treatment, only a few days later, of a child, thought to have mild haemophilia,[1623] treated with Factorate. His medical records read “He will need twice daily cover with cryoprecipitate for at least 7 days to cover the operation”, but the words “or FVIII concentrate” have been added after “cryoprecipitate”.[1624] As the witness says in his statement, “It seems apparent to me that in 1979, at just four weeks old and ultimately misdiagnosed as a mild haemophiliac, I was treated with Armour FVIII and contaminated with HCV at a time when Dr Hill had been alerted to the dangers of NANB and chronic liver disease by Dr Craske.”[1625]
In May 1979 Dr Craske wrote to Dr Anthony Aronstam at Treloar’s referring to a study of NHS Factor 8 that had been going on for almost a year; he suggested that for the second year of the study “some of this material should be used to treat mild haemophiliacs coming up for non urgent operations such as tooth extractions. We have found from observations at Oxford this is the best way of finding out whether the material is associated with cases of hepatitis, as most patients treated under these circumstances will be susceptible to non-A, non-B viruses in the transfused material.” It would, he said, “provide valuable information if you could use some of the material issued in the way I have suggested.”[1626]
This was an astonishing suggestion: that people with mild haemophilia, undergoing non urgent operations (for which alternatives such as cryoprecipitate or DDAVP would be available), should deliberately be treated with Factor 8 concentrates in order to observe whether the material transmitted non-A non-B Hepatitis. Whilst it is right to note that Dr Aronstam expressed total disagreement with this idea, and indicated that he would use either DDAVP or cryoprecipitate,[1627] the fact that the suggestion could be made indicates that there was a culture whereby a determined focus on the pursuit of knowledge relegated the best interests of the individual patient to second place.[1628]
As discussed earlier in this chapter, cryoprecipitate was used as a mainstay of treatment at the Royal Free in the 1970s for longer than in many other haemophilia centres, because of Dr Katharine Dormandy’s enthusiasm for it. But when she died, two new co-directors, Dr Kernoff and Dr Edward Tuddenham, “came in in 1978 and very rapidly changed everybody to concentrate.”[1629] Dr Kernoff had, following work in the US, become “most interested in the aspect of hepatitis and treatment with Factor VIII or Factor IX products”, and according to Professor Tuddenham, “he came in with the knowledge of that and the intention to study it in detail.”[1630]As described in the submissions on behalf of the core participants represented by Milners Solicitors, Dr Kernoff, having developed a special interest in hepatitis in people with haemophilia, “moved to the Royal Free where there existed a cohort of patients largely untreated with concentrates, and had then immediately transferred those patients’ treatment from the comparatively safer cryoprecipitate favoured by Dormandy, to large pool concentrates, with the intention of studying the known higher risk of infection.”[1631]
Writing to Armour in March 1983 to seek funding for “research support into AIDS”, Dr Kernoff described the Royal Free’s haemophilia centre as having “an intensively-followed group of patients who have been exposed to a variety of different types of commercial and non-commercial blood products, and has comprehensive records of treatment extending back for many years. Many of these records are computerized, and the related problem of hepatitis is a major departmental research interest.”[1632]
The British Journal of Haematology carried, in 1985, a report of a study undertaken at the Royal Free Hospital entitled “High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin”.[1633] The scope of this study was described in the following terms:
“During the 5 year period April 1978 to March 1983, 58 patients with congenital deficiencies of coagulation factors VIII or IX received 60 first exposures to factor VIII concentrate, factor IX concentrate or cryoprecipitate at the Royal Free Hospital Haemophilia Centre. Events following 31 of these first exposures, which included five episodes in which ISG was used in addition to concentrate, were prospectively studied by serial clinical assessment and blood sampling before and after exposure. In the remaining 29 instances, problems of patient accessibility and compliance prevented the acquisition of adequate prospective data. Evaluation of outcome in this latter group was therefore retrospective, and largely limited to analysis of clinical rather than biochemical or serological information. Unless otherwise stated, data given in this report refers only to prospectively studied patients.”[1634]
The report explains that of the patients studied, “Only a minority of the patients were ‘virgin’ – although most needed infrequent treatment, a majority had received blood, plasma or cryoprecipitate therapy before their first exposure infusions.” It is clear, therefore, that some of the patients were “virgin”or “PUPs” (previously untreated patients) and that most of the patients needed infrequent treatment. It was known to those conducting the study that “patients who have been infrequently or never previously exposed to blood products are at higher risk”: the report expressly so states.[1635]
The report continues that
“Of the 30 patients who were studied prospectively (one patient received first exposures to both cryoprecipitate and concentrate), 13 had haemophilia A, four had haemophilia B, and 10 had von Willebrand’s disease. Three female carriers, two of haemophilia A and one of haemophilia B, were also studied. Five patients (six exposures) were aged less than 5 years at the time of their first exposure, and nine were aged between 5 and 20 years ... Of the patients with haemophilia A or B, seven were classed as haematologically severely affected, having less than 1 u/dl circulating factor. Treatment was given either to stop bleeding or as prophylaxis before surgery.”
It follows from this data that ten of those with Haemophilia A or B did not have severe haemophilia.[1636]
The extent of the participation of children speaks for itself.
In relation to each such patient, blood samples were taken and the patients clinically assessed immediately before their first exposure infusions, and thereafter at 1-2 weekly intervals for 3 months and 1-2 monthly intervals for a further 6 months. Biochemical liver function tests were carried out on all blood samples “and were normal in all patients before first exposure infusions.”[1637] It is apparent from this – and explicitly recorded in the report in any event – that this was a prospective study: the patients were already being studied at the point in time at which the treatment was given. Yet there is no evidence whatsoever that the patients themselves were made aware of that.
Under the heading in the report “Ethical and legal considerations”, it is recorded that: “ISG and Kryobulin-G are unlicensed products in the U.K. and were used on a ‘named patient’ basis under the provisions of the Medicines Act 1968. The nature of the study, and the reasons for wishing to use these products, were explained in detail to all recipients and their verbal consent obtained. The study had institutional Ethical Committee approval.”[1638] The clear inference from this paragraph, and in particular from the phrase “these products”, is that the explanation about the study and the seeking of verbal consent was only in relation to the patients (five in total) who were receiving the unlicensed products ISG (immune serum globulin) or Kryobulin-G (a product comprising a mixture of Factor 8 concentrate and ISG).[1639] The majority of the patients, accordingly, did not have the nature of the study explained to them, nor was their consent obtained.[1640] No evidence of any broader ethical committee approval has been found.
The results of the study were that none of the 5 patients treated with cryoprecipitate developed hepatitis; all 9 patients treated with commercial Factor 8 concentrate, and 10 of the 12 patients treated with NHS Factor 8 concentrate, developed acute non-A non-B Hepatitis (as did the 4 patients treated with NHS Factor 9 concentrate). A table within the report provides more details of the treatments administered to the patients on the study. A 4-month-old baby, an 8-month-old baby, a 27-month-old baby and a 4-year-old child, all treated with concentrates,[1641] all developed hepatitis. The 19-month-old baby treated with cryoprecipitate did not.[1642]
In its conclusion, referring to the importance of studies of new products of possible reduced infectivity, the report noted that critical to the evaluation of such new products would be patients who were “first exposure recipients”, but added “One problem of such studies will be patient accrual, since many patients with mild bleeding disorders, who in the past might have been considered suitable for therapy with concentrates, are now considered more appropriately treated with cryoprecipitate or desmopressin (DDAVP).” According to the report, the duration and dosage of therapy, and the choice of therapeutic product, “were influenced by clinical circumstances, local availability of products, and departmental policies which operated at the time treatment was given.”[1643]It might be said, on the basis of this, that the study was not the driver of the choice of treatment.[1644] I have considered whether the patients were enrolled because they were receiving clinical treatment appropriately involving concentrate for the first time (or when they had received only little of it before), such that the study was merely incidental to “normal” treatment, but from all the material before the Inquiry this seems unlikely.. This was a prospective study (the report says so) run by a clinician, Dr Kernoff, who was keen to study the known “higher risk” of infection. Previously untreated patients, minimally treated patients, patients with mild haemophilia, and children were treated with concentrates at a time when safer treatments (in terms of viral transmission) existed. Research is the obvious explanation for their treatment with concentrates.
Professor Christine Lee argued in her evidence to the Inquiry that the study was “retrospective in the sense these people were not recruited to go into a study. They were people who came in with a bleeding problem, and then they were retrospectively identified. And because there had been the collection of the samples and the results of the liver function tests, it was possible to retrospectively analyse that information.”[1645] I reject this description, which is not consistent in any event with the report of the study that was published, and which would not explain why so many participants were treated with concentrates when a different treatment would have been an obvious and safer choice.[1646]
The Inquiry heard evidence about three individuals who were in all likelihood patients treated as part of this study and infected with Hepatitis C in consequence of that treatment: Mark Stewart, his brother Angus, and their father, also Angus.[1647] All three had von Willebrand disorder – Angus senior’s condition being so slight that he went undiagnosed until his sons’ diagnosis as children.[1648] As noted in the submissions on behalf of the core participants represented by Milners Solicitors, “The idea that he required factor concentrates at the very point in the time of the study, having not had them during the first 30 years of his life, defies the credibility of any suggestion that the study was restricted to severe haemophiliacs, or those who had a significant need for the treatment.”[1649] All were treated at the Royal Free for the first time with concentrate within the timeframe of this study.
Angus, Mark’s father, died in 2002, having developed hepatocellular cancer.[1650]
Mark’s brother Angus was diagnosed with liver cancer in 2008. He died in 2013.[1651]
Mark told the Inquiry that he lives “in fear of suffering the same fate and often feel it’s only a matter of time before something similar happens to me.”[1652]
Neither Mark nor his brother nor his parents were warned of the risks of treatment with concentrate, nor that liver function would be tested and monitored. Mark learnt he had Hepatitis C only in 2007.[1653]
Professor Lee provided a written statement to the Inquiry in response to Mark’s own written evidence. Her statement said that treatment for von Willebrand disorder was (until the mid 1990s when treatment with large pool concentrates became possible because of improved von Willebrand factor content) with cryoprecipitate; that DDAVP was a treatment for mild to moderate von Willebrand disorder which came into use from around 1981;[1654] and that Mark was treated with Factor 8 concentrate in 1981.[1655] Her statement concludes as follows:
“it was not known at the time that the blood products used to treat patients with bleeding disorders resulted in these patients becoming infected ... We were certainly not conducting research on these patients. Importantly, we were using previously collected samples to conduct retrospective analysis of our data in order to understand the natural history of non-A non-B hepatitis to aid diagnosis and prospective treatment.”[1656]
For the following reasons, I do not accept this explanation. It was certainly known, at the time when this study was being undertaken, that blood products transmitted non-A non-B Hepatitis. The study described above was undoubtedly research and it was prospective in nature, rather than a retrospective analysis of data. I have no doubt too, from the facts set out already, that this research most probably influenced the choices of treatment, and that consequently participants in the study were treated with concentrates when they should not have been.[1657]
In Scotland, as elsewhere, interest in people with bleeding disorders as objects of research was never far away. At a meeting of the Haemophilia and Blood Transfusion Working Group in Edinburgh in November 1983, for example:
“Dr [John] Cash reminded members about the collection of data on liver function tests of ‘virgin haemophiliacs’, and raised the question of the number of virgin patients available in Scotland. Dr [Charles] Forbes said that there were not enough virgin patients. He was however writing up his experience of hepatitis in 12 mild cases treated with PFC VIII. This data he would submit to Dr Cash. It was agreed to wait until Dr Forbes’ data was available before considering the use of English patients. When there was a sufficient amount of the new product available Dr Ludlam would be prepared to try it out.”[1658]
The group of bleeding disorder patients treated at the Royal Infirmary of Edinburgh was regarded as “unique” in being exposed to concentrate “only from the local blood transfusion service and not, as in other centres, commercial concentrate”. Abnormalities of liver function in these patients, and evidence of deterioration since the introduction of pooled concentrate, were “therefore of considerable interest”, according to a study published in the Journal of Clinical Pathology in 1981, assessing the liver function of “38 Edinburgh haemophiliacs” over a five year period from 1974.[1659] Furthermore, Edinburgh was one of the centres which had a “longitudinal sera store”.[1660]
Professor Ludlam, in his oral evidence to the Inquiry, accepted that a fundamental principle of medical research was that the participants or subjects give their informed consent.[1661] He suggested that most of the investigations that were being undertaken in Edinburgh, “although they were labelled as research, were in fact for the ongoing evaluation of the patient ... for the ongoing benefit of the patients. And patients were actually quite interested to learn a bit more about the research, and we were happy to tell them.”[1662]
On 19 January 1983 Dr Ludlam attended the meeting of the Hepatitis Working Party in Oxford, where Dr Craske reported that ten cases of AIDS had occurred in Haemophilia A patients in the US (the youngest aged seven), five of whom had since died, and that it “seemed possible that factor VIII or other blood products administered to these patients might be implicated”; three cases associated with whole blood or platelet transfusion were also discussed.[1663] The main “defect” in these cases was “a disorder of cell mediated immunity” and there was discussion of studies of T-cell helper/suppressor ratios.[1664] Dr Craske suggested that “one study which might be contemplated was a prospective study of the effects of various factors of cell mediated immunity in haemophilia A patients, especially the comparison of the effect of NHS factor VIII treatment compared with that of U.S. commercial factor VIII.”[1665]
Within a matter of weeks, in March 1983, Dr Ludlam embarked upon the “AIDS Study” (as the tests were labelled)[1666] in Edinburgh, supported by a grant from the Scottish Home and Health Department. In collaboration with a colleague at the Western General Hospital in Edinburgh (Dr Michael Steel), the immune function of haemophilia patients treated at the Edinburgh Centre was studied.[1667]
On 28 May 1983 a letter written by Dr Ludlam was published in The Lancet. It was in response to a letter in the same publication the previous month from Dr Robert Gordon of the National Institutes of Health in Maryland. Dr Gordon had encouraged studies of T-lymphocyte subpopulations in haemophiliacs treated with blood products.[1668] Dr Ludlam’s letter in response published the “preliminary results of a study of haemophiliacs in South-East Scotland”. The results showed immunosuppression in a number of those studied,[1669] and Dr Ludlam speculated[1670] that this might result from “foreign protein or a ubiquitous virus rather than a specific AIDS virus in the factor VIII concentrates”.[1671] As submitted on behalf of the core participants represented by Thompsons solicitors, “The fact that [Dr Ludlam] was contemplating that there was such a virus clearly meant that he knew that there was a risk that the products were harmful as a result of this putative virus, yet he continued to allow his patients to be exposed to that risk. They were a group which appeared at that time to be of interest in the emerging knowledge about the disease.”[1672]
The final results of the immune function research were published in The Lancet in June 1984. The study found evidence of immunological abnormalities, which the authors thought resulted from intravenous administration of blood products; the report also recorded the presence of deranged liver function and chronic liver disease.[1673] Even if unrelated to AIDS, those studied should have been told of these findings. They were not.[1674] The continuation of the existing treatment regime should have been reviewed with the individual patients, in the light of the threefold risk that Professor Ludlam had recognised in early 1983. It was not. The fact, as it now appeared, that (whether or not it was a precursor of AIDS) the giving of blood products intravenously caused derangement of the immune system was known to the clinicians concerned (they reported it in The Lancet) and ought to have been shared with the patients first.
Following the publication of The Lancet study in June 1984, there was a further investigation of immune function in autumn 1984 to ascertain whether there were any significant changes in helper and suppressor numbers or the helper/suppressor ratio between 1983 and 1984. Patients remained in the dark that these investigations were being undertaken. They were published in The Lancet in August 1985. The conclusions in that publication included: that the chance of developing HTLV-3 was dependent upon, in addition to the helper/suppressor ratio, the number of transfused vials of infected Factor 8 and the total annual consumption of Factor 8.[1675] These conclusions were not shared with those being studied, so that they might understand how, when and why they had become infected.
There was no ethical committee oversight of the 1983 AIDS Study.[1676] Patients were not told that this study was being carried out and were unaware of it.[1677] Professor Ludlam thought this was not actually research, but rather was monitoring the health of his patients. I do not think he was right in this, for the following reasons. It was not part of the routine monitoring of their bleeding disorders. It involved the testing of the immune function of blood samples as well as skin tests (Professor Ludlam accepted that skin tests were research but he said they were also done to monitor the health of the patients, and contribute to their care).[1678] There is no tenable difference in principle between the skin tests and the taking of blood samples as he described them, because he said that both were done to monitor the health of the patient. A distinction volunteered by him in evidence was that the skin tests were intrusive. I cannot see that this is any more the case than blood tests, especially since both involve puncturing the skin.[1679] Further, his description of testing to monitor the health of patients makes little sense unless there was some yardstick which would enable a clinician to see that a particular result indicated a particular state of health or of deterioration in health. Yet as I understood his evidence, he was conducting the tests in order to find out if there was any correlation between results and states of health: this is a process which is research – in order to discover what results meant, not in order to check them against an established meaning. Finally, the fact of publication indicates this was research, as the medical ethics experts to the Inquiry pointed out.
It follows that I cannot accept Professor Ludlam’s evidence on this point.[1680] It was undoubtedly research, despite his suggesting otherwise.[1681] Patients were never informed of the results of the investigations and the studies led to no review of the treatment regime. It did, however, lead to publications in Dr Ludlam’s name and those of his colleagues.
His own description of the AIDS Study to the General Medical Council was as follows: “The background to this research project was to investigate the immune status of haemophiliacs in Edinburgh who had been treated exclusively with factor VIII concentrate prepared from Scottish blood donors ... The above research project was part of a more extensive research project into infections transmitted by clotting factor concentrate.”[1682] It was set up “in direct response to the AIDS threat.”[1683] Having discovered that some of the Edinburgh patients had “immune abnormalities”, it was, according to Professor Ludlam, “imperative to monitor their evolving immune status”, which was done “when they were having blood taken for other routine investigations.”[1684] In other words, it was in essence more a process of discovery than of treatment.
This investigation, however, was undertaken without the knowledge or agreement of the individuals in question. Had they been informed about the studies being undertaken they would also have to have been told why, and would then have become aware of the dangers of the treatment they were receiving. Some or all may then have refused to continue to be treated with concentrates. They would not then have been infected with HIV.
In MRC News it was observed, of the “Edinburgh Haemophiliac Cohort”, that “we have had the opportunity to study a unique group of haemophiliacs who became infected in the Spring of 1984 by transfusion of a single batch of factor VIII concentrate ... This cohort of haemophiliacs has become one of the most extensively studied groups of HIV infected individuals in the world.” The “success” of the project was described as due to “the close collaboration between a group of investigators with a variety of medical and scientific skills.”[1685] It is a sad reflection that this extensively studied cohort was for the most part left in ignorance of this work.
In Glasgow research was carried out in 1983 by Dr Forbes (with colleagues) on the “cellular immunity of a group of Scottish patients with haemophilia who were treated with factor VIII derived exclusively from Scottish donors and prepared by the Scottish Blood Transfusion Service.” Of the 19 patients so studied, 5 had also received commercial concentrate during the past two years and only 2 had never been treated with commercial concentrate. The results of the study, published in the British Medical Journal in October 1983, showed that they had immunological abnormalities “similar to those in their American counterparts”.[1686] Professor Lowe thought that this study commenced sometime in 1982 and that it was “very much” triggered by reports from the US of AIDS in people with haemophilia.[1687]
No evidence has been given to this Inquiry to suggest that the individuals involved in the study were told that their immune functions were being investigated, or of the purpose of the investigations.[1688] However, it is right to note that Professor Forbes told the Penrose Inquiry that patients “were just asked if they would mind giving a sample of blood, that we were going to look at some immunological tests that required fresh blood samples, to look at their cells and see if there was anything happening that we should know about.”[1689]If this was what was said, it is not easy to describe it as “informed” consent, especially given the purpose of the investigations. Nor were patients told of the results of the investigations.[1690]
The final paragraph of the published article stated that “Whether these abnormalities in the T cell ratios and [a lymphocyte function test] are sufficient to render the patients immune-deficient and therefore, possibly, in a prodromal stage of the acquired immune deficiency syndrome, will become apparent as the patients are followed up clinically.”[1691] Thus the authors recognised the possibility that the patients may already be infected (and infectious), yet nobody was told and there is no evidence to suggest any alteration in the treatment regime.
This was followed by the study, published in The Lancet in December 1984, which reported on the HTLV-3 testing of 77 Scottish haemophiliacs and 22 Danish haemophiliacs.[1692] The Scottish patients were not informed that they had been and were being tested, and were not informed of the results of these tests (11 Haemophilia A patients and 1 Haemophilia B patient were HTLV-3 positive), which must have been known by October 1984.[1693] The study also reported on a Scottish patient who had experienced symptoms typical of AIDS during his last seven months (in other words, since early 1984, as he died in late October 1984), a development which did not appear to lead to any change in the treatment regime in Glasgow or to the information provided to patients.[1694]
In the early 1990s various clinical trials were conducted in relation to the SNBTS product HPVIII (high potency Factor VIII), also known as Tartan Factor 8 and licensed as Liberate.[1695] These trials included children as young as nine months old.[1696]
The patient information for trials HP012 and HP013 informed patients that the product was prepared from plasma collected from unpaid Scottish and Northern Irish blood donors, who were all tested for the presence of Hepatitis B surface antigen. It made no other reference to viral risks. In particular it did not refer to non-enveloped viruses such as parvovirus.[1697] The trial protocol for HP014 contained no patient information. The patient information for trial HP016 referred to donors being tested for the presence of antibodies to HIV and for the presence of Hepatitis B surface antigen but said nothing about other viral risks.[1698]
SNBTS’ application for clinical trial certificate exemption described the viral inactivation process as “designed to inactivate lipid enveloped viral pathogens.”[1699]
A number of child participants in these trials seroconverted to parvovirus B19. These included children who were, at first infusion, aged 9 months, 11 months, 12 months, 18 months, 2 years (3 children), 3 years (2 children), 5 years, 6 years and 7 years.[1700]
At a meeting of haemophilia directors, SNBTS and Scottish Home and Health Department (“SHHD”) officials in May 1994 the trials were discussed and it was said that in general terms haemophilia directors and patients “were very pleased with this product.” But it was noted that “Concern had been raised in relation to viral safety, particularly of Hepatitis A and Parvovirus transfusion via solvent detergent virus inactivated products such as HP VIII.”[1701]
Professor Ludlam described the importance of parvovirus in these terms to the Inquiry: “it can cause severe disease in some individuals (e.g. hydrops fetalis[1702] and severe arthropathy[1703]). It is also important because it is a non-lipid coated DNA virus that is resistant to some heat treatments and solvent-detergent action.”[1704]
Thus, even in the 1990s – at a point in time at which lessons which should have been learned from the transmission of HIV and Hepatitis B and C, and the fundamental importance of providing clear and unequivocal information about risks of viral transmission to participants in research should have been at the forefront of the design of clinical trials, and that safety was paramount – children were being recruited to clinical trials being organised by SNBTS without proper information about the risks being provided. This was unethical and wrong.
The Inquiry heard evidence from Mr AB, the father of twin boys treated at the Royal Hospital for Sick Children in Yorkhill – boys who were treated with commercial concentrates, prophylactically, from the age of three.[1705] That such treatment was utterly wrong – wholly unethical – will be apparent from the next section of this chapter which focuses on the treatment of children. Both boys were infected with HIV. One of them died of AIDS at the age of 17.[1706] Mr AB’s written statement to the Inquiry explained:
“It now appears from the records and from my boys’ diagnoses that they were being tested over a number of years for HIV, Hepatitis B and Hepatitis C. That my wife and I were not told about that makes me angry and upset that there was a lack of control over what was happening to our children and that they were being treated like lab rats. It has undermined my trust in doctors and the NHS.”[1707]
When he gave oral evidence to the Inquiry, he explained in addition how he and his wife were asked to give permission to a post-mortem.[1708] They did so, but understood that body parts including his brain would not be removed. This was, understandably, important to them.[1709] “In summary”, he said, “we had not given informed consent to the post-mortem”.[1710] Subsequent to his oral evidence, Mr AB received previously undisclosed medical records. His response is best conveyed in his own words:
“I was shocked and uncontrollably distressed by the disclosure and content of these records, because until then I was unaware as to the nature and extent of the post-mortem, let alone the taking of so many samples of my late son’s body parts, and the fact that they had been circulated amongst various medical schools, individual researchers, and organisations unknown to me and all without my permission.”[1711]
He stated that the dignity of his late son had been abused and wanted the Inquiry to appreciate the catastrophic impact on him and his entire family.[1712]
Whilst the doctors in question have not accepted that there was a lack of informed consent to the post-mortem,[1713] the point made by Mr AB is a powerful one, namely that:
“The fact is though neither myself nor my late [wife] fully understood what we were being asked to agree to. Whilst I knew what a post mortem was I did not understand what was entailed, and I learn more about this when I see statements, reports and medical notes concerning my late son and his death ... It would be useful to set out in straightforward language, in writing, why a post mortem is required, the potential ‘benefits’; and the downside to not giving consent.”[1714]
In his submissions to the Inquiry he has emphasised “a lack of respect and dignity in the care and treatment that my family and late wife had to experience, as the medical model failed to respect victims and families. At the time research was being done without parental permission and this left a drastic impact on individuals and families’ lives. As one example of this, being informed through the Inquiry of the unauthorised post mortem distribution of body parts was devastating.”[1715]
Dr James McMenamin and Dr Dermot Kennedy have told the Inquiry that at the time a consent form was signed by Mr AB neither of them was in possession of “full” information relating to the nature and extent of the post-mortem: the post-mortem itself and all associated decisions, before, during and after the post-mortem were in the full control of the pathologist and neuropathologist who were to perform it – and the doctors make the valid point that they could not pass on information they did not have. It seems that neither the treating doctors, nor Mr AB had the information which it was necessary for Mr AB to have had.[1716]
As to lessons to be learned from Mr AB’s distressing account, had the process of consent been that which is now seen as appropriate rather than the practice as it was in 1992, it seems likely there would not have been the lack of information which Mr AB needed to have, and that the system would have been such as to ensure that the doctors concerned were in a position to give more detail, more accurately, than happened. The last word, however, belongs to Mr AB. He said if only one lesson were to be learned from the Inquiry “this should be that the medical profession accepts that it must be honest and transparent at all times.”[1717] That fundamental lesson is the entire message of this chapter.
Medical research is important and its benefits can be immense. No-one should be frightened of research. Essentially it is about adding important knowledge to our existing understanding. Research may not produce a benefit in itself – but that does not mean it is worthless, for learning that something apparently promising, or even long accepted, actually does not work is a valuable addition to knowledge in itself.
People who participate in research should feel able to be proud of that fact. Researchers, whether academic or clinical, will not only feel proud that they have contributed to the store of human knowledge, but where their research is accepted for publication may gain professional kudos. That, as well as the public good, can be a powerful incentive. None should ignore the fact that without their patients, whose experiences then form part of the published research, there would be no research, and no publication. Those patients never get the kudos, though they may share the pride in advancing knowledge which benefits others – if they know that they have participated in research, what they have participated in, and what the results have been. If, as is now well accepted, the clinician-patient relationship is one of collaboration in the treatment of the latter informed[1718] by the expertise and expert knowledge of the former, then that is the least they should know. However, the evidence before the Inquiry has shown that in the great majority of cases they did not. They did not feel the pride they might have had where the research was useful: that pride, and the professional esteem that came with it, was the sole preserve of the clinicians who had conducted this research on them without their knowing (or in the case of Liberate, without being fully informed).
In particular, it should be clear what personal benefit patients should expect from research which involves them. If it does not potentially lead to an improvement in their own treatment, they should be told that in the clearest possible terms, for they will then potentially be prejudicing their health for the sake of improving the health of others. Ideally, the researcher or clinician who asks them to do this should not be one who is currently (or prospectively) treating them, for the power imbalance in the clinician-patient relationship may then make the patient feel obliged to accept participation in a study, or be fearful of damaging the relationship if they do not. It is much easier to say “No” to a third party than it is to someone much closer.
Where children are an obvious focus for research[1719] the need for it to be of benefit for the child in their own treatment becomes critical. Children cannot themselves consent to suffering harm in the hope that by their doing so other people might benefit, unless there is at the same time clear personal benefit in their own immediate treatment. The law is clear that the best interest of the child is a paramount concern. Parents should never be asked to provide consent for their child to undergo any such process: it is probably unlawful for them to give it, even in respect of their own child.[1720]
None of the research described in this chapter led to patient benefit. None of it led to safer treatment. Worse still, much was undertaken with no reasonable prospect of advancing the immediate personal treatment of the patient. At Treloar’s, for instance, a trial of prophylaxis involved one half of a cohort of children being given concentrate (which was known potentially to be harmful) at levels where it was believed it would probably do them no good, in order that it could be shown how much better children in the other half had fared.[1721] Giving children factor concentrate, known to transmit hepatitis, was likely to do them harm without any counterbalancing benefit to them. Dr Craske’s letter to Dr Aronstam, asking for previously untreated patients to be given factor concentrates even though their own treatment might not require it, was an invitation to him to cause his patients to suffer potential harm without any realistic expectation of personal benefit in their treatment. Of course, Dr Craske wanted treatment as a whole to be improved in the long run by the knowledge this would yield; and of course he recanted (under pressure from Dr Aronstam’s retort) from the suggestion in his letter, so far as Treloar’s was concerned, but his mindset was clear. He had already shown this in writing. And the implications are chilling.
There is a real danger that a desire to study a group of patients becomes the central focus rather than the interests of an individual patient in the progress of their treatment; that those interests, and patient safety, slip to become second best to the interests of research. Dr Craske’s letter, and the mindset it indicates, suggests that there was often pressure to provide treatments which both treated a bleed and serviced a general desire to help to progress research. It is not difficult to see how combining the two objects may lead to a treatment being given which would not (but for the fact of research) have been given. To an extent, an inclination to favour research may have been natural among many haematologists of the time, for haematology was principally a laboratory based discipline until the early 1970s, and was then becoming a more clinical one. It is understandable that those who had spent much of their professional lives working mainly in a laboratory setting might be more interested in research, and give it priority.
It may not entirely be surprising therefore that a heavy emphasis was placed on research by principal haemophilia centres: but being unsurprising does not mean it was acceptable to conduct it in many cases. Moreover, this chapter has shown that it was often conducted in ways that were unacceptable.
There is no doubt that patients were frequently viewed as research subjects rather than first and foremost as individuals with varying clinical needs whose informed consent should have been central to the studies that were undertaken. The Treloar’s chapter begins its section on Research by recording that it was in the 1960s that the “nearly 40 haemophiliacs in the College”provided“an opportunity for research”;[1722]which by 1979 had become a “necessity” since the “concentration of haemophiliacs found at Treloars is unique within Britain.”[1723]
Core participants have emphasised this point. They are right to do so. As Thompsons submit “Campaigners from the bleeding disorder community have described themselves as ‘useful material’. They have done so in order to illustrate the extent to which they rightly feel dehumanised by this process. They reasonably interpret the way that they have been treated as being [as] the guinea pigs of a medical profession”.[1724] Importantly, they were regularly treated in this way without their knowledge or consent as if (again in the words of Thompsons) this was a part of treatment which had saved them “from an early death or life as a ‘cripple’” and the use of “their material [ie sera] without their knowledge or consent being the price they should pay for what they had received.”[1725]
Patients were regularly monitored for the presence of diseases that might be transmitted by their treatment. Blood samples were taken from them repeatedly without any clear explanation of what they were for. Samples were retained, without the knowledge and consent of those whose blood it was. Some – possibly many – people with bleeding disorders were involved in research without their informed consent. Some of that research exposed them to greater risks. This was simply unethical.
There is limited evidence of any kind of effective oversight by ethics committees in the 1970s and early 1980s.
In short, this chapter has dealt with four major failings in relation to research:
These failings have been aggravated by the way in which previously untreated patients – in particular children – were sought out to become the subject of research, and in some cases to be given treatments which were unnecessary, or conferred no advantage but only additional risk. The ethics of this are clear. It was, and is, unacceptable.
The result of people discovering that they were tested, made subject of research, and then not told the results, and might have been given risky treatment more to advance research than their own personal interests, has had two serious practical consequences. The first is loss of trust in the NHS, and in doctors generally, to the extent that many feel they may have been given treatments not because they needed them but rather to see what would happen, whether this can in their individual case be proved or not. The second is that the failures have seriously compounded the harm to which individuals had already been exposed, as has been powerfully conveyed by the evidence of Mr AB. An insult to patient autonomy, which the combination of these failings constitutes, is not something which is a concept burrowed deep in a textbook on Medical Ethics and nothing more. It has a real impact on personal lives; it aggravates the psychological impact of what has happened; it is dehumanising.
It can easily be overlooked that, with rare exceptions, bleeding disorders like haemophilia and von Willebrand disorder are lifelong conditions. People have them from birth. Accordingly, throughout the periods of particular interest to the Inquiry, there has always been a continuous pattern of people needing treatment for the very first time, when particularly vulnerable. This simple fact argues eloquently that clinicians need to be particularly astute to ensure that as risks of treatment to those who are adult become apparent, clinicians learn – and, in the light of that learning – avoid those risks coming to affect those children who are new to treatment.
Safety is paramount for all patients. But nowhere is the need for it more visible, and a lack of respect for it of greater importance, than in the case of children.
Around 380 children with bleeding disorders were infected with HIV.[1726] Many of those died in childhood or young adulthood, having endured a level of pain and fear that no child or young person should ever have to face. Some survived but have lived their entire lives under the shadow of HIV and AIDS, with an appalling toll on their physical and mental health.
All those children who were infected with HIV were likely[1727] to have been coinfected with Hepatitis C. Others escaped HIV infection only to learn later that they had been infected with Hepatitis C, sometimes with deadly consequences; and those who survived have also suffered profound ill health and endured the horror of the early treatments with interferon. Some were also infected with Hepatitis B and with other viruses.
How did it happen that in the second half of the 20th Century so many children could be infected with fatal viruses from their NHS treatment? In seeking to answer this question, this next part of this chapter will look at the available evidence about treatment practices at seven paediatric haemophilia centres. Treloar’s is considered in a separate chapter.
Alder Hey Children’s Hospital was the principal Liverpool site for the treatment of children with bleeding disorders from at least the late 1970s onwards, treating children from the Merseyside area and North Wales. In around their mid teens children would then transfer to the Haemophilia Centre at the Royal Liverpool Hospital.[1728]
Dr John Martin was the director from the mid 1970s. He was not a haematologist.[1729]
The annual returns for Alder Hey show a distinct shift from cryoprecipitate to concentrate from the late 1970s to the early 1980s for the treatment of patients with Haemophilia A. The Centre’s use of products in 1977 is unclear: the 1977 return recorded 643 packs of cryoprecipitate but in relation to concentrates, no figures were provided and the return contained the handwritten statement “as supplied by Dr F E Boulton Liverpool Royal Infirmary.”[1730] The 1978 return, whilst also confusing, showed the use of cryoprecipitate and both NHS and commercial concentrate,[1731] as did the return for 1979.[1732] However, in 1980 the use of commercial concentrate (Factorate) increased[1733] and in 1981 Alder Hey treated its haemophilia patients almost exclusively with concentrate (both NHS and Factorate).[1734] This pattern continued in 1982 with the Centre using almost exclusively concentrate, most of which was commercial,[1735] and in 1983 where the return recorded the almost exclusive use of concentrate, mostly Factorate.[1736] In 1984 Alder Hey treated its Haemophilia A patients only with concentrates, both commercial and NHS.[1737] The 1985 annual return is missing. In 1986 Alder Hey treated its Haemophilia A patients only with concentrate.[1738]
Although the returns themselves are imperfectly completed, what is clear is that cryoprecipitate gave way to concentrate and that in 1983 and 1984, when it would be expected that haemophilia centre directors treating children would strive to avoid treatment with commercial concentrates, Dr Martin did the opposite. That this was his approach to treatment is all too apparent from two medical reports regarding Dr Martin’s treatment of a child patient, Stephen Hallwood. Stephen and his brother Brian were both infected with HIV as a result of their treatment at Alder Hey and died in childhood.[1739]
The first report was prepared by Dr Savidge in 1992. It reveals that Stephen, at the age of just two years old, was treated with US commercial concentrates on 32 occasions in the course of 1982.[1740] He was treated with US commercial concentrates repeatedly again in 1983 and 1984, including as late as December 1984.[1741] In early 1985 Stephen was twice treated with unheated US concentrates.[1742] Dr Savidge’s assessment of his treatment was scathing:
“There are two notable features of this case with respect to the adopted therapeutic approach. Firstly, there is no documentary evidence to suggest that single donor pool cryoprecipitate was ever contemplated in the management of this case, not even when the patient was initially treated. Secondly, there is evidence to indicate a defined preference to use U.S. commercial products (45 treatments) over NHS factor VIII concentrate (9 treatments) during the period 1982-1985 when initially only unheated, but subsequently heated products were available.
In the late 1970s and early 1980s, the majority of U.K. paediatricians treating infants and children with severe haemophilia considered cryoprecipitate obtained from single blood donations to be the therapeutic product of choice, but if not available NHS factor VIII concentrate should be used ... The lack of consideration and disregard of the then current therapeutic recommendations for the treatment of children under the age of 4 years regarding the use of cryoprecipitate in this case was negligent ... The overwhelming use of commercial U.S. concentrates in preference to cryoprecipitate or NHS factor VIII is remarkable, particularly in a large city such as Liverpool known to have an active BTS with facilities for cryoprecipitate production and regularly supplying plasma to Elstree for fractionation. The lack of a well-defined therapeutic policy regarding preferential use of domestic plasma derivatives in children at this time was negligent”.[1743]
As for Dr Martin’s decision to treat Stephen with unheated commercial concentrates in January 1985, after the issue of UKHCDO’s AIDS Advisory Document:
“Despite this information with which a competent practicing paediatric haematologist could be expected to be conversant, and a further report by Bloom in January 1985 (Lancet i, 336), which stated that at least 2 batches of NHS concentrate had transmitted HIV and urged the use of heat treated concentrates, Stephen ... was given two infusions of unheated US concentrate in January 1985 and two infusions of unheated NHS concentrates in March 1985. The infusion of these untreated therapeutic agents at these times when heat treated concentrates were commercially available was negligent”.[1744]
Sadly, there is no reason to think that Dr Martin’s treatment of Stephen was atypical. His brother Brian was treated with commercial concentrates from the age of two.[1745] Such treatment continued after the June 1983 letter sent on behalf of UKHCDO to all haemophilia centre directors and after the December 1984 meeting of reference centre directors and others at BPL.
The second report relating to Stephen’s treatment was prepared by Dr Ludlam. Dr Ludlam noted this:
“In Dr Martin’s evidence it is stated that he was aware of the risks of hepatitis transmission by concentrates, that cryoprecipitate was effectively phased out in 1980 and that treatment was advised by the Royal Liverpool Hospital (RLH). It is therefore necessary to know what policy was operated by the RLH. Dr McVerry’s evidence does not accord with this[.] Why was it decided to phase out cryoprecipitate in 1980? Was there a policy about which patients should receive NHS and which commercial concentrates? Why was concentrate purchased from Armour rather than another supplier? The patient could have been treated effectively with cryoprecipitate in the first few years of life whilst receiving treatment as an out-patient. If cryoprecipitate was not available then NHS concentrate would be the most appropriate therapy.”[1746]
The “evidence” of Dr Martin to which this report referred was a statement prepared for the purposes of litigation, in which Dr Martin said that “there was certainly no instruction to use cryoprecipitate for mild haemophiliacs or that it should be the treatment of choice in particular circumstances”. Cryoprecipitate was said to have been “phased out in the early 1980’s and was not generally available in the hospital.”[1747] He did not regard the risk of hepatitis as a reason to alter any treatment regime.[1748] His aim was, he said, “to keep children out of hospital as much as possible.”[1749]
His aim should have been to treat children as safely as possible. Instead he exposed them to wholly unnecessary risks.
Dr Martin had no recollection of the 24 June 1983 letter from Professor Bloom and Dr Rizza but accepted that he would have received it; however, in his own words: “There was no alteration in the treatment regime at this time as a result of the letter.”[1750]
Dr Martin was the director of the haemophilia centre at Alder Hey. It was a separate, recognised centre, with its own centre number (065), and Dr Martin was clearly identified as the director on the annual returns which he submitted. Dr Martin did not attend any UKHCDO meetings in the 1970s and 1980s: that can only have been a matter of choice on his part[1751] and provides no excuse or justification for the utterly inappropriate treatment policies and practices at Alder Hey under his directorship. The minutes would have been sent to him and it was his professional responsibility to keep up to date.
Information from legal claims relating to other children treated at Alder Hey reveal the same approach to treatment.[1752] They detail a child treated with concentrates from an early age at Alder Hey until May 1984 and then from Glynedd Hospital, North Wales, on home treatment.[1753] Another child was treated with concentrates from 1978 onwards and this was described as “the policy at Liverpool Children’s Hospital”; the records did not identify the type of batch number (in itself a clear indication that no batch dedication policy was followed) and the child was treated with commercial concentrate in January and December 1983.[1754] A patient with mild/moderate haemophilia was treated with concentrates for elective surgery in September 1983. Their notes were “insufficiently detailed” to identify the products used but “Dr Martin’s statement confirms that no distinction was made at Alder Hey Hospital in terms of which product to prefer and the product he would have received would have been that which was available.”[1755] Another child with mild haemophilia was treated with what appeared to be NHS Factor 8 in late 1982 and commercial Factor 8 between March and July 1983.[1756] A child born in 1980 (inferentially with severe haemophilia) “received a substantial amount of concentrate, the majority of it being commercial concentrate. The type of concentrate would have been dependant [sic] upon availability and treatment was standard.” It was said that there was “Nothing atypical about treatment given to this Plaintiff.”[1757] That in itself is damning. A child with mild haemophilia had received “commercial Factor VIII in December 1983 for a tooth extraction”; this treatment “would not seem to be justified.”[1758] A child with severe haemophilia was regularly treated at Alder Hey with concentrate, “at least some of it commercial after mid-1983.”[1759] Each of these children was infected with HIV in consequence of their treatment.
A medical report on a child born in 1981, with moderate haemophilia, shows that he was treated with concentrates from the age of one and received treatment with concentrates on four occasions in 1983. The report from Dr Ludlam raised the following questions:
“As small children with this degree of severity of haemophilia only bleed infrequently treatment should ideally have been with cryoprecipitate. Although this is lightly [sic] harder to give than factor VIII concentrate it was still the treatment of choice, and used by many Centres. If it was not available, as Dr. John Martin maintains, then he should have been treated with NHS factor VIII concentrate.
To justify the use of commercial factor VIII concentrate for this child it will be necessary for Dr. Martin to demonstrate that despite requesting cryoprecipitate from the Regional Transfusion Centre they refused to provide it. He will also have to demonstrate that there was no way in which he could reserve NHS factor VIII concentrate for the treatment of patients who only bled occasionally. Although Dr. Martin maintains that treatment policy was directed by the Royal Liverpool Hospital this does not accord with the statement of Dr. McVerry. I think Dr. Martin has to justify his treatment policy as an independant [sic] clinician.” [1760]
A report from the solicitors representing the defendant health authority in the litigation recorded that “We are unable” to show that cryoprecipitate and NHS Factor 8 concentrate were not available and that Dr Martin “says that he gave no consideration to alternative treatment.”[1761] Dr Martin himself said that his treatment of the child was “consistent with the standard treatment being given to patients at the time.”[1762]
Other evidence confirms that: DDAVP was not in use until after 1988/89;[1763] there was no system of batch dedication to reduce donor exposure;[1764] and (by 1989) a “large proportion of the clinical notes of children affected by HIV were on close inspection missing essential treatment and decision-making details.”[1765]
The precise number of children infected with HIV as a consequence of their treatment at Alder Hey is unclear: data from UKHCDO suggests that 13 were infected; a July 1987 report recorded 16 cases; Dr Ball recollected approximately 12 boys who were HIV positive.[1766] Dr Ball’s recollection too was that, as a proportion of children registered per centre in the UK, “this was one of the highest (if not the highest) proportion of HIV positive haemophiliacs.”[1767] To put those figures into their (horrifying) context, the 1983 return showed 16 patients with Haemophilia A treated that year; the 1984 return showed 14 patients.
Birmingham Children’s Hospital (“BCH”) was the largest centre for children in the UK: as at 1974 it had 120 patients registered.[1768] Children transferred to the QEH between the ages of 16 and 18.[1769] Dr Frank Hill succeeded Dr Mann as centre director in 1976.[1770]
In a statement Professor Hill made to the Inquiry he stated that in the late 1970s non-A non-B Hepatitis was thought to be a minor, self-limiting condition with no serious long-term consequences.[1771] If that was Professor Hill’s genuine understanding at the time, it was wrong, for reasons explored elsewhere in this Report.[1772] Whether it was in fact Professor Hill’s view may be debatable, given that in November 1976, at a meeting of the West Midlands Working Party on the Treatment of Haemophiliacs, he raised the hepatitis risk in respect of freeze-dried Factor 8 concentrates and asked whether it might be advantageous to reserve the NHS concentrate for children, leaving the concentrate “obtained from commercial sources, largely of foreign origin” for adults.[1773]
The annual returns for BCH reveal an increasing move away from cryoprecipitate and increasing reliance upon commercial concentrate. As at 1977 BCH treated its Haemophilia A patients predominantly with cryoprecipitate together with some commercial concentrate. No NHS Factor 8 was used that year.[1774] This was a change from 1976, in which no commercial concentrate had been used and treatment was predominantly with cryoprecipitate, with a small amount of NHS concentrate.[1775]
By the following year, 1978, Factor 8 concentrate outstripped cryoprecipitate, with more commercial concentrate being used than NHS. The use of cryoprecipitate had reduced substantially from the previous year.[1776]
By May 1979 BCH had 17 patients on home treatment (with a further 5 being trained), of whom 8 received NHS product and 9 received commercial product.[1777] Commercial concentrate usage in 1979 was almost double that of 1978.[1778] Factorate usage then more than doubled in 1980[1779] and remained the mainstay of treatment in 1981[1780] and 1982, with the latter year seeing a substantial fall in the use of cryoprecipitate.[1781]
In 1983, when the risks of AIDS should have led to a different and more cautious approach, Factorate usage increased again and there was no indication of any increased use of cryoprecipitate.[1782] And whilst 1984 saw a very modest increase in the amount of cryoprecipitate used, and an increase in NHS concentrate, the amount of Factorate used rose yet again to 1,669,266 units.[1783]
The numbers of patients treated over this period varied, but did not significantly differ from year to year.[1784]
It is right to note that at a meeting of the West Midlands Working Party on the Treatment of Haemophiliacs in November 1981 Dr Hill “raised the problem of the large amount of Commercial Factor VIII used at the Children’s Hospital, compared with NHS Factor VIII ... He referred to the high cost that this incurred for the Central Birmingham District and asked if NHS Factor VIII could be distributed on a more even basis.” The Working Party agreed to recommend to Dr Ala, the regional transfusion director, that NHS concentrate should be distributed in proportion to the number of patients treated.[1785] It does not appear that the idea of prioritising NHS concentrate for the treatment of children was pursued. At the June 1982 Working Party meeting, and in response to an anticipated temporary (six-month) reduction in the production of concentrate at BPL, Dr Ala recommended that all centres should endeavour to cut down on the use of Factor 8 and increase the use of cryoprecipitate. The Working Party however agreed that “any shortfall would have to be met by increased purchasing of Commercial Factor VIII.”[1786] The annual returns for 1982 suggest that Dr Hill did not increase the use of cryoprecipitate at this time.
In his 1992 statement, Dr Hill claimed to have become aware of the possibility of AIDS being a condition encountered in people with haemophilia in early 1983, adding that he “had no knowledge of whether the condition was associated with a virus infection or could be associated with imported Factor VIII concentrates.” It was, he said, “not thought that there was any call for any treatment alteration because of the association between haemophilia and AIDS based on information available in 1983 and to withhold treatment of acute haemorrhages was considered more dangerous.”[1787] This statement calls out for comment in a number of respects. First, Dr Hill was one of the attendees at the Heathrow hotel meeting in January 1983 and can have been under no illusions as to the nature and severity of the risk of AIDS transmission: to suggest that the information available in January 1983 merely conveyed the “possibility” of AIDS being a condition encountered in people with haemophilia is to misrepresent or misunderstand the position significantly.[1788] Second, in June 1983 he was sent a letter from Treloar’s informing him that one of his patients was exhibiting AIDS stigmata.[1789] It is unclear whether he took any action in response but again that should have been a matter of acute concern. Third, Dr Hill would have received the 24 June 1983 letter from Professor Bloom and Dr Rizza, following the special meeting of reference centre directors in May 1983. That should have alerted Dr Hill to the importance of avoiding treating children with commercial concentrates. Yet there is no evidence to suggest any significant change in treatment practice at BCH in response to the risks of AIDS before December 1984.
Nor is there any evidence to suggest that a batch dedication policy was in operation – indeed there is evidence to the contrary. A 1992 medical report (from Dr Savidge) was scathing about Dr Hill/BCH’s approach to treatment:
“It would seem that Armour was the sole supplier of commercial factor VIII to Birmingham Children’s Hospital at that time, and Dr. Hill was purchasing large amounts (0.25-0.5 million units) of low unitage (200 units) vials at any one time. However, instead of allocating an individual small group of patients on any one batch to ensure long-term continuity of management of such cases on the same batch, it would seem that, with a few exceptions, the vast majority of Dr. Hill’s patients received the same batch over a few months until the batch was used up. This rather bizarre approach to patient management resulted in the child receiving a relatively large number of batches of vials of material containing few units in a remarkably short time.”[1790]
The child referred to in the report was given commercial concentrate as a baby and Dr Savidge observed that “As cryoprecipitate treatment of infants was the recommended policy of the hospital and indeed nationally, the administration of this large donor pool commercial material in preference of cryoprecipitate or NHS concentrate without authorisation was negligent.”[1791] The report detailed multiple treatments with commercial concentrates over the course of the period from 1981-1984. In relation to 1983-1984, the report continued:
“During 1983 and into early 1984, Armour concentrate was used exclusively although there is no satisfactory documentation to indicate that the boy had developed allergic reactions to cryoprecipitate uncontrolled by antihistamines, had shown any signs suggestive of reduced efficiency of cryoprecipitate or was established on a home treatment programme. This policy was pursued, with no reference to the availability of NHS concentrate at the hospital in the face of growing concern and increasing information in the public and medical press that AIDS was transmitted by blood products.”[1792]
Further:
“Although it would seem that Dr. Hill, as a number of haemophilia treaters in the U.K. at this time, believed that continued use of the same batch confined the risk of infectivity, this was clearly not practised in the case of this child. This is evident from the fact that between 1981-mid 1984, 20 different batches of Armour factor VIII were used, and during the relevant period (1981-1982) when infection with HTLV III most probably occurred, some 7 different batches comprising the total unitage of 5516 units of Armour factor VIII were administered. This very small unitage, however, carried a very high potential for possible infection as the material from all these batches was probably derived from at least 70,000 paid U.S. blood donors. From this aspect, cryoprecipitate and to some extent NHS concentrate if used consistently would have imparted a far lower infectious risk, particularly as the Armour material originated in the U.S. where paid blood donations were the commercial companies plasma source, and where AIDS was believed to have originated and had already started to become manifest as a clinical entity in U.S. haemophilia patients.”[1793]
There is no reason to think that Dr Hill’s/BCH’s treatment of this individual child differed materially from the approach to the treatment of children at BCH more generally.[1794] On the contrary, it is consistent with both the annual returns and the evidence which the Inquiry has received from those treated at BCH and their families. Dr Hill, in a statement produced for the purposes of litigation in 1992, made clear that cryoprecipitate was not favoured at BCH for use in home treatment,[1795] and was therefore used only for treatment on demand in the Centre. The introduction of the home treatment programme in 1976 required, he said, increased amounts of factor concentrate and commercial concentrates “were more available than NHS concentrates.”[1796] Children were considered for home therapy at about three years of age, but it was not uncommon for it to be earlier.[1797] It is thus clear that children including infants as young as or younger than three years old would be treated at BCH with commercial concentrates.
The evidence of Andrew Evans, who, having been initially treated with cryoprecipitate and NHS concentrates, was then treated with US concentrates, casts light on Dr Hill’s attitude towards the risks of AIDS. In early 1983 the New Scientist published an article which referred to the possibility of AIDS being spread through Factor 8 concentrates.[1798] It was read by Andrew’s parents. This led to a meeting at BCH during which his mother asked Dr Hill outright whether there was a chance that her son and the sons of the other parents present would get AIDS from Factor 8 and Dr Hill’s reply was “Madam, your son has more chance of becoming debilitated with arthritis through not taking Factor VIII than he has of getting AIDS.”[1799]
He developed AIDS.
It was not until after the Elstree meeting on 10 December, when the West Midlands Working Party held an extraordinary meeting on 17 December 1984 to discuss the implications of the deaths of two people with haemophilia from AIDS, that there was any significant change of approach and an interim treatment policy was agreed, whereby mildly affected patients with Haemophilia A and von Willebrand disorder should be treated with DDAVP or cryoprecipitate, newly diagnosed patients with severe haemophilia should be treated wholly with cryoprecipitate; patients with no previous exposure to commercial Factor 8 should continue on NHS Factor 8; and patients with previous exposure to commercial Factor 8 should continue on NHS product if available and heat-treated commercial product if not.[1800]
The commercial heat-treated Factor 8 product used at BCH in 1985 and 1986 was Armour’s product.[1801] It may or may not have been a coincidence that Armour made regular financial contributions to Dr Hill’s “research fund” as can be seen from a letter from Robert Christie of Armour to Dr Hill in March 1985.[1802] In April 1985 Robert Christie visited Dr Hill, to discuss a number of recent possible Hepatitis B cases and also to discuss Dr Hill’s “research on AIDS and Haemophiliacs”. The note made by Robert Christie recorded that Dr Hill continued to screen children for HTLV-3 antibodies, that just over 50% were positive and that “Dr Hill suspects that all children who have had a long exposure to concentrate may well be infected!”[1803]
In a report prepared by Dr Franklin and Dr Hill in April 1986, it was reported that 60% of the patients at BCH were positive for HIV.[1804]
In September 1986 Dr Hill reported to Armour that two children had seroconverted to HIV following their use of Armour heat-treated Factorate.[1805] In late October 1986 Dr Hill reported to Armour that a third child had seroconverted.[1806]
The director of the Royal Manchester Children’s Hospital (“RMCH”) in the 1970s and 1980s was Dr David Evans. The Centre treated children up to the age of 16 or 17 years.[1807] In 1977 Dr Evans was sufficiently concerned about the transmissibility of hepatitis to write to Professor Blackburn (then chair of UKHCDO) wanting to know what different laboratories were doing “about the potential hepatitis risk with haemophiliacs.”[1808]
The annual returns between 1976 and 1982 show a clear move away from cryoprecipitate towards commercial concentrates for the treatment of children with Haemophilia A.[1809] Thus in 1976 the annual returns show the use of 270,970 units of cryoprecipitate, 32,973 units of commercial concentrates and 3,535 units of NHS Factor 8.[1810] Over the following years the balance shifted, such that by 1979 for the first time more units of concentrates (predominantly commercial) were used than cryoprecipitate;[1811] in 1980 significantly more units of concentrates (predominantly commercial) were used than cryoprecipitate;[1812] in 1981 and 1982 Haemophilia A patients were primarily treated with commercial concentrate (and no NHS concentrate was used at all).[1813]
Cryoprecipitate tended to be used for hospital treatment and concentrates for home treatment, at least as at September 1982[1814] when Dr Evans wrote “We normally give the young patients with haemophilia treatment with Cryoprecipitate rather than Factor VIII concentrates. In the past we found several developed jaundice when they were given Factor VIII concentrates and I think the incidence of hepatitis is much lower when we use North Western Cryoprecipitate than when we use the imported concentrates. We tend to keep the concentrates for use with patients who are on home treatment, and use Cryoprecipitate in hospital.”[1815] Viewed from the perspective of safety rather than convenience, the logical flaw with such an approach is that patients on home treatment were being exposed to the greater risk of hepatitis. Home treatment with an element of prophylaxis had been introduced in the early 1970s and families were advised that “Some children may be able to have an injection to provide cover for a day or so for an important examination, or to tide them over a period when bleeds are particularly troublesome.”[1816]
There was no policy of restricting patients to single manufacturers or batches of commercial concentrate.[1817]
The annual returns give no indication of any response to the developing knowledge of the seriousness of non-A non-B Hepatitis. There was no discernible change of approach in 1983 and 1984: at a time when the risks of AIDS should have been uppermost in any haemophilia clinician’s mind, the predominant treatment for the children at RMCH remained commercial concentrates, although NHS Factor 8 continued to be used as well.[1818] Dr Evans was a regular attender at UKHCDO meetings[1819] and attended the January 1983 Heathrow hotel meeting referred to earlier in this chapter. He was also the recipient of correspondence from Dr Aronstam at Treloar’s in July 1983 which would have alerted him to the fact that Treloar’s was undertaking “AIDS related tests” and looking for “the stigmata of AIDS”.[1820]
It is not clear when RMCH introduced heat-treated concentrates, but as at May 1985 it appears that the Centre had not provided BPL with a list of named patients to receive heated NHS Factor 8.[1821]
That Dr Evans did not make any significant adjustments to his approach to treatment in response to the risk of AIDS is apparent from an article he wrote in 1997: “It was apparent by 1983 that the risk of infection was greater with concentrates derived from large donor pools, and advice was given to change from large pool products to cryoprecipitate; but because AIDS was still rare, the cause was unknown, the benefits of home treatment with concentrate were substantial, and a change back to cryoprecipitate would have disrupted the arrangements for making freeze-dried concentrate in the UK, this advice was not followed.”[1822]
In 1987 the RMCH produced a leaflet containing information on HIV for patients and their families, which stated “Some years ago some of the freeze-dried concentrate, imported from America, were infected by the virus. At this time no-one was aware that this was so. It took time before it was known that AIDS was carried by a virus, and longer before it was known that it was present in blood and blood products ... The hospital staff had no idea at the time that their treatment carried this risk.”[1823] This was not a transparent or candid way in which to explain the position to patients. On the contrary, it was positively misleading. Certainly by (at the very latest) January 1983 Dr Evans did know of the risk of transmission from commercial concentrates.[1824]
UKHCDO data suggests that 16 patients were infected with HIV at RMCH.[1825]
In Belfast children with bleeding disorders were cared for at the Royal Belfast Hospital for Sick Children (“RBHSC”) until around the age of 14, when they transferred to the haemophilia centre at the Royal Victoria Hospital.[1826] Dr Stanley Dempsey was the consultant paediatric haematologist at the hospital from August 1980, taking over from Professor John Bridges.[1827] The cohort of patients under Dr Dempsey’s care in the 1980s all had either mild or moderate Haemophilia A; there were also some patients with von Willebrand disorder.
There were no separate annual returns for the RBHSC: the returns were amalgamated with the adult haemophilia centre at the Royal Victoria Hospital and sent to Oxford “as a unified whole.”[1828]
When Dr Dempsey took up his post in August 1980, cryoprecipitate was used “fairly exclusively”; this was the policy of his predecessor.[1829] Following a “difficulty” with a child admitted in 1981 following an accident where cryoprecipitate “failed to do the job that was asked of it on that occasion”, Dr Dempsey’s “confidence in cryoprecipitate” was shaken[1830] and he began to use commercial concentrates in its place for the moderately affected patients, although cryoprecipitate remained the product of choice for mildly affected Haemophilia A and von Willebrand disorder patients. The commercial concentrates used were those in the blood bank at the time (Hemofil and Armour), which were ordered by Dr Mayne.
Looking back Dr Dempsey said the best decision would have been to go onto NHS material.[1831]
From late 1981 to June 1983 children at the RBHSC with moderate haemophilia were treated with these commercial concentrates; children with mild haemophilia were treated with DDAVP and tranexamic acid.[1832]
Dr Dempsey recalled that the pharmaceutical firms were “keen to emphasise the fact that they’d tightened up on the type of donor they looked to for their plasma source” and this gave him “reassurance” such that he was “disposed to look favourably on commercial concentrates at that point in time.”[1833] Dr Dempsey said that he had to rely on the fact that these firms were telling the truth. He also got the impression from reading UKHCDO minutes that things had improved considerably in relation to the safety of commercial concentrates.[1834]
Dr Dempsey described batch dedication as “extremely difficult” and as something that ultimately did not work.[1835]
Notwithstanding the assurances from the pharmaceutical firms, Dr Dempsey was aware that there was still a risk of non-A non-B Hepatitis from commercial concentrates, but there was also a risk from NHS concentrates. He acknowledged that the risk with cryoprecipitate was “very much less.”[1836] He recalled that non-A non-B Hepatitis was not thought sufficiently serious to merit withdrawal of “the only really effective treatment for severe/moderate haemophilia.”[1837] Dr Dempsey suggested that “we” were “on a learning curve from 1980 on.” There was a “general feeling” amongst clinicians that it was not a major concern, but there were patients who did have evidence of chronic liver disease.[1838]
Following the circulation of the UKHCDO’s 24 June 1983 letter, Dr Dempsey switched from commercial to NHS concentrate (the SNBTS product). Had such advice been given earlier by UKHCDO, it is reasonable to assume that this switch would have taken place earlier.
In retrospect he would not have used concentrate at all “given what was likely – or what was going to happen further down the road”; looking back, the NHS product might have been a “better modality of treatment” to have employed back in 1981.[1839]
Dr Dempsey continued to use SNBTS concentrates until late 1984 when he became aware of the infection of patients in Edinburgh. The heat-treated Scottish product became available to him in late 1984 and he was using the heat-treated product NY until July 1987 when the next generation product Z8 became available. He was aware that non-A non-B Hepatitis could still be transmitted by NY.[1840] He was not aware, however, that BPL was producing a product at this time (8Y) which did not transmit hepatitis; had he known about it, he would have phoned BPL and requested a supply.[1841]
It is unclear whether any children treated at the RBHSC were infected with HIV in consequence of their treatment there, but Dr Dempsey’s understanding was that there were not.
All of his patients in the moderately affected category – who would have been treated with commercial concentrates and SNBTS concentrates – were infected with Hepatitis C.[1842]
The director of the centre at Great Ormond Street Hospital (“GOSH”) was Professor Roger Hardisty from around 1968 to 1987, when he was succeeded by Professor Ian Hann.
Professor Hardisty told a meeting at the DHSS in 1970 that at GOSH the emphasis was on early treatment of minor bleeds in children to prevent crippling; that more treatments were being given per patient; and that some 30% of 69 registered patients attended frequently or fairly often.[1843] GOSH was regarded as being in a unique situation as a supra-regional children’s hospital, with patients drawn from a number of different southern/eastern regions.[1844] By 1976 all patients on home treatment were receiving commercial Factor 8 concentrates, through a special allocation from the DHSS.[1845] In September 1977 GOSH was complaining of a shortfall of NHS concentrate and a need to purchase more commercial concentrates.[1846] In September 1978 it was recorded that a shortage of factor concentrates for home therapy was leading to patients being transferred to other centres at a much younger age.[1847]
The annual return for 1976 shows substantial use of both cryoprecipitate and commercial concentrates, with very little NHS concentrate.[1848] By the following year the amount of cryoprecipitate used had reduced considerably, with some rise in NHS Factor 8 but with treatment being predominantly with commercial concentrates.[1849] 1978 showed a similar pattern.[1850] In 1979 Factorate was the main treatment,[1851] as it was again in 1980,[1852] and in 1982, although the amount used in 1982 showed a substantial increase from 1980.[1853] Whilst 1983 saw an increased use of NHS Factor 8, there was little use of cryoprecipitate, although the volume of Factorate fell substantially compared to the previous year.[1854] The position in 1984 was different: NHS Factor 8 concentrate was the product in greatest use, with a significant reduction in the amount of commercial concentrate.[1855] In February 1985, writing to Dr Snape with the names of seven patients who had tested positive for HIV (and a number of others whose results were awaited), Professor Hardisty indicated that he would like to switch to the heated NHS products for all patients, irrespective of their antibody status, as soon as supplies permitted.[1856]
There is comparatively little contemporaneous evidence regarding Professor Hardisty’s approach to treatment, beyond what is revealed by the annual returns. He was, however, a regular attendee of UKHCDO meetings. He was also at the January 1983 meeting at the Heathrow hotel, at which he was recorded as pointing out (along with Dr Hill) the ethical difficulties of using newly diagnosed children as first candidates in a trial of hepatitis-free Factor 8.[1857] Unfortunately, GOSH was unable to locate any stored relevant documentation from the 1970s and 1980s (except individual patient records) to provide to the Inquiry, and there was no personal paperwork of Professor Hardisty’s from the time to be found in storage.[1858] It is therefore not possible to conclude whether the use of products in 1984 represented a conscious decision to use less commercial concentrate or not.
UKHCDO data suggests that 11 patients were infected with HIV at GOSH.[1859]
The haemophilia centre at the Royal Hospital for Sick Children (“RHSC”) in Yorkhill, Glasgow, provided haemophilia treatment to children from the Glasgow area and across the West of Scotland. As at 1980 there were 55 patients with Haemophilia A, 14 with Haemophilia B and 1 with von Willebrand disorder registered with the centre.[1860] Children transferred to the care of the Royal Infirmary in Glasgow at around the age of 15 or 16.[1861] The centre director was Dr Michael Willoughby who was involved in the treatment also of children with haematological and non-haematological cancers. Dr Anna Pettigrew took up a post as a part-time clinical assistant there in May 1980.[1862] Dr Willoughby left in 1983 and was replaced by Dr (later Professor) Ian Hann.
Dr Pettigrew’s recollection was that the policy in practice (under Dr Willoughby) was that newly diagnosed patients and those with mild haemophilia were treated with cryoprecipitate, and those on home therapy and frequently attending patients with severe haemophilia not on home therapy would be treated with concentrate or cryoprecipitate depending on the severity of the bleeding episode.[1863] She recalled the commercial product as being more “user friendly” in that it dissolved more quickly[1864] and each box contained the necessary supplies and even child-friendly medical plasters. Parents administering home therapy often, she said, expressed a preference for this.[1865] If they had known that commercial products came with a greater risk for their child, it seems inconceivable they would have persisted with such a preference. The fact that Dr Pettigrew was able to recollect this therefore comes with the inference that parents were not told of the risks of the treatment their children were having.
Home therapy and prophylactic therapy were introduced by Dr Willoughby for what Dr Pettigrew described as both psychosocial and clinical reasons.[1866] She recalls the rationale for prophylaxis being explained to her by Dr Willoughby – that a twice weekly regular dose of Factor 8 would provide sustained though low levels of Factor 8 which would be sufficient to prevent spontaneous bleeding episodes. The effect of prophylaxis, of course, is that patients receive significantly more by way of concentrate (and in Yorkhill’s case, that would mean commercial concentrate) than they would if they were simply being treated as and when required. The risk of being infected with a virus was, therefore, all the greater.
There was no system of batch dedication.[1867]
The annual returns reveal the extent of Dr Willoughby’s use of commercial concentrate:[1868]
When Dr Hann arrived, he described a parlous state of affairs at the RHSC.[1875] He stopped the purchase of commercial Factor 8 and adopted a policy of using SNBTS concentrate and cryoprecipitate and DDAVP (and then only heat-treated concentrate).[1876]
Dr Willoughby did not attend UKHCDO meetings.[1877] He preferred commercial concentrate because (according to Dr Hann) of its purity and to a limited extent its availability. Dr Willoughby’s account to the Penrose Inquiry was that “We wanted to make things as easy as possible for the parents. So, for home therapy, we used a commercial source of Factor VIII ... It was much easier to reconstitute with its diluent.” He claimed that “We had no idea that we were exposing these patients to serious viral diseases”, believing “that problem only started coming to light in around 1983, after I had left the UK.”[1878]
Dr Willoughby’s statement made no reference to availability, although Dr Pettigrew’s impression was that reliability of supply was a factor in his thinking, noting that the commercial concentrates tended to be used for patients on home therapy and NHS for patients who were not.[1879]
As to availability, Professor Hann’s evidence was that within days or a few weeks of taking up his post he contacted the Blood Transfusion Service and asked “what the score was, why are we using all this commercial concentrate” and he was told “If anything, we will give you priority. I can’t guarantee you absolute full supply but I think we can do”. And within days or weeks at most, Dr Hann stopped all use of Factor 8 concentrates from abroad.[1880] He knew that the type of donors used in the US were “very high risk in this context” and “could not contemplate continuing the use of commercial concentrate.”[1881] Dr Hann also adopted a more conservative approach to the use of concentrates; after discussion with families, terminated prophylaxis in some patients; and encouraged the use of DDAVP.[1882]
The reality is that if Dr Hann could make those changes in 1983, Dr Willoughby could have made them in the preceding years.
It was Dr Pettigrew’s view that “All clinical staff involved, such as Dr Willoughby who instituted home therapy with Factor VIII concentrate, acted in what was thought to be in the best interests of their patients.”[1883] Insofar as Dr Willoughby was concerned, I disagree. No steps were taken whilst Dr Willoughby was director to reduce or minimise the risk of patients being infected with a virus.[1884] He did not act in the best interests of his patients, nor can he have legitimately concluded that his treatment policy was in their best interests. It cannot possibly have been in the best interests of the children treated at Yorkhill to receive commercial concentrates, and to be treated on a prophylactic basis with such concentrates, in circumstances where commercial concentrates carried a higher risk of transmitting viral infection and cryoprecipitate and/or SNBTS concentrates could (and should) have been used.[1885] Contrary to the view that prevailed at the Yorkhill,[1886] cryoprecipitate, although certainly less convenient for use, was not impracticable for home treatment.
It makes little sense for Dr Willoughby to have committed Yorkhill to the purchase of commercial concentrates when throughout the period of interest Scotland was effectively self-sufficient in NHS factor concentrates: it is ensuring safety, not saving cost, which is and should be the governing principle. It could be anticipated at the time that his policies would be harmful. In retrospect it can be seen they were.[1887]
Dr Pettigrew described Dr Willoughby as a practitioner who acted autonomously (in contrast with his successors, Dr Hann and then Dr Gibson, who communicated more with the Royal Infirmary).[1888] It follows that responsibility for the policies which he adopted was his.
Twenty-one children with haemophilia were infected with HIV at the RHSC: nineteen with severe haemophilia and two with moderate haemophilia.[1889] Though much focus on HIV infection in Scotland has understandably been on “the Edinburgh cohort”, the numbers of those infected in consequence of the unsafe prescribing practices adopted at Yorkhill were greater, and the proportion of patients affected greater still.
Although there were two distinct hospitals in Bristol – the Bristol Royal Infirmary and the Bristol Children’s Hospital – they were physically very close to each other and were sometimes referred to collectively as the Bristol Centre[1890] (or the Children’s Hospital was described as an associate centre), and the annual returns covered both hospitals. Dr Scott was the director at the Royal Infirmary from 1976; at the Children’s Hospital Dr David Burman was in post from 1978. Both were invited to UKHCDO meetings although in practice it appears that one or the other would usually attend rather than both. Dr Scott said that it was always his policy to use NHS products in preference to commercial products, because of the risks of infection, but that commercial blood products had to be purchased to make up the deficit as there was not sufficient NHS product to cover their needs. He also suggested that priority for NHS products was given to children and to adults who had previously received little treatment.[1891]
In 1979 Dr Scott complained to Dr Tovey of the regional transfusion centre about the insolubility of the BPL product, stating that “I cannot use this material for home treatment any longer and this will mean a considerable increase in the amount of commercial Factor VIII which has to be purchased.”[1892]
Dr Burman instituted home therapy for children with severe haemophilia from the age of about four. Cryoprecipitate was not used, it being considered, according to Dr Helena Daly, as impractical for home therapy. DDAVP was not used until 1983.[1893]
Lee Turton was treated at the Bristol Children’s Hospital with Factor 8 concentrates in early 1982 when he was still a baby. His medical records contained an entry to the effect that the treatment was “swapped” from cryoprecipitate to Factor 8 in 1982 “because cryo not available.”[1894] Given the ease with which cryoprecipitate could be produced, that was not a proper reason for treating a baby with concentrates.
Dr Scott wrote to a patient and his wife in October 1983 as follows:
“As I am sure you know one of the patients attending the Bristol Haemophilia Centre has recently died of AIDS. The cause of this condition is still unknown but there is evidence to suggest that it is due to an infection which can be transmitted by blood or blood products. There is reason to believe that the source of the infection in this case was imported Factor VIII concentrates but this is not proven and it cannot be said with certainty that these were the source of infection. I can understand that you are extremely worried that you have contracted a similar condition by using imported blood products. However, I would like to make it clear that the risk of this is extremely small. Thousands of Haemophiliacs in Europe and America have been treated with Factor VIII concentrates for over ten years and the number of reports of AIDS have been extremely small. As far as possible we are avoiding the use of imported Factor VIII concentrates but there is not enough NHS produced Factor VIII available at the moment to meet our needs so we will have to continue to use some commercial Factor VIII for the time being. The production of NHS concentrate is being increased and hopefully we shall be self-sufficient in the not too distant future. In the meantime I think that the dangers of refusing treatment if only commercial concentrate is available is greater than the danger of contracting AIDS.”
Dr Scott expressed the hope that this “allays your fears”.[1895] When Lee Turton’s parents, Colin and Denise, became aware of news reports about AIDS and the possibility of it affecting the haemophilia community, they asked Dr Burman if there were any risks to Lee. He told them “that Lee was only having British Factor VIII so there was no risk.”[1896]
UKHCDO data suggests that 3 patients were infected with HIV at the children’s hospital.[1897]
During the 1970s to 1990s the Sheffield Children’s Hospital (“SCH”) acted as the paediatric wing of the haemophilia reference centre for patients in the North Trent region, providing care to those aged 16 and under.[1898] Prior to 1975 the responsibility for treatment of paediatric patients with bleeding disorders was primarily that of Professor Blackburn; from 1975 to 1995 Dr John Lilleyman was the consultant haematologist at the SCH with responsibility for their treatment.
There were close links between the adult and paediatric treatment and the clinicians would meet at least weekly for journal reviews and discussion of clinical problems. There was also a close relationship with the regional blood transfusion centre; the regional transfusion director used to hold a formal clinical session with Dr Lilleyman weekly and “was a useful contact for the supply of blood products, in particular cryoprecipitate.”[1899]
In contrast to the paediatric centres described above, Dr Lilleyman would reiterate frequently that:
“for children who were small and required less Factor VIII per dose than adults, cryoprecipitate had many advantages and for most admissions for joint bleeds, bumps and scrapes, heavy bruises and minor surgery, was to be preferred since it only exposed patients to a very small number of UK donors and reduced the risk of viral transmission that was becoming a recognised problem with large pool fractionation processing.”[1900]
DDAVP and tranexamic acid were also used. Cryoprecipitate remained the treatment of choice at the SCH for all but the most serious bleeds or surgery “particularly after the problems of viral transmission of NonA NonB hepatitis started to appear.”[1901]
The annual returns show that for the period 1976 to 1981 cryoprecipitate remained in significant use at the hospital, although concentrates (both NHS and commercial – but with increasing use of NHS over commercial) were also used.[1902] However commercial concentrate ceased to be used to any significant extent after 1981 for the treatment of patients with Haemophilia A. The 1982 return recorded the use of both cryoprecipitate and NHS concentrates, but no commercial.[1903] The return for 1983 recorded the use mainly of cryoprecipitate and NHS Factor 8, with a small amount of Factorate.[1904] In 1984 and 1985 no commercial concentrates were used: cryoprecipitate and NHS concentrates were the main treatments provided.[1905]
The particular approach to treatment at SCH reflected the earlier (compared to many other centres and clinicians) realisation there of the potential seriousness of non-A non- B Hepatitis, with a study that was published in 1980[1906] reinforcing the view at SCH that cryoprecipitate was a safer product than concentrate.[1907]
Dr Lilleyman recalled becoming aware of the association between AIDS and blood products around the time the matter was raised at the UKHCDO meeting in September 1982.
Dr Lilleyman’s recollection was that no children at SCH were infected with HIV. Whilst that is consistent with the data received from UKHCDO,[1908] the evidence available to the Inquiry demonstrates that one child was in fact infected with HIV.[1909]
The comparison between large children’s hospitals, one on one side of the Pennines (Alder Hey) and one on the other (Sheffield), is telling.
It is easy to look in hindsight at the facts that:
However, the reason for the difference was not a matter of hindsight. It was the opposite. It was foresight. Dr Lilleyman expressly sought to use cryoprecipitate because he foresaw that using products made from the plasma of much larger numbers of donors who were from foreign countries would create more risk of infection. He deliberately chose to use as little concentrate as possible, favouring NHS concentrate where he could.
This shows that to focus on patient safety was not to ask too much of clinicians because of the benefits of hindsight. It shows that those who operated the paediatric regimes described above (and in particular at Alder Hey, Birmingham, Yorkhill, and Treloar’s, given the scale, in terms of numbers and proportions of those infected who were there) did so without sufficient regard for the dangers to their patients of what they were doing. They had all the information they needed to do better. They did not use it.
In consequence, children suffered. They did not need to do so.
Not all children with bleeding disorders were treated at paediatric haemophilia centres. Some received their treatment through the centres that provided treatment to both adults and children. All too often they were treated as if they were adults, with devastating consequences.
Consideration of some individual cases will serve to illustrate this wider point.
Christopher Fowle was treated at the haemophilia centre at Harrogate General Hospital, initially with cryoprecipitate, from the age of two. Shortly after he started school he began to be treated with Factor 8 concentrates: both NHS and commercial concentrates (Factorate).[1912] His parents were pleased with this change, believing that it would be less painful and more convenient. As his mother, Christine, told the Inquiry “The doctors never said anything negative about the FVIII products and it did not cross my mind to question the hospital’s professional judgment [sic] as to whether or not the products were safe to use. I did not think doctors would use products on Christopher that were unsafe.”[1913]When news media started to report about AIDS and blood, she asked the consultant about the safety of the products “and he assured me that I didn’t have to be [concerned] because it was generally in the homosexual community.”[1914] This was false reassurance. When Christopher was about nine years old, his parents were told that he had been infected with HIV.[1915]
They decided to try to do everything they could to make his years happy ones, having been told that he might expect to live another 12 years or so.[1916] When Christopher was 15 years old, they told him of his diagnosis. He was angry as he got older, lost any sense of purpose, began not to care what was happening around him.[1917] In the last 18 months or so of his life, “he started to go down, started to lose weight ... and he just got worse”.[1918] He developed “ulcers, horrible ulcers, infected ulcers in his legs, and a lot of pain, a lot of pain.” Then he went blind: “that was the last thing I remember really of him not being able to see.”[1919]
Christopher died the day after his 22nd birthday. His parents “have been denied seeing him get married, have children, travel and most of all sharing our lives with him as we get older. We do not think time will heal our pain because we forever think about what might have been.”[1920]
Martin White was treated at Cardiff Haemophilia Centre. In 1978 and 1979 (then aged eight or nine years old) he was treated with commercial concentrates; from 1980 to 1985 he received NHS Factor 8.[1921] His parents were never informed of the risk of infection with hepatitis or HIV.[1922] Although he received cryoprecipitate in 1981, thereafter he was treated solely with concentrates, notwithstanding the increasing risk of AIDS. In March 1983, writing to the GP, Professor Bloom recorded that four days previously Martin had “had a routine dose of Factor VIII concentrate as part of his normal twice weekly prophylaxis”.[1923] “Normal twice weekly prophylaxis” means that Martin was being given Factor 8 not in response to a serious bleed, but to protect him against the possibility he might have one. It was to give him, therefore, more than was needed, and put him more at risk because of this. Martin had become unwell and was seen in Professor Bloom’s clinic, with “rather a worrying blood picture” which suggested “a virus infection or possibly some form of serum sickness as a result of the Factor VIII treatment.” At the present time, however, “there is certainly no evidence that he has developed the acquired immune deficiency syndrome recently reported in Haemophilia in the United States.”[1924] This information, revealing clearly Professor Bloom’s understanding that concentrates could cause AIDS, was shared with the GP, not with Martin’s parents.
Martin’s mother, Valerie, told the Inquiry that there was nothing in his medical records “to say that he was being tested, when he was being tested, when he was diagnosed, or when we were informed of his infections. It seems as though one minute he was normal and the next minute his notes report that he was HIV positive. When I applied for them, I had hoped that Martin’s records would clarify what had happened to Martin for me, but to my disappointment, they did not.”[1925]
Martin’s life “changed forever the day he was diagnosed with HIV”.[1926] His family’s life too was shattered.[1927] Martin died in June 2003.
Colin Smith was born in 1982. He was treated with Factor 8 concentrate in July 1983, when he was less than 1 year old.[1928] An entry in his medical records for 21 July 1983 noted that Colin had fallen back and hit the back of his head that day; it recorded that he was a “Known Haemophiliac – Not Treated” and “Never given VIII conc or cryo”.[1929] A letter from Professor Bloom to the GP, following a clinic on 28 July 1983, recorded that:
“I saw Colin in the clinic again this week. I understand that he turned up at the paediatric ward about a week ago having falling [sic] down and hit the back of his head. He received an intravenous injection of one bottle of 250 units of Factor VIII concentrate and made an uneventful recovery without any evidence of intracranial bleeding. The concentrate which we used was prepared from British blood from the Lister Institute. However, all these materials carry the risk of hepatitis, particularly non-A, non-B, but this is something that haemophiliacs have to accept.”[1930]
He added that Dr Hewlett (consultant haematologist at the Royal Gwent Hospital) and he “will keep a close observation on him as the months go by.”[1931] Thus, a child who was no more than a baby was treated with factor concentrates, in the express knowledge that this carried the risk of transmitting non-A non-B Hepatitis – but also, given that this was July 1983, in the knowledge that this carried the risk of transmitting AIDS.[1932]
Colin’s parents were not told, whether by Professor Bloom or by any other treating clinician, that there was a risk of him developing non-A non-B Hepatitis.[1933] Nor was any information provided to them about possible risks of AIDS, or indeed any risks associated with the use of Factor 8 concentrates.[1934] Although Colin’s treatment in July had been with NHS Factor 8, in August and September 1983 he was treated with a commercial concentrate (Kryobulin) and in June 1984 with a different commercial concentrate (Armour).[1935] There was no discussion with his parents about the use of commercial concentrates; as far as they were aware “it was all the same product.”[1936]
When Colin was about 2 or 2 ½ years old, in hospital with a bad chest, Professor Bloom told his parents, in a hospital corridor, that he was HIV positive.[1937] They were unaware that he had been tested.
Colin died in January 1990, just seven years old. His mother, Janet, told the Inquiry that “the devastation of having your child on your lap watching the rise and fall of his chest and waiting for it to stop is absolutely heart-breaking.”[1938] His father, Colin, said “There’s no way a child should have to die the way he did. It wasn’t pleasant. It still affects us now ... I could cope with death but not with the death of my son. I still have trouble today with the fact that he’s in a grave on his own, and the guilt will never go away.”[1939]
Lee Harding was born in 1978 and treated at the Cambridge Haemophilia Centre. From around 1979 to 1983 he was treated with cryoprecipitate in hospital. In 1983, aged five, he began home treatment, initially with cryoprecipitate and then with Factor 8 concentrates.[1940] “In all of the time prior to Lee being diagnosed with HIV” his mother, Patricia, “was never told about the risks of the treatment.”[1941] She discovered that Lee was HIV positive when she received a letter from Dr Seaman[1942] to that effect. When she went to speak to Dr Seaman, she was told that “there was more chance that Lee could get run over by a bus than developing anything from his HIV infection.”[1943]
Lee died in 1988. He was ten years old. In the last months of his life his illness became worse and worse: “He was like a skeleton and he was getting more and more rashes and lumps on his body.”[1944]
Steven Walker was treated with cryoprecipitate for the first 3-4 years of his life, but in December 1983 his family moved to Norfolk and responsibility for his treatment transferred to the Norfolk and Norwich Hospital. He was first given Factor 8 concentrates during 1984,[1945] when he was about four years old, and his mother, Gwynneth, was encouraged to try home treatment:
“I was provided with a sharps disposal box and understood the need to ensure sharps were disposed of safely but I cannot recall any information being shared, explaining that the medication could contain infections that might harm my little boy or that from receiving treatment, he could infect me or my younger child ... At no point was I given any information or advice regarding the risks of infection from the use of Factor VIII to Steven”.[1946]
In 1984/1985 Gwynneth was informed, by a nurse in a corridor at the hospital, that her son had tested positive for HTLV-3 but that it could be “a good thing” to have developed antibodies; the diagnosis was formally communicated by the GP in December 1985.[1947] Steven had also tested positive for Hepatitis B in 1985, which was transmitted to his mother. She had never heard of hepatitis prior to that, and the potential for infection had never been discussed.[1948] Steven’s health deteriorated over the years. Feelings of despair and hopelessness affected his compliance with treatment. He “struggled on quietly ... he didn’t want his own misery and hopelessness to sadden the rest of us”.[1949]He experienced constant pain and his existence was “a daily struggle.”[1950] In 2017, aged 37, Steven (“gentle, intelligent, generous of heart and witty”) died of a heart attack.[1951]
Rosemary Calder’s son, Nicholas, was treated at Northwick Park Hospital. He was initially treated with cryoprecipitate but from 1977 onwards – when Nicholas was not yet three years old – he began to be treated with Factor 8 concentrate.[1952] Rosemary “was advised by the hospital that the use of Factor VIII would be a great improvement in his care allowing us to eventually go on to home treatment.” She was “never asked if I was agreeable to the change and I was never informed that there was a risk of viruses being carried in the blood product.”[1953] Although Nicholas was treated mostly with NHS concentrate, there were occasions when he received commercial products: Factorate in 1978 and 1982.[1954] By the time Nicholas was nine, in 1983, he was being treated prophylactically, with three injections per week.[1955] In early 1983, prophylactic treatment should have been known to increase the risks (of both hepatitis and AIDS). There would be no improvement in safety by doing so.
When Rosemary, having heard about AIDS in the news, sought advice from Dr Cecil Reid, the centre director, and from the Haemophilia Society, she was “told to carry on his home treatment as normal as the risk of him contracting an infection was minimal.” Rosemary was never given the option of a reversion to cryoprecipitate.[1956] Nicholas was infected with HIV from this treatment – a diagnosis that was communicated by letter, following a test undertaken without her knowledge and consent, when he was 11 years old.[1957] In the 1990s he developed AIDS and his condition deteriorated over a period of years. Nicholas died in 1999, aged 25.[1958]
Stephen Finney was first treated with Factor 8 concentrates in January 1974 at Oxford Haemophilia Centre. They were commercial concentrates: Hemofil. He was just two and a half years old at the time. Entries on the National Haemophilia Database record that this treatment related to “Dr Craske’s research work”.[1959] He contracted Hepatitis B as a result.[1960] In 1978-79 he was treated with Oxford Factor 8 (NHS). From 1979 he received his treatment at Bournemouth: sometimes with NHS concentrate from BPL, sometimes with commercial concentrates (Hemofil and Kryobulin; in 1985 he received Factorate).[1961]
Stephen’s parents were not given adequate information about the risk of exposure to infections to enable them to make a sufficiently informed decision: “The only information we received from official medical sources was about how to best manage my Haemophilia condition and that now this new FVIII treatment was becoming available, I should be able to lead a relatively normal life. It was never about the clear or present dangers of potentially deadly viral pathogens associated with FVIII.”[1962] At the age of 14 he was told that he had been infected with HIV; five years later, he learned he had also been infected with Hepatitis C.[1963]
Stephen’s written statement to the Inquiry explains the enduring physical, mental and social impacts of being infected with Hepatitis B, Hepatitis C and HIV in the 1970s and early 1980s.[1964] As part of this, he describes spending a total of 28 weeks in four different hospitals in 2002. He lives with untreated post traumatic stress disorder. He told the Inquiry:
“Suicidal thoughts have crossed my mind but I have never considered going through with it. I believe if I had, then those who I believe are/were responsible for what happened to me and others would have got away with what they have done ... It is very rare, even to this day, that a day has gone by when I have not thought about it but the thought of just basically becoming another digit on the ever-increasing mortality statistics of this tragedy keeps me from giving in to it.”
Robert Hodgkins was first treated with Factor 8 concentrates in 1973/74. This too involved treatment with Hemofil for “Dr Craske’s research work”. He was five years old and developed Hepatitis B as a result.[1965] Thereafter he was treated, at the Hammersmith Hospital and in Bournemouth, with a range of different concentrates – sometimes NHS, but often commercial (Hemofil, Koate, Factorate and Kryobulin).[1966] His parents “put full trust in the doctors and merely accepted the change” from cryoprecipitate to concentrate: “They were not told this carried any risk of infection.”[1967] He received treatment prophylactically from the mid to late 1970s to the early 1980s.[1968] Robert was about 15 years old when he was told that he was HIV positive. The dreadful toll taken on his physical and mental health, his education and his ability to work is detailed in his written statement to the Inquiry.[1969] He says: “I feel terribly let down by the health system. I cannot comprehend how this could be allowed.”
Another man with mild Haemophilia A (described as “only very mildly affected”[1970]) was treated with Factor 8 concentrates at a hospital on the Isle of Wight in 1983, when he was undergoing tooth extractions. He was not yet a teenager and had not previously received factor concentrates.[1971] A test in 1985 confirmed that he had been infected with HIV; he later learned that he had been infected with Hepatitis C as well.[1972] He told the Inquiry of his feelings of isolation and depression, and his lack of faith in the NHS: “I feel robbed of my life when I think of all the things I could have done and should be doing but I now cannot.”[1973]
At Leeds, a boy was treated with commercial Factor 8 concentrates from the age of six or seven: even in 1983, when the risk of AIDS should have been plain, he was given Factorate. No information or advice was provided beforehand regarding the risks of exposure to blood borne infection. Both he and his two brothers were infected with HIV and Hepatitis C. He describes the feeling of being told that he had been diagnosed“as being struck by lightning.”Because of those infections he decided never to have children or get married.[1974]
Stuart Mclean was about nine years old when he was treated in 1978 with Factor 8 concentrate in the mistaken belief that he had a bleeding disorder.[1975] This treatment took place after he had been referred to a consultant haematologist at West Kent General Hospital, Dr Nalinda Naik, who was “interested in defects in blood clotting.”[1976] She formed the view that he was suffering from von Willebrand disorder and wrote to the Oxford Haemophilia Centre to that effect.[1977] However, Dr Rizza wrote to her stating that he did not think too much significance could be attached to the level of Factor 8 coagulant activity; Dr Matthews (also from Oxford) informed her that the results were completely normal and there was no reason to suspect any coagulation abnormality.[1978] Notwithstanding these letters, Dr Naik wrote to Stuart’s GP in November 1977 reiterating her suspicion that he had von Willebrand disorder, even though “‘the King of Clotting’ does not support my hypothesis.”[1979]
The following year, Stuart fell and injured his knee. He was taken to West Kent General Hospital where he was treated by Dr Naik and received fresh frozen plasma, cryoprecipitate and Factor 8 concentrates. She described this as being given as “prophylactic treatment”for a “possible” haemorrhage.[1980]
The treatment administered to Stuart showed a cavalier disregard for safety. He did not have von Willebrand disorder in the first place, and thus did not require such treatment. Dr Naik had been told this, by the “King of Clotting” and apparently thought she knew better. Even if he had von Willebrand disorder he did not require such treatment – with three different types of treatment – for what was only a possible haemorrhage. Prophylactic treatment was plainly unsuitable for a bleed which might develop from a specific injury, in any event, and multiplied the risks of infection; and even if he did require treatment, DDAVP would have been available, and concentrates should never have been used. In consequence of that treatment, Stuart was infected with Hepatitis C – a diagnosis he received for the first time in 2013, 35 years after the (wholly unnecessary) treatment which infected him.[1981] He has – rightly – been very angry about the treatment he was given.[1982]
These examples discussed above reveal that, in general haemophilia centres, just as in the paediatric haemophilia centres:
It is apparent that in the general haemophilia centres there was no clear or consistent understanding of who was to be regarded as a child for treatment purposes. That will no doubt be surprising to those reading this Report. It might be thought that it is obvious that “child” encompasses those who are under 18. However, for the purposes of centres’ treatment policies, the position is much less clear-cut. Children were, in effect, treated like adults, often after the age of four or five (or in the case of Colin, above, at an even younger age).
The Inquiry has received many more statements, detailing the treatment of children in haemophilia centres, which raise similar issues and themes to the eleven individual cases discussed above.[1983] This evidence, taken together with the evidence relating to the way in which children were treated at paediatric haemophilia centres, point to a single, inescapable conclusion: that clinicians failed in their duty to ensure that children were treated in a way that prioritised their safety above other considerations. Rather than taking steps to ensure that children, new to treatment, were not exposed unnecessarily to the risks of viral transmission, children were in practice treated in a way that starkly exposed them to those risks. Many died as a consequence; those who survived have lived lives that have been dominated by pain, suffering and stigma.
There can be fewer worse condemnations of any healthcare system than describing how it failed children. This section of the chapter has looked at failures which condemned children to a shorter expectation of life, one of debilitating pain and thwarted ambitions, robbing them of the fun and joys of youth, limiting the happy social interactions of childhood and early adolescence, and replacing growing up with wasting away. It condemned their parents to watch as it happened. It saddled some with guilt, and many with the stigma of being associated with an HIV victim, adding to the injustice. It need not have happened, as the Alder Hey/Sheffield Children’s Hospital comparison shows. It ought not to have done.
This report has drawn attention to the multiple failures which have led, as if in a complex jigsaw, to the treatment disasters the Inquiry has been investigating. Many are both serious and disturbing. But in my view, the way in which children were made victims, when they should not have been, is the worst of them all.
Earlier parts of this chapter have looked at the treatments provided to people with bleeding disorders, treatments which led to infection with hepatitis and HIV. This part of the chapter looks at the information that was – or more usually was not – provided to people about the risks of treatment, about the undertaking of tests and about the results of those tests. It reveals a disturbing and sorry picture.
The evidence before the Inquiry[1984] overwhelmingly establishes that people were not properly advised of the risks of hepatitis or of AIDS. People with bleeding disorders had the right to know that factor concentrates (or other treatments made from blood) might infect them with a serious or fatal disease for which there was no treatment. Parents had the right to know that such treatments might infect their children with such a disease. In practice, either they were given no information at all about such risks, or they were falsely reassured that the treatments were safe.
Some examples will serve to illustrate the position.
Michael Saunders, whose son Andrew was infected with HIV and Hepatitis C following treatment with commercial concentrates at Birmingham Children’s Hospital, was given no information about the potential risks associated with Factor 8 concentrates.[1985]
Paul, as a young man with mild Haemophilia B, underwent an operation in 1984 to remove a birthmark, following which he received treatment with Factor 9 concentrate which infected him with Hepatitis C. At no stage was any cautionary information given: rather he was allowed to undergo an elective, non-vital procedure at a time when it was known that factor replacement therapy was potentially both HIV and Hepatitis C infectious.[1986] He only learned that he had Hepatitis C in 1999.
The mother of a boy whose treatment changed from cryoprecipitate to Factor 8 concentrate in around 1983 was given no warnings about the products at Charing Cross Hospital where her sons were treated but “was just told it was an amazing thing”.[1987] Both her sons were infected with HIV.
Sean Nevin, who has mild haemophilia and was given concentrate as part of training sessions in 1982 at the Royal Liverpool Hospital as a child, explained that his family was “told Factor VIII was safer, less bulky, easier to store and easier to use than Cryoprecipitate.”[1988] Whilst ease of storage and use was correct, it was plainly incorrect to say that Factor 8 concentrates were safer than cryoprecipitate.
Paul, whose care was reviewed at Oxford, was switched from cryoprecipitate to concentrates in 1976: Dr Rizza wrote to his referring haemophilia clinician in Nottingham to suggest that it would be “wise to try as far as possible, to treat him with the N.H.S. concentrates ... As a last resort I think it might be justified to put him onto one of the commercial Factor VIII concentrates.” The reason for that recommendation was not specified, but in any event his parents were never told of any risk of infection associated with the use of factor concentrates.[1989]
Matthew Johnson’s treatment at the Oxford Haemophilia Centre, as a boy with severe Haemophilia B between 1981 and 1983, included the prophylactic use of concentrate. His parents were assured that if he were to contract hepatitis it would be no more severe than a bad cold. They were not told the true risks – rather they were assured and “were told that this product was ground-breaking, it was clean and it was as good as good can be.”[1990]
Mr AN, who was treated with commercial concentrates at Birmingham Children’s Hospital from 1977 (having previously been on home treatment with cryoprecipitate), was told nothing of any risks, nor were his parents: “All we were told was that this was a groundbreaking medical development ... the miracle cure that would solve all of our problems”.[1991]
The widow of a man treated at QEH recalled how her husband was “really against switching to Factor VIII as he had seen an article in the Mail on Sunday in May 1983, which said that Factor VIII presented a risk of HIV transmission.” He took the newspaper cutting to the haemophilia centre and was told that it was “blown out of proportion” by the press. He expressly requested during 1984 to be treated with cryoprecipitate or NHS concentrate but was told that the risk of him developing AIDS from the US product was “a million to one.” He was infected with both HIV and Hepatitis C.[1992]
Nothing was said to the parents of Colette Wintle, a symptomatic carrier of Haemophilia A, about the risks of treatment when she was given commercial factor concentrates instead of cryoprecipitate at the age of 17 when her tonsils were removed in 1976. Nor was Colette told about the risks of factor concentrates, or offered the safer alternative of DDAVP, when she had a procedure under general anaesthetic in 1982; instead she was treated with commercial concentrates, as she was again in 1985, still without being advised of the risks or offered safer alternatives.[1993]
Irene Brierley’s husband, who had Haemophilia B, was expressly told in January 1985 in Liverpool that Factor 9 was safe to inject without fear of infection – although not heat treated it was “safe”.[1994] This is not an assurance that could properly or truthfully be given.
Simon and Nigel Hamilton, twin brothers treated in Belfast (one with mild, one with moderate Haemophilia A), were not given, nor were their parents, any information, warning or advice about the risks of blood-borne viruses associated with the use of factor concentrates.[1995]
A woman with mild Haemophilia B was first given Factor 9 concentrate in 1980 for dental treatment at Royal Stoke Hospital. She did not know she was being given a blood product; she was not told what it was and she was not told about any risks of infection. She had a second treatment with Factor 9 concentrates in 1987. On that occasion she had said she did not want to receive it because of the fear of HIV but she was given it whilst drowsy from pre-med and felt that she was not given a real choice.[1996] She was informed in 1992 that she had been infected with Hepatitis C.
A man with von Willebrand disorder was treated with Factor 8 concentrates for the first time in 1983 or 1984 at the Royal Hallamshire Hospital; he was never told of any associated risks.[1997]
Su Gorman’s husband, Steve Dymond, who had mild Haemophilia A, was led to understand that Factor 8 “was the future, it was the wonder drug, it would make life easier. As a mild haemophiliac he only ever needed treatment in case of accidents or medical emergencies ... Yes, it was very much it would improve the quality of our lives.” Neither she nor Steve were told of the risks of infection.[1998]
Alice Mackie recalled that her husband, Robert, who has severe Haemophilia A and was treated in Edinburgh, repeatedly asked about the risks of treatment and was reassured: “he trusted these doctors ... it was every doctor that he saw and they would always come out with the same thing, ‘Nothing to worry about, Robert’, and in the end he was actually told to stop asking, ‘You’re just causing trouble.’” When he asked about AIDS, “he was always told, ‘our blood donors don’t have AIDS. It’s safe. We don’t have the likes of that in this country’ ... he was told it was safe, we didn’t have AIDS in Scotland or HTLV-III in Scotland.”[1999]
Carol Carruthers’ husband, Oliver, was treated at the Royal Victoria Infirmary in Newcastle and was given prophylactic Factor 9 when he had dental treatment in 1977 and 1979. He was never made aware of the risk of infection. In May 1989 he had a tooth extraction and was given Factor 9, despite having raised concerns about the need for, and safety of, such treatment; as his widow said in her oral evidence to the Inquiry he“trusted that the doctors wouldn’t knowingly put him at risk”.[2000]
A woman with von Willebrand disorder was treated with Factor 8 for the first time in 1981 and 1982; she thought it unlikely that she was told of any risks as she would have questioned whether there were alternative treatments available. She was a qualified nurse.[2001]
Mr M, who was treated at the Leeds Haemophilia Centre, was not given any information about the risks of infection associated with treatment with factor concentrates, nor had his parents been advised of the risks. “We trusted the doctors and it was all about improvement. The message was that things were getting better. The nirvana was there would be a cure. The new boxes of product and kit were smaller and more convenient, leaving more room in our freezer for my mother to use. My brother and I thought our lives were getting better, not shorter.”[2002]
Perry Evans was given no advice or information regarding the risks of the factor concentrates with which he was treated at the Hammersmith Hospital. A letter from the hospital written to his GP in July 1983 noted that “We have recently been inviting all our haemophiliacs to visit the clinic ... We have been particularly concerned because of the development of AIDS (acquired immune deficiency syndrome) in some haemophilia patients in the United States who have been using pooled factor products which have probably included donation from people who were incubating AIDS.” Perry himself was given no information regarding the risks of AIDS. He was not told of the particular concern of those treating him. He was infected with HIV following treatment in the first half of 1984.[2003] Perry died in April 2024.
The evidence which the Inquiry has received from people who were infected or affected is consistent with what some clinicians have said, either to the Inquiry or previously.
Dr Pettigrew acknowledged, talking about the children treated at the Royal Hospital for Sick Children in Glasgow, that there was no policy to inform parents about the risks of HIV and that in relation to hepatitis risks, the focus was on Hepatitis B.[2004] Dr Hann accepted that inadequate information had been provided to parents about the risks of AIDS and that rather than proactively contacting them to discuss risks of AIDS, the approach was reactive.[2005]
Dr Martin, the director at Alder Hey, “did not make it [his] practice to raise the hepatitis issue with families”. And when he first became aware of AIDS he did not “wish to worry parents with what at first seemed to be a tenuous link.”[2006]
At Birmingham Children’s Hospital, Dr Hill claimed that it was his practice to keep patients informed of the risks “as we knew them.”[2007] Whatever he meant by that phrase, people were not given adequate (or usually any) information about the risks of treatment, whether at the Children’s Hospital or at the adult Centre where Dr Hill also worked.[2008]
At the Royal Manchester Children’s Hospital there is evidence to indicate that there may have been very general references to hepatitis, but nothing specific about NANBH, or AIDS. In a document about home treatment, authored by Dr Evans in November 1978 and clearly designed for parents (or possibly for the older children), there were detailed instructions about how to administer the concentrate but the only reference to infection was a statement that “Used syringes and needles should not be put in the dustbin – they could infect anyone emptying the bins.”[2009] An article in Nursing Times in 1981 by the haemophilia nurse at RMCH, Alex Susman-Shaw, referred to a patient who had been infected with Hepatitis B from a contaminated batch of Factor 8, but then contained the reassuring statement that “The problem of hepatitis B transmission owing to the use of large donor pools from a high-risk population has been now virtually eliminated. This has been achieved by routinely testing all donations and all batches of FVIII by radioimmunoassay and by using a lower-risk population.”[2010] Quite apart from the debatable accuracy of the reference to a lower-risk population, and the exaggerated claims for the efficacy of screening tests, there was no reference at all to the risks of NANBH. It is reasonable to conclude, therefore, that parents and patients were not provided with the information that they should have been about NANBH transmission.
The information which Dr Bevan thought that Professor Flute would have provided to patients at St George’s Hospital about hepatitis risks was that:
“they would be likely to get a brief period where their liver function was affected, that there was a form of hepatitis was almost inevitable – as it was – very soon after first exposure to commercial pooled product. He would tell them about this, but he would tell them about it, and us, in a reassuring way: everybody goes through this, it doesn’t seem to cause any problem, people don’t get very sick with it, sometimes you don’t even have jaundice sort of thing.”
As Dr Bevan observed, therefore, patients were informed about it but not “fully” or “validly” informed.[2011]
To similar effect, Dr Colvin thought he did discuss whether liver function tests were abnormal or normal, but in response to the question whether he told patients that the treatment may carry a risk of a hepatitis virus that was not Hepatitis B and that might cause long-term chronic liver problems, he said “I think we could have done better” and “I think it’s possible that the patients didn’t get the advice or information that maybe they should have had.”[2012]
Professor Bloom, writing in September 1991, expressed the view that “it was not necessary to inform patients or parents” of the risk of AIDS “at that time” (he was talking there of the period up to June 1983, but there is no evidence that it was his practice at any time thereafter in 1983 or 1984 to provide information to patients or parents about such risks).[2013]
Dr Al-Ismail, the centre director at Swansea, did not tell patients in 1983 or 1984 of the risks of AIDS. He believed that “haemophiliacs knew the risk.”[2014]
Dr Al-Ismail was not alone in seeking to argue that patients themselves were well informed about the risks. Some clinicians argued in oral or written evidence that patients were well informed because they had access to information from the Haemophilia Society.[2015] It is certainly true that, in a general sense, many patients were familiar with the word “hepatitis”, and that it could be an illness which came with treatment. If their haemophilia was severe they came to meet and get to know other people who like them were severely affected, for they had treatment from the same centre, possibly several times a year. Many undoubtedly would talk about their treatments. However, the Haemophilia Society, rightly, advised its members to take their medical advice from their doctors: its information merely enabled those who wished to do so to know what questions to ask their clinician. The doctor was the person a patient would trust to give them information about theircase, the probability of infection for them, what the consequences of infection meant for them, and most important, perhaps, of all, what alternatives there might be to taking the treatment being offered. That was because a patient is, and is entitled to see themself as, an individual to whom risks in general may or may not apply – and it is their doctor who should most be trusted to give them that information, specific to their case, and in the cases of the patients who gave evidence to the Inquiry was trusted to do so (at first).
It lacked insight into the nature of the doctor-patient relationship for a doctor to think that a patient would get, and rely upon, information about their treatment given by anyone else than them.[2016] It not only was not insightful, but unbecoming for doctors – and to an extent an abdication of their role – to shift the ethical burden of providing sufficient information to the Society, or to fellow sufferers, or to the popular or medical press; or, for that matter, to avoid accepting their own professional failures to provide it. Yet there was a sense in some of the evidence that some doctors were doing that. That said, the Inquiry would itself be lacking insight if it did not accept that it must have been particularly difficult for doctors to be faced with their treatment having caused what was probably a terminal illness, and more besides, in a large proportion of their patients. This is especially so when it was the opposite of what they came into medicine to do. It is hard. It is not easy. But where it is, in truth, their responsibility, the only proper course of action is to face it, admit it, and deal with the consequences (which, after all, are worse for their patients, however hard it is for them).
An example which supports a sense of clinicians seeking to spread responsibility to others is provided by the actions of Professor Ludlam. He prepared a document for the Penrose Inquiry[2017] setting out a summary of the information about HIV available to patients in Scotland prior to 1 December 1984, over 17 paragraphs in 4 pages, followed by information about HIV available to patients in Scotland after that date, over 42 more paragraphs and 7 more pages, concentrating on what the Haemophilia Society said at the time, before saying (in 9 lines):
“In summary,[2018] whilst the above Haemophilia Society publications were sent to all members and copies made available at Haemophilia Centres, it was the contact with the Centre staff which offered the most personal and potentially applicable information and counselling. HIV/AIDS was a completely new and bewildering condition, which was very different from any previously known infection; information, arrangements for anti-HTLVIII testing, monitoring of immune function, prophylaxis against opportunistic infections and anti-HIV treatment evolved from 1982 onwards.”
He was absolutely right to suggest that it was what the clinical staff at the centre had to say, when (and if) providing information personally to a patient, that an individual patient had to rely on, whatever might elsewhere be said generally about others. Unfortunately, setting out at such length other sources of general information is unnecessary to convey that message. His doing so therefore gives the impression, rightly or wrongly, that he is seeking to hide behind the actions of others. It was at best ill advised.
Another example from another course is that in his book, Haemophilia Home Therapy, Dr Jones wrote “Every family knows that the use of human blood products carries the risk of hepatitis. They are aware that this risk has been linked particularly to commercial concentrates prepared from the blood of paid donors, and they know that these risks still exist despite the increased sensitivity of donor tests for hepatitis B.”[2019]
The evidence available to the Inquiry does not support a conclusion that patients were well informed about the risks to them from the treatment which they were receiving or would receive.[2020]
Some people may have had a basic understanding that jaundice or hepatitis might be a consequence of treatment, but what they lacked – and what it was the responsibility of clinicians to provide – was information about (in particular) NANBH and the possibility of chronic and serious liver disease.
Some clinicians asserted to the Inquiry that patients were told that they would inevitably be infected with NANBH and that a substantial proportion could go on to develop chronic liver disease; see for example the statement of Dr Jones.[2021] That is not, however, consistent with the vast bulk of the evidence received by the Inquiry from individuals, which I accept.
In relation to AIDS, it was the responsibility of clinicians to tell their patients that treatment carried with it a risk of transmission of the virus/agent that caused AIDS and to explain that AIDS was a very serious, usually fatal, disease for which there was no treatment. The vast bulk of evidence received by the Inquiry from individuals, which I accept, was that they were not provided with that information. To the extent that reliance might be placed by clinicians on what was in Haemophilia Society publications, the material published by the Society in 1983, 1984 and 1985, which was authored by clinicians, provided a false reassurance as to the safety of treatment.[2022] It is truly astonishing – not in a good way – that at a time when potential blood donors were being told “Can AIDS be transmitted by transfusion of blood and blood products? Almost certainly, yes”, and in relation to people with bleeding disorders, “Should just one of the donors be suffering from AIDS, then the Factor VIII could transmit the disease”,[2023] that the recipients of products made from donated blood were not being given that same information.
It should be emphasised that the above are examples only. The evidence available to the Inquiry establishes overwhelmingly that the vast majority of people were not told about the risks of treatment, and that this was not merely something that went wrong in one or two haemophilia centres, but in centres across the entire United Kingdom. There are undoubtedly some examples of people being given sufficient information by their clinician, but these are few and far between compared to evidence given from many different people, from many different walks of life, with different capacities to recall what has or has not been said, who have said in oral testimony, in written statements, or through intermediaries that they were not told of the risks in any adequate form or at all.
Further, had information as to the risks of NANBH or AIDS been provided as it should have been, that should have been recorded in the medical records of the individual concerned. Such medical records as the Inquiry has considered in the course of reading and listening to the testimony of people infected and affected do not generally record advice being given about viral risks of treatment.
The evidence before the Inquiry establishes that, in many (although not all) haemophilia centres, testing for HIV in the mid 1980s and for Hepatitis C in the early 1990s was undertaken without the knowledge – and, it follows, without the consent – of patients (or in the case of children, their parents).
In a number of centres, tests were undertaken using stored samples – in circumstances where people were unaware even that samples of their sera, or of their child’s sera, had been stored.[2024] This was, for example, done at the Royal Free where patients were tested for HIV without their knowledge.[2025] It was also done at the Edinburgh Royal Infirmary both in relation to the HIV testing that was undertaken in 1984 and in relation to testing for Hepatitis B with the second-generation tests.[2026]
Even where people were made aware that blood samples were being taken (as was often routinely done at appointments) or that some form of test was being undertaken, they were often not told what that test was for, still less offered any form of pre-test counselling. Thus, for example, in Inverness a letter sent in February 1985 stated “Because of the recent problems with AIDS, we are now producing new types of Coagulation Factors. Before this can be issued, we need to do a blood test on each of our patients.” This letter did not explain what the blood test was for and did not state that it would be a test for HIV.[2027]
One of the consequences of people not being told that tests were being undertaken – quite apart from the affront to their personal autonomy – was that the results of such testing then came out of the blue.
Bruce Norsworthy’s son had an operation on his ankle in 1982 or 1983 and he says“I do not know if he became infected [during the operation] or whether he had already been infected, but it was after Richard had that operation when we were notified that he was HIV positive. We were not even aware that a test was being carried out.” They learned that Richard was HIV positive when they received a telephone call from the hospital one evening. It was “a pretty awful blow.”[2028]
Kathleen Algie recalls being told of her husband’s infection with HIV in or around May 1988:
“we were invited in for a seemingly normal review day ... At the end of this meeting they informed us that John had been diagnosed with HIV. I was not particularly surprised, as I had been under the impression for some time that haemophiliacs treated with these blood products might end up getting HIV or AIDS ... What was a shock however was that John was being tested for HIV at all, as we had not been informed of this previously. We were told at the meeting that he had been HIV positive for 3 years.”[2029]
Although this does not excuse individual clinicians, there was no guidance or advice – whether from UKHCDO or the Chief Medical Officer or central government or elsewhere.
When advice was given by the General Medical Council later in the 1980s, not all agreed with it. Dr Thomas Taylor (Inverness) wrote in 1988 that it was “inappropriate, unethical and illogical that we have to seek patient consent before testing for HIV.”[2030]
This pattern was repeated for many people when Hepatitis C testing became available: multiple witnesses have told the Inquiry that they were not aware that they were being tested for Hepatitis C.
The evidence before the Inquiry shows that there was no uniform approach to people being told that they, or their child, had been infected with HIV or with Hepatitis B or C. It is right to acknowledge that some were told in person, as they should have been, and that attempts were made to explain the position to them and to help them understand on the basis of the (sometimes limited) information that was then available. In some instances testing was undertaken soon after it became available and there were no significant delays before the results were communicated.
But for many that was simply not the case.
Again some examples serve to illustrate the position.
I have described elsewhere in this Report how children at Treloar’s were informed of their diagnosis of HIV.[2031]
At Birmingham Children’s Hospital Elisabeth Buggins recollected a large meeting in October 1984 at which Dr Hill informed the parents that “some boys, mainly those treated with large numbers of units of Factor VIII were at risk.” She later saw, on the fridge door, a list of patients which included her son’s name – and after requesting to speak to Dr Hill he confirmed her son was HIV positive.[2032] Brenda Haddock, another mother, recollected attending such a meeting and Dr Hill “stressing that it’s in the boys’ best interests to carry on with the treatment.” She added:
“And in those days we all -- you know, we believed doctors. We’d put our faith in doctors ... we followed what the doctors said. So, you know, we blindly carried on giving the treatment. But I do wonder, afterwards, why couldn’t they just temporarily stop the Factor VIII treatment while they investigated exactly what was going on, and give us some more information? You know, why did we have to sort of blindly carry on?”[2033]
The parents of a child treated at Birmingham Children’s Hospital were not told that he had been infected with HIV – their son, still a child, had been told at an outpatient appointment with Dr Hill; he assumed (understandably) that his parents had already been told, and did not speak to them about it because of that assumption.[2034]
At the Royal Manchester Children’s Hospital, parents, unaware that their children were being tested for HIV,[2035] were informed of the test results by letter: “We have been sending blood samples away from the children with haemophilia and similar diseases to see if they are at risk of AIDS. None of our patients has developed AIDS or has shown any signs of doing so, but all of us, both parents and staff, are anxious about the problem. The results are now coming through. The blood tests on your child ... show that he is positive for antibodies to HTLVIII.”
The letter stated that this did not mean that the child had AIDS but there was a “small chance” that he might get it, before continuing “Of the first 16 patients we have tested, over 60% have given a positive result. Nearly all of them have been treated with the old factor VIII concentrates made in the USA.”[2036]
Quite apart from the lack of humanity involved in informing a person by letter that they had been infected with HIV, it was utterly thoughtless and inappropriate to do so, not least because letters can go missing or be misdelivered.[2037]
The evidence in relation to Liverpool suggests that patients were being told the outcome of testing only in the second half of 1985 and into 1986. When Professor Hay arrived in Liverpool in 1987 he found the records to be poor and uninformative and was unable to obtain the results of the tests that had been carried out. He was told by patients that they were informed of HIV positive results by letter. Dr McVerry left no record of the results, even though he published them.[2038]
Where patients in Liverpool were told in person, as opposed to by letter, it was not done as it should have been. The widow of a Haemophilia A patient described her husband being told during a routine appointment that a stored sample had tested positive, but the patient had not known his blood was being stored or tested. “This consultant was flicking through my husband’s medical records and came to a page which was marked with the words “HIV” . The consultant just said the words “HIV” in a very matter of fact way and then continued to flick through the notes. My husband stopped him and said ‘HIV, what is that? I did not know anything about that.’ The consultant basically said words to the effect “yes you have this.””[2039] Another, concerned about her husband’s health, raised concerns with Dr McVerry that he was suffering from the symptoms of AIDS but Dr McVerry denied it and told her not to be neurotic. She ended up speaking to Professor Anthony Pinching at St Mary’s who agreed to discuss it with Dr McVerry – the latter then told her “not to question his standing or undermine his opinion.” Her husband died not long after that.[2040]
At York Haemophilia Centre some were told by letter of their infection with HIV (unaware that they had been tested);[2041] Derek Martindale had himself proactively asked to be tested in August 1985, no test having been offered or undertaken.[2042]
Doctors in the Cardiff Haemophilia Centre suspected that Ruth Major’s husband, Peter, might be suffering from AIDS, but did not share that with him. A form regarding a hospital admission on 12 March 1984 noted “HTLV 3 pos”.[2043] On 16 July 1984 a letter was sent to Peter’s GP, referring to symptoms of candidiasis, lymphopenia, lymphadenopathy and splenomegaly, and stating that “It remains a distinct possibility that he is developing the acquired immune deficiency syndrome (A.I.D.S) and we shall review him more carefully in the Outpatient clinic.” The letter continued that “Obviously” they had not discussed this with him “as it would inevitably lead to major alarm.”[2044] On 20 November 1984, a letter was sent to Peter’s GP, referring to weight loss and lymphadenopathy, and expressing the concern that “he may be developing the syndrome of A.I.D.S. The relevant diagnostic tests are difficult to perform and not currently available in South Wales. We have not mentioned our suspicions to him or his wife on this subject.”[2045] Ruth thought her husband was only told that he was HIV positive in the spring of 1985.[2046]
Paul Summers was a patient of the Cardiff Haemophilia Centre. An entry in his records noted that he had had the same batch numbers as a patient whose name was blacked out but which was in all likelihood a reference to Kevin Slater.[2047] This information was not shared with Paul. In September 1984 Professor Bloom wrote to Paul’s GP in terms which make it clear that he had been examining Paul for symptoms which might be indicative of AIDS.[2048] Nothing was said to Paul.[2049] In September 1985 Professor Bloom wrote to Paul’s GP. Having referred to grossly abnormal liver function tests the previous year (which Paul had not been told about), Professor Bloom then informed the GP that the tests for HTLV-3 “came out as positive” and expressed the intention to “keep a close eye on him and review him from time to time.”[2050] Paul still “knew nothing about it ”.[2051] In September 1986 Professor Bloom’s clinical assistant wrote to a haematologist at Plymouth General Hospital, Dr Stafford, to tell him that Paul would shortly be coming to reside in Plymouth. The letter stated that Paul was HTLV-3 positive.[2052] This had still not been shared with Paul, who only learned that he was HIV positive when he went to the hospital in Plymouth in November 1986 “and the doctor asked him how he was handling his HIV and that was the first Paul had heard of it.”[2053]
Some were told not at a special appointment, the purpose of which they would have been aware of, but at their next routine attendance. The problem with that approach was threefold. First, it might mean that in the case of child patients the parent bringing the child – usually the mother – would be on their own and would receive the news without the father or other family members present.[2054] Secondly, it might well lead to a delay in the individual being told, which would put those close to them at risk. Thirdly, there were some instances in which the individual, unaware that they had been tested, would not attend for the appointment, and would thus remain ignorant of a positive test result.[2055]
The mother of a boy infected with HIV following treatment with Armour’s heat-treated Factorate was told of her son’s diagnosis by telephone.[2056]
Large-scale meetings, such as that described in relation to Birmingham Children’s Hospital, took place at various haemophilia centres, and inevitably led to confusion and distress. Christine Woolliscroft, whose son Michael was treated at Birmingham Children’s Hospital, recalled being worried about what was said at the meeting but on asking the haemophilia sister on the next occasion if Michael was all right, she was told that he was fine. Then about a year and a half later she went to a meeting with Dr Hill, understanding that it was about Michael’s transfer to the adult Haemophilia Centre, and at the end of that meeting Dr Hill “dropped the bombshell” that Michael had HIV.[2057]
In Edinburgh a group meeting for patients took place on 19 December 1984. It was precipitated by Professor Ludlam learning that the Yorkshire Post intended to publish a news story on 20 December.[2058] On 12 December he wrote to patients referring to publicity in the press and TV about the HTLV III virus and AIDS and explaining that Dr Forbes and he were holding a meeting to discuss with patients “some of the anxieties and issues that have been raised.” The letter itself did not refer to any difficulties with Scottish Factor concentrates, nor to the fact that patients had been tested.[2059] One problem with the letter is that recipients might simply have thought it was a meeting designed to reassure and that they were not personally at risk (having received “safe” Scottish products) and that there was no need for them to turn up. Professor Ludlam’s recollection was that, having invited hundreds of patients, only a few tens turned up.[2060] Following the meeting it was left to patients to make contact with the Centre to find out if they had been tested and what their tests results were. The potential for confusion with such a large group meeting was apparent from the evidence of one of the attendees: Alice Mackie explained how what she and her husband took from the meeting was that he had not been infected, because if he had been one of those infected he would have been told.[2061] An information sheet sent out to patients subsequent to the meeting informed them that “tests are now available and will be carried out on your routine visits to your centre.”[2062]
In January 1985 a letter from Dr Wensley was sent to adults with haemophilia treated at the Manchester Royal Infirmary. The letter was written in the light of recent media coverage about AIDS and the deaths of two people with haemophilia. It explained that many people with haemophilia had been exposed to HTLV III but that it was expected that most people with haemophilia exposed to the virus “will remain well and will eventually become immune to it.” Recipients were told “Until the right tests are available, it is probably best to assume that you could be carrying the HTLV 3 virus.”[2063] Shortly afterwards, in early February 1985, a special meeting on AIDS was held at the Manchester Royal Infirmary.[2064] Some time then appears to have elapsed before patients were tested: the earliest letter offering a test which the Inquiry has seen is from 22 May 1985; another example is dated 2 September 1985.[2065] Evidence from individuals suggests that some were informed at routine appointments, others by letter.[2066]
People treated at the Belfast Haemophilia Centre had memories of meetings being held there. Some attendees recalled Dr Elizabeth Mayne giving those present the choice of whether they wanted to know the result of their HIV test.[2067] Dr Mayne recalled three such open meetings being held: in addition to patients, “members of portering, catering and cleaning staff were all invited to attend and express their worries and queries about HIV infection.”[2068]
Sometimes there were substantial delays between the test results being available and the patient being informed. In May 1985 Dr Pettigrew wrote to Dr Taylor at Inverness about a young boy who had previously been treated at the RHSC. She informed Dr Taylor that stored samples had been tested and found to be positive, adding “I thought you ought to be informed so that you can arrange for appropriate measures to be taken.” But the man who was the subject of this letter understands his own parents were not told until 1987 or 1988, ie some two or three years later.[2069]
In Glasgow Royal Infirmary, the 77 patients whose blood was tested for HIV as part of a study were not told that these tests were taking place. The samples were sent off from Glasgow Royal Infirmary to Dr Robert Gallo’s laboratory in the US for testing sometime after July 1984, with the results being received back in September/October. The results of the study were published in December 1984 (and would have been prepared a month or two before publication).[2070] Yet none of the 12 patients who had tested positive had been told of the test results. Remarkably, it does not appear to have occurred to those involved that the right people to be told first were the patients.[2071] A letter was then prepared to send to all patients in January 1985, inviting them to be tested,[2072] but it appears likely that that letter was never sent and instead a letter was sent out in April 1985, offering to discuss AIDS at the next clinic appointment, or earlier if the patient would wish it.[2073] It follows that (if the January letter was sent) something in the region of four months elapsed after Dr Forbes knew that there were 12 seropositive patients before an attempt was made to offer them an appointment; and that if the January letter was not sent, over six months elapsed. It was Dr Forbes’ duty to ensure that his patients were notified as soon as possible; instead he prioritised the publication of the research.
The lack of a uniform approach to testing and informing patients may to some extent reflect the lack of consensus at the Elstree meeting on 10 December 1984. There was a “long discussion” on whether people found to be HIV positive were to be informed. The note of the meeting records that “Several differing views were expressed. It was agreed that each clinician would decide for each case depending on the facts of the case but in general to provide information if asked for.” The minutes do not reveal which clinicians expressed what views, although Professor Bloom is noted as summarising the views as “saying that testing should be instituted as soon as possible, and that information on the test results, should not be given automatically but if asked for.”[2074] That clinicians contemplated the possibility that people infected with HIV through their treatment should not be told of the infection is incomprehensible, both ethically and from a public health perspective, let alone the perspective of their partners, families, and associates, and whether viewed from the perspective of today or the perspective of the 1980s. It was utterly wrong even to consider, let alone regard as acceptable, withholding such a diagnosis. Dr Mark Winter rightly described this as “utterly bizarre”.[2075]
There was a similar lack of any uniform approach to testing for Hepatitis C and informing patients of their test results. Some patients were tested using stored sera, often without any knowledge that sera had been stored or that tests were being undertaken on it. Others were tested using blood taken at routine appointments, unaware of the purpose of the test. The communication of test results was often delayed, with people learning that they had been infected with Hepatitis C sometimes years after they were tested and often only at routine appointments so that they were ill-prepared for the news.
A common account in the evidence which the Inquiry received was of people with bleeding disorders learning that they were Hepatitis C positive in the mid 1990s, sometimes in the late 1990s, tests having been available to centres since 1990. For example, Thomas (Dai) Griffiths was informed in December 1999, although his medical records contained test results for 1990 and 1991.[2076] Mr Z did not learn that he had Hepatitis C until the late 1990s, even though his positive test results were communicated to his GP in early 1992.[2077] Dr Dawson suggested in her statement to the Inquiry that “the prime reason for our apparent inertia was that we did not know what to tell our patients, and we did not know how to treat them until the mid to late 1990s.”[2078] Graeme Malloch tested positive for Hepatitis C in 1992 but was only told in 1995.[2079] Gerald Stone was tested in December 1990 and again in June 1991 but was only told that he had been infected in July 1993 (in contrast to his GP who was informed in January 1992).[2080]
In some cases even longer periods of time elapsed: by way of examples, Colin Catterall, who has moderate Haemophilia B only learned that he had Hepatitis C in 2010;[2081] another witness with mild Haemophilia B only discovered that he had been infected with Hepatitis C in 2018.[2082]
Some found out their diagnosis “accidentally”: Rosamund Cooper, who has von Willebrand disorder discovered that she had Hepatitis C in 1993 during a pre-operative chat prior to an ankle operation: “it was mentioned in passing that I had HCV, in terms of precautions to be taken during the operation. I was shell shocked by this information. My mother had just left the hospital and I was alone. The doctor discussing the diagnosis was surprised that I was not aware of the infection.”[2083] Ms E, who had von Willebrand disorder, learned that she had Hepatitis C through a casual conversation with Dr Mayne in the corridor: “She stopped us and said, ‘Well, how are you feeling now?’ I said, ‘I am still feeling very tired, still don’t feel great. I feel like there’s something really wrong.’ She replied, ‘If it is not your ME, it must be your hepatitis C.’ That was the first I had any knowledge that I had hepatitis C.”[2084] Ms J, a symptomatic carrier of Haemophilia B, was told that she had been infected with Hepatitis C at a routine check-up, in the middle of which she was asked “How are you coping with your hepatitis C?” She was unaware that she had been tested and “nearly fell off the seat. There and then I just thought, ‘I have been handed a death sentence ... my whole world just collapsed.”[2085] Bruce Norval, who has moderate Haemophilia B, was told that he had tested positive for Hepatitis C by a senior registrar whom he bumped into at the hospital.[2086]
Colette Wintle was told that she had Hepatitis C only in late 1991, but the Royal Free Hospital told her GP (though not her) in 1985 that she had chronic non-A non-B Hepatitis.[2087]
Simon Hamilton’s medical records contained a positive test result for Hepatitis C in October 1990.[2088] He was not told that he had been infected with Hepatitis C until March 1994.[2089]
Some people never found out in their lifetime that they had been infected with Hepatitis C: one woman learned that her husband had been infected with Hepatitis C only from the post-mortem report following an autopsy. Her husband had never been told, despite medical records showing that he had been tested and found positive a year before his death.[2090]
Some of the evidence which the Inquiry heard from clinicians sought to explain that the 1970s and 1980s, and even the 1990s, were part of an era of clinical paternalism, where things were done differently – one implication being that they should not be judged by the standards of today.
However, a different perspective was offered by the expert panel of medical ethicists who provided a written report to the Inquiry and gave oral evidence over two days in January 2021.[2091] There are, as the experts told us and as I find in any event, certain fundamental ethical norms and principles which lie at the heart of medical decision-making and doctor/patient interactions. Of central importance to this Inquiry are the principles of respect for autonomy, beneficence (the imperative to do good – “you should promote people’s well-being”) and non-maleficence (“you shouldn’t harm people”).[2092]
The latter two principles are reasonably self-explanatory but the concept of autonomy merits some wider exploration. As Professor Bobbie Farsides explained, “it’s something that goes beyond your individual liberty because it locks into you as an individual, your values, your beliefs, what matters to you, your plans, your projects”.[2093] Ultimately, “it’s the patient who has to lead their life and the doctor is, essentially, a public servant, a servant to that end, using their knowledge of diagnosis and treatment and medicine to enable that.”[2094]
Informed consent is a basic and fundamental principle of clinical practice and the philosophical basis for that is patient autonomy. Not being informed fundamentally undermines autonomy because the person is denied the opportunity of real choice; “you should always treat human beings as an end and not merely as the means, and how you treat somebody as an end is essentially if you get their informed consent, in a nutshell.”[2095]
The doctrine of informed consent also promotes human dignity, partnership and trust. Dignity is a concept which again derives from autonomy: it involves independence and is determined by the person’s own values and idea of their life. Partnership is about being given information, having a dialogue, supporting the patient in making a decision on the basis of the relevant information. Trust involves trusting individual clinicians to respect an individual’s autonomy and dignity.[2096]
Some doctors almost certainly took the view that they knew what was best for the patient, or assumed that there was no need to tell patients of the risks associated with particular treatment because they believed that the patients would press ahead with the treatment in any event, irrespective of the risks, because of the advantages of that treatment perceived by the doctor (in particular in terms of efficacy and convenience).[2097] But that was never a justifiable basis on which to proceed. As the medical ethics panel told the Inquiry: “unless you at some point raised the issue of risk and associated that with the treatment that you are assuming the patient wants because of their wishes and the outcome that they hope for, you don’t know whether that is actually what they want because they have the right and the ability to weigh up the significance of that risk against their overall goals.”[2098] Moreover, “there’s a huge amount of literature that suggests that clinicians are rubbish at predicting, you know, or knowing full well what patients want ... other health professionals are also rubbish, sometimes slightly less, but doctors are particularly bad at it ... you have to have that conversation.”[2099]
As John McDougall, whose son was fatally infected with HIV through treatment with Factor 8 powerfully expressed the position, the importance of knowing the risks and being able to take an informed decision was a “complete no-brainer” – “for any parent if you’re comparing convenience with eliminating risk for your child, then you’re always going to select the elimination of risk for your child over convenience, of course”.[2100]
Having regard to these principles, and in addition to the principle of veracity or truth telling,[2101] it was unethical and wrong that people were not told of the risks of treatment, and the consequences of the failure to do so was that people were treated without their informed consent.
It was unethical and wrong that people were not told that they were being tested for HIV or for one or more of the hepatitis viruses. The failure to tell them was a denial of their personal autonomy.
It was unethical and wrong that people were not told, or not told promptly, of the result of such tests. Again, as explained by the ethics panel, “once a diagnosis is known by the doctor, then the doctor needs to inform the patient because ... without that information the patient cannot actually exercise their autonomous choice about what to do next and what kind of treatment to explore, what kind of options to explore and they will need accurate and transparent information about this particular diagnosis, even if it means doing nothing.”[2102]
A culture of paternalism, a “doctor-knows-best” attitude, may explain some of these ethical failures, but it does not excuse or justify them. As the ethics panel observed by reference to two examples of once-accepted practice that horrifies today (the pelvic examination of women under anaesthetic at training hospitals without their consent and the retention of organs at Alder Hey without parental consent), “there are certain things that happen where when it happened, in terms of time and space, are not going to excuse them”.[2103] What happened to people with bleeding disorders, as detailed in this section of this chapter, is just that: something that is not excused by reference to when or where it happened.
This chapter examines the provenance of blood and plasma processed by pharmaceutical companies. It looks at commercial pool sizes, the product information supplied, knowledge of and response to AIDS, and measures taken to reduce risk. The focus is on how these issues affected the blood products that were made available to NHS patients in the UK. For a fuller picture, this chapter should be read in conjunction with Regulation of Commercial Factor Concentrates and Viral Inactivation.
1973 - 1976 five commercial Factor 8 products granted licences in the UK.
December 1975 Broadcast of World in Action documentary Blood Money in the UK.
Mid-1970s FDA inspection regime commences in the US.
July 1982 MMWR reports three people with haemophilia have contracted AIDS in the US.
August 1982 Alpha informs FDA it will not be using plasma from hyperimmunised donors for factor concentrate manufacture; Cutter adopts similar approach.
December 1982 - February 1983 pharmaceutical companies start excluding high risk donors (especially male homosexuals, intravenous drug users).
4 January 1983 meeting in Atlanta discusses AIDS risks and response.
7 January 1983 Alpha press release: risk of AIDS in Factor 8 concentrates.
March 1983 FDA recommends excluding high risk plasma from blood products.
19 July 1983 US Blood Products Advisory Committee discusses product recall and concludes it should be decided on case-by-case basis.
Dr Dennis Donohue director of the Division of Blood and Blood Products, FDA
Kelly Duda, Michael Gillard, Ed Harriman investigative reporters/filmmakers
Dr Bruce Evatt director of the Division of Immunologic, Oncologic and Hematologic Diseases, CDC
Dr Don Francis epidemiologist, CDC
Dr John Hink director of plasma procurement, Cutter
Dr Steven Ojala director of regulatory affairs, Cutter
Dr Henry Kingdon vice-president and general manager, Hyland
Dr Michael Rodell vice president of regulatory affairs, Hyland (1982 - 1983), vice president of regulatory and technical affairs, Armour (1983 - 1990)
Dr Edward Shanbrom medical director and director of research, Hyland, (until 1975)
CDC Centers for Disease Control and Prevention
FDA Food and Drug Administration, US
NHF National Hemophilia Foundation, US
The events which are described in this chapter took place more than 34 years ago and, mostly, 40-50 years ago. Since then, many voices have been raised in criticism of pharmaceutical companies in respect of the damage done in the UK by some of the products manufactured in the US or in Austria, which were licensed, imported and distributed in the UK.
In the chapter which follows, the labels “Armour”, “Cutter”, “Travenol”, “Hyland”, “Baxter”, “Immuno”, “Abbott”, and “Alpha”” are used to describe the companies who produced the main factor concentrates that were imported into the UK and used in the treatment of patients within the UK. This is done for readability.[2104] On occasion reference is made to other companies that formed part of the wider corporate entity to which the companies referred to above belonged – for example where it is necessary for context to distinguish between the manufacturing company in the US or Austria and either the UK company that held the relevant product licence or its ultimate owner.[2105]
Care needs to be taken in understanding that this chapter relates to events which took place in the 1970s and 1980s. Some of the companies named generically in the way described above no longer have any separate identity which the law would recognise: many have been dissolved or liquidated, or their businesses have been absorbed into another company by a takeover or acquisition, such that the labels used here must be seen as having historical significance only.
It follows that though the same names may be recognised in today’s world of commerce, it would be inappropriate simply by reason of a commonality of label to hold them (as they exist now) responsible for what was done by what were different corporate entities some considerable time ago. Readers should understand the report, where it is critical, of being so in relation to companies as they were then, not as they are now.
Second, the chapter describes both what happened in the UK (importation, licensing, marketing, and distribution) and what happened abroad (the collection of plasma, production, and product development). The Inquiry has powers to compel the production of documents which are held in the UK or by a UK company which still exists, but those powers do not extend beyond the UK. Nor is it possible, practically, to obtain many documents from companies which have ceased to operate. Notwithstanding this, the Inquiry has managed to piece together a view of what happened, from a number of sources (including some companies, voluntarily). It has nonetheless to be recognised that there is a greater chance that this view might be less complete than is the case in respect of other chapters.
Third, it is right to note that no pharmaceutical company sought core participant status in this Inquiry.[2106] Accordingly, no pharmaceutical company sought to have access to the wider range of documentation that the Inquiry shared with core participants, and no pharmaceutical company sought to exercise the right that core participants have to make detailed submissions to the Inquiry in the form of opening and closing statements.[2107]
The actions and omissions of pharmaceutical companies are described throughout parts of this Report, in particular in the chapters dealing with Regulation of Commercial Factor Concentrates and Viral Inactivation. What follows should be read alongside those chapters. It seeks to avoid duplication. So a reader will not find a comprehensive account of the parts pharmaceutical manufacturers played in what occurred in the UK. Instead this chapter describes:
The focus of the chapter is on how these issues affected blood products that were made available to NHS patients in the UK.
Blood and plasma donated for the production of medical products was, throughout the period relevant to this report, a scarce and hence valuable commodity. Writing in 1998, Douglas Starr observed that it “must certainly rank among the world’s most precious liquids.” At that time, the annual worldwide supply amounted to “sixteen million gallons ... the equivalent of thirty-two Olympic-size swimming pools” and its value by volume was over 1,500 times that of oil. By his estimate, the world market for blood and its derivatives was then in the region of $18.5 billion per year.[2108]
It is unsurprising that pharmaceutical companies saw blood, plasma and blood products as an area for commercial opportunity. The UK was a marketplace for five main commercial Factor 8 products:
Many of these companies were the subject of acquisitions and mergers in the 1970s, 1980s and beyond. For the purposes of this Report it is not necessary to trace those corporate changes. What is important to note is that while these companies manufactured the products, in general UK subsidiaries were responsible for applying for and holding the UK product licences.[2110] These allowed the UK companies to import, sell and market products to UK customers. After an initial experiment with a central contract negotiated by the Department of Health and Social Security (“DHSS”), those customers were haemophilia centres, hospitals and regional health authorities. Again, it is not necessary in this Report to trace the changes in corporate structures of the UK companies.
These companies produced other blood products that were used in the UK at times relevant to this Report, including Factor 9 products. Some of these were licensed, for example Prothromplex and Proplex, the Factor 9 products produced by Immuno and Hyland respectively. Others, such as Konyne and Profilnine, the equivalent products produced by Cutter and Alpha, were not but were supplied on a named patient basis. FEIBA, an Immuno product designed for Factor 8 inhibitor patients, was regularly prescribed in various forms from the mid 1970s but appears to have been licensed for only ten months between 1985 and 1986 before a further licence was issued in June 1993.[2111]
Much more commercial Factor 8 was used in the UK than Factor 9, both because of the higher number of patients and the greater degree of Factor 9 self-sufficiency for most of this period.[2112] For that reason, the focus of this chapter is on Factor 8 concentrates, although many of the issues that arise apply to both sets of products.
The story of the levels of use of commercial Factor 8 products in the UK can be told in the following broad terms. Kryobulin and Hemofil were the first products to be licensed for use in the UK and, in 1973, were the subject of a one year central contract for ten million international units (“IU”) between the UK companies importing them and the DHSS and Welsh Office.[2113] Although this approach did not result in the expected levels of onward purchase by regional hospital boards,[2114] it did contribute to those two products stealing a march on their rivals. The sales figures for the year ending October 1976 showed the following pattern of usage:
In total, 10.6 million IU of commercial Factor 8 products had been used by UK patients at a cost of £1.2 million over a twelve-month period. Cutter’s Koate had not made an impact on the UK market at that time.
The monthly figures for October 1976 revealed the shift in balance between the products. Hemofil remained the most popular, accounting for 63% of usage in October 1976, but Factorate – the cheapest of the products – had overtaken Kryobulin into second place (20% compared to 17%). This was only one month’s data, but it marked a continuing trend.
In 1983, the DHSS obtained estimated figures for annual UK sales from the commercial manufacturers. These showed that total usage of commercial Factor 8 products had risen over the previous seven years from 10.6 million IU to between 42 and 48.5 million IU. The distribution of market share had changed significantly:
The advent of heat treatment and the development of domestic heat treated products shifted usage patterns again. In particular, Profilate HT gained market share as a consequence of growing confidence that its technique of “wet heat treatment” (in a suspension of n-heptane at 60°C for 20 hours) reduced, although did not eliminate, the risk of infection with non-A non-B Hepatitis as well as inactivating HIV.[2118] In February 1989, Profilate HT was stated to have the largest share of the commercial market, though it is unclear for how long it had held that position.[2119] The size of the commercial market had, however, diminished due to the greater availability of NHS products as England and Wales approached self-sufficiency.[2120]
According to Douglas Starr, the “wildcat days” of the commercial blood product industry occurred in the early 1970s, when increases in demand for blood products and limitations on domestic supply and regulation resulted in American companies seeking blood and plasma from what were then low-income countries.[2121] Plasmapheresis centres supplied US companies from Nicaragua, Mexico, Belize, the Dominican Republic, Costa Rica, El Salvador, Colombia and Haiti.[2122] Haiti has a particular significance, for when AIDS cases first came to public attention in 1981 immigrants from Haiti were found to be at high risk of infection and hence unsuitable as donors.[2123]
Plasma brokers developed to provide a conduit between locally owned plasmapheresis centres and international pharmaceutical companies, in some instances providing different fractions of the plasma to different companies. American companies established their own plasmapheresis centres along the southern border of the US so that Mexicans could access them on foot, importing the donor rather than the donation.[2124]
In Douglas Starr’s analysis, two factors combined to bring the wildcat days to an end.
Elliott Richardson, US Secretary of Health, Education and Welfare, read Professor Titmuss’s critique of the blood industry, The Gift Relationship. In early 1972 he directed his staff to form a task force to look at new ways of managing the American blood supply. Douglas Starr reports that President Nixon ordered Elliott Richardson’s Department to make an intensive study of this.[2125] Thereafter, blood for transfusion in the US was to become more closely supervised, and payments for blood (though not for plasma) were discouraged.
The US Government decided to transfer responsibility for regulation of the blood industry from the Division of Biological Standards to the Food and Drug Administration (“FDA”), which led to the possibility of greater intervention and inspection from a better resourced regulator.[2126]
Douglas Starr’s analysis in this respect is supported by a draft written statement from 1990 given by Dr Henry Kingdon, Vice President and General Manager at Hyland Division. Dr Kingdon was due to appear as a witness in the UK HIV litigation, having been approached to do so by the Blood Products Laboratory (“BPL”). His statement was prepared with the assistance of BPL’s lawyers, but drafting notes and surrounding correspondence show that it was at an advanced stage and had been considered in some detail by Dr Kingdon; it was, however, never finalised or signed as the litigation settled.[2127] In a corrected draft of his statement, Dr Kingdon recorded that:
“In the mid-1970’s the FDA mandated source plasma as a licensed product. In order to obtain a licence for the production of source plasma every collection centre must be inspected annually. Annual inspections are carried out by the FDA who look closely at all procedures in the collection centres including donor selection, labelling of donations and testing. Prior to the direction that source plasma be licensed, a certain amount of plasma was imported for the production of concentrates.”[2128]
The previous draft of Dr Kingdon’s statement included the observation that before the change of regulation “a number of manufacturers in the United States imported plasma from countries such as Haiti and certain countries in Africa for use in the production of concentrates.”That had been crossed out by Dr Kingdon, who recorded no reason for why he wanted this change to be made. Both versions of the statement went on to state that:
“All importation stopped following the FDA direction that source plasma and the centres producing source plasma be licensed; the FDA would not inspect offshore sites which meant that imported plasma would not be approved plasma and therefore could no longer be used in the manufacture of blood products.[2129] As a result, since approximately 1978, all plasma used for the production of concentrates in the United States has been obtained from donors in the United States.” [2130]
Second, and as is discussed elsewhere in this Report,[2131] the World Health Organization published Resolution 28.72 in May 1975.[2132] The preamble noted “the extensive and increasing activities of private firms in trying to establish commercial blood collection and plasmapheresis projects in developing countries,”and identified three concerns. First, such activities “may interfere”with efforts to obtain national, non-remunerated self-sufficiency in the affected country. Second, there was a “higher risk of transmitting diseases when blood products have been obtained from paid rather than from voluntary donors”. Third, there were harmful consequences on the health of donors as a result of too-frequent donations, a potential consequence of payment. The Resolution urged Member States to promote national self-sufficiency on the basis of voluntary donations and to “enact effective legislation governing the operation of blood services and to take other actions necessary to protect and promote the health of blood donors and of recipients of blood and blood products.”[2133]Read in the context of the whole Resolution, the latter provision can be seen as a call for governments to enact domestic laws and regulations to prevent exploitative practices in the international plasma trade.
Elsewhere in his statement, Dr Kingdon dated the inspection regime to approximately 1975, and commented that, “In any event, it is unlikely that the industrial manufacturers [in the US] would have continued to use imported plasma in the manufacture of concentrates for any significant period; much of the imported plasma was infected with HBV and was therefore unable to be used to manufacture concentrates.”[2134] The US Institute of Medicine committee (discussed later in this chapter) had the advantage of hearing from a number of witnesses much closer to the time[2135] and dated the inspection regime to 1977.[2136]
This gives rise to four observations, even having regard to the important caveat that this statement was not finalised. First, during the early 1970s – including a time when screening tests for Hepatitis B were relatively insensitive – some US manufacturers were using imported plasma, much of which was likely to be infected with Hepatitis B, in factor concentrates. While testing improved and became compulsory, it was still not perfect and hence using a source of plasma with higher levels of Hepatitis B is likely to have increased the risk of viral infection of some blood products (including Factor 8 and 9 products), seemingly until 1978. Second, and as is discussed elsewhere in this Report, there is a correlation between a donor having Hepatitis B and the likelihood of their having other viruses. Third, the length of time between the introduction of the FDA inspections (approximately 1977) and the point by which all plasma used for the production of concentrates in the US came from domestic donors (approximately 1979) provides a further example of the time lag between the introduction of a protective measure and the (full) beneficial effect working its way to patients.
Dr Kingdon did not explain the reasons for this time lag and – keeping in mind that the statement was not finalised – caution should be exercised in drawing judgements from it. However, even allowing for the exhaustion of stockpiles and the manufacturing process this seems a long time, particularly as Dr Kingdon also explained that a manufactured product might have a shelf life of two years.[2137] It follows that it could take another two years for the product to be supplied for use in a patient. Taken together, this suggests that concentrates derived from plasma imported into the US and manufactured in 1978 might still have been in use as late as 1980.
Fourth, Dr Kingdon’s statement refers to the importance of the FDA, and inspection by the FDA of blood and plasma centres, in changing practices in the plasma industry.[2138] As is discussed in more detail below, the evidence the Inquiry has heard is mixed on how rigorous and effective the regulatory regime in the US was. Professor Sir Michael Rawlins of the Committee for the Safety of Medicines was complimentary in his oral evidence to this Inquiry.[2139] However, this view does not sit easily with such snapshots as the Inquiry has of actual practice in 7,000 blood and plasma centres in the land[2140] and with what was said nearly 30 years ago, by the Krever Commission of Inquiry on the Blood System in Canada, which considered (again, much closer in time) much of the US history of blood products for haemophilia therapy. The Krever Report noted gaps in protection. For instance, licences were not required and nor were inspections conducted by the FDA for most of the US blood centres that sold recovered plasma to fractionators. Thus it was possible for commercial concentrates manufactured in the US to contain material which came from sources which had neither been licensed nor inspected.
A somewhat less favourable view than Dr Kingdon took of the extent to which reliance could be placed on the success of the FDA’s processes in ensuring compliance was expressed by Dr Duncan Thomas. He was a senior medical officer on the secretariat of the Committee on Safety of Medicines Sub-Committee on Biological Products (“CSM(B)”) between 1971 and 1974 (therefore during a period when the first licences for commercial distribution of Factor 8 were granted) and as such had a role in advising the CSM(B) whether it should recommend granting a licence. In his evidence he said:
“We would liaise closely with the FDA but this was not a rubber-stamping exercise. We still checked every application carefully and we would not be influenced or swayed by licensing within another jurisdiction. From my perspective, I recall that occasionally we were reluctant to accept evidence from the Americans where they said a product had already been licensed for a few years without causing problems and that we should take this into account. We would look at all the evidence carefully but we were not influenced by other jurisdictions’ licensing processes or decisions.”[2141]
Over 20 years after the first blood products were licensed for distribution in the UK, a committee to study HIV transmission through blood and blood products was set up in the US by the Institute of Medicine at the request of the Secretary of Health and Human Services. A number of the leading experts in various disciplines throughout the country undertook a two-year study and reported in July 1995. Their report was critical of the FDA in the way it had managed regulation of blood and blood products in the early 1980s, in particular identifying that it had failed to take a proactive approach to regulation and had relied too heavily on the pharmaceutical industry. It noted that there was evidence that the agency did not adequately use its regulatory authority.[2142] The FDA had a Blood Products Advisory Committee (“BPAC”) which, though it contained members drawn from a variety of scientific disciplines, in the 1980s had a substantial membership drawn from those involved in blood banks and fractionators – representatives of the very bodies that were potentially subject to regulation – despite the obvious conflict of interests created by the extent of this representation.[2143] Though it is not unusual for regulators to constitute bodies that allow for representation from the industries that are being regulated, the point in the Institute of Medicine report was that the BPAC was too weighted towards the blood and fractionation companies, not that their presence alone represented a conflict of interest.
The views of the committee are consistent with individual experiences, as will be described, both from investigative journalists and film-makers and from comments relayed at second hand.
In the UK, and as is discussed in the chapter on Regulation of Commercial Factor Concentrates, the licensing authority could and did require manufacturers to state the source of their plasma in their licences. A ministerial submission from January 1976, relating to the product licence application for Factorate, set out what was known at that time about the sources of plasma for Factor 8 concentrates that were used in the UK, including whether the Medicines Inspectorate had visited facilities:[2144]
| Product / Company | Licence | Country/Agency for Blood Collection | Medicines Inspectorate Visits |
|---|---|---|---|
| Profilate (Abbott) | 22 May 1975 | United Biologics Donor Centres, all in the US[2145] | Visit to manufacturing premises and collection centre by DHSS in May 1975. |
| Koate (Cutter) | Under consideration[2146] | Various Agencies in the US and Mexico | Visit to manufacturing premises and collection centre by DHSS in 1972. Manufacturing premises visited by National Institute for Biological Standards and Control. |
| Kryobulin (Immuno) | 23 March 1973 | Manufacturer’s own centres – 5 in Austria and 2 in West Germany. Under contract from centres in the US.[2147] | Austrian Inspectors under Pharmaceutical Convention May 1973. Informal visit to manufacturing premises and blood centre by DHSS in June 1973. |
| Hemofil (Hyland) | 19 February 1973 | Hyland Laboratories’ centres in the US and Travenol International Centres in South America. | Visit to manufacturing premises and blood centre by DHSS on 24 October 1972. |
The ministerial submission recorded that Armour’s application was for products to be manufactured from “blood collection clinics licensed by the [FDA] and by non-licensed clinics (that is to say, clinics outside the USA).” It invited the Minister, Dr David Owen, to make it a requirement of the licence that plasma should be obtained only from donor centres in the US or other specified countries that satisfied the licensing authorities.[2148] That recommendation was followed in the product licence.[2149] Armour itself had undertaken that plasma “will be only from donor centres in the USA, and from USA sources.”[2150]It is not clear what this comment meant. Certainly it allowed for Armour to purchase plasma from US companies in order to supplement the supply it obtained from its affiliate plasmapheresis organisation, Plasma Alliance. Robert Christie, director of clinical studies at the UK subsidiary of Armour from 1975 to 1986, told this Inquiry that Plasma Alliance located its centres in the midwest of the US and complied with FDA regulations and directives. However, he also stated that he understood “that Armour US purchased small amounts of plasma necessary to address shortages. I do not know the details of any such purchases.”[2151]Nor does the Inquiry. It remains unclear whether the UK licensing authority had any greater knowledge, a matter that is discussed further in the chapter on Regulation of Commercial Factor Concentrates. By 1978, when Armour applied for a product licence for a high potency variant of Factorate, the company stated that all plasma was collected from establishments licensed by the FDA “and transferred to Armour under conditions defined”in the Code of Federal Regulations.[2152] The company had not achieved self-sufficiency in plasma by 1980,[2153] though it was able to state publicly the following year that all of its source plasma was collected from FDA regulated centres on the US mainland.[2154] It appears that self-sufficiency, at least for Factorate, had been achieved by June 1983.[2155]
The ministerial submission, the work of Douglas Starr and draft statement of Dr Kingdon are consistent with an account given by Dr Thomas Cleghorn, then Director of the North London Blood Transfusion Centre, to the investigative reporter Michael Gillard about the early provision of Hemofil. According to Michael Gillard’s notes of the interview, Dr Cleghorn was told by a representative of Hyland that plasma for initial supplies of the product came from Puerto Rico.[2156] He had also been told that from November 1975 only plasma from the mainland US would be used.[2157]
The Inquiry has seen evidence of other reports[2158] of sources of plasma outside the US or Europe being used in the production of factor concentrates. In a memorandum dated 17 September 1979, Dr Peter Jones recorded a conversation with two representatives from the Revlon Health Care Group, which then owned Armour. According to Dr Jones’ note, he was told that “one third of plasma supplies to Travenol is from Betise [Belize] and Lesoto [Lesotho],” and that Kryobulin Red, which purported to contain European plasma in fact contained plasma bought from the US.[2159] The latter claim is rejected by Peter Coombes, formerly of Immuno Limited, in his statement to the Inquiry. Peter Coombes says that he was aware of this rumour and received categorical confirmation from the joint managing director of Immuno AG that only European source plasma was used in Kryobulin Red.[2160] The claim that Lesotho (with Belize) provided a third of Travenol’s plasma in 1979 is open to the challenge that internal Travenol documentation records that their sole plant in Lesotho closed in 1976.[2161] However, there is evidence from other Travenol documentation that plasma from those countries was still being “routinely” used in the production of albumin products at its facility in Lessines, Belgium in 1979, that those products were imported to the UK, and that if this became known to the licensing authority it would be prohibited.[2162] It is not possible at this point in time to ascertain whether other such rumours or second-hand reports contained any elements of truth, not least as commercially obtained plasma was used in products that were reserved for non-UK markets.
More concerning still is the written statement of Ed Harriman. As an investigative journalist he researched the blood business in Nicaragua and Belize. He had been led to go there when, researching for a World in Action programme, he followed up reports that a company called Plasmaferesis, in which President Somoza and his family had been involved, had been buying blood cheaply from poor and desperate Nicaraguans in order to send it to Europe and the US for huge profits. The story had been broken by a local newspaper, La Prensa, in a series dubbed the “Vampire Chronicles”. The “homeless, drunks and poor people” went every morning to sell half a litre of blood for 35 (Nicaraguan) cordobas (by 2016, worth about £1). According to Douglas Starr, during the 1970s Nicaragua was “the developing world’s largest plasma collector”, taking blood from up to 1,000 people per day at its peak. The assassination of the newspaper editor provoked riots which ultimately led to the overthrow of President Somoza, although he had blamed Dr Pedro Ramos, the chief owner of Plasmaferesis, for the killing. Ed Harriman spoke to the editor’s widow and family to find out to whom Plasmaferesis had sold and exported the plasma, and what had happened to the company. He was told that the only country to welcome it was Belize: so that was why Ed Harriman next went there. He discovered the blood business. Down the road was a bar/cafe for which donors would receive a chip for food from the blood business: many were drunk and on drugs. The picture he paints is depressing and disturbing. Though he had arranged to speak to a local surgeon about what was going on, when he turned up to the appointment he was told no-one would speak to him; he was told that evening at his hotel that he should take the first plane out the following morning – which he took as a warning, so that is what he did. However, he was able to speak by phone to Dr Ramos who said he did a good business, selling blood to the US, Europe and the UK, though he gave no specific names for the buyers in the UK.[2163]
This account was of late 1979.
He wrote about his Belize experience in the New Scientist in 1980 in an article in which he described how he was told that one of the buyers of the plasma was Travenol (in Europe) for use in Factor 8 (amongst other products).[2164]
There is no reason to doubt what he described as seeing for himself. It is clear that a brisk business was being done obtaining cheap plasma from the riskiest of sources, for onward sale, though he did not see for himself any evidence of to whom that sale was being made.[2165]
The chance of those facilities (or for that matter those he understood to have been in Nicaragua) being inspected and regulated by the FDA is laughable. The Inquiry cannot, of course, say where the plasma ended up, or whether it was incorporated into plasma products.
The information provided to the licensing authority, which formed the basis of the ministerial submission discussed above, was obtained from documents submitted during product licence applications. What it did not tell the DHSS, and does not tell us, is whether sources of plasma that were used in unlicensed factor concentrates provided on a named-patient basis differed from those used in licensed products. It is not possible now to establish what was known by UK authorities and doctors at that time about those plasma sources.
By the mid 1980s the position had changed. In June 1983 the DHSS collated the responses of pharmaceutical companies to a series of questions about their plasma supply. Armour, Alpha (who were by then producing Profilate), Travenol/Hyland, Miles/Cutter and Immuno all confirmed that their plasma came from plants that were licensed by the FDA and that the origins of their plasma were identifiable.[2166] Lists of plasmapheresis centres compiled as part of applications for product licences by Cutter (February 1983) and Travenol (October 1983) record plasma centres located solely within the US.[2167] Profilate had always been produced from US-only plasma.[2168]
At a meeting of fractionators, officials and clinicians convened at the UK National Institute for Biological Standards and Control in February 1984, Dr Newt Ashworth, vice president of Scientific Affairs at Cutter, (describing the situation across the industry, not just Cutter) stated that there were some 340 plasmapheresis stations in 42 states, employing 6,000 people. Approximately one third of these were owned by the fractionation companies, with the rest of the plasma being supplied under contract. All plasmapheresis centres in the US were licensed by the FDA. He also referred to a single centre in Belize, which was also licensed (and hence should have been inspected) by the FDA.[2169] However, this is difficult to reconcile with the aforementioned list given to the UK regulator of the sources of plasma for blood products to be supplied in the UK – unless, of course, care was taken to segregate plasma from Belize from plasma from the US for use in products for different markets. The Inquiry however does not know why plasma should be obtained and transported from Belize to the US if it were not then to be used there in production of any product for which plasma was the base material.
Two broad narratives have emerged at the Inquiry of the rigour and effectiveness of regulation and inspection of plasmapheresis centres in the US. They are not mutually exclusive.
The first narrative is that of those who attended some plasmapheresis centres during the 1970s. Dr Thomas of the DHSS reported on a visit in 1972 to what was described as a “commercial blood bank” in downtown Los Angeles that was owned and operated by Hyland:
“The donors were all men, mostly middle-aged, and predominantly of Mexican origin. They were euphemistically described to me as ‘people who need $5,’ which is the amount they were paid for each donation of blood. From what I saw, they were certainly not affluent, although they could not fairly be described as down-and-out alcoholics ... However, the medical screening of the donors was rudimentary: a microhaematocrit determination of ear lobe capillary blood, blood pressure and temperature and that was about all ... In conclusion, obviously the main problem with this product is the hepatitis hazard. The donors do not inspire confidence” [2170]
Two years later, the ITV World in Action documentary “Blood Money” filmed and investigated Hyland plasmapheresis centres in Baltimore, Baton Rouge and California. They noted the location of the centres in areas of social deprivation and identified donors drinking alcohol immediately before donations, contrary to what were described as “Government rules.” In an interview one donor in San Jose explained that he was unemployed, on parole and was making the donation because he needed the money. When asked if he answered the questions asked at the centre honestly, he said: “No, you know ... yes, most of the time.”When asked which he did not answer truthfully, he referred to questions about drinking and diet. The journalist, Michael Gillard, said that from talking to donors he had found that it was not unusual for them to lie about their health. One interviewee stated that most of his fellow donors were alcoholics. A plasma centre manager accepted that he was sure that some alcoholics made it through his screening procedures and that there was a “fairly high” possibility that drug addicts did as well. By offering to sell plasma in five Hyland centres, Michael Gillard’s team found that no checks were made on the false addresses that they gave, the doctors did not always carry out checks intended to identify drug use, physical examinations were not always done fully but were certified as such, and that some medical questions were not asked but were filled in as having been answered satisfactorily.[2171]
Michael Gillard’s team were accompanied for at least two of their visits by Professor Arie Zuckerman of University College, London, a virologist and expert in hepatitis. In his view, most of the donors he saw would have been rejected by the UK blood transfusion services.[2172] Douglas Starr quoted Professor Zuckerman as describing a Hyland facility in Los Angeles as “an offense to human dignity”.[2173]
The second narrative is a picture of a strict, methodical and effective system. An example comes from the evidence to this Inquiry of Dr Brendon Gray, UK medical director at Bayer plc from 2019 to 2021 and subsequently vice president, head of Pharmacovigilance Regions at Bayer AG.[2174] As those dates suggest, Dr Gray was not personally involved in the manufacture of plasma products in the 1970s and 1980s, and was instead giving evidence based on materials seen by him. His evidence concerned the operations of Cutter in the period relevant to this Report.
Dr Gray set out the regulatory requirements of the FDA from 1973 and Cutter’s own procedures.[2175] By 1976 a manufacturer wishing to obtain a product licence had to comply with the system for regulation published in the Federal Register in 1973.[2176] A 25-page FDA instruction booklet from 1981 sets out in detail the matters to be inspected, including the requirements for medical supervision, donor identification and consent, the medical examination of donors, the process of obtaining plasma, record keeping, plasma separation and pooling following donations, the equipment used for plasmapheresis, the reinfusion of red blood cells, general facilities, testing for Hepatitis B surface antigen (whether or not performed on the premises), testing for syphilis, product labelling, storage, and distribution. The booklet stressed that inspection involved both observation and the examination of records.[2177] Dr Gray stated that inspections were carried out by both federal and state authorities and were done without forewarning. Violations could result in corrective action memos and, in the case of gross violations, the FDA had the power to shut down a plasma centre.[2178]
Dr Gray described the internal protocols developed by Cutter from 1976, which provided a “step-by-step plasma collection procedure for procuring plasma ... in order to apply the FDA’s Code of Federal Regulations and good manufacturing practices. [These] were official licensing documents required, reviewed and approved by the FDA.” They were revised over time as regulations and science evolved and any breach amounted to a breach of the plasma centre’s licence to operate. The centres – both Cutter’s own centres and contracted centres – were inspected by Cutter’s internal plasma procurement department, as well as the FDA and state authorities.[2179] The UK authorities were provided with quality assurance plans as part of product licence applications.[2180] As the Inquiry has heard, other companies had similar procedures in place.[2181]
Dr Gray’s account of a rigorous system on paper (he cannot speak from first-hand as to practice), finds some support in a report from a UK clinician, Dr Jones of the Newcastle Haemophilia Centre, who used substantial quantities of Armour product in his practice. A visit by him in 1980 to inspect and report on facilities supplying Armour with plasma through its subsidiary company, Plasma Alliance, was organised and facilitated by Armour. Dr Jones inspected five of the company’s twenty-two plasmapheresis centres and was impressed by what he found. He considered that “In all cases all operating procedures were strictly observed”and praised the “exceptionally high”standards of the donor room staff. He did identify concerns, notably some inconsistency in the detail in which screening was undertaken and a failure by some centres to ensure that a physician was present on site at all times; those centres relied instead on arrangements with local hospitals, something that Dr Jones considered to be contrary to FDA requirements. However, overall he commended Plasma Alliance as a “first class organisation with a sound commitment to quality control.”[2182]Since his visits were organised and facilitated by Armour there was a risk of his being given only selective access: however, his positive assessment is echoed in an internal report of inspections produced in 1983, which also commented on the “excellent” track record “recently” in federal inspections of Plasma Alliance.[2183]
This evidence might suggest that regulation and inspection of plasmapheresis centres in the US improved and became significantly more organised and rigorous over time in the 1970s and 1980s. However, caution must be exercised when considering the extent to which the policies, protocols and inspection documents were reflected in the practices in all centres. A memorandum dated 7 May 1982 from Robert Spiller, associate chief counsel for enforcement of the Department of Health and Human Services, criticised the Bureau of Biologics’ “long-established” practice of giving advance notice before some inspections. Robert Spiller wrote that he was “startled”to discover this practice and pointed out the obvious dangers of concealment and superficial, transient improvement to which it gave rise. He urged that the policy be changed and pointed out that of the five past or potential criminal prosecutions of which he was aware, none was first detected as a serious violator as a result of an inspection; all were brought to the attention of the enforcement authorities through “employee-informants or media reporting.”[2184]
Further, it remained the case that payment for plasmapheresis was likely to attract those who most needed the money. In his 1990 statement, Dr Kingdon stated that plasma collection centres tended to be located “near areas where there is likely to be a population willing to spend 2-3 hours donating plasma for a small payment,” such as near universities, army bases and “in the lower socio-economic sections of a city.”[2185] William Hartin of Alpha stated in a deposition of 24 April 1989 that: “When you’re dealing with paid donors the likelihood of people from the lower socioeconomic bracket becoming donors is much greater than from the higher socioeconomic bracket. And so, yes, to locate out centers in areas where ... the income is lower is important.”[2186] This inevitably gave rise to an economic incentive to answer questions in a way that would allow the donation to proceed.
The fact is that there may often be a gulf between the policies which an organisation has in place and what actually happens in practice. A degree of realistic scepticism is justified when reviewing the effectiveness of regulations and protocols; assertions that they are observed to the letter rarely accord with the common experience of life.
It is clear from evidence before the Inquiry that both Hyland and Cutter obtained plasma from plasmapheresis centres located in prisons in the US and used that plasma in the production of factor concentrates. Contemporaneous documents record that it was estimated that prison plasma accounted for approximately 2% of the total plasma collected in the US as of mid 1982 and was obtained from no more than six to eight centres.[2187]
In respect of Hyland, a document dated 20 October 1983 recorded that, following discussion with Dr Dennis Donohue from the FDA’s Division of Blood and Blood Products, the company had “decided that we will promptly discontinue the use of such plasma for the manufacture of coagulation factors.” As of the time of writing, prison plasma remained in “pools in process” and hence the decision would take effect from the end of that week. The context was concern about the transmission of AIDS through blood products. The Hyland document states expressly that: “Any intermediate fractions manufactured from plasma pooled this week, or in previous weeks, would be processed to final product.”[2188] The shelf-life for such a product could, on Dr Kingdon’s evidence, be two years.[2189]
It is not evident from the face of these documents which products were manufactured by Hyland using prison plasma, nor for which markets they were intended. However, there is no suggestion that prison plasma was intentionally excluded from certain products or markets. It has not been suggested at this Inquiry that Travenol took any steps to ensure that prison plasma was not used in blood products that were imported into and used in the UK.
Cutter collected plasma in plasmapheresis centres in either two or three prisons located in Arizona and Nevada.[2190] An internal memorandum from June 1982 recommended accepting an invitation from the warden of Arizona State Prison to establish a plasmapheresis centre there as it represented a “great opportunity for us to produce some low cost plasma.”[2191] Three prison centres were included in a list of plasma sources in a document dated 8 February 1983 that was compiled as part of a UK product licence application for Koate.[2192] Their inclusion on this list strongly suggests that plasma from the prisons had been used prior to February 1983 in the manufacture of blood products that were licensed for use, and were used in the UK until, as described below, Cutter stopped releasing Koate made from prison plasma.
On 4 January 1983 an open meeting was held in Atlanta, attended by representatives of Cutter and other plasma companies, officials from the FDA, the Centers for Disease Control (“CDC”) and other agencies, and interested groups and individuals. Following the meeting, Dr John Hink of Cutter prepared an internal minute that recommended, among other things, that no action be taken to close or limit Cutter’s plasmapheresis centres in prison beyond a public education campaign to discourage high risk donors to exclude themselves. Dr Hink recorded that there were two prison centres then used by Cutter that produced 3,000 litres of plasma per month. It is not clear why there is a discrepancy between the two centres cited by Dr Hink and the three contained in the list provided to the UK licensing authority. Dr Hink argued that “there are no data to support the emotional arguments that prison plasma collected from adequately screened prisoners is ‘bad’.”[2193]
Notwithstanding Dr Hink’s minute, the following month, February 1983, it was decided that the company would no longer release Koate from prison plasma.[2194] A document dated 28 February 1983 confirms that, by that date, the use of prison plasma in factor concentrates had been discontinued. The amendment to the internal protocol document recorded that the reason for the change was “a potential safety measure regarding AIDS.”[2195]
While Dr Gray pointed out in his statement that the FDA’s licensing and inspection requirements applied to plasmapheresis centres in prison as they did elsewhere, he also acknowledged that a meeting was held in July 1982 with the US authorities during which the potential for prison plasma to contain the causative agent in AIDS was discussed, and that by December the FDA was seeking agreement from Cutter and other fractionators to exclude plasma from prisons.[2196] Moreover, the evidence that licensing and inspection requirements applied to prison centres is not evidence that these requirements were always faithfully observed. Evidence from inmates[2197],[2198] involved in prison plasmapheresis programmes, given in depositions in later litigation, describes practices which showed a wholesale disregard for the requirements of the FDA: no proper physical examinations;[2199] questionnaires pre-filled by inmates working in the plasmapheresis centres that were not checked by the donor;[2200] plasma given by a donor who had been tattooed in prison, had used intravenous drugs from the age of 13 and had a history of Hepatitis B infection and meningitis;[2201] and a failure to ask about intravenous drug use before donations.[2202] If this evidence is well-founded it shows that FDA regulations and recommendations were observed more in the breach than in practice in at least some instances.
The investigative film-maker, Kelly Duda, explored much of the evidence relating to prisons in Arkansas. He has given evidence to the Inquiry that many inmates told him of the extent of subterfuge that was practised in order to enable them to earn a few dollars by selling their plasma.[2203] Though the prisons were inspected by the FDA (annually, though only once every two years after 1983) and the Arkansas Department of Correction (“ADC”) had its licence to provide plasma revoked on 17 May 1984, the plasmapheresis programme continued much as before after a week, though now run by Arkansas Blood Components (“ABC”) instead of ADC. The plasma was sold through brokers, in particular North American Biologics which was bought by Continental Pharma.[2204] Kelly Duda also describes finding a connection, traceable through the available records, with Pete Longstaff, a man with haemophilia who died of his infections, who in 1980 had been given several vials of a Cutter product (batch NC8196) which “was made with the plasma of 297 inmates from Arkansas”.[2205] This provides some evidence that Cutter had been supplied not only from the prisons it listed in 1983, as set out above, but also from Arkansas.
There were advantages to plasma collected in prisons for other blood products. Prisons were a “major source of hyperimmunised donors,” whose high titre plasma could be used to manufacture gammaglobulin products such as hepatitis, rabies and tetanus immune globulins. It was because, as a cohort, prisoners had been exposed to unusually high levels of pathogens that their plasma was important to those manufacturing blood products.[2206] Yet this also made them “high risk donors”.
The risks associated with this plasma were recognised at that time. When the issue of hyperimmunised donors was raised with Dr Donohue of the FDA in December 1982 he suggested that the plasma could be excluded from factor concentrates. Dr Donohue also expressly referred to the “homosexual link”in prison plasma and responded to the observation that there had been no cases of AIDS reported from prisons by arguing that “insufficient time had transpired” in light of the aetiology of the disease.[2207] Armour – a company known for its competitive pricing strategy – did not use prison plasma at that time and showed no interest in suggestions made in April 1985 that the use of screening tests and heat treatment might permit a return to the use of prison plasma in factor concentrates.[2208] In a letter to the FDA from 9 November 1982, which is discussed further below, Alpha’s president, Thomas Drees, wrote that his company’s position was that: “We ... think that plasma from prisons should be avoided.”[2209] The following month, Alpha’s US medical director wrote to US haemophilia centres saying, among other matters, that: “We do not operate prison donor centers which have a large high risk population, nor do we purchase plasma from prisons.”[2210]
Nor should it be thought that criticism of the use of prison plasma did not emerge until the 1980s. Dr Edward Shanbrom worked for Hyland as medical director and director of research between approximately 1965 and 1975. In a deposition that he gave on 30 October 2002 in the course of litigation in the US he stated that he objected to Hyland’s use of plasma from the Angola Prison in Louisiana on the basis of the hepatitis risk at that prison. He stated that he “very strongly” expressed his objections to the president of the company, Fred Marquart, and his successor, Norm Achen. The exchange went like this:
“Q: What were their reactions to your objections?
A: I was fired.
Q: Okay. So would it be fair to say in that part of the -- of the collection of things that led to your termination, involved your objections about using prison plasma from Angola Prison?
A: I’d like to think so, but I don’t really know.” [2211]
By way of comment, it would be naive to think that prisons were not a high-risk source to use to procure plasma. It would be naive to suppose that in a system in which people could make some money selling their own plasma that many prisoners in the US would not go to considerable lengths to do it. It would also be unrealistic to expect a once-a-year inspection to expose the worst practices permitting this, or to close the loopholes that allowed it – especially when evidence suggests that prisons, as with other centres, might be forewarned of the date of an inspection visit.[2212] The focus of this Inquiry is on the safety of UK blood and blood products, and how it was that infections came to be transmitted through them. It is unnecessary therefore to pass any final judgement on the issues raised in respect of the US systems of collection from prison. It can nonetheless be said that clinicians, civil servants and ministers should not be naive, especially when it comes to blood safety. The DHSS should have understood, from the licensing process, the risks associated with plasma from prisoners in US blood products and this should have given greater urgency to the need to establish self-sufficiency, and underscores the dangers of reliance on all being done exactly as it should be done because there is a system of regulation in a foreign country.
There was a market for antibodies to Hepatitis B, with which people could be vaccinated so that they were able to resist the virus. The strength of this market led to pharmaceutical companies seeking plasma which was rich in such antibodies – essentially because the people from whom that plasma was obtained had been significantly exposed to the virus, and had developed an immunity to it. The UK blood services were clear that people who had been infected with Hepatitis B should be excluded from donating blood (or plasma) – the only issue, domestically, was whether this should exclude the donor for all time or whether after a year without symptoms they should be cleared to donate again.[2213] However, far from rejecting such donors US pharmaceutical companies actively sought them out – the purpose was to use the plasma as a source of immunoglobulins in the manufacture of vaccines.[2214]
Prisoners often had high levels of antibodies to Hepatitis B in their blood – it was thus said to be “high titre”. They were not the only donors sought out by plasma companies. Advertisements were published as part of efforts to recruit gay men to give blood in order to obtain “hyperimmunised plasma” (that is, plasma with a high titre of antibodies).[2215]
Two examples of these advertisements follow:
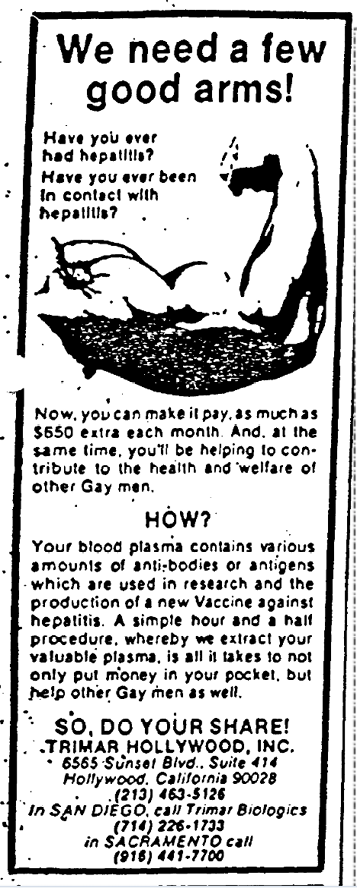
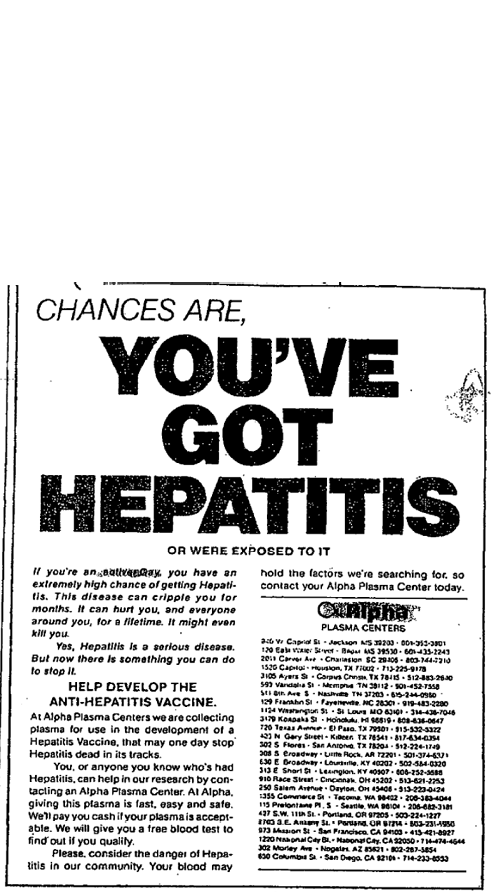
Whilst there were good reasons for seeking hyperimmunised plasma for the production of vaccines, these advertisements give reason for concern.
First, the date of Figure 1 is 13 May 1982. It had been known for nearly a year by then that gay men in particular were at risk of developing a failure of the immune system, which was indeed called GRIDS (Gay Related Immunodeficiency Syndrome).[2218] It was known within at least two of the pharmaceutical companies to be a possibility that it was transmissible through blood.[2219] Yet at one and the same time gay men were being recruited so that components of their blood might be injected into others.
Second, it was known by the start of 1982 if not earlier that non-A non-B Hepatitis might be associated with Hepatitis B infection.[2220] Non-A non-B Hepatitis could not be tested for specifically at the time: but it was estimated that as much as a third of such infections could be avoided if blood rich in anti-HBc was excluded from use in transfusions.[2221] Though it could be useful in producing immunoglobulins and a vaccine against hepatitis B,[2222] it thus became at best an uncertain base material for therapeutic products for human use in treating bleeding disorders, and at worst dangerous for any pooled product not virally inactivated.
A third matter was that plasma from these sources which had been left over from the production of immunoglobulins was then used to make factor concentrates. This is more a matter for alarm than just concern.
Figure 2 above is from Alpha and though the wording is not very distinct, it begins “If you’re an active Gay ... now there is something you can do [to help to stop Hepatitis]”. It lists Alpha plasma centres, most in downtown urban areas, which were to buy the plasma.[2223] Evidence before the Inquiry suggests that Hyland also targeted gay men for whole blood donations for the purpose of obtaining hyperimmunised plasma;[2224] while it did not use plasma recovered following this process for its own factor concentrates it did sell this on to Alpha, and Alpha then used that plasma as part of its pools when manufacturing factor concentrates.[2225] The risks of non-A non-B Hepatitis being transmitted by this means are plain. It probably followed that material which would be excluded from any production of concentrate in the UK because of the high risk it posed was included in the concentrates Alpha exported to the UK (there is no reason to think that the UK product would be any different in this respect from that distributed in the US).
The FDA knew this was happening but sought to persuade rather than enforce.[2226] The evidence that the FDA knew is that in August 1982, in response to the risk of AIDS, Dr Donohue of the FDA urged Hyland and other companies to refrain from using plasma to make factor concentrates where that plasma had been obtained from recruitment aimed at gay men. This indicates that he considered that it was happening.[2227] In December 1982 Dr Michael Rodell, vice president of Hyland, wrote to the National Hemophilia Foundation to state that: “Within the past several months, we have made a commitment to withhold from AHF [antihemophilic factor] manufacture any plasma obtained as a result of specific recruiting activities aimed at the gay community ... we no longer allow this plasma to enter those pools leading to AHF manufacture.”[2228] The wording of this letter indicates that Hyland had previously permitted the use of such plasma in concentrate manufacture. The letter did not specify when that decision had been made and said nothing of what would be done with high titre plasma that had already been collected and distributed to plasma pools. It did not say that products already under manufacture, or in storage awaiting distribution, were free either of prison plasma or from plasma obtained from areas where Hepatitis B was thought to be rife.
As for Alpha, it wrote to the FDA on 30 August 1982 to inform it that “until further notice Alpha Therapeutic Corporation will not be using the cryoprecipitated material from plasma from hepatitis B surface antibody donors in the manufacture of Anti-haemophilic Factor (Human). Such plasma is used by Alpha in the manufacture of Hepatitis B Immune Globulin (Human).”[2229]A later letter, dated 7 September 1982, referred to the 30 August correspondence as evidence that Alpha had “voluntarily suspended”that practice.[2230] The phrasing of both letters, taken with the evidence cited above, strongly suggests that Alpha had been using plasma obtained for the purposes of manufacturing Hepatitis B immunoglobulins in factor concentrates. However, in a letter to the National Hemophilia Foundation, Alpha’s president, Thomas Drees, expressly stated that: “While we have purchased some plasma collected from homosexuals for Hepatitis B Gamma and Vaccine, we have never used it to make AHF.”[2231] This comment is difficult to reconcile with the other evidence cited in this section.
Cutter’s practice is reflected in an internal memorandum also dated 30 August 1982. Dr Hink recorded that: “Until recently, Cutter’s anti-HBs plasma (all collected from centers dealing predominantly with homosexuals) has been used in the manufacture of coagulation products.” He stated his intention that remaining high titre plasma, dating from July 1982, would be processed in experimental products that would not be used for human use. A proposal would also be brought forward for Cutter to exclude voluntarily such plasma from the manufacture of Koate and Konyne, as Dr Donohue had requested. Dr Hink concluded: “I believe we must agree to a temporary exclusion for political, moral and liability reasons.”[2232]The temporary nature of the exclusion is demonstrated by an internal memo a few days later. Dr Lee Hershberger advised that Cutter had “placed a hold on this for one month ... [and that he] expected to obtain confirmation from management ... to continue the hold beyond the one-month period.”[2233]
It follows that, until September 1982, plasma obtained from “from centers dealing predominantly with homosexuals” was used to produce Koate and Konyne.[2234] There is no evidence that the Inquiry has identified to suggest that concentrates manufactured in this way were excluded from the UK market.
In his memorandum of 30 August, Dr Hink gave his view that Dr Donohue “is not basing this request on scientific concerns that such plasma or coagulation by-product transmits AIDS but believes that the action is a political necessity to prevent national adverse publicity and (at this time) undue concerns in the hemophilic population.”[2235] In his memo Dr Hershberger recorded that Dr Donohue “feels that the hold [ie suspension of use of such plasma] will not be necessary for more than two or three months unless more donors develop AIDS.”[2236]Other prominent individuals were less sanguine. The practice of using plasma intentionally obtained from gay donors in factor concentrates was strongly deprecated by Dr Don Francis of the CDC. In an expert report produced during US litigation he argued that the pharmaceutical companies:
“could not have selected a higher risk population for the transmission of AIDS than Hepatitis B positive urban homosexual men. These donors were infected with Hepatitis B in direct correlation to their number of sexual partners. Those at highest risk of Hepatitis B were also at highest risk for all other sexually transmitted diseases, including AIDS.
By the mid-1970s, it was well known to [plasma companies] and the scientific community that urban homosexual men had an exceptionally high prevalence of Hepatitis B ... By the same time it was also well known that a substantial portion of this population engaged in a lifestyle of sexual promiscuity involving multiple partners, which caused widespread sexually transmitted diseases, including not only Hepatitis B, but also Hepatitis C (then unidentified and described as ‘non-A non-B’ or ‘NANB’ hepatitis) cytomegalovirus (CMV), and Epstein Barr disease. Thus, the same conduct that made urban homosexual men valuable HBIG [Hepatitis B immunoglobulin] plasma donors caused multiple other diseases that made this population inappropriate donors for any other blood or plasma product.
Because of the exceptionally high prevalence of identified and unidentified, blood-borne and sexually transmitted diseases among urban homosexual men, peer-reviewed literature as of 1975 had recommended that such persons be advised not to donate blood. See Szmuness, Annals of Internal Medicine 1975[2237] ... The same rationale applies equally to donations of plasma, which would contain and transmit some of the same diseases.” [2238]
By way of comment, Dr Francis’ views are exactly right.[2239] The evidence shows that three of the four major US pharmaceutical producers of factor concentrates were involved in using plasma obtained specifically because the donors were at very high risk of having Hepatitis B to make those products. It shows that they did so until August or September 1982. Moreover, product made before that date would remain available for distribution and use for some two years after that, such that anyone taking Alpha or Cutter products before mid 1984 was put at increased risk (unless those products had been produced later or had been heat-treated, or were simply not released to market).
It is also clear that hepatitis would be likely in prison populations, both by the nature of the prison environment, and probably the social background of many inmates. It is notorious that illicit drug-taking is associated with criminality, and in turn that the unlawful use of drugs is widespread in prisons. For men in prison the only opportunity for sex is likely to be with other inmates, and probably unprotected. They too were undoubtedly a high risk group. It is highly likely that prison blood conveyed blood-borne disease; that it is likely to have contributed to the spread of hepatitis, both Hepatitis B and non-A non-B Hepatitis, amongst users of commercial concentrates, and that previously unidentified infections such as HIV were transmitted through this route.
The Licensing Authority in the UK would be aware of the sources of the products which had been declared as part of the licensing applications seeking permission for distribution in this country. Though there is evidence therefore that they knew that some plasma was sourced from US prisons (in the case of some manufacturers), there is nonetheless no evidence that the authorities were alert to the particular heightened risks that this posed. Nor is there evidence that the Licensing Authority or the DHSS more widely had been told of the use of hyperimmunised plasma, or at least that it too might end up being used in the manufacture of factor concentrates as well as vaccines for Hepatitis B. However, there is evidence – reviewed elsewhere in this Report – that records a recognition in the DHSS that product made from plasma collected in the US before March 1983 was of higher risk because “high risk” groups had not been excluded. This led to fears that it might be “dumped” on the UK market, at first causing concern, though then leading to an eventual acceptance that this should not be prevented because of fears of a shortage of supply of commercial concentrates.[2240]
The risk is underlined by one example. Dr Francis set it out like this:
“A memorandum prepared by Dr. Tabor of the FDA, Office of Biologics, describes an incident in August 1982, concerning a donor of plasma to the Valley Medical Center, a predominantly male homosexual plasma collection point, who had been diagnosed with Kaposi’s Sarcoma, one of the AIDS-defining conditions. Dr. Tabor’s memorandum of August 20, 1982, reported upon a meeting with Cutter representative C. Moore, indicating that the AIDS donor’s four plasma units had fortunately not been pooled by Cutter with other plasma because they had thawed during shipping, and due to temporary closure of a facility. However, Dr. Tabor’s memorandum continued:
‘under usual circumstances these units would have been processed by this time. The units would have been pooled with other units collected for use in Hepatitis B immunoglobulin (HBIG). The cryoprecipitate would have been removed and pooled with cryoprecipitates obtained from ordinary plasma pools; the remaining plasma would have been processed separately from ordinary plasma to produce Factor IX Complex ... as well as HBIG.’” [2241]
He went on to describe an internal company memo as saying:
“We were extremely fortunate that we were able to quarantine the 4 units of Source Plasma ... before they were pooled. Had they been pooled, the [FDA Bureau of Biologics “BoB”] might have found it politically expedient to make hard line decisions regarding the fate of the products made from the pool. This kind of risk will continue until there is solid data to prove that AIDS is not transmitted by blood products. Meanwhile we should try to help the BoB develop a rational policy of dealing with AIDS that will withstand political panic.”[2242]
I am unable to disagree with Dr Francis’ comment which then followed:
“These documents show that Cutter’s standard practice was to pool the plasma from urban homosexual men, collected for HBIG production, with normal plasma for Factor concentrate production. The finding of an AIDS patient who gave plasma at a predominantly homosexual center should have confirmed to Cutter that using such plasma for Factor concentrates was dangerous and improper.”[2243]
Dr Gray, in his statement given on behalf of Bayer plc, explained that from 1974 FDA regulations mandated large pools of at least 1,000 different donors for the manufacture of immunoglobulins to ensure the inclusion of a broad spectrum of antibodies. As the same pools were then used to make factor concentrates, those concentrates were derived from plasma from at least 1,000 donors.[2244]
The FDA regulation referred to the production of immunoglobulins, not the production of concentrates. Dr Gray did not suggest that it was impossible to establish processes to manufacture factor concentrates from pools containing fewer than 1,000 donations and immunoglobulins from larger pools, although this plainly would have been less efficient (using “efficiency” in the sense of producing a product, rather than producing the safest product). In the event, it seems that all commercial manufacturers concerned here used at least a 1,000-donor pool as the starting point for the manufacturing processes for both immunoglobulins and factor concentrates in the 1970s and 1980s.
It is important to keep in mind the different metrics that can be used to judge plasma pool sizes. First, there is the volume of the plasma, usually expressed in litres. Then there are the number of donations that go into the pool. This is often greater than the number of donors, on the basis that with regular plasmapheresis the same donor may contribute more than once to the same plasma pool. Finally, and confusingly, there are some references in the documents to the “pool of donors” from which a company derived its product, in other words the total number of people “on the books” to supply plasma in a given period.
It appears from the documents available to the Inquiry that of the US commercial fractionators, Armour’s pools were, over time, the smallest. In February 1976 the company stated in correspondence to the DHSS that “the number of donations is approximately 1,540 per batch to give a pooled plasma of approximately 1,000 litres.”[2245] This figure was used as part of the firm’s marketing, featuring prominently on the roundel used in correspondence with doctors.
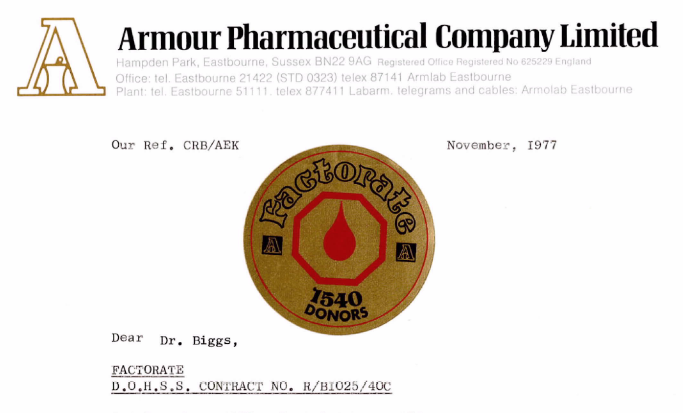
This fact on its own was an attempt to recruit sales because it suggested that Armour used smaller pools than its rivals, and smaller pools were an advantage. The obvious advantage was that it would expose any recipient to a lower risk of transmitted infections.
In oral evidence to this Inquiry the author of some of those letters, Christopher Bishop – who was then products and marketing manager at the UK subsidiary of Armour – stated that the company was “particularly proud of [that figure] because that compared with, you know, 20, 25,000 donations applicable to other products.” He agreed with the proposition that this reflected an understanding that the larger the pool size the greater the risk of viral transmission.[2247] Christopher Bishop’s evidence was that the pool size did not change over the 1970s and 1980s.[2248] His colleague Robert Christie, director of clinical sciences in the UK and later clinical and technical affairs director for Europe, also told the Inquiry that he could not recall any increase in pool size.[2249] An Armour publication from July 1981 referred to Factorate being manufactured from pools of “only approximately 2,000 donors.”[2250] It is not clear if this is a less precise formulation of the same idea, or whether it reflects an increase in the size of the plasma pools between the mid 1970s and 1981.
The same publication referred to the total number of donors providing plasma to Plasma Alliance, the plasma collection company affiliated with Armour: “Plasma Alliance’s 22 centres are responsible for collecting from approximately 22,000 donors registered at any one time.”[2251] Annually, over one million plasma donations were processed.[2252] It follows that a patient receiving a single infusion of Factorate in the later 1970s would be exposed to somewhere in the region of 1,540 donations. If that patient continued to receive Factorate that was not carefully selected by treating clinicians from the same batch, he or she would be exposed to thousands more donations, up to 22,000 Plasma Alliance donors (or more over time).
Dr Thomas referred to pools of 6,000 donors in his 1972 report on Hyland facilities, which was considered as part of the Hemofil product licence application.[2253] Figures provided by Travenol in support of a product licence application for Proplex, a Factor 9 product, in 1976 referred to a plasma pool size of approximately 6,000 litres; the number of donations was not specified, but would have been higher (on the basis that less than a litre of plasma was obtained at each donation).[2254] The size of pool used by Hyland/Travenol appears to have increased over time as, in his draft statement of 1990, Dr Kingdon referred to “start pool” sizes of up to 15,000 donations. He did not provide further details of when, how and why the pool size had changed.[2255]
Cutter
During its application for a product licence application for Koate, Cutter was asked to provide further information on its pool sizes. It did so in a letter dated 27 February 1976:
“Each pool consists of 2,500 litres of plasma. Each unit of Source Plasma (Human) is approximately 600 ml. Therefore, the pool would be comprised of approximately 4,000 units or more. Generally the plasma pool is such that it is comprised of approximately equal donations from at least 1,000 individual donors. A given lot of KoateTM is usually made up from material fractionated from 3 to 5 pools, i.e. the AHF suspension obtained from 3 to 5 separate plasma pools is combined in solution to form the final product.”[2256]
The figure of “at least 1,000 individual donors” per pool seems to reflect the FDA requirement for at least that number contributing to a start pool used for immunoglobulins. The wording used in the application allows for the probability that considerably more than 1,000 donors contributed to each 2,500-litre pool. Given the possibility that one donor might make more than one donation to the same pool it is not possible to state definitively to how many donors a patient using Koate would be exposed. However, the information provided by the company suggests that each lot at that time was produced from somewhere between 12,000 and 20,000 donations.
In November 1983, Cutter’s director of medical services, Dr George Akin, wrote to an American doctor concerning a donor who had been identified as having AIDS. In the course of the letter Dr Akin argued that the “enormous dilution”of this donor’s plasma made it “highly unlikely that transmission of AIDS to a recipient would occur.” In this context, Dr Akin was more willing to provide an estimate of the amount of donors involved: “Each AHF pool contains plasma from as many as 7,000 to 15,000 individuals.”[2257] It is not clear how this figure was reached, or whether it represented an increase in the pool sizes when compared to the situation in 1976. Three years later, in a letter to three British doctors providing more information on Profilate HT, Linda Frith, the sales development manager for the UK subsidiary of Cutter, used the earlier wording: “Koate HT is prepared from pooled human plasma from at least 1,000 healthy donors.”[2258] The same phrase was used in the Koate HT application for a renewal of the Koate HT product licence in November 1989.[2259] There is no evidence before the Inquiry, including from Dr Gray, that the plasma pools used to produce Koate and Koate HT reduced in size after Dr Akin’s letter of November 1983.[2260]
The Inquiry has less information about the pool sizes used by Abbott and then Alpha to produce Profilate, but a letter to The Lancet published on 28 September 1985 concerning a study on the heat-treated variant recorded that it was produced from plasma pools of “5,000 to 32,000 donors per batch”.[2261] No further information was given to explain the difference in the pool sizes.
The Inquiry also has limited evidence about the size of the plasma pools used by Immuno in the production of Kryobulin and its Factor 9 product, Prothromplex. A report by Dr Thomas in respect of the initial product licence application for the former recorded that the pool size was 1,000 donors between the ages of 18 and 65, whose plasma was obtained from centres in Austria and West Germany.[2262] The same figure of 1,000 donors appeared on a product label for Kryobulin Red (made with European plasma) in the mid 1970s,[2263] and on a draft product label for Prothromplex in November 1984.[2264] However, other labels – including the label provided with the original Kryobulin product licence application – do not give a figure.[2265] It is unclear whether this is because the size of the plasma pools increased over time.
In February 1984, a meeting was held at the National Institute for Biological Standards and Control (“NIBSC”) between civil servants, American and British fractionators, clinicians and scientists. Among the issues discussed was the size of donor pools. The draft minutes recorded that:
“it was pointed out that the pool sizes used by the commercial fractionators ranged from 1,000 to 10,000 litres of plasma, though sometimes pools were combined at the cryoprecipitate stage, giving a possible maximum of 20,000 litres of plasma equivalent. The average volume collected from plasmapheresis donors was 680 ml, with a minimum pool size of around 1,500 donors and maximum of around 30,000 donors. The maximum pool size used by NHS producers is 1,000 kg of [cryoprecipitate – corrected by hand to plasma], incorporating material from about 5,000 donors.”[2266]
These draft minutes, which were corrected on one point of detail but otherwise were not amended following correspondence with the attendees, reflect the evidence cited above. The minimum pool size – 1,000 litres and around 1,500 donors – may refer to the approach taken by Armour, and possibly also Immuno. A maximum of around 30,000 donors is broadly consistent with the figure given in The Lancet in 1985 for heat-treated Profilate produced by Alpha. Combined plasma pools containing 20,000 donations is consistent with the evidence concerning Cutter.
It follows that a single transfusion of a commercial factor concentrate during the 1970s and 1980s would expose a patient to plasma from at least 1,000 paid donors, and more probably from 10,000 or more. A patient who required regular treatment over an extended period of time would – depending on the practices of his or her doctors – face exposure to thousands and very possibly tens or even hundreds of thousands of paid donors.
The chance of a transfusion of a single-donor unit of blood transmitting serum hepatitis (whether Hepatitis B or C) or HIV was real, but small. The risk of transmission depended first upon the prevalence of transmissible infection amongst those who sold their blood or plasma. This varied from time to time, depending on the particular infection, and the degree of success there was with viral screening. In the case of Hepatitis B, for instance, tests were not sufficiently sensitive to detect every infected unit for over a decade after screening first became available;[2267] and, in the case of plasmapheresis centres, the degree of care that was taken with the screening process. Even for a recipient who had had, say, a thousand transfusions each of a single-donor unit, the risks of being infected by the next single unit would be no greater than the risk that the first unit would be infective. (It is a fallacy to think that the risk on each occasion a new transfusion is given is any different from the risk on the previous one, even though it is obvious that someone who has had a thousand separate donations will be more likely to be infected at some point during his treatments than a person who has had just one or two).
However, if a thousand donors contribute to a pool from which the single unit is taken, each of those thousand has to be free of transmissible infection if the pool is not to be infected. The larger the pool, the more likely this is.[2268]
From time to time, it has been wondered if the sheer size of a pool would have the effect of dilution, so that the infectious particles in a single dose which might be highly infective on its own would be so spread throughout the pool that none would be likely to cause infection. However, so far as hepatitis is concerned, that idea should have receded following the work by Roderick Murray in 1955.[2269] There was no information which would lead anyone to suppose that the AIDS virus did not behave in a similar way, and would not be diluted but would infect a whole batch. Indeed, that appears to be the basis on which, as discussed in more detail in the section of this chapter about the response to AIDS, Dr Rodell’s presentation in July 1983 suggested that, given the pool sizes used in the US, four infected persons could contaminate the entire world supply of Factor 8 concentrate.[2270]
This contribution at a public meeting is chilling in its implications. The issue he was addressing is whether, as a logical corollary of the measures which the FDA was recommending should be taken to protect against the risk of AIDS from blood products, batches of product produced from a pool to which a person known or suspected to be suffering from AIDS had contributed should be recalled for destruction. His point was that if a donor was subsequently found to have AIDS, and the product was recalled, the likelihood was that his donations “could easily be represented in as many as 50 plasma pools in one year ... 25 to 250 million AHF activity units could be affected, all in various stages of pooling, production, and distribution.” Given the amount of concentrate produced by the industry in a year, and the size of the pools, the minutes recorded that the potential for serious disruption of AHF supply as he described it “seems quite real.”[2271] His argument was one of extremes, a “Doomsday scenario”, for rhetorical effect: that to provide by regulation for there to be automatic recall would, because of just a few donors who had repeatedly donated, leave patients untreated and thus facing agonising pain, and putting those patients at risk of death if a cerebral bleed were left untreated. His thesis was thus that the need to go on supplying a product trumped the question of whether it was safe from the risk of causing AIDS. Recall was left at the discretion of the pharmaceutical industry, to be exercised on a “case-by-case” basis.[2272]
This demonstrates that two things had grown too large to be allowed to fail – the industry as a whole, on which so many people with bleeding disorders worldwide had come to depend and, of relevance to this section of the Report, the size of the pools that were used which had the effect that it had become impracticable to attempt to recall product.[2273]
When the evidence of pool sizes (no doubt chosen to become larger and larger in part at least because of the manufacturing efficiency this offered and the costs advantages that followed) is combined with a purchasing strategy of buying plasma from the cheapest sources,[2274] and the practice of using residual material from hyperimmune plasma to make concentrates,[2275] it is fair to say that commercial concentrates fully deserved the reputation they had had since the start of the 1970s as being riskier than domestic concentrates, and far riskier than single-donor cryoprecipitate. It is, sadly, unsurprising that they were a principal source of HIV infection in the UK.
As is discussed in the chapter on Regulation of Commercial Factor Concentrates, it was a requirement of a UK product licence that labels and information provided with the product would be approved by the licensing authority. The approved wording would then have to be used unless and until an application to amend the licence was accepted, again by the licensing authority. This resulted in a system that was slow to change product information because of the time, work and delay that would be involved.
There were three elements to the product information provided for factor concentrates. Most visible was the text used on the packets and labels for the products. The amount of information conveyed in this way was naturally limited by the space available and so a longer exposition was contained in the product leaflet that would be included as an insert in the package. The third element was the data sheet, which could be provided independently of the product, for example to clinicians who wished to know more about it. Data sheets were similar in length and detail to the product leaflet but were not necessarily identical. If they so wished, companies could voluntarily submit data sheets to a compendium produced (more or less) annually by the Association of British Pharmaceutical Industry (“ABPI”).[2276]
Other countries, notably the US, operated similar systems in respect of licensing product information.
Pharmaceutical companies therefore had a choice to make on how to organise their approaches to different jurisdictions.
Cutter
Dr Gray’s evidence was that Cutter/Bayer used the same text for identical products on the UK and US markets, modified only to reflect the name of the UK distributor and licence number.[2277] The Inquiry has, however, seen evidence that UK divergence was at least considered in the context of the September 1986 product licence application for Koate HS.[2278]
Immuno
Immuno employed a system of “Neutral texts” (wording that could be used in any countries where there was no requirement for a specific formulation, including for unlicensed products in the UK) and “UK specific texts” which had the approval of the UK licensing authority and had to be used for a licensed product.[2279]
Travenol/Baxter
According to Ronald Feakes of the UK subsidiary of Travenol/Baxter, the literature supplied with the company’s products was initially drafted in the US and was reviewed by the UK Regulatory Department to ensure compliance with the then current product licence requirements. The UK and US companies would liaise if any changes were required.[2280]
Armour
A similar approach to that of Travenol appears to have been adopted by the Armour companies operating in the US and UK.[2281]
Who decided what data to record?
This evidence suggests strongly that it was the parent companies that played the leading role in determining what appeared on the product labels and data sheets, but that it fell to the UK subsidiaries to ensure that this was compliant with UK regulatory requirements. This is unsurprising given that it was those subsidiaries that applied for and held the product licences for concentrates that were developed and manufactured elsewhere by far larger, multi-national companies with greater scientific and other resources.
The information was for doctors, not patients
The evidence of those pharmaceutical representatives involved in the licensing process in the 1970s and 1980s is that the product information was intended to be read by the clinicians responsible for prescribing the products, and was not intended for patients.
Linda Frith, who worked for Cutter UK in sales and marketing between 1984 and 1990, stated that throughout that time:
“there was no regulatory requirement for pharmaceutical companies to provide information directly to patients. As the Factor concentrates supplied by Cutter in the UK were available on prescription only, Cutter provided information to prescribers in relation to such products, including through the product information [that was approved by the UK licensing authority]. The treating clinicians could then discuss the products and the associated risks tailored to the medical condition and circumstances of the individual patient. Cutter did not participate in those discussions”[2282]
Christopher Bishop of the UK subsidiary of Armour told the Inquiry that the product literature was produced in the expectation that it would be read and considered by doctors rather than patients.[2283] His colleague, Robert Christie, stated that it would not have been ethical for Armour UK to have sought to communicate directly with patients about their treatment, that being a matter for patients to discuss with their haemophilia clinicians.[2284]
Peter Coombes of Immuno Ltd gave similar evidence.[2285]
Ronald Feakes of the UK subsidiary of Travenol/Baxter recorded in his statement that data sheets and product information were “principally directed towards clinicians and other healthcare professionals.”[2286] He did not provide further details of whether there was a secondary audience for this material, though he thought that patient information leaflets were only prepared much later, towards the end of the 1990s when required by legislation.[2287] The terms of some of the warnings and some internal documents also support the proposition that the material contained was directed to clinicians, not patients.[2288]
The terms of the warnings: Hepatitis
All the pharmaceutical companies told the UK Licensing Authority, at the time of licensing, that their products carried a risk of transmitting and thus causing hepatitis. It was not hidden. There was a contrast when it came to the risk of AIDS, when warnings were much less emphatic.
The product licence application for the product in November 1972 contained the following information in the proposed package leaflet:
“CAUTIONS ... This concentrate is prepared from large pools of fresh human plasma. Such plasma may contain the causative agents of viral hepatitis. There is no known laboratory test to demonstrate either the presence or the absence of such agents, and the concentrate has not been subjected to any treatment known to diminish the risk of transmission of hepatitis since such treatments greatly increase the loss of AHF activity during preparation. The concentrate should, therefore, be used when its expected effect is needed in spite of the unknown hepatitis risk associated with its use. Special consideration should be given to the use of the concentrate in newborns and infants where a higher morbidity and mortality may be associated with hepatitis.”[2289]
The labels on the bottles of Hemofil contained the warning: “The risk of transmitting hepatitis is present.”[2290] During consideration in 1973 of whether to license Hemofil, a report was produced as part of the licensing process by Dr Thomas of the Medicines Division. He commented that: “no attempt is made to disguise the risk of hepatitis, and it may be considered that the decision to use this material could be left to the individual clinician who can balance the potential hazard against the anticipated therapeutic benefit to the patient.”[2291]
The question of Hemofil-related hepatitis being caused in the UK was raised by reports into an outbreak of hepatitis in Bournemouth in 1974. A number of UK Haemophilia Centre Directors’ Organisation directors met at the Churchill Hotel in London on 10 June 1975 to discuss it with representatives of both the US parent company and Travenol UK; the meeting was arranged by Travenol. Dr Jones reported on it. He regarded the association between the outbreak and Hemofil as having “now been proved”.[2292]
The Hemofil hepatitis warning attracted criticism from Michael Gillard in the course of his investigation for World in Action on the basis that the warning was insufficiently strong. He spoke to the US Bureau of Biologics at the FDA. His criticism came to the ears of Dr Theodore Cooper, US Assistant Secretary of Health, who wrote to Dr Henry Yellowlees, the Chief Medical Officer for England shortly before Michael Gillard’s documentary was broadcast. He wrote asking for details of the lots of Hemofil which had been identified as conveying hepatitis. Dr Cooper’s view, no doubt reflecting the then official position of the US Government, was that: “We feel that the warning is quite direct and adequate; in fact, it is generally appreciated in the U.S. that every lot of this particular product is probably contaminated with hepatitis B virus. Nevertheless, the benefits achieved by using the product in hemophilia therapy have been considered to outweigh the hepatitis risk”. Dr Cooper indicated that he would be interested in the views of Dr Yellowlees both on the labelling of the products and the “benefit-to-risk considerations”.[2293]
Amongst the matters Dr Cooper raised was that Hyland did manufacture product in Belgium, “in facilities which are not licensed by us and therefore not subject to our regulations”; that although Hemofil was described as “tested and non-reactive [to Hepatitis B surface antigen] ... it is generally appreciated in the U.S. that every lot of this particular product is probably contaminated with hepatitis B virus.” He also stated that “Source plasma collected outside the U.S. and shipped to overseas consignees manufacturing products not licensed by us are not subject to any U.S. regulations.”[2294]
This prompted a response within the DHSS,[2295] especially given the view that “every lot of [Hemofil] is probably contaminated with Hepatitis B virus”. Dr Sheila Waiter, in a memo written after the screening of the World in Action documentary, wrote:
“while it is generally accepted that the benefits of having Hemofil readily available for the treatment of bleeding episodes far out-weigh the risk of acquiring hepatitis B nevertheless the statement that ‘every lot of this particular product is probably contaminated with hepatitis B virus’ will come as a surprise to many clinicians using the product, especially if the practice of issuing a warning on the label has been discontinued, as is indicated in the letter from Dr Cooper ... I have the impression that clinicians accept a risk as I have indicated above,[2296] but it seems that the size of the risk has been underestimated, possibly even misrepresented by the manufacturer.” [2297]
Dr William d’A Maycock was asked to review the labelling. He responded in January 1976 that since August 1975 the product was negative on testing by radioimmunoassay (“RIA”); and that the warning “I would say ... overstates the risk, given that both the plasma and concentrate are tested in a proper manner by RIA.” He went on, nonetheless, to state:
“The prevalence of hepatitis in U.K. associated with U.K. blood and blood products has long been smaller than that in U.S.A. However, until concentrate prepared from UK plasma is available, I would have said the benefits attaching to Hemofil and other similar concentrates of antihaemophilic factor, used with discrimination, outweigh the risk. There is always the problem of non-B hepatitis; some American authorities now say that this may account for 90% of transfusion associated hepatitis. This opens a new vista of complications.” [2298]
In the product licence application for Kryobulin, also considered in 1973 for the first time, the proposed package insert referred to the manufacture of the product from “pooled plasma of healthy donors” and to steps taken to test donations for GPT level (a test for liver function now known as alanine transaminase ‘(“ALT”))’ and hepatitis-associated antigens, before stating: “Despite these precautions, the risk of transmission of homologous serum hepatitis can only be diminished, and not completely eliminated.”[2299] Later, the same leaflet recorded the following under the heading “Side Effects”: “Despite the precautions taken in the selection of donors, the risk of transmission of homologous serum hepatitis cannot be entirely excluded when administering human coagulation factors.”[2300] Kryobulin was licensed in March 1973.
In 1975, following the infection of a patient with Hepatitis B, Dr David Dane of Middlesex Hospital wrote to the managing director of the UK subsidiary of Immuno, Norman Berry, with a number of concerns about the testing regime employed for Kryobulin and about the hepatitis warning, saying that in light of recent UK experience: “I do not consider the warning about homologous serum hepatitis on the leaflet to be adequate.”[2301] Norman Berry replied, pointing out (correctly) that the warning had been submitted to and accepted by the Committee on Safety of Medicines.[2302] In response, Dr Dane wrote that: “My comment about the warning in your leaflet was a personal observation, and I am aware that my own views and those of several of my colleagues do not coincide with those of the committee on the Safety of Medicines.”[2303]
Dr Dane’s concerns were seen and considered by officials in the DHSS but did not lead to any action on the product licence.[2304]
Abbott/Alpha (“Profilate” )
The Abott/Alpha product, Profilate, was licensed in 1975 initially with the following warning: “This product is prepared from units of human plasma which have been tested and found nonreactive for Hepatitis Associated Antigen. However, it is recognized that presently available methods are not sensitive enough to detect all units of potential infectious plasma and the risk of transmitting hepatitis is still present”.[2305]
Over the years the text was amended to take account of changes to screening tests, but the final sentence remained unchanged.[2306] Later data sheets, however, contained an additional warning: “Patients with mild deficiencies who consequently have not received multiple transfusions of blood, or blood products, are at greatest risk. Under such circumstances, the benefits of Profilate administration must be weighed carefully against the risk of viral hepatitis; single donor products are preferable whenever possible.”[2307]
This data sheet was included in the 1976 and 1978 ABPI Data Sheet Compendiums.[2308] It was also contained in the application for a product licence for heat-treated Profilate made in January 1985, prefaced by the words: “Viral hepatitis may be transmitted by this product.”[2309]
The package insert on the Cutter product, Koate, as submitted to the licensing authority for approval in October 1975, contained the following text (maintaining the original capitalisation):
Under the heading “Description”:
“THIS PRODUCT IS PREPARED FROM UNITS OF HUMAN PLASMA WHICH HAVE BEEN TESTED AND FOUND NON-REACTIVE FOR HEPATITIS ASSOCIATED (AUSTRALIA) ANTIGEN. UNFORTUNATELY THIS TEST DOES NOT WITH CERTAINTY PRECLUDE THE PRESENCE OF HEPATITIS VIRUS. SEE WARNING.”[2310]
Under the heading “Indications” it said:
“CAUTION: BECAUSE OF THE POSSIBILITY THAT ANY LOT OF KOATETM MIGHT CONTAIN THE CAUSATIVE AGENTS OF VIRAL HEPATITIS, ITS USE MUST BE CONSIDERED IN LIGHT OF THIS HAZARD, PARTICULARLY IN PERSONS WITH FEW PREVIOUS TRANSFUSIONS OF BLOOD AND PLASMA PRODUCTS.
Kasper and Kipnis[2311] have concluded that those who had little exposure to blood products had a high risk of developing hepatitis after introduction of clotting factor concentrates, such as this product. For those patients, especially those with mild hemophilia, they recommend single donor products. However, for patients with moderate or severe hemophilia who have received numerous infusions of blood and plasma products, they feel that the risk of hepatitis is small. They believe that the clotting factor concentrates have so greatly improved the management of severe hemophilia that these products should not be denied to appropriate patients.” [2312]
Under the heading, “Warning” and contained in a box:
“KoateTM concentrate is a purified dried fraction of pooled plasma obtained from many donors. SINCE THE PRESENCE OR ABSENCE OF HEPATITIS VIRUS IN KOATETM CONCENTRATE CANNOT BE PROVEN WITH ABSOLUTE CERTAINTY, THE PRESENCE OF SUCH A VIRUS SHOULD BE ASSUMED and the hazard of administering KoateTM concentrate should be weighed against the medical consequences of withholding it.”[2313]
The following paragraph, outside the box, stated:[2314]
“Since there is this definite risk of hepatitis, we suggest that the physician give consideration to explaining to the patient (or the patient’s family) the relative risks of giving or withholding this product. Then, should the patient develop hepatitis, as a result of the injection, it will not come as a surprise, and there is not nearly the likelihood of resentment, which will almost surely follow an unexplained and unexpected infection.”[2315]
The label for the side panel of the carton contained the following text:
“WARNING: Since the presence or absence of the virus of hepatitis in KoateTM cannot be proven with absolute certainty, the presence of such a virus should be assumed and the hazard of administering Koate should be weighed against the medical consequences of withholding the use of KoateTM.”[2316]
A UK package leaflet from 1979 had updated wording to reflect development in tests for Hepatitis B surface antigen. It concluded with the observation that as the significance of Hepatitis B surface antigen testing had not been established when applied to the reconstituted product, “the product should continue to be considered to carry a risk with respect to hepatitis.”[2317]
A data sheet from January 1981 published by the UK subsidiary Cutter Laboratories Ltd under the UK product licence number, included a further detail in that it was stated that: “Koate concentrate is a purified dried fraction of pooled plasma obtained from many paid donors” (underlining added). The warning about the need to assume the “presence of hepatitis virus” (singular) was retained.[2318]
Package inserts from March 1981 and December 1981 demonstrate changes to the information to reflect the use of third-generation testing for Hepatitis B surface antigen. The December 1981 insert referred to the product being “prepared from the large pools of human venous plasma collected from many paid donors.” It also referred to the possible presence of “hepatitis viruses” (now in the plural).[2319]
Armour’s 1975 application for a product licence for Factorate contained two slightly differently worded warnings. The first, on the label, warned that “Despite careful selection of donors, it may contain causative agents of viral hepatitis.”[2320] This was updated in the application for Factorate HP made in 1978 to read: “Despite careful selection of donor and non-reactivity of the reconstituted solution for hepatitis B antigen by the radio-immuno assay procedure, freedom from the causal agents of hepatitis cannot be assumed.”[2321] The second warning, on the package insert, recorded that RIA testing for Hepatitis B surface antigen had been done on each plasma donation and stated that “since no completely reliable laboratory test is yet available to detect all potentially infectious plasma donations, the risk of transmitting viral hepatitis is still present.”[2322] This warning, amended to reflect changes in testing regime, remained in the inserts for Factorate and the high-purity Factorate HP variant, and in relevant data sheets into the late 1980s.[2323]
Commentary
The evidence shows that the warnings were addressed to the regulator and to the clinician, rather than to the patient. Two of these leading pharmaceutical companies issued warnings in starker form than the others: thus the warning on the Hemofil bottle was unqualified: “The risk of transmitting hepatitis is present”,[2324] without any attempt to “sugar the pill”. However, the package leaflet was less clearcut, and to the effect that the risk of hepatitis was “unknown”.[2325] There is a contrast (at least in the likely perception of a reader) between a “known risk” and a risk which is “unknown”. The first is present; the second may not be. A clinician reading the product leaflet would not necessarily appreciate that the chances of contracting hepatitis by using the product were more than possibly being present – there was a real risk, even if one could not say of any individual batch that it was actually infective. This does seem to “sugar the pill”.
The other one to issue a warning in starker form was Cutter in respect of Koate: it advised that the presence of hepatitis virus “should be assumed”.[2326] In my view, this is the clearest and starkest warning. There is detail which accompanies it which suggests that rather than use Koate, people with mild haemophilia should use “single donor products” (ie such as cryoprecipitate). Moreover, the clinician was advised to discuss the risks and explain them to their patient.[2327] This is the only company which went that far (and it was entirely appropriate to do so).
The other three companies considered here – Immuno, Abbott/Alpha, and Armour – all used formulations which could be read as suggesting that their product was really not very likely to transmit hepatitis. There would be nothing, one might have thought, to justify anything approaching the assumption which Cutter invited users to make, namely that the risk was there and they should proceed only on the basis they were prepared to run it. Thus: Immuno said the risk “cannot be entirely excluded”, and by these words which suggested it could largely be excluded, when coupled with references to “healthy” donors and to having tested all donations for hepatitis associated antigens conveyed a picture of minimal risk.[2328] Abbott/Alpha described that tests had been negative for the presence of hepatitis, but not “all units” of “potentially” infectious plasma could be detected so the risk (the inference is, only a little) was “still present” (their later data sheets did however advise the use of single-donor products where possible);[2329] and Armour, in common with Immuno and Alpha, began by emphasising the precautions taken to render the product safe before saying that despite those the product “may contain causative agents of viral hepatitis”; and rather than say, as Cutter did – “assume there is a risk” – it said, in a roundabout formulation that “freedom from the causal agents of hepatitis cannot be assumed.”[2330]
From the UK perspective, it is worth reflecting that the careful reading one would expect haemophilia clinicians to give before a first use of any of the products would lead them all to recognise not only that there was a risk, but also that the very same commercial firms as were interested in selling their large pool products were (so far as hepatitis is concerned) advising in two cases out of five that single-donor products should be used in preference (in the case of those with limited prior exposure to concentrates (Cutter); more generally in the case of Abbott/Alpha), if hepatitis risks were to be minimised.
The warnings for Hemofil were thought by Dr Dane, and by Dr Waiter, to understate the risk (even to the extent, according to Dr Waiter of having possibly “misrepresented” it, though she does not give specific reasons for this).[2331] It would appear from Dr Dane’s letter that “several of [his] colleagues” shared his view. Dr Maycock, and (it would seem from Dr Dane’s letter) members of the Committee on Safety of Medicines thought the warnings did not do so, to the extent that Dr Maycock thought they “overstated” the risk.[2332]
Dr Maycock appears to have taken this view because he had had in mind the risks of “hepatitis” as being those of Hepatitis B. He was aware that a virus, causing hepatitis, which was neither Hepatitis B nor Hepatitis A, was likely to be present in any large pool preparation, and hence all the more so in those made from plasma collected from donor populations in which hepatitis (in all its forms) was particularly prevalent, such as those used in the US. This could not be tested for. Its potential effects were yet to become clear, but they could not be ignored. The Bournemouth hepatitis outbreak, which was the background to the correspondence over product warnings, involved non-A non-B Hepatitis (as well as Hepatitis B). Yet none of the warnings flagged up this risk. They were linked to Hepatitis B testing, and it would reasonably be expected that as testing slowly improved, the risk of Hepatitis B would recede. But this could not be said of non-A non-B Hepatitis. Dr Maycock did refer to non-A non-B Hepatitis at the very end of his letter; noted that some American authorities now said it might account for 90% of transfusion-associated hepatitis, and that this “opened up a whole new vista of complications.”[2333] It thus seems that it is best to view his letter as expressing his view about the adequacy of a warning of Hepatitis B alone. However, he did not, as he should have done, urge that the warnings should refer specifically to what had by now become the recognised risk of non-A non-B Hepatitis.
Haemophilia clinicians, and the licensing authority, either knew of the risks of non-A non-B Hepatitis or should have done. The warnings were addressed to them. If they had been read by a patient receiving home treatment, it is highly unlikely they would have understood that if they used the product there were risks to their health – of an unknown extent, which could not (properly) have been assumed to be negligible, for which the product had not been tested because there was no test that would detect it. It was for their clinician to tell them of these risks. However, though factor concentrates were distributed through hospitals and clinics, some clinicians who did not regularly care for people with bleeding disorders might use them and they would not necessarily know of the risk if they were not alerted by a product warning. In the absence of wording to the effect that it should be assumed that a virus was present which would cause hepatitis, with potentially serious consequences, which could not be excluded by any available test, the warnings about hepatitis were therefore inadequate for the UK market. They did not sufficiently identify a risk of non-A non-B Hepatitis by referring generally to hepatitis, especially in the case of warnings which spoke about the product having been tested and found non-reactive, for testing could not have extended to non-A non-B Hepatitis.
Although the pharmaceutical companies involved in the production of concentrates did not, with the exception of Alpha, acknowledge in public until well after the start of 1983[2334] that there was a real risk that AIDS might be transmitted or caused by using factor concentrates, they nonetheless were (or ought to have been) well aware of this risk.
Alpha was first to state it in public. There is some uncertainty about the date this was first done. However, following internal urgent communications on AIDS sent on 16 December 1982,[2335] Alpha took action to avoid taking plasma from high-risk groups, and issued a press release of 7 January 1983. This said:
“The evidence suggests, although it does not absolutely prove, that a virus or other disease agent was transmitted to [patients with haemophilia who have now developed AIDS] in the Factor VIII concentrate, derived from pooled human plasma which they rely on for life – and for sustaining a relatively normal lifestyle.
Surveys now being conducted by [the National Hemophilia Foundation] are producing other disquieting findings:
The press release also pointed out that: “In recent months, three cases of AIDS appear to have occurred in persons who are not haemophiliacs, as the result of receiving blood transfusions – and blood bankers are fearful that there soon may be many more.”[2337] It said it had contacted its “several hundred plasma suppliers” that, as of 20 December 1982, they “must ‘exclude donors’ who may be part of three potentially high-risk groups: persons who have been in Haiti: drug abusers and male homosexuals. There is a ‘higher incidence of AIDS’ in these groups than in the community at large, the company says.”[2338]
When it came to repeating the essence of this in product sheets, the evidence is that by March 1984 Alpha warned:
“The causal factors of Acquired Immune Deficiency Syndrome ... have not been fully defined. However, HTLV-III/LAV virus has been implicated as a possible agent of the disease. It is not presently known if other transmissible agents are involved. Alpha uses screening procedures to eliminate high risk plasma donors and a heat-treatment step in the manufacturing to reduce the risk of transmitting AIDS. However, despite the careful selection of donors, it may be possible that the AIDS causative agents may still be present in and be transmitted through this product.”[2339]
The product information sheet is dated as “Issued March 1984” and contains the name and address of the UK distributor.[2340] It is likely, therefore, that this information was provided when Profilate HT was provided on a named patient basis in the UK from May 1984, and possibly earlier.[2341]
During the subsequent licensing process, the licensing authority required references to heat treatment to be that it was intended to “reduce the risk of transmission of infectious agents” rather than making claims about it reducing the risks of HIV or non-A non-B Hepatitis by name.[2342]
Other companies were well aware of the risk of AIDS, too. Thus in an internal memorandum dated 29 December 1982, Edward Cutter of Cutter Laboratories wrote:
“It appears to me to be advisable to include an AIDS warning in our literature for Factor IX and Factor VIII. I realize that very little is known about AIDS and the relationship the products we manufacture have in causing the syndrome. However, litigation is inevitable and we must demonstrate diligence in passing along whatever we do know to the physicians who prescribe the product. In my opinion, three steps are called for, once we agree the wording of our message.
The Inquiry has not investigated if there was any response to this memorandum and it is not clear what action, if any, it prompted. Though there may have been something said earlier, so far as the Inquiry is aware,[2345] nothing was said in public until around a year later. Cutter and the FDA then (in November 1983) discussed adding an AIDS warning to US product information and this led to the addition of such a warning in December 1983.[2346] It was in these terms:
“Isolated cases of Acquired Immune Deficiency Syndrome (AIDS) have been reported in hemophilics [sic] who have received blood and/or coagulation factor concentrates, including Factor VIII concentrates. It is not known if the disease is due to a transmitted specific agent, secondary to multiple antigenic exposures, or to some other mechanisms. The physician and patient should consider that Factor VIII concentrates may be associated with the transmission of AIDS and weigh the benefits of therapy accordingly.”[2347]
By way of comment, this envisages a discussion between doctor and patient about the risks and benefits of taking the concentrate in the light of the risk of AIDS. There is little evidence that any such discussions took place in the UK, where in October 1983 Professor Arthur Bloom was maintaining to the annual general meeting of haemophilia centre directors there was no proof that commercial concentrates were the cause of AIDS.[2348]
While an AIDS warning was added to US product information in December 1983, the earliest product warning in the UK which the Inquiry has been able to identify is in March 1984.[2349] The terms of that warning are identical to that set out above.
It is to be inferred that Hyland knew in 1982, if not earlier, that there was a real risk that factor concentrates might transmit whatever caused AIDS. Dr Kingdon wrote a memo on 5 January 1983 which began:
“We have been closely monitoring the AIDS issue at Hyland since the original description of the syndrome in male homosexuals in the December 10, 1981 issue of The New England Journal of Medicine, and more intensively since the first three hemophilia cases were reported in the Morbidity and Mortality Weekly report from the CDC on July 16, 1982. Many of us have been involved in considering the problem and in discussions with the CDC on its implication for our blood products.”[2350]
The CDC had suggested since at least early to mid 1982 that AIDS might be caused by an infectious agent transmitted by sex or by blood or blood products,[2351] and pursued that line persistently since then – so it is inevitable that in Hyland’s discussions they would be alerted to the possibility. Indeed, much of the memo was concerned with the prospect that Hyland’s heat-treated product, about to be licensed, might lessen the risks of AIDS transmission.
As is discussed in the chapter on Regulation of Commercial Factor Concentrates, the Committee on Safety of Medicines advised against issuing a product licence for heat-treated Hemofil in September 1983 in part because of the absence of evidence that AIDS was transmitted by a virus and hence might be affected by heat treatment.[2352] Christopher Bishop, of the UK subsidiary of Armour, gave oral evidence to this Inquiry to the effect that the content of product information was a matter for the licensing authority to determine in discussion with the scientists from the companies applying for licences, and that in the absence of firm evidence of a product being implicated in the transmission of AIDS he – as someone involved in marketing the product rather than its licensing – was not concerned about the absence of a warning.[2353]
Whatever the reason, the result was an absence of AIDS warnings from many of the licensed factor concentrates provided in the UK. The Inquiry has an extensive selection of data sheets and product leaflets relating to Kryobulin in the early and mid 1980s. None mention AIDS, HTLV-3, LAV or HIV.[2354] Nor were there warnings in the product literature identified by the Inquiry for Factorate and High Potency Factorate, Armour’s products, in this period.[2355]
The Krever Report records that: “In the autumn of 1983 and early 1984, U.S. fractionators added warnings about the risk of AIDS to the information in the product inserts – Armour, for its factor VIII concentrate, in October 1983; Cutter, for its commercial factor VIII concentrate, in January 1984; and Hyland, for its factor VIII concentrate, in March 1984.”[2356] However, the Krever Report does not cite the evidence on which it relies and the Inquiry has not found evidence of such warnings in the UK material, other than is set out above.[2357]
The product information labels and leaflets were not the only means by which pharmaceutical companies communicated with haemophilia centres and clinicians. As is discussed elsewhere in this Report, there were regular contacts between representatives of the companies and their existing or prospective customers, which would include the provision of information about products and risks associated with them. As described, Alpha made it clear in a press release of 7 January 1983 that there was a real risk that taking factor concentrates might lead to AIDS.[2358] All the companies would also, on occasion, send circulars. One such example is a letter sent by Ken Fitch, the chairman and managing director of the UK subsidiary of Armour, to all haemophilia centre directors on 19 May 1983. The context was the first withdrawal of batches of a blood product (Hyland’s Autoplex) from the US market following the identification of a donor who was thought to have contracted AIDS.[2359] The Armour letter ran to five pages and set out the company’s understanding of AIDS and the steps that it had taken in response to its emergence. The letter began by stating that:
“Despite the fact that there is little evidence to associate plasma component therapy with the transmission of AIDS, Armour, through its affiliate organisation, Plasma Alliance, has had programmes in operation for several months, which have been designed to help prevent the utilisation of plasma obtained from members of high risk groups associated with AIDS in the production of clotting factor concentrates.”[2360]
Those programmes, and the approach of Armour and other pharmaceutical companies to further measures proposed in this period, are discussed in greater detail below. In terms of the communication of risk, Ken Fitch’s letter referred to approximately 1,500 identified cases of AIDS, a worrying increase in the rate of incidence, and a mortality rate of 40%. These figures applied to the general population, not people with bleeding disorders. In respect of the latter, Ken Fitch wrote that:
“Of additional concern to Armour Pharmaceutical Company and to others in the health care field is the indication, from data generated by the CDC, that AIDS is being seen in recipients of blood, blood components, and blood derivatives. In a summary presentation made in May, 1983, the CDC stated that 14 haemophiliacs have apparently contracted AIDS, and that an as yet unidentified number of non-haemophilic recipients of blood and blood components also have developed the syndrome. The CDC is investigating the possible relationship between AIDS and the use of blood and blood derivatives, and is attempting to determine whether transmission of AIDS via transfusion is indeed occurring.”[2361]
Later in the letter, having set out the steps taken by Armour and Plasma Alliance to try to exclude high-risk donors from its plasma pools, Ken Fitch stated that these measures were: “predicated on the possibility that AIDS may be transmitted through blood and certain blood derivatives, although it must be re-emphasised that no agent responsible for transmission has yet been identified. However, one must consider that an infectious organism may be involved, and that the appearance of AIDS is prevalent in groups with high incidence of Hepatitis.”[2362]
The UK subsidiary of Hyland/Travenol appears to have sent a similar circular on 9 May 1983, at the time the recall of batches of its US product was announced. This was shorter than Ken Fitch’s letter and concentrated on donor screening measures, heat treatment and the reasons behind the product recall (which are discussed below). On the risk of AIDS it stated that: “While the causative agent of this disease remains to be identified, some evidence suggests it is caused by a virus that can be transmitted by blood and certain blood products.”[2363]
When they received these letters in May 1983, the effect would have been more to confirm UK haemophilia centre directors in an awareness that there was a real risk that factor concentrates would transmit the cause of AIDS than inform them for the first time of this. They had first discussed it as a group in September 1982, many had been present at the detailed discussions at a Heathrow hotel in January 1983 and in May 1983 the reference centre directors had faced the press concern that broke at the very start of the month.[2364]
Commentary
The risks which were recognised by the companies in the US, that factor concentrates could lead to AIDS, were not adequately reflected in product warnings provided to clinicians in the UK. Although the weaknesses in the UK response to the threat of AIDS were not the responsibility of the pharmaceutical companies to understand and mitigate, might such warnings have made a difference? Much was written generally about AIDS in the popular press in 1983, to which UK clinicians had access, and much in the scientific literature. Yet there remains a possibility that it could have done so given Professor Bloom’s approach, that of the UK Haemophilia Centre Directors’ Organisation he chaired, and given the “no conclusive proof” line by the DHSS. Though it should not be overstated, if it had been seen by clinicians, politicians and civil servants that the main commercial producers were all suggesting there was risk to be taken seriously that their products might lead to contracting AIDS, it is certainly possible that they would have revisited their views and started to take some action a little sooner.
As recorded elsewhere in this Report, the response of the UK to the risk that factor concentrates posed was characterised by a mixture of disbelief, delay and inaction. It cannot be said with confidence that product warnings about a risk of AIDS would have made some difference to this, but there is a real possibility they might have made a not insignificant one. It is not that there were no warnings at all – as set out above, there was communication at the start of 1983 which in the case of one company (Alpha) publicly recognised a risk that using their factor concentrates risked AIDS,[2365] but the Inquiry had no material which shows that the other companies told clinicians in the UK of the risks of AIDS until after the FDA had recommended (on 24 March 1983) that in the light of these risks the use of plasma from high risk donors should be abandoned from then on. Neither the letter from Armour nor from Hyland/Travenol[2366] were written before Professor Bloom had written his letter of 4 May 1983 to the Haemophilia Society in a dismissive response to the reports of two AIDS cases involving people with haemophilia – and the latter would have arrived after the UKHCDO had adopted a letter of advice which commended, in essence, making no change in the approach to haemophilia therapy.[2367]
Warnings could have been given earlier. They could have been given on product data sheets. If the very firms whose products were said by many third parties to be most implicated as being potentially causative had confirmed that, as they themselves also saw it, there was a realistic case that they might indeed be linked to AIDS this would have been a powerful reaffirmation of the risk.
The emerging knowledge of the risk of AIDS to those using blood and blood products in the UK is considered in earlier chapters.
Commercial pharmaceutical companies rapidly became alert to the fear that their products might form part of a chain of transmission between an AIDS victim and a patient. The prestigious journal, The New England Journal of Medicine, published an editorial and three articles on AIDS in its issue of 10 December 1981.[2368] This alerted Dr Kingdon of Hyland/Travenol, who recorded just over a year later that since that date “we have been closely monitoring the issue at Hyland”.[2369]
An internal task force on Kaposi’s sarcoma (a rare form of skin cancer previously found only in elderly men) and pneumocystis carinii pneumonia (which until then had been found only in patients with severely weakened immune systems) had already been set up by the CDC in July 1981, to investigate and monitor what appeared to be a new disease in clusters of predominantly homosexual men: by the time of The New England Journal of Medicine articles, it seemed an epidemic was on the way. The task force found that the diseases, resulting from an acquired cellular immunodeficiency, had recently appeared in both intravenous drug users and homosexual men, suggestive that an infective agent might be the cause. This view was strengthened by June 1982 when case numbers rose significantly within the heterosexual population. Of the 355 cases reported then, 16% were heterosexual – and a quarter of these were women. Only about half were intravenous drug users.[2370]
In the first half of 1982, it was reported to the CDC task force that cases of Kaposi’s sarcoma and pneumocystis carinii pneumonia amongst patients with haemophilia were being investigated, and three had been identified, all in different parts of the US.[2371] This led the CDC to convene a small ad hoc expert advisory committee to identify the implications of this for blood products. Thus on 9 July 1982 the FDA (which was represented on the committee) wrote to manufacturers of plasma fractionation products to tell them:
“Three cases of Pneumocystis carinii pneumonia (PCP) in patients with Hemophilia A receiving antihemophilic factor have recently been reported to the Centers for Disease Control. All three patients were heterosexual white men without a history of intravenous drug abuse.
During the past year several hundred cases of life-threatening opportunistic infections have been reported in persons without predisposing diseases. Most of these infections have been in homosexual men and individuals who were IV drug abusers ... Although the cause of this outbreak is unknown, the information suggest that a transmissible agent might be involved and concern about transmission through blood and blood products has been raised.” [2372]
16 July 1982, a week later, was the date on which the Morbidity and Mortality Weekly Report (“MMWR”) published a report that three people with haemophilia had contracted AIDS, thus beginning to fuel concerns in the UK about the safety of concentrates.[2373]
Even if pharmaceutical companies had not, as Travenol/Hyland had, monitored the developing situation closely since December 1981, they were now all alerted to the real possibility that their products might transmit the cause of the new disease. Though the note was short, it suggested that whatever the cause was it was capable of leading to AIDS in gay men and in intravenous drug users and in people with haemophilia. They would quickly have realised, if they had not done so already, that women as well as men were suffering – suggestive therefore that the cause was not restricted to male homosexual activity.
Since the National Hemophilia Foundation was also alerted, and broke the news to its members on 14 July (saying that the CDC believed that the immune deficiency might be caused by a virus transmitted through blood or blood products as was hepatitis, but advising its members that the risk of contracting this immunosuppressive agent was minimal),[2374] it is almost inescapable that from then on pharmaceutical companies knew there was a real risk that their products led to AIDS amongst recipients. The National Hemophilia Foundation was a body representing a large number of consumers of their products.
By way of comment, the fact that the news broke a week before the MMWR published a report relaying information about the three people with haemophilia who had contracted AIDS may explain why Dr Harold Gunson in the UK was probably alerted to the risks and able to notify the DHSS as promptly as he did, even slightly before the publication.[2375]
A committee on opportunistic infections in patients with haemophilia in the US met to exchange information about the cases and to conduct surveillance. At its second meeting in Washington DC on 27 July 1982 it considered whether the cause of immunodeficiency in people with haemophilia was the same as the cause of immunodeficiency in members of other high-risk groups, and whether certain blood products placed recipients at risk of contracting this form of immunodeficiency. The American Blood Resources Association, the fractionators and plasma collectors’ trade body, participated. There was agreement that the disease was caused by an infectious agent, and that those at risk of developing the disease included intravenous drug users and Haitians, in addition to homosexual men. Whether people with haemophilia were at risk of contracting AIDS from blood products was not yet considered clear, but it was agreed that the possibility must be explored and that techniques should be developed immediately to reduce or eliminate the risk of infection from Factor 8 concentrates.[2376]
This meeting was the first public expression of the tensions that would affect the response to AIDS among regulators, scientists, and the voluntary and commercial blood sector in the US. While leading figures within the CDC became still more convinced both of the threat posed by AIDS and that it was caused by a blood-borne infection, those they sought to convince demanded more evidence to justify proposed actions. As Dr Bruce Evatt wrote in a retrospective article – The Tragic History of AIDS in the Hemophilia population 1982-1984 – “As these cases accumulated, the author routinely provided briefings to the blood industry, FDA panels and NIH [National Institutes of Health] conferences of blood banking experts, who seemed only to request more patients and proof, without yielding on recommendations for changes in blood policy.”[2377]
As will be seen, a number of proposals for action were met with requests for studies, while different actors pointed to the lack of conclusive proof about the aetiology and transmission of AIDS as a justification for maintaining the status quo. It is important to note that this was not just the plasma companies; indeed for many months the frustrations of Dr Evatt and his colleagues were primarily directed at the voluntary blood bankers within the US system who were more intransigent, particularly on matters concerning donor selection. As Dr Steven Ojala of Cutter wrote after one meeting in January 1983, quoting a colleague from Hyland: “It is unusual for us [the commercial companies] to come away wearing the white hats while the ‘volunteer’ sector wears the black.”[2378] Individual clinicians, gay rights groups, and the National Hemophilia Foundation all joined calls at various stages to obtain more information before taking steps or “stigmatising” donors or users of blood products.[2379]
The tension became still more pronounced at the end of 1982 and the start of 1983. By then, the CDC had published a report of the transfusion-related case of a 20-month-old infant in San Francisco who contracted AIDS; the same edition of MMWR confirmed that the three people with haemophilia whose cases had been reported in July had all died.[2380] Dr Evatt, in his Tragic History article, stated that he and his colleagues “were now convinced that in spite of the absence of an identified agent, the pattern of the epidemiological evidence was sufficient to implicate a blood-borne disease.”[2381] He anticipated that a public meeting to be held at the instigation of the CDC in Atlanta on 4 January 1983 would be a “pro forma stamp for action, that is, review the data, accept the evidence as significantly supporting the case for blood-borne infection and produce recommendations that high-risk groups be excluded from the donor pool and/or adopt a surrogate test.”[2382] He was to be bitterly disappointed. Various accounts exist of the meeting, which are set out in Counsel to the Inquiry’s presentation, but it is succinctly summarised by Dr Hink of Cutter in an internal memorandum:
“difficulties in communication and political power struggles made progress towards these objectives difficult. The anti-discrimination position of the gays, self-serving comments of blood bankers and lack of data to provide legitimacy to many proposals resulted in an overall stalemate. I felt a great deal of empathy for the meeting chairperson”.[2383]
The meeting became heated, with attendees criticising the CDC’s data and conclusions. In response one CDC attendee, Dr Francis, slammed his fist on the table and asked in effect how many AIDS cases, or how many deaths, would be needed before those attending took action.[2384] Dr Evatt’s retrospective view was that:
“Two views emerged. To us, the attendees’ reactions seemed to be those of a group approaching an idealized science problem in an abstract world; to the audience, their position was that of a group acting as careful scientists in accordance with their training.
All attendees underestimated the already high disease incidence in the population because AIDS was obscured by a long, still undetermined incubation time. Dismissed as inadequate were our data on the high frequency of immune disorders affecting the hemophilia population that were identical to those found in homosexual patients with lymphadenopathy associated syndrome. Above all, the blood bank organizations remained unconvinced that the CDC had shown the condition to be a blood-borne disease and some FDA officials remained unconvinced that AIDS was actually a distinct disease. Dr Koplan [who chaired the meeting] proposed a set of consensus recommendations at the end of the day and all were soundly defeated.” [2385]
Institutional concerns also played their part. Dr Evatt accepted that the CDC were intruding into regulatory areas that were properly the responsibility of the FDA. Some organisations expressed suspicion of the CDC’s motives. A senior official at the American Red Cross wrote in a memorandum that: “it has long been noted that CDC increasingly needs [a] major epidemic to justify its existence ... In short, we can not depend on CDC to provide scientific, objective, unbias[ed] leadership”.[2386]
An overview, derived much closer in time to the events than this Inquiry can be, is provided by the Krever Report. Mr Justice Krever summarised the result of the meeting in this way:
“Although the participants reached a consensus that ‘it would be desirable to exclude high-risk donors to reduce the risk of AIDS transmission,’ there was no agreement about a method of accomplishing that goal. There was also no consensus on the question whether AIDS was caused by a transmissible agent, on the risk of AIDS from blood donations, or on the desirability of introducing new methods of donor screening or testing to reduce the risk of transmission. Instead, the CDC, the Food and Drug Administration, and the National Institutes of Health were each asked to submit a set of recommendations, after the meeting, for the prevention of AIDS in patients with hemophilia and for other recipients of blood and blood products so that a uniform set of recommendations might be developed.”[2387]
These recommendations were announced by the US Public Health Service on 4 March 1983, when their principles were endorsed by the American Red Cross, the American Association of Blood Banks, and the Council of Community Blood Centers.[2388] On 24 March the FDA requested that blood and plasmapheresis centres immediately adopt procedures to ask donors in high-risk groups (“persons with symptoms and signs suggestive of AIDS, sexually active homosexual or bisexual men with multiple partners, Haitian entrants to the United States, present or past abusers of intravenous drugs and sexual partners of persons at increased risk of AIDS”) to refrain from donation, and immediately to “institute procedures with your plasma suppliers to assure that they have adopted appropriate donor screening practices and procedures.” Products from donations made before this had to be labelled to indicate this had been done, and high-risk groups thereby discouraged from donation.[2389]
By way of comment, where a risk is identified, action should follow in case the risk might become a certainty. What should not follow is delaying until certainty can be established as a prerequisite for acknowledging the risk. There can be no doubt, objectively, that those at the meeting of 4 January 1983 faced a real risk that using concentrates might spread AIDS. What was argued was close to seeking certainty before action was to be taken – that the cause of AIDS had to be proved conclusively to be a transmissible agent before action was needed. This was to focus on the wrong question, namely whether there was certainty, or near-certainty. Dr Evatt summed this up as needing “more patients and proof”.[2390] An analogy is that if there is smoke in the building, the fire alarm will go off and everyone will evacuate. Though experience may teach there are many false alarms, the time to take action is still when the smoke triggers the alarm: leaving it until there is the certainty of flames licking round the door is always going to be too late.
Whatever was said in the discussions mentioned above about a lack of information, patients and certainty, and hence a lack of consensus as to whether the postulated cause was “real”, the fire alarm bell that was ringing was nonetheless heeded by some of the pharmaceutical companies in respect in particular of donor exclusion and screening.
Two measures in particular were considered of importance by the CDC in late 1982 and early 1983: the exclusion of high risk donors and surrogate testing. Pharmaceutical companies were amenable on the former but, with the exception of Cutter and to a lesser extent Hyland, resistant on the latter.
In December 1982 the pharmaceutical companies were asked to commit to avoiding collection centres in “high risk” areas. These were notably the major urban centres of San Francisco, Los Angeles, Miami and New York. They were asked, too, to improve the education and screening of donors from “high risk populations” – gay men, Haitians and intravenous drug users.[2391]
Alpha was the first of the companies to take significant measures in this respect. At a meeting on 15 December 1982, its Executive Committee agreed a number of steps including suspending deliveries of plasma from the Irwin Memorial Blood Bank in San Francisco, implementing direct questioning about whether a donor was in a high risk group (including whether they had had sexual contact with a man), and providing information about AIDS and the high risk groups to donors. Alpha implemented these steps at their own centres and asked that they be introduced at plasmapheresis centres and blood banks that contracted with them.[2392] It announced on 7 January 1983 in a press release that it had done this with effect from 20 December 1982, and expressly said why.[2393]
Alpha’s willingness to take these steps, and to sustain the costs associated with them, is informative. It amounted to an acknowledgement that – whatever the scientific uncertainties about aetiology and transmission – there was sufficient prospect of blood products being implicated in AIDS to justify such an action. The company’s medical director, Dr Clyde McAuley, was quoted in its winter 1982 newsletter: “So long as there is any question about the involvement of blood products, Alpha is taking all possible steps to reduce the potential risk for the hemophiliac receiving our factor VIII and factor IX concentrates.”[2394]
The measures taken on donor education and exclusion had a rapid and significant effect. Within the first three weeks, 308 gay donors had been excluded.[2395] By the summer of 1983, 800 potential donors had “voluntarily disqualified themselves from the pool.”[2396] Tellingly, Alpha’s insistence on these measures meant that they lost contracts with some blood banks that sold recovered plasma as they were not prepared to implement them.[2397] The contrast between these measures and the exclusions to which they led may be contrasted with the much slower progress towards issuing a donor leaflet in the UK, which when it came was weak in its terms: the “donor leaflets” in use in the UK are considered in detail in the chapter on Role of Government: Response to Risk.
Whilst the early implementation of these measures is laudable, they also shed light on the sources of plasma that were previously being obtained. This included donations from third parties where Alpha exercised less control over procedures, including plasma from the Irwin Memorial Blood Bank which was identified at an early stage as being associated with high risk donors.[2398] It included plasma from a significant number of gay donors, notwithstanding the known greater risk of hepatitis (which had encouraged Alpha and other companies to recruit such donors in order to produce immunoglobulins for use in making Hepatitis B vaccines). Alpha itself operated a plasmapheresis centre in San Francisco until the second half of 1982. In a letter to the National Hemophilia Foundation dated 9 November 1982 Alpha’s President, Thomas Drees, stated that: “We have no centers ... in San Francisco,” without mentioning that this was because its previous establishment had recently closed.[2399]
Further, while these steps were claimed by the company to be evidence that “Alpha is taking all possible steps to reduce the potential risk,”[2400] they were prospective, affecting plasma that was yet to be collected and processed, not that which had already entered the system. There is no evidence identified by the Inquiry to show that previous plasma donated by the donors who were excluded as a result of the enhanced screening was discarded, or that product was recalled. This means that although Alpha is to be applauded for taking the steps it did at some apparent cost to its business, the claim to have taken “all possible steps” cannot be taken literally.
It remains the case, though, that Alpha was the first of the US pharmaceutical companies to take such measures. On 28 January 1983, the American Blood Resources Association made a public statement accepting that the cases of AIDS in people with haemophilia “suggest that AIDS may be of infectious etiology.” The organisation urged that “steps be taken as soon as possible to screen plasma donors to minimize the possibility of transmitting AIDS.”[2401]The other companies subsequently adopted their own enhanced screening measures, including those in respect of questioning those who came to sell their plasma and medical examinations. Hyland did so in late January or early February 1983, and Cutter and Armour in February 1983. These actions were criticised as an overreaction by some, including Dr Joseph Bove, the chair of the Blood Products Advisory Committee (“BPAC”) and the director of the Yale New Haven Hospital blood bank.[2402] By the time the FDA gave recommendations in March 1983 for the greater screening and medical examination of donors, the four US fractionation companies could state that they had already introduced their own measures that were broadly equivalent.[2403] As has been noted, however, Hyland continued to collect prison plasma and use it in factor concentrates until the autumn of that year.[2404]
However, the logical corollary of the acceptance of the recommendation is that products made from plasma that was obtained before measures equivalent to the FDA March 1983 recommendations were put in place were of higher risk. Thus, if safety of the patient was the guiding principle these products should not have been issued – provided this could be done without unreasonably denying patients a choice between taking factor concentrates, on the one hand, or such other alternatives that could be offered in the US (including the absence of any treatment) or, if issued, should have been recalled (again subject to the same provisos). They were not recalled in the US. However, the implications of these recommendations were there for those in the UK to appreciate – they knew of them; and the position in the UK is the focus of this Inquiry. It was thus an issue for the UK regulator to consider.[2405]
In 1982 and 1983 various surrogate markers were suggested, discussed and studied.[2406] Anti-HBc testing came to be regarded, and argued over, as the most likely surrogate test, not least because the epidemiological pattern of AIDS was considered to be similar to that of Hepatitis B.[2407] With the notable exceptions of Cutter and Hyland, pharmaceutical companies joined with most blood banking organisations in opposing such tests.
Surrogate testing was raised at the BPAC meeting on 3 and 4 December 1982, where the minutes recorded “a sense of urgency because of the continuing spread of AIDS and because of its long incubation time.”However, the committee did not recommend any immediate changes in regulations or regulatory activities, instead noting that several investigations were being “intensely pursued”by the relevant agencies, organisations and companies.[2408]
Surrogate testing was raised again at the public meeting in Atlanta on 4 January 1983.[2409] The case in favour of this was said to be that 90% of known definite AIDS cases were positive for the antibody to Hepatitis B core antigen (anti-HBc). This compared to a 5% figure in the general population of voluntary donors. Those present did not agree about the frequency of anti-HBc in people who could transmit AIDS.[2410] The case against was that it would be expensive and that it would lead to the destruction of plasma without direct evidence that the plasma was infected with AIDS. The test was not sufficiently specific. Some concerns were also raised about the availability of materials for the test, and the need for additional training procedures. Dr Hink, of Cutter (someone who would later come to support the use of anti-HBc as a surrogate test) summarised the debate in the following terms: “Question of cost and implementation bothered many but not CDC, several objected on scientific grounds.”[2411]
No agreement was reached.
Shortly afterwards, on 14 January 1983, the National Hemophilia Foundation called a meeting bringing together pharmaceutical companies, blood bankers, regulators, the CDC, clinicians and the National Hemophilia Foundation. Before the meeting, representatives of the major fractionation firms and the American Blood Resources Association met together to determine their strategy. This was to seek to delay the implementation of surrogate testing, by arguing that although they accepted the concept it should wait until a more specific test was available.[2412] Strategy caucuses of the plasma collection and manufacturing interests in advance of their meeting regulators, the CDC and others were to become a common occurrence.[2413]
The attendees at this meeting agreed that “whenever possible we would try to deflect activity to the NIH [National Institutes of Health]/FDA”rather than the CDCwhichit was agreed “was getting increasingly involved in areas beyond their area of expertise”.[2414] Dr Ojala’s record reads as if this was a view based on concerns about expertise, but the NIH and FDA were less inclined at that time to push for the more stringent measures that at least some members of the CDC were proposing. In that sense, their views were closer to those of the plasma companies.
The companies’ concerns about the impending introduction of surrogate testing were not realised at the meeting. The recommendations from the National Hemophilia Foundation’s Medical and Scientific Advisory Committee were for, “Evaluation and implementation (if verified) of surrogate laboratory tests that would identify individuals at high risk of AIDS transmission.”[2415]The immediate request was, therefore, for more research, a position that the companies could accept. At the meeting there had been a general willingness to accept an exclusion rate of around 10% of donations and the higher costs associated with testing if an appropriate testcould be found.[2416] Dr Ojala’s view was that Dr Rodell of Hyland and Dr Donohue of the FDA:
“very effectively presented the viewpoint that surrogate testing was a positive step, but was only at the R&D stage currently. The NHF [National Hemophilia Foundation] seemed to accept the approach that we would accelerate any and all efforts in this area ... Donahue [sic] stated that the approach should be to develop tests, then validate and implement rather than to incorporate additional testing blindly and hastily.”[2417]
This approach – accepting the potential value of surrogate testing but emphasising the need for further research – was maintained by the majority of the US pharmaceutical companies and blood banking organisations until HTLV-3 was isolated and a specific test for it had been developed.
The FDA did not include surrogate testing in its March 1983 recommendations, and work continued on various studies throughout that year. A meeting took place on 15 December 1983 – jointly convened by agencies of the NIH and FDA – at which this research was considered. Dr Donohue of the FDA recommended that the time had come for anti-HBc testing to be implemented for plasma (but not whole blood) collection, but Dr Rodell (who by then had moved to Armour) successfully averted this by suggesting that a task force be established to consider the matter and report within three months. According to Dr Ojala’s account of the meeting:
“This proposal was one that had been agreed upon by all the fractionators the previous evening. The general thrust of the task force is to provide a delaying tactic for the implementation of further testing. It was generally agreed that core testing would eventually become a requirement. The addition of core testing is expected to eliminate approximately 15% of plasma donors, and 6-7% of whole blood donors if used by blood banks ... The fractionators met with Donohue following the meeting and, although Donohue was not completely satisfied with the task force approach, he agreed to it. He stated that we should also take on the responsibility for all testing of recovered plasma [ie plasma recovered from whole blood donations]. Rodell was named chairman of the Task Force and a meeting will be scheduled in January ... In summary, the conclusion of this meeting was that the time had come for Hepatitis core anti-body testing for plasma. Implementation will probably be achieved during 1984 for the industry.”[2418]
Dr Ojala’s prediction proved to be inaccurate. The task force produced an interim statement in March 1984 and a full report in July 1984. The interim statement recorded that the group was divided in its position on the use of anti-HBc as a surrogate test, with the “majority believing that such testing was not appropriate for that purpose.”[2419]The group did, unanimously, support further studies on beta-2 microglobulin levels as an alternative surrogate test, on the basis that this may correlate more closely with AIDS.[2420] A memorandum prepared by Dr Hink for his colleagues at Cutter revealed that three of the eleven members of the task force voted at a meeting in March 1984 in favour of anti-HBc testing – Dr Donohue of the FDA, Dr William Srigley of Hyland and Dr Hink of Cutter. Dr Robert Gerety of the FDA was thought to have abstained. The other seven members of the group voted against; they included Dr Rodell, Marietta Carr of Alpha and representatives of various blood banking organisations.[2421]
Dr Hink’s memorandum set out some of the arguments deployed at the meeting. It records that different speakers pointed to differing experiences of the percentage of gay donors who were anti-HBc positive, which were lower than the percentage the CDC was then claiming (75%); others argued that there might be a plasma shortage if the test were implemented. Arguments included one advanced by Dr Rodell, “showing anti-HBc testing and rejection of positive donors should cost several million $ per year.”[2422]
The following month, April 1984, saw the announcement that HTLV-3 had been isolated and that the Secretary of Health and Human Services, Margaret Heckler, was committed to the rapid introduction of a specific blood test.[2423] As is discussed in the chapter on Viral Inactivation, in the months that followed confidence grew that HTLV-3 was amenable to the heat treatment regimes already implemented by the pharmaceutical companies. Given the promise of heat treatment and a specific test, the pressure for the introduction of anti-HBc as a surrogate test for AIDS diminished.
Although a combination of some of the plasma companies and the blood banking interests successfully resisted the implementation of mandatory anti-HBc surrogate testing, Cutter unilaterally introduced its own programme that ran from April 1984 until the end of October 1984.[2424] The move had clearly been some months in the planning, as Dr Ojala wrote in a memorandum of 19 December 1983 that:
“John Hink, in a prescient move, has already begun core testing at Cutter centers. We recommend that the implementation of core testing be accelerated to the maximum degree possible to obtain a competitive advantage in the market place. The approval of our heat-treat submission, in conjunction with core-screened plasma could present us with a potent marketing advantage. We made no mention of our plans to the others.”[2425]
Internal Cutter documents from a review of the decision in May 1984 provide evidence of the perceived advantages and disadvantages of anti-HBc testing at that time.[2426]
Cutter supported surrogate testing notwithstanding some pressure from other companies to maintain a united front against anti-HBc testing. In his memorandum on the March 1984 meeting of the surrogate testing task force, Dr Hink recorded that: “Immediately prior to the conclusion of our meeting it was recommended that the Industry should refrain from starting anti-HBc testing. Carr was adamant that Alpha would not begin, Rodell said Armour would not use the test unless a competitor was using it to competitive advantage. Srigley [Hyland] indicated he could not speak for his company management and I parroted his comment.”[2427]
The other main debate concerning commercial blood products in the period between the emergence of AIDS and the isolation of HTLV-3 was the question of what was to be done over the recall of batches of concentrates that contained a donation from someone known or suspected to have developed AIDS. Here, the pharmaceutical companies were united in adopting and encouraging consideration on a case-by-case basis, rather than the introduction of firm rules or guidance from the FDA that would result in a policy of automatic recall in given circumstances.
In December 1982, Alpha’s Executive Committee discussed what was to be done with products produced from three units of plasma that had been obtained from a person described as “the AIDS donor”. The context of the note suggests that this donor had given blood to the Irwin Memorial Blood Bank, and Alpha had fractionated the recovered plasma into blood products. This included at least one lot of factor concentrate comprising 2,841 vials. The situation was to be reported to the FDA and the committee agreed to wait for the FDA’s opinion on what should be done.[2429] Two months later, in February 1983, the company’s AIDS Task Force considered what to do with 11 plasma donations from a donor in Dallas who “possibly”had “some AIDS symptoms”in the form of lymphadenopathy,but no diagnosis and “little else to connect him with AIDS.”The task force decided to release four lots of factor concentrate containing his plasma but not to use any plasma from the donor that had not yet been pooled. Marietta Carr was tasked with discussing with the FDA what would be done “if we do find a donor who comes down with AIDS and we do have plasma in product in the field.”[2430]
In May 1983, Hyland recalled one lot of anti-inhibitor coagulation complex (Autoplex) from the US market and quarantined factor concentrates that contained the plasma of a donor who had been identified with symptoms related to AIDS, including an inverted T4/T8 ratio and generalised lymphadenopathy. In a letter to the DHSS, Hyland stated that the donor was “a member of the high risk groups”, though he had denied this on several occasions prior to donating. The company stated that no products fractionated from plasma pools containing the donor’s plasma had been shipped to customers in Europe. Hyland explained that it had taken this action unilaterally and not at the request of the FDA.[2431]
The following month, in correspondence with the DHSS, Cutter stated that while it had not had to make any decisions about the disposition of a lot of Koate from a donor who developed AIDS, should that occur “It is our plan that ... the decision concerning the lot would depend on many factors including, most importantly, receipt of advice from government health authorities based on the latest knowledge concerning AIDS.”[2432]
A few days later, on 9 June 1983 and at the request of the FDA, representatives of the fractionators met FDA officials to discuss the approach to be taken to future recall of products. By this time the CDC had identified more than 1,500 cases of AIDS in the US of whom 15 were people with haemophilia.[2433] The FDA considered there was a need to develop a policy in a public forum involving the CDC, National Hemophilia Foundation and other interested parties, who were notably not at the meeting on 9 June. According to the Hyland note of the meeting the FDA explained that their position was that:
“the policy must be one which does not interrupt the supply of coagulation products to hemophiliacs or cause a panic condition in the mind of users. Given the degree to which a relatively small number of donations can affect a large number of product lots and the uncertain – but long – gestation period for the disease, developing a policy which is acceptable to the major interest groups is seen as a real challenge.”[2434]
In his note of the meeting, Dr Ojala of Cutter recorded:
“The discussion clearly identified that hypothetical situations could result in major problems in the source of supply of concentrates unless a balanced view of the risk was maintained. For example, if one donor had routinely donated plasma to a single manufacturer over the course of a year, that company’s entire production of coagulation product could be contaminated by the single donor. The consequence of this situation would be a major interruption in product availability.”[2435]
The Alpha note of the meeting also referred to repeated discussion of “the potential for this wiping out a manufacturer totally economically.”[2436]
Despite “considerable discussions”no consensus was reached at the meeting.[2437] The FDA appear to have urged the manufacturers to “recommend a course of action based on what is practical and achievable”prior to the open meeting that would take place in July.[2438] In her note for Alpha, Marietta Carr wrote that: “Dr [John] Petricciani [of the FDA] stated quietly but firmly that he considered it essential that the manufacturers, in presenting their proposal, discuss the feasibility of doing what we suggest, and the potential availability of product. The message is loud and clear. He stated frequently that this is a social, economic, public relations and emotional issue, not a scientific one.”[2439]
Dr Ojala also recorded that Dr Donohue of the FDA was to attend a series of meetings in Europe about the screening processes in the US: “Donahue [sic] stated that his mission was to defend our current procedures. He asked assistance from the manufacturers to convince those overseas that we are doing an acceptable job of screening out any AIDS donors.”[2440]
The open meeting on product recall took place at BPAC on 19 July 1983. Dr Rodell spoke on behalf of the Plasma Manufacturers Association. His contribution is described in this way in the record of proceedings:
“Because the industry estimates that the average frequent plasma donor makes between 40 and 60 donations a year, a single donor could easily be represented in as many as 50 plasma pools in one year. Were this donor subsequently found to have AIDS and a decision made to recall all units collected in a time period of one year prior to that, 25 to 250 million AHF activity units could be affected, all in various stages of pooling, production, and distribution. Given the PHA estimate of 800 million AHF activity units produced annually by the fractionation industry, the potential for serious disruption of AHF supply described by Dr. Rodell seems quite real.”[2441]
Dr Ojala presented the Association’s recommendation, which was that current policies should continue and a policy of automatically recalling products would lead to “serious product shortages.”He argued that “recall decisions should be made following each company’s policy in close consultation with the FDA and should be considered on a case-by-case basis in light of current knowledge of AIDS.”[2442]
Dr Rodell and Dr Ojala were followed by Dr Louis Aledort, who put the National Hemophilia Foundation’s position statement. This had been that products should be subject to recall where a donor was either diagnosed with AIDS or had “characteristics strongly suggestive of AIDS”. However, he stated that the National Hemophilia Foundation did not have access to the Plasma Manufacturers Association data when the statement was formulated, “and that there was great concern about the continued supply of AHF.”[2443]A Canadian Red Cross observer noted that Dr Aledort made his statement “with some degree of embarrassment and actually disclaimed any personal responsibility for it. He stated that personally he feels that the recall position for AIDS contamination should be similar to ... that stated by Steve Ojala.”[2444]In the aftermath of the first withdrawal of products by Hyland in May 1983 the National Hemophilia Foundation had continued to urge its members to use factor concentrates as “the life and health of hemophiliacs depends upon blood products.”[2445]
The warnings of Dr Rodell and Dr Ojala – informed as they were by the earlier discussions in the meeting with FDA officials – had their intended effect, and not just with Dr Aledort. The committee concluded that (emphasis added):
“It was very clear that confronted with this complex problem the Committee felt that a balance must be struck between theoretical risk of the product to recipients against the need for an uninterrupted supply of a life-sustaining therapy. As several members of the panel stressed, it would be undesirable to distribute and use a lot of product which incorporated plasma from a donor with a definite diagnosis of AIDS. However, signs and symptoms suggestive of AIDS (e.g. persistent lymphadenopathy, night sweats, etc.) would not be persuasive enough to dictate a recall of product. Enough concern was expressed about the question of supply that the Committee was unwilling to advise the agency to take an unalterable regulatory position calling for an automatic recall which would likely jeopardize product availability. Adding to the uncertainty with regard to the decision of whether to quarantine or recall a product lot, several Committee members and other participants expressed the opinion that the risk of AIDS from transfusion of plasma derivatives or use of AHF concentrates has not been definitively established. They cited the fact that nearly all the hemophiliacs with AIDS had used material from different lots, and that many other hemophiliacs receiving those same lots had not developed AIDS. They stressed the need for studies to followup recipients of blood products derived from AIDS patients. The consensus of the Committee was that the action to be taken for each incident of inclusion of plasma from a donor who might have AIDS into a product pool should be decided on a case-by-case basis.” [2446]
The “case-by-case” approach remained that adopted in the US despite further withdrawals of products in the autumn of 1983, and the National Hemophilia Foundation restating in October its original position statement that products should be automatically recalled where a donor was diagnosed with AIDS or characteristics strongly suggestive of AIDS.[2447]
At the meeting of 4 February 1984 held at NIBSC the position was explained in the following terms:
“Dr. Thomas asked Dr. Petricianni [sic] whether the FDA had specifically requested the manufacturer to withdraw batches that had been made from an affected pool. Dr. Petricianni [sic] replied that no formal instruction had been issued by the FDA, but the withdrawal had taken place as a result of informal discussion and agreement. The general feeling of the meeting was that if the diagnosis of AIDS in a donor is definite, then products prepared from pools to which the donor had contributed should be withdrawn. If a donor is found to have symptoms and signs, such as lymphadenopathy, which were associated with incipient AIDS, but were neither diagnostic nor specific for the condition, the recall of material to which the subject had previously contributed plasma was not justified. It was recognised that the scientific rationale for this course of action left much to be desired, but that no other action could be taken which would not imperil the supply of Factor VIII.”[2448]
On one reading, the final sentence reflects the position that had been discussed repeatedly in the first half of 1983. The issue was not approached purely as a scientific one, but as a question of policy that took into account concerns about economics and the perceived need to maintain the supply of fractionated blood products.
Another perspective, attributing no force at all to scientific information, is cast by the note of Marietta Carr, who attended the meeting on behalf of Alpha. She recorded that: “The four U.S. market withdrawals were discussed and we explained that we were all still making decisions on a case-by-case basis. The decisions were not being made based on scientific information but simply because of emotional and political considerations. During this discussion it was very emphatically noted that three out of the four market withdrawals involved volunteer donors not paid donors.”[2449]
The purpose of this chapter has been to show how NHS patients in the UK were affected by commercial pharmaceutical companies’ practices in relation to the supply of plasma, choice of donors, use of plasma from high risk groups, pool sizes used, labelling and warnings given about the risks of hepatitis and AIDS, and the response of pharmaceutical companies to the emerging threat of AIDS and to taking measures which might reduce the spread of AIDS.
What the evidence shows is that before 1975 there seems to have been little regulation over the sources of plasma for US manufacturers,[2450] and some was imported – presumably from cheaper sources still than the US urban, socially disadvantaged, sources filmed for Granada’s documentary screened at the end of 1975.[2451] There is little doubt that commercial concentrates imported into the UK were in consequence seriously infective. Moreover, such was the time lag between the manufacture of factor concentrates and their distribution that it is quite likely that cheaper imported plasma[2452] formed the basic material for concentrates distributed into 1977 and 1978.[2453] It shows that two of the major producers sourced plasma from US prisons until the early 1980s; and that surplus material from the use of “hyper-immune plasma” found its way into plasma pools. Warnings about using these concentrates because of the risks of hepatitis, and other viruses which might be endemic amongst these source populations, such as those given by Professor Joseph Garrott Allen in the 1970s were fully justified.[2454]
Different perspectives were given as to the effectiveness of FDA inspection once a requirement began in the mid 1970s for each plasma collection centre to be licensed. Though it may be that in many cases this regulation, based on an annual inspection, was effective, it clearly could not prevent malpractice in some places (such a regime relies upon the threat of removal of a licence being sufficient to ensure compliance through the rest of the year, and necessarily operates “after the event” control if that threat is not taken sufficiently seriously. It would be naive to think that given the value of the product there were not several breaches, and the chapter contains evidence of reports of some.
Pool sizes increased the risk as they grew. They generally contained plasma from a significantly greater number of donors than did UK produced concentrates, and it must be borne in mind that a large number of US donors were likely to sell their plasma at such frequent intervals that the number of donations to a US pool would always be larger than the number of donors to it.
The risks this posed in a system in which one donor might make several contributions to one large pool were dramatically emphasised by Dr Rodell’s presentation on 19 July 1983 that suggested at that rate as few as four donors (infected with the cause of AIDS) could infect the whole world supply of factor concentrate.[2455] Manufacture based on such a large pool had grown too large to be allowed, through regulation and recall, to fail, for the risk that it might leave people with haemophilia without treatment then became too great. The decision to leave recall to be decided on a case-by-case basis, was effectively to permit the distribution of product where there was not only a known risk that it might cause AIDS, but an enhanced risk of this happening. It was almost a year before the first products (commercial ones) heat treated to inactivate HIV were made available on a named patient basis, not yet licensed, in the UK. In the meantime, UK patients remained exposed to risks that products made from those showing some of the symptoms of AIDS or its precursor would be distributed in this jurisdiction.
Pharmaceutical companies did warn of the risks. To the extent that patients in the UK were unaware of these warnings, that was a failure on the part of haemophilia clinicians in the UK to alert them. However, though warnings were given from the very start they did not draw attention to the risks of non-A non-B Hepatitis specifically when that might have been expected, and did not alert a user to the risk of AIDS. The way they were expressed was aimed at clinicians and regulators – so that they depended upon the patient being informed, which (on the evidence) few were, except to downplay the risk. The first of these shortcomings was known to the DHSS, but no regulatory step was taken to require a more specific reference than “hepatitis”. Nor did the UK regulator require AIDS to be referenced. A user – professional or individual – would have to understand from a reference to “viruses” that taking the concentrate risked contracting AIDS. They would have to do so in 1983 and until early 1984 despite the Government regularly repeating that there was no conclusive proof that it was a virus which led to AIDS.
The recommendation by the FDA to pharmaceutical companies not to use plasma obtained from the high-risk sources identified on 4 March 1983 has as a logical corollary that product manufactured from plasma collected before that date was probably of higher risk. This move by the FDA had the status of a recommendation, not a requirement. It led to a requirement to label product with the date on which the source plasma had been collected, but not to a withdrawal of any earlier product from the market. This was despite the recommendation being that pre-March plasma should not thereafter be the base material for any product used for the treatment of haemophilia. The effects on the UK market of the continued supply of “pre-March plasma products” is described in the chapter on Regulation of Commercial Factor Concentrates.
What has been described above should not be seen in isolation. It raises two much wider matters.
This chapter considers the role and influence of the Haemophilia Society (“the Society”) in the 1970s and 1980s and in particular the advice which it provided to its members as to the risks of hepatitis and AIDS. It also looks at aspects of the Society’s campaigning work.
1950 Society is formed and becomes an independent charity in 1964.
1970s Society presses for self-sufficiency in blood products.
19 January 1983 David Watters seeks guidance from Professor Bloom regarding AIDS.
Spring 1983 Society Bulletin has Q&A session from Dr Kernoff who expects AIDS to remain a rare disease.
23 April 1983 Professor Bloom tells Society’s AGM not to get “over-concerned”
about AIDS.
4 May 1983 Rev Tanner circulates to Society members Professor Bloom’s letter in response to the Mail on Sunday article “Hospitals using killer blood”.
12 May 1983 Executive Committee decides its policy is to encourage members to continue present treatment programmes “until there was evidence to prove otherwise”.
15 August 1983 Society requests DHSS not to suspend the importation of US commercial products without definite evidence this is necessary.
September 1983 Haemofact asserts that “the advantages of treatment far outweigh any possible risk.”
Summer 1984 Society Bulletin article states “All things considered, haemophiliacs have no reason to be worried about using commercial concentrates.”
1986 Society takes legal advice on compensation for members and circulates counsel’s opinion to leading clinicians.
November 1987 the Government announces a £10 million payment for the Society to establish a trust (the Macfarlane Trust). It becomes a separate charity.
November 1991 Society’s project team concludes hepatitis “should not be a major concern” such as to justify campaigning.
1993 the Manor House Group starts campaigning for those infected with Hepatitis C infection.
November 1994 Society resolves to seek “maximum help” for those infected with Hepatitis C and “equitable treatment in financial terms” with those infected with HIV.
July 1998 Society’s campaign for compensation rejected by the Government.
September 1999 Society presses Scottish Executive for an inquiry.
January 2001 Society’s objectives are reset: a public inquiry into blood-borne infections, a hardship fund for those affected by Hepatitis C and recombinant for all.
Professor Arthur Bloom chair UKHCDO
Ken Milne trustee, member of the Executive Committee (1979 - 1983), vice-chair
(1983 - 1993), chair of the blood products sub-committee (1983 - 1993)
Karin Pappenheim CEO (1998 - 2004)
Reverend Alan Tanner chair (1975 - 1997)
David Watters coordinator/general secretary (1981 - 1994)
The Haemophilia Society began when, in 1947, two men with haemophilia realised that a mutual support group was needed to bring people who had haemophilia together. By 1950 a society had been formed.
Looking back at these origins in 1998[2456] Reverend Alan Tanner[2457] described how the Haemophilia Society began with a group which met for mutual support, expanded, and then began to look for some kind of base where they could congregate more often and have an office from where they could operate. When a fire station in Southwark became surplus to requirements and was “made available” it was the beginning of the formal organisation of the Society. “It was done by volunteers[2458] supporting each other and beginning to become rather aggressive in their style in relating with their doctors[2459] and dealing with the Government and so on. They began to organize one or two campaigns.”
ln practice the purposes which the Society sought to fulfil[2460] were those of providing support, friendship, advice and information to people with haemophilia and those involved in their care. This was achieved through various publications,[2461] and by encouraging, for example, the formation of professional groups for nurses and social workers as well as local groups of members. Secondly, the Society sought to encourage and support research into the causes, diagnosis and treatment of haemophilia and related blood disorders.
In 1964 it became an independent charity.
Towards the end of the 1960s it lobbied for the increased use of cryoprecipitate, and then recalled of the 1970s “We had seen stories on the television of blood donors in the United States being recruited from Skid Row and we spoke very forcibly to Dr David Owen to let him know that we were not prepared to accept the risk of hepatitis coming from the blood products issued from the United States.”[2462] This would have been very shortly after Reverend Tanner took over the reins as chair,[2463] a role he was to retain, unpaid, until 1997. Reverend Tanner, the vicar of St Botolph’s Bishopsgate, was a figure to whom others paid deference. Though most of the trustees were themselves people with haemophilia, his familiarity with the condition came because he had a son with haemophilia.
From the beginning of his tenure as chair, Reverend Tanner made contact with those in government. He sought to influence policy in respect of haemophilia, as the expression of his view to Dr David Owen demonstrates. Indeed, this was part of consistent pressure[2464] by the Society to obtain self-sufficiency in blood products for the UK. Its concern in doing so was sparked by knowledge of the risks to patients from hepatitis, and of the fact that the World Health Organisation (“WHO”) had advised that self-sufficiency was a goal to be pursued. The Society also envisaged that with increased domestic production sufficient quantities of factor concentrate would be both more consistently available, and also cheaper for the NHS. This would reduce the general financial obstacles which stood in the way of improving the availability and development of therapies for people with haemophilia. Being convinced that the whole of the necessary supply should be produced from local sources (a medium-term aim) the Society did not give any detailed consideration to the ways in which risks posed in the meantime by imported commercial concentrates might be reduced. It did not, for instance, advocate for patients being informed of the differing risks related to treatment choice, nor ways of reducing the need for so much commercial concentrate to be obtained, for instance, by a change of emphasis in therapy. The trustees thought that the members would not welcome a move away from the use of factor concentrate, nor a reduction in home therapy, nor a reversion (as they saw it) to cryoprecipitate.
Many high profile figures leant their names to the charity’s work: Wilfred Pickles, a famous media personality of the day, was vice president for some seven years in the 1950s; as was Professor Gwyn Macfarlane, from 1954 until 1987, when he died after a lifetime of achievement in developing scientists’ understanding of haemophilia and its treatments; it was after him that the Macfarlane Trust[2465] was named. HRH Duchess of Kent became patron in 1973 and for many years the author Catherine Cookson was a vice president. The association with so many distinguished personalities lent clout to the public perception of the Society, and to their campaigns. It may also have created a perception that the Society was a large organisation.
Such a perception was misleading. In truth, the Society functioned with a very small staff. It employed a secretary from January 1953 onward, supported by an assistant or temporary secretary from time to time, and a public relations officer in the 1970s. David Watters became its first employee in the post of coordinator/general secretary (the role was initially called the former though the functions were the same). He described how, when he joined the Haemophilia Society in 1981, there were two part-time secretaries who worked mornings only, as the only paid employees in addition to him.[2466] He described to the Inquiry how at the outset his (paid) role was regarded with suspicion by a number of trustees.[2467]
Though the Society regarded itself as the mouthpiece of its individual members (and others, including government, saw it that way) this too could mislead: it was not an organisation in which the grassroots usually had any direct influence on what the central body – the Executive Committee – had to say. It was, instead, governed top-down.[2468] There were a number of regional groups, of varying size and effectiveness, which tended to be concerned with their particular local issues and local fundraising rather than with national policies. Two members from each regional group formed a Council which met with the Executive Committee two or three times a year.[2469] They did not necessarily see eye to eye with the Executive Committee.[2470] It was the members of the Executive Committee who formulated policy, not the Council.
Though it was the only national organisation which spoke on behalf of people with haemophilia (though for the reasons just given it tended to assume it knew what they would say, rather than collecting their views systematically) not all people with haemophilia were members. David Watters said in his statement that only a minority of individuals in the UK who were living with haemophilia were members.[2471] Part of the perspective of the Society was shaped by the personal experiences of the trustees, who attended the bigger centres in London and were not attuned to the predicament of those who attended outpatient departments in local hospitals elsewhere.[2472]
The scientific and medical information it received during the 1970s and 1980s was limited, in part, because of its small size. The sources were The Lancet and The British Medical Journal which, though received, were rarely read,[2473] together with what could be gleaned from contact with similar bodies in other countries – in particular the Irish Haemophilia Society, and the National Hemophilia Foundation in the US – and the information which some haemophilia clinicians in the UK offered either directly, or through personal contact with a trustee.[2474] It resulted in what David Watters summarised as, in effect, a “lack of outreach and a lack of grasp of big issues”,[2475] at least at the time he began to work for the Society, though his appointment came just after Society committee members had attended the First International Conference on Haemophilia held in Bonn in October 1980.[2476]
The office was close to the Department of Health and Social Security (“DHSS”) headquarters at the time. There were regular meetings with the civil servants principally responsible for blood products and supply. In the early 1970s a focus became a drive to secure self-sufficiency, to ensure a sufficiency of product to meet the needs of all people in the UK with haemophilia, without the need for foreign products. From 1981, central issues were supply and self-sufficiency; and from 1983 onwards AIDS became a primary topic. Seeking compensation then took over centre stage. Access to ministers, however, was relatively limited, generally to junior ministers.
In respect of treatment and infection, the Society principally relied upon the advice given to it by its Medical Advisory Panel.[2477] This met infrequently, if at all, as an actual panel.[2478] Rather, it was a list of clinicians who were prepared to advise the Society from time to time, if asked. David Watters described the panel as having consisted “to some extent at least of ‘favoured’ Reference Centre Directors”. By “favoured” he meant well known and long-serving. It was not as wide a panel as it might have been, because those who tended to serve on the panel were those who had a particularly close relationship with the Society. David Watters described it in evidence as being “rather like The Haemophilia Society when I came. It was a very inbred organisation, with a group of people who had been around for a very long time together, and the list of eight people listed below kind of summarises the situation with the Medical Advisory Panel.”[2479] In his view, the panel was too large, lacked terms of reference, and the members of the panel were always defending the position of the UKHCDO rather than advising the Society (there being a difference, as he saw it). The Society in turn was unable to “capitalise on the valuable resource” which could have been available to it. It was, he said, “more interested in maintaining a friendly relationship with those powerful clinicians”.[2480]
David Watters became concerned that the Society was not getting the best, unbiased opinions. A constant problem, given the facts that seniority and service in a large centre were likely to be reflected in membership of the Panel, was that the principal source of information for the trustees, both from fellow members of the Executive Committee and from the Panel, related to the reference centres and not to the smaller centres. In the 1980s appointments to the Medical Advisory Panel were, in his view, nepotistic. Concerns about independence, possible bias, and that clinicians on the Panel took an overly conservative approach to emerging threats – allied to a sense that turnover in its membership was so low as to be unhealthy – led eventually to a review of the panel in 1991.[2481]
By taking advice only from senior members of UKHCDO, the Society at the time effectively disabled itself from scrutinising the treatment policies and recommendations made by UKHCDO, though there was an awareness that some younger haematologists might have had a different approach.[2482]
It followed from David Watters’ testimony that in the early to mid 1980s the Society placed a heavy reliance in particular on the views of Professor Arthur Bloom who was not only chair of the UKHCDO at the time but a principal point of reference for the Society when seeking advice. This view is confirmed by the testimony of Peter Wetherell, a member of the Executive Committee from April 1983 until June 1985.[2483] In its closing submission to the Inquiry, the Haemophilia Society accepts that this was the case.[2484]
The Society picked up its first information about the threat of AIDS in late 1982 or the start of 1983. On 19 January 1983 it sent an article which had appeared in The Observer to Professor Bloom and asked for guidance.[2485]
Professor Bloom’s response recognised that AIDS had become a “rather serious”disease in the US, but “at the present time the cause is quite unknown and neither has it been proven that it is transmitted through contaminated blood products. The incidence of the condition in America is not known but seems to be about one per thousand of the severely affected treated patients. On this basis if the disease exists in the UK we could reasonably expect two or three cases amongst British haemophiliacs. So far none have been reported.” He suggested that there was “certainly no need for the haemophilic community to be unduly concerned about this ‘new’ syndrome”,and also noted that: “Further developments will depend upon identifying the responsible agent or constituent of concentrates, if it exists, and no doubt then steps can be taken to attempt to eliminate them in much the same way as steps are being taken to reduce the risks of hepatitis.”[2486]
This was a “wait and see” approach.[2487] Moreover, to appear to equate the risks of acquiring AIDS with the risk of hepatitis[2488] and to suggest that similar steps as those taken to reduce that risk (steps which were slow, taking a very long time to reach fruition, had led to no change of therapeutic approach, and had been amplified in the case of domestic blood products by the increasing size of pools used for manufacture) should be adopted, was a completely inadequate response to a disease which caused the fatalities it did and which had spread among – and beyond – the gay communities in which it was first recognised with such increasing speed as to become an epidemic.[2489] These words, which played down the risk rather than suggesting that something might be done to combat it, fell on receptive ears amongst the Executive Committee.[2490] It is clear that the trustees did not face up to the risk of AIDS seriously enough: they preferred to regard it as a purely American phenomenon of little likely impact in the UK. David Watters recalled a meeting at the Kennedy Hotel by Euston Station where Clive Knight[2491] and he had great difficulty persuading the others that AIDS was going to be a problem: “Things were being said like, ‘Oh, you know, we don’t have bath houses in the United Kingdom like they have in the United States’, and we [Watters and Knight] were saying ‘No, but we are certainly using the same blood product’.”[2492]
The Society communicated with its members through concise publications including The Bulletin. In its first Bulletin of 1983 (edited by Clive Knight) was a “question and answer” session with Dr Peter Kernoff, who said that there had been no reported case of AIDS among British people with haemophilia and although it was possible that they could get AIDS “I’d still expect AIDS to remain a rare disease. The idea that there is an epidemic of AIDS amongst haemophiliacs is ludicrous.”[2493] Though the Executive Committee may not by then have discussed the issue,[2494] a talk was given at its AGM on 23 April 1983 by Professor Bloom. This touched on AIDS.[2495] In a question and answer session from the AGM as reported in The Bulletin, Professor Bloom said: “It is unfortunate that haemophilia has been linked with AIDS. Apart from that we must not overlook the AIDS problems. One of my patients may have a mild form of it. Some patients show laboratory changes. Laboratory changes do not mean that it is a serious disease.[2496] I do not know of any haemophiliac with AIDS in the UK, France, or Germany. I do not think we need to get over-concerned about this. At the present time it would be absolutely wrong to curtail treatment.”[2497]
What did make the Society’s Executive Committee react to the questions posed by AIDS was the publication on 1 May 1983 in The Mail on Sunday of an article by Susan Douglas with the front page headline “Hospitals using killer blood”, which referred to two people with haemophilia suspected to be suffering from it in the UK.[2498] On the Sunday morning of its publication Reverend Tanner contacted David Watters. They agreed to consult Professor Bloom about what was being said in the article. He responded on 3 May[2499] with a letter designed for publication to the membership.[2500] Reverend Tanner had it circulated to the entire membership of the Society on 4 May without his actions in doing so having been approved by the Executive Committee beforehand. When the Executive Committee next met, on 12 May 1983, the decision was taken unanimously that “until there was evidence to prove[2501] otherwise”[2502] the Society’s policy would be to encourage members to continue with their present treatment programmes, subject to the advice of their centre directors: Peter Wetherell observed in evidence that it was effectively a fait accompli – by publication of the letter the decision had effectively been taken, and the policy of the Society determined.[2503]
It is clear that the Society was not given the full facts which Professor Bloom knew, including that on 26 April 1983 he had reported one of the two patients referred to in The Mail on Sunday article to the Communicable Disease Surveillance Centre in the UK as a probable case of AIDS.[2504] What he said was neither faithful to the facts, nor to the epidemiology, nor did it reveal what he had been told by others who were better placed to know than he was.[2505] The Society today regards his behaviour in misleading the Society and its members as he did as “unfathomable”, and I agree.[2506] His views nonetheless shaped the Society’s direction of travel.[2507] Professor Bloom was heavily influential, and the Society at the time knew no better.
However, the Society had not sought and did not seek advice from anyone other than Professor Bloom at the time (though it did obtain another view a month or two later).[2508] The extent of his influence over the Society is demonstrated by a letter of 25 July 1983 in which he enclosed a letter which Dr Charles Rizza and he had circulated to haemophilia clinicians and said “I do not think it would be appropriate to circulate this letter to the membership at large.”[2509] It was not medical advice, and he had no executive power, but it demonstrates the extent to which he considered he had influence, and thus is itself evidence of his influence.
In the light of Professor Bloom’s downplaying of the risk, the trustees regarded the risk of AIDS as being “just one more [risk] that severe haemophiliacs had to accept”.[2510] It adopted this approach despite knowing that the Irish Haemophilia Society was “under the impression that the risk of AIDS is being played down” and was seeking to press the Irish Government to use products made in Ireland to decrease the risk of American commercial products.[2511] The belief of the Executive Committee (which in retrospect appears more of an article of faith[2512]) that any form of haemophilia was more dangerous than AIDS seems to have taken hold on 4 May 1983 and been close to unshakeable thereafter. The Society did not support any ban on the importation of commercial concentrates from the US, and added its influence to those who opposed it. It was not alerted to the Council of Europe Committee of Ministers’ Recommendation in June 1983 to avoid where possible the use of factor products prepared from large plasma pools,[2513] despite frequent contact with the DHSS, which was well aware of it. Nor did it know of concerns raised by the Communicable Disease Surveillance Centre[2514] less than a week after Professor Bloom wrote his letter.
When the Society became aware of cases of AIDS in people with haemophilia being reported elsewhere in Europe, it asked Professor Bloom (in July 1983) whether he wished to say anything further to the views he had expressed in the letter circulated to members on 4 May.[2515] Professor Bloom responded that he did not regard there as having been any major change.[2516]
In August 1983 – anticipating a meeting with Lord Glenarthur on 8 September – the Society wrote to say that there should “be no attempt to suspend the importation of US Commercial Products [without] definite evidence that this would be necessary.”[2517]
By 8 September 1983 the Society had become aware of the death of a person with haemophilia from AIDS and began to question whether a synthetic product might appear more sensible.[2518] Ken Milne expressed the view that not suspending imported products was now a “shakier position” than when first agreed as the policy.[2519] However, those doubts do not appear to have been expressed to the membership at the time. Nor did the Society choose to lobby against the dumping in the UK of stock made from “pre-March” US plasma which was believed to be riskier than product manufactured from plasma collected after March 1983. It did not, as it could have done, use the September 1983 edition of Haemofact to warn members that their centre might be using stocks of blood product manufactured from plasma collected prior to March 1983,[2520] and that they should ask questions and seek to have only post-March blood products given to them. Nor did it advise treatment policies which would have lessened the risks of infection whilst maintaining protection against the worst bleeds. It continued to adhere to its position that “factor VIII concentrates must continue to be imported from the USA”.[2521]
Having been initially dismissive of the risk of AIDS in early 1983, reaffirmed in that view by communications and interactions with Professor Bloom, by the end of September that year it was sufficiently concerned about the risk of AIDS to its members that it chose to allocate £17,000 for AIDS research (a large sum for a small society) whilst calling upon the Government to devote more money still than it had already committed (a third of £1 million) for the same purpose.[2522] In his evidence Peter Wetherell described how by the time of a Society’s Council Meeting of 8 October 1983 “the penny had pretty well dropped” (at least with the membership) that a crisis was looming. He described orally that it dawned that there was an awful possibility that damage had been done, the “Grim Reaper was lurking in the room”, and that Professor Bloom was downplaying the issue.[2523] In December the Executive Committee had it confirmed that the Cardiff case was indeed one of AIDS, but no questions were asked of Professor Bloom about this.[2524]
In short, the Society woke up too late to the threat of AIDS; its Executive Committee needed to be persuaded to take the risk more seriously; and it relied very heavily indeed upon the views of Professor Bloom without question, even when questions were obvious. By July 1983 it was prepared to question whether those views might have changed, and by September was less sure of the validity of a decision not to ban the imports of foreign concentrates.[2525] But it still did not yet begin to advocate any change in its previous advice to carry on taking the treatment as before. It was still some time before the Society started to regard AIDS as a really serious risk.
Whether the information provided by the Haemophilia Society to its members was intended to be relied on, and precisely how, and whether it was actually relied on were matters upon which words were often carefully chosen by witnesses, but inherent contradictions remain. The purpose of giving information was said by Simon Taylor (a member of the Executive Committee for the first time 1985-1988) to be to “enable and empower people with haemophilia”, but when asked what weight such people were putting on the information it was “not a lot”; and the central question remains: why give out information as a responsible society to “enable and empower” members if it is not intended that they place reliance on it? Simon Taylor did accept that by 1986, at least, the Society was “seeking to be an authoritative voice on AIDS and haemophilia to both members of the Society and the wider public” and that by 1991 the Society’s publication “Essentials of Haemophilia Care” also set out to educate district health authorities.[2526]
David Watters was asked in evidence: “Q. Would you regard the following as a fair criticism of the Society in relation to 1983, that it saw its role predominantly as one of allaying concerns rather than ensuring that members were properly informed of all risks? A. I wouldn’t agree with that entirely. I mean, we were concerned to allay concerns but we were also keen to advise of known risks, established risks.”[2527] Yet he also accepted that “looked at broadly, the Society’s message during 1983 to its members was that very strongly they should keep treating themselves with factor concentrates? A. Yes, subject to the advice of their own Haemophilia Centre Director.”
In the light of what were known to be risks, there might have been consideration of “what can be done to reduce these risks?” (such as modifications to treatment regimes) about which members might usefully have been informed, but there is little evidence of the Society adopting this role in the early to mid 1980s.
Wishful thinking remained a feature in some of the trustees’ actions. For instance, the September 1983 Haemofact – described as a “fact sheet” – noted that “Blood collection in the USA has been improved to the satisfaction of the Federal Health Authorities and our own DHSS. Assuming blood to be a transmission agent, it is not yet possible to state that imported blood products are AIDS-free (nor indeed that UK product is so), the chances are that the risk involved in imported concentrates has been reduced considerably.”[2528] There does not appear to be any factual or evidential basis for saying this. Moreover, the Society knew from Lord Glenarthur that product made from plasma collected before any of the improvements in screening of donors which had “satisfied” US federal health authorities was still being made available in the UK. There is no hint of this in the Haemofact, as there might well have been. The position of the Society, and indeed David Watters, is demonstrated by the following:
“Q. You could have made clear to members in the course of 1983 that it was likely that AIDS was transmissible by blood and blood products.
A. I think that would have possibly been a slight overstatement, that - and we were always looking to the fact that what were the alternatives? Were there real alternatives?[2529] Were there tangible alternatives that could be made available, that would be as effective as Factor VIII? … I think we went as near to saying that as we felt we could comfortably say.
Q. You could have spelt out to members that AIDS itself was a disease with a long incubation period and high mortality rate.
A. We didn’t know that to be the case in haemophilia.[2530]
Q. You could have conveyed uncertainty about how many might be infected, rather than a strong message or steer that very few would be infected.
A. If that had been advice we were being given by those equipped to give us advice, we should have followed that advice; we would have followed that advice.
Q. You could have spelt out to members, or advised members generally, that they might want to raise with their clinicians alternatives to factor concentrates and explore that with their clinicians.
A. All our publications said ‘Discuss this with your own Haemophilia Centre Director’ … As I say, if we had known of a viable alternative that could be produced in large quantities and been capable of meeting the needs of the community, we would have been publicising that.
Q. Do you know if the Society gave any particular consideration in the course of 1983 to the position of those who were mild haemophiliacs or moderate haemophiliacs, and whether it considered if different advice should be given to those cohorts of patients?
A. We would have assumed that that cohort of patients would already have been receiving a priority for home-produced product, and things like that, and that was a reasonable assumption to make, given the decisions made by the Haemophilia Centre Directors Association and the Reference Centre Directors.
Q. I think you referred in the course of your evidence to an understanding that there wouldn’t be sufficient quantities of cryoprecipitate. What was the source of your understanding, or the Society’s understanding, about the availability of cryoprecipitate, which we understand to have varied regionally in 1983?
A. It was, first of all, a very clumsy material, as far as I understand, that lacked the convenience of ready infusion and required storage in freezers and such. But the advice would have come via the Blood Products Sub-Committee from BPL, and from the blood services.” [2531]
Without detracting from the picture painted by the answers as a whole, which is of a “head in the sand” attitude, the first two responses are of particular note. The first implies that a reason for not telling members of the likelihood that the cause of AIDS was transmitted by blood or blood products was that there was no alternative therapy. That is not a good reason for failing to tell people of a risk, so that they may decide for themselves whether this is so in their own case. The first and second both betray a desire to minimise the seriousness of AIDS: there was no good reason to think that the natural course of the condition if it occurred would be any different merely because the patient concerned had haemophilia.[2532]
Some four months after Peter Wetherell identified a sense of gathering doom, during which the advice given to members had not changed, the Executive Committee agreed unanimously in relation to AIDS that “until the situation became clearer in relation to blood supplies, it would be wise for the Society to ‘wait and see’.”[2533] In short, little that was proactive was done.
The Executive Committee had not been told that it had by now been reported authoritatively from the US that the wife of a person with haemophilia was reported to have developed AIDS, suggesting that it was sexually transmissible, as well as transmissible by transfusion of blood or blood products.[2534] It would be optimistic, sadly, to think that if it had been it would have taken significant steps given the “head in the sand” attitude it had adopted.[2535] Thus, there is no evidence that the Executive Committee discussed an editorial in The Guardian on 2 November 1983[2536] which at the second paragraph introducing a page-long report on AIDS said “Our own Government’s response to what may prove a major medical and social problem here has so far been slow and insufficient … Mr Norman Fowler may soon have to explain convincingly why he has maintained his decision to depend largely on American Factor VIII blood for Britain’s haemophiliacs, instead of continuing to buy from countries where AIDS is not prevalent, or seeking to become self-sufficient”and in measured tones summarised the position as being that “Most study suggests that Aids is not highly infectious and only transmissable [sic] through most intimate or prolonged bodily contact.”[2537]
By contrast, Ken Milne (who became the vice-chair of the Society in 1984, and served for ten years) wrote an article entitled “Blood Products” in The Bulletin in 1984.[2538] In it he said: “We have no evidence as yet [as] to whether AIDS may be acquired more readily from commercial Factor VIII than from the NHS product but, of course, if AIDS becomes established in the UK then NHS blood and plasma supplies are just as likely to transmit AIDS as commercial concentrates. All things considered, haemophiliacs have no reason to be worried about using commercial concentrates.”[2539] It is surprising that this was cleared for publication, for on careful reading it makes little sense. The second sentence assumes that the risk of AIDS from pooled concentrates is linked to the underlying incidence of infection in the donor population, and assumes that AIDS is not yet established in the UK as it is in the US. It must follow logically that the risk is higher from products made in the US from US donors where the disease is established. It ought to have followed that the Society should have advised its members that NHS concentrates were safer for now, albeit not completely safe.[2540] The acceptance of this for publication demonstrates a lack of careful thought, or a blindness to the risks to which members were subject.[2541]
Even in the December 1984[2542] and April 1985[2543] editions of Haemofact the Society advised “everyone with haemophilia, however mildly affected,[2544] to continue to accept medication as prescribed by medical staff”.[2545] There was no caveat advising those with mild haemophilia, or those who were parents of youngsters with haemophilia, that they should not be treated with large pool Factor 8 concentrates without there being special reason.[2546]
Indeed, the 1984 annual report of the Society (published in mid 1985)[2547] said: “One subject dominated all others in the Society’s work during 1984 when we became increasingly aware of the serious problems arising from the transmission of the acquired immune deficiency syndrome, known as AIDS ... The Executive Committee has seen its main responsibilities as being in keeping members informed about developments and in emphasising its policy that: [italicised] ‘the benefits arising from the continued use of blood products far outweigh any risk involved with regards to AIDS’.”[2548]
The only detailed consideration given to AIDS[2549] in 1984 (apart from considering the paper from the Blood Products Sub-Committee mentioned above in February) was at a Council meeting of 24 November.[2550] It was the first item on the agenda: the upshot appears to have been that “nothing had changed”, although it is apparent that the Society was urging the Government to import supplies of heat-treated products without delay and irrespective of cost.
By March 1986 the Society turned to seeking compensation, urgently, for the people with haemophilia who by now were known to have been infected with HIV. The campaign involved sympathetic journalists, media, letters to MPs and meetings with ministers.
It sought legal advice as to claims for compensation. It then published the fact in its annual report for 1986 that it had done so, under a bold italicised heading: “Compensation”.[2551] Not only did it then state that the advice was that the Society itself could not pursue a case on behalf of its members,[2552] collectively or individually, but went on to add that on the present known facts and in the light of Counsel’s advice the prospect of the majority of claims by individuals succeeding was remote, for two reasons – the difficulty of proving negligence, and that of identifying the proper body or person from whom compensation should be sought. Though it might be understandable for the Society to relay the advice that it, as a body, had no standing to sue (since some members may have wished it to take a stand on their behalf and they needed to know there was no legal right for it to do so) it is not immediately obvious why it should wish to sabotage the chances of its members individually doing so, which might seem to be the effect of this.[2553]
What therefore at first sight seems an extraordinary act, for a Society which had resolved to pursue compensation for its members, yet might now be seeming to torpedo any realistic chance they had of it, was not the only aspect to raise eyebrows. There were two other remarkable features of what happened.
First, even before the annual report was published, the Society wrote to Professor Bloom, with copies to Drs Aronstam, Colvin, Forbes, Rizza, Jones, Mayne and Tuddenham enclosing a copy of Counsel’s provisional (negative) opinion and the Society’s commentary on it.[2554] When it was suggested by Counsel for the Inquiry to David Watters that it was “somewhat odd” for a society trying to do its best to get compensation or recompense for individual members to share its negative advice about the prospects of litigation with those who were amongst the most likely to end up on the other side in the litigation, he accepted that – albeit with hindsight – the point was well made.[2555]
Second, this was compounded by the Society sending what it called a “submission” to the Government in October 1987, in which it repeated that it had been advised that “claims for compensation as such are most unlikely to succeed because of the difficulty of proving negligence.”[2556]
Why did the Society do this? Piecing the evidence together, and making the assumption that the trustees sought honestly to do their best[2557] for members of the Society generally, there was some reason behind it. The strategy was to place heavy emphasis on a moral claim for those who, as a cohort of people with haemophilia, were already uniquely disadvantaged even before, through no fault of their own, they were given infections by NHS treatment. Part of the reasoning was that it would be a long drawn out process before a legal case (or cases) reached a conclusion. It was feared that most sufferers would not be alive to claim the fruits of victory if it were won. It might further risk their health if they were to take part in protracted litigation. Moreover, to pursue a legal case was thought likely to lessen significantly the chances of receiving any interim financial support, though people had a pressing need for it, because making any payment even of an expressly ex gratia nature could invite awkward questions for the government. It would be defending potential claims. Making any payment at all might be seen as accepting responsibility for what had happened, whereas the defendants would be saying they had none. It must have seemed likely therefore that no support payments would be made in advance of a court judgment. If the plaintiffs were to lose their cases, the court’s decision that there was no liability might lessen the chances they would get any meaningful ex gratia support, if indeed anything at all were paid. This view might be summed up as amounting to “a bird in the hand being better than two in the bush”.
On this basis, taking the step of telling the Government it was likely to win any challenge in court was more likely to secure some money, and sooner, for a greater number of people, even though the amounts received by any individual would be nowhere as great as their individual success in litigation would ensure. It was not unreasonable to adopt this strategy, though it might have been preferable simply to point to the difficulties in the way of success (leaving open at least some possibility of it) rather than express a considered legal view that in the light of those problems there was no chance.[2558]
It happened that the strategy almost certainly resulted in sufferers receiving some money much earlier than they otherwise would have done, and did avoid the risk that individuals might fail altogether in their claims. It was bold, but it worked – to an extent.
However, the strategy aimed to secure some funding for immediate needs from the Government, not from clinicians. The act of sending Counsel’s negative opinion to several leading haemophilia clinicians remains an indefensible action, potentially harmful to some members of the Society whilst giving no benefit to the others. The clinicians were not going to be in a position to provide some money on a gratuitous basis to those infected or those close to them. No justification for circulating the adverse opinion is apparent to the Inquiry. Nor is it, as David Watters suggested, that only hindsight reveals this as a “somewhat odd” thing to do.[2559] Anyone with a working knowledge of business and law, as the trustees must be assumed to have had, or even common sense, would understand that handing round to third parties an adverse opinion which was confidential to the Society – thereby waiving any right to confidentiality over it[2560] – without being clear as to the benefit in doing so was completely misguided.
The campaign had some success when, after only a short time, the Government announced (November 1987) that a payment of £10 million would be made to the Society to enable it to establish a special trust fund. The Society was appreciative of this, but not content with it. It headlined its next Bulletin with the words “It’s a Start”, and in December Haemofact announced “The Campaign Continues”. As a result of the early success, it had established “a moral obligation”[2561] and felt it could expose the inadequacies of what had just been provided, as well as securing a weekly benefit payment and speedier DHSS procedures for established benefits, and possibly life insurance and mortgage protection.[2562]
The strategy did not succeed at first. Nearly two years later, however, the Society revisited the issue of compensation. On Newsnight in June 1989 David Watters announced that some 250 individuals had brought claims for compensation; the Society had reviewed the situation, and now believed that “the Government must recognise the need for compensation NOW rather than in five to ten years’ time.” There being “strength in numbers” it urged members to register their intention to claim, and offered to give them contact details of lawyers local to them.[2563]
By November that year, Reverend Tanner and David Watters (together with the Society’s adviser on parliamentary lobbying) met Strachan Heppell, a senior civil servant. They were recorded as expressing the Society’s interest in achieving an out-of-court settlement,[2564] provided the level met with the approval of the plaintiffs’ solicitors. Despite that, they went on to say that the Society’s present view “having consulted lawyers” was that “a sum of £120 million … would be required to bring legal action to an end.”[2565] Matters progressed. In November 1989 David Watters was recorded as having phoned the Department of Health to say that “having again consulted with their lawyers the sum of £86 million … would be required to bring legal action to an end.”[2566] This has all the hallmarks of a negotiation being conducted through a (partial) intermediary.
Just over a year later, widespread speculation that an out-of-court settlement of the claims might be imminent emerged. It led to the Society sending an urgent message to all its members.[2567] This told them that the Society was not and could not be involved in negotiations about a settlement despite speculation to the opposite effect.[2568] It then went on to say that the role of the Society throughout had been to make it politically expedient for the Government to “settle our case”[2569] out of court now rather than in three or four years’ time, and that money “paid out now is guaranteed, whereas there are certainly no guarantees associated with the final outcome of the legal case.”[2570]
What is the overall effect of this evidence? Though legally the Society had no interest in the outcome of a case being litigated between others, and no power to agree a settlement decisively, it is an inescapable fact that it did involve itself (probably as a friendly go-between) in settling the litigation, and using such influence as it had to help achieve that end.
The first record of the possibility of campaigning on behalf of members who had been infected with hepatitis by their treatment is in Executive Committee minutes of January 1990. David Watters was tasked with looking into the position.[2571] By June 1990 it was recorded at a meeting of the policy committee that the Society was neither for nor against pursuing such compensation. This committee felt that the Society did not have sufficient resources[2572] nor did it have the “co-operation of Centre Directors”.[2573]
It seems to have been over a year later before the question was revisited – a project team was then set up to identify “possible areas of action”, to inform and support members with hepatitis, but on the question of compensation it was noted that where individuals wished to pursue claims for compensation the Society was doing no more than refer them to an appropriate lawyer.[2574]
On 14 November 1991 the project team reported. It concluded that hepatitis “should not be a major concern for the Society. 80% of people infected with HCV and HBV would show no clinical signs[2575] and the treatments available were limited; the understanding of the progression of liver disease[2576] could only be established through liver biopsies, now considered unethical. The team felt that the Society was in danger of creating concern and worry where they need not exist. Publicity and high press coverage would be out of proportion to the threat that actually existed.”[2577]
This express desire to allay distress and prevent worry seems to echo that which underpinned the Society’s actions in respect of AIDS in the first half of the 1980s.[2578] It suggests that the Society was speaking forits members rather than to them;[2579] it downplays the significance of the infection.[2580] David Watters observed in his written statement (albeit with the benefit of hindsight) that the Society may not have pursued claims for compensation for hepatitis with the enthusiasm it should have done.[2581]
However, the Society’s position speedily evolved. Though first disbanded after its lukewarm report in November 1991, the project team was re-established as the Hepatitis Task Group in the middle of 1993.[2582] It began to plan public events to draw attention to hepatitis, such as the first Hepatitis Awareness Day in February 1994. A legal “brief” was to be prepared.[2583]
However, the Society was initially hesitant to contemplate campaigning on issues related to members contracting hepatitis through their treatment by the NHS.
The first campaigning group for those suffering with Hepatitis C infection was the Manor House Group.[2584] It grew out of conversations at a conference of the Haemophilia Society in 1993, and drew together a number of people who had separately expressed concern (for some years) that fellow members of the Society were dying because of Hepatitis C, and that no one seemed to be doing anything about it. It grew to over 300 members, but although it sought support from the Haemophilia Society it initially had none. However, it was invited to join the Hepatitis Task Group set up by the Society, became a special interest group of the Society[2585] and was allocated time at the annual conference of the Society in 1995. It succeeded in arranging a meeting with Stephen Dorrell, the Secretary of State for Health, in 1995, again a “first” amongst campaign groups in respect of Hepatitis C.[2586]
It was the early activity of this group that led to active reconsideration by the Society in 1994 as to campaigning for support for those with Hepatitis C. Concern was expressed in the Service Committee of the Society that “the Society would have to be seen to be actively dealing with the issue of hepatitis otherwise members such as the Manor House Group may approach the press themselves”.[2587] Two days later the front page of The Independent carried the headline “Contaminated blood kills 12: Doctors believe 5,000 adults and children have caught liver disease from transfusions and clotting agents”. Simon Taylor, by now vice-chair of the Society, was quoted as saying “because the information about hepatitis C is so slight we are not sure which way we should proceed … one thing we are considering is seeking compensation when people become ill”.[2588] On the same day, though, the Society issued a press release which said “We have no plans to seek compensation from the government, our priority is to ensure help and support for people who are unwell as a result of hepatitis C.”[2589]
However, the Society still blew hot and cold on the issue. A later review of the media campaign assessed that “The report in the Independent brought down a media storm on the Society … the Society was largely unprepared. It did not have the information it needed on hepatitis C and had not considered launching a campaign. As a result the Society took the cautious route and made holding comments. With hindsight, this was a major opportunity missed by the Society. Had it been in a position to jump on the media bandwagon it is quite possible that a campaign with limited objectives could have been successful within a few short weeks.”[2590]
It may have been (as one written statement suggests) that since the haemophiliac community had endured significant stigma during its recent campaign over HIV, many members of the Society did not wish to “undergo further media torment”.[2591]
Nonetheless, just two months later a campaign group was meeting.[2592]
There was little early sign of success. A new CEO, Karin Pappenheim, was appointed with effect from March 1998. At the outset of her appointment she was given to understand that the campaign was a very high priority.[2593]
Moves to push the issue of payments to people with haemophilia infected with Hepatitis C higher up the government agenda had some initial success. They led to a debate in the House of Lords; the strength of a moral case that infection with Hepatitis C through NHS treatment deserved recompense, without further delay, was stressed. There was a “day of parliamentary action” on 22 July 1998, a mass lobby, a question was put during Prime Minister’s Questions, and a petition presented to the Government. There was a meeting with a junior minister in the House of Lords. There was complaint that Frank Dobson had promised ten months earlier to give a speedy response, but it had not yet come.[2594]
When the response then came it was negative.[2595]
The Society expressed its determination not to give up despite this huge setback. It began to focus more on securing a public inquiry, which in turn it hoped would raise the profile of the issues on which the campaign had centred. It also recognised the opportunities presented by the consequences of devolution: that now each of the devolved nations had the power to determine health policy and were free to establish their own financial assistance schemes.[2596] In particular, it was able to point to the delay in Scottish production of a Factor 8 concentrate treated so as to be free of Hepatitis C when compared with England. Scottish Ministers[2597] appeared receptive. Susan Deacon became Minister for Health and Community Care in the Scottish Executive upon her election to the Scottish Parliament in May 1999. Although she was advised in an early briefing paper to follow her predecessor in rejecting the Haemophilia Society’s claims for financial support for its members who had been infected with Hepatitis C, she told the Inquiry she had not wished to sign the pre-prepared letter of rejection without at least meeting delegates from the Society.[2598] Further impetus came when she learned that the BBC were planning to run a story on 6 August 1999 on claims for compensation for people with haemophilia in Scotland who had been exposed to risks of infection for over a year longer than their English counterparts because of delay in introducing heat-treated NHS concentrates in Scotland.[2599] She made a commitment to re-examine this Scottish-related issue, part of which was her proposed meeting. The meeting occurred on 14 September 1999 – the chair, vice-chair and chief executive attended for the Society along with a Scottish representative.[2600]
Although the conclusions of the limited internal inquiry, when its report was finally published in October 2000, were condemned by the Society as being “thin” and not well enough based[2601] and although nothing came directly from this passage of events, the pressure the Society put on the Scottish government was a significant factor in what was to occur.
In January 2001 there was a campaign review, and the objectives were reset – more clearly seeking (a) a public inquiry into blood-borne infections; (b) a hardship fund for those affected by HCV; and (c) recombinant for all.[2602] It was also an aim to achieve “the best treatment and care for people with haemophilia and related bleeding disorders infected with HCV”.[2603] Recombinant for most was eventually achieved; but not (initially) the other two aims. An agency was hired, at considerable cost, to steer the campaign.[2604] Success proved elusive, and was costing more than the Society was willing to continue funding. Activity was scaled back after June 2002.
Ultimately, the Skipton Fund was announced in August 2003.[2605] Although the pressures exerted by the Society, including its interactions with Susan Deacon and with the Scottish Parliament, were in part responsible for this, so far as Karin Pappenheim recollected it came out of the blue.[2606] When it was set up, this answered the second aim. But it did not entirely satisfy the Society. The sums of money fell “far short” of those which an expert group led by Lord Ross had reported was appropriate. The scheme made no provision for those who had died, or those who had cleared the virus through treatment; and by opting for cirrhosis as a trigger for higher payments it missed out many suffering significantly from serious advanced liver disease or liver damage, falling short of actual cirrhosis.[2607] A public inquiry had to wait:[2608]
Throughout its life in the last century the Haemophilia Society campaigned on a number of issues reflecting what were seen as major concerns of its members. Though Reverend Tanner had spoken forcefully to Dr Owen around the end of 1975 about the need to avoid the dangers of hepatitis, the chosen strategy was to achieve this by pressing for self-sufficiency to be achieved. It may be that the principal concern of the Society in the mid 1970s was the danger of Hepatitis B infection, rather than the then recently recognised non-A non-B form; but the aim was soundly based on the understanding of the time.
There is limited evidence now available that the issue of self-sufficiency was pursued with any real vigour after 1976, though it remained an aim until the start of the 1980s.[2609] Part of the reason for this may have been that the dangers of non-A non-B Hepatitis were not as fully appreciated as they should have been.[2610] The medical advice given to the Society in the early 1980s, on which the Society no doubt relied, suggested that non-A non-B Hepatitis was a relatively mild condition.[2611]
Nonetheless, David Watters’ recollection was that at a meeting with the Minister of State for Health, at the time Dr Gerard Vaughan, on 21 October 1981 the risks of hepatitis would have been discussed. He commented that “I certainly have no recollection whatsoever of The Haemophilia Society ever accepting that self-sufficiency should only be aimed for if it could be shown to be economic to do so. Our interest was never based on economics; it was based entirely on the health of people with haemophilia.”[2612] Although there is little doubt that the medical division within the DHSS was by then of the view that hepatitis was a serious disease with significant long-term consequences,[2613] there is no reflection of that view in the briefing note for the meeting.[2614] The departmental official at the meeting with the Minister was not from the medical division. Hepatitis and its risks were not on the agenda. Dr Vaughan was not briefed specifically about them. It is regrettable, in retrospect, if for these reasons – as seems likely – the internal view of the DHSS was not given to the Society at this or other meetings.
If it had been, the Society would have had a solid basis for questioning the dismissive view taken by the Society’s advisers as to the risks of hepatitis, given David Watters’ view that priority was to be given to the health of the Society’s members. There is no significant evidence that the Society asked any such question; but there is some force in its complaint that this was partly because information which could have been passed to it by others in the field (such as, in this case, the Government, and medical professionals) was not.[2615]
In his evidence to the Inquiry, David Watters agreed that non-A non-B Hepatitis was not foremost in the Society’s mind in 1981, that it was considered to be a mild condition and that little information about it had been provided by the Society to members by the early 1980s.[2616]
Throughout the Inquiry, many have sought to deny their own responsibility as a reliable source of advice on the basis that it was for someone else to provide it. A particular example of this is that a refrain of some clinicians in their evidence has been that people with haemophilia in their care knew of hepatitis (both Hepatitis B and non-A non-B Hepatitis) because they were informed of it by the Haemophilia Society (such that there was less, or even no, need to tell them of it and its possible consequences). However, those who were involved in the Haemophilia Society have responded that they took their information from clinicians, and that reliance should have been placed by individual members on what the clinician in charge of their treatment told them, not so much on what the Society imparted. Neither approach is justified, though there is more to be said for the Haemophilia Society than against it in this respect.
The Haemophilia Society was, in truth, a very small organisation, of which only a proportion of people with haemophilia were members, and in which responsibility for policy and for information gathering rested entirely on volunteers (save for some, little, secretarial assistance) until David Watters first took office. It punched above its weight, making light of its very limited resources, to the extent that it was seen by the government not so much as the mouthpiece of a few amateurs lobbying for their own opinions but as an authoritative voice speaking for all those with haemophilia.
The truth was that a small group of volunteers, the bulk of whose experience lay in the largest of the haemophilia treatment centres, spoke for a wider haemophilia community without any structured means of canvassing its opinions. It gained significant media traction. It necessarily had to rely on the advice some haemophilia clinicians were prepared to give gratuitously, and had no resources to obtain a range of opinion or to conduct its own research. As a result its views as to the availability of treatments, their desirability, efficacy and risks were effectively dictated by a narrow group of those clinicians who treated haemophilia. It did not reflect a wider range of opinion. A lack of resources and the limited number of clinicians who had influence over its thinking meant that its views reflected those of others. They were not truly independent.
The Society is open to criticism for not urging the risks of non-A non-B Hepatitis more strongly than it appears to have done;[2617] and for retreating to the comfort of the status quo so far as treatment policy went when first faced with considering the risks of AIDS that factor concentrates clearly presented. Though it did not have sufficient expertise to challenge the views of Professor Bloom, which were so influential in 1983 and early 1984, it gave a platform for those views to be voiced, without asking questions about them so it could better understand their basis. It could and should have asked those questions.
More significantly, for some time after the start of September 1983 it did not convey generally to its members what the evidence shows to have been some growing concerns about the position it had adopted. It had adopted it in good faith, in reliance on what Professor Bloom was saying, but doubts were developing. It failed to pick up what should have been increasingly clear from other sources. Yet members were being told that – although they should take the advice of their haemophilia consultants – they should continue with their current treatment regimes; there was no urging of government, nor of the regulator, to revisit whether permission for importation should continue; and it not so much stayed silent about the continuing distribution of “pre-March 1983 product” as actively suggested that concentrates supplied from the US since that date were much improved in safety.
It was slow in reacting to the risks of Hepatitis C and probably unduly hesitant in beginning to mount a campaign for it. However, the fact that it did so, and that it was well served by Karin Pappenheim in this respect, ultimately bore fruit especially when it focused on Scotland as a part of the UK that might be more responsive to its arguments.
The Society accepts in its final submissions that it failed in some respects, as indeed I have found. However, I reiterate that it should not be forgotten that this was a small Society, whose volunteer Executive Committee consisted of members most of whom were themselves taking factor concentrates, and they too were infected. Simon Taylor said: “Individuals on the Trustee Board itself were living under the personal pressures of living with haemophilia, HIV and hepatitis … we were working alongside friends and colleagues who we watched become ill and die, knowing that this same fate awaited ourselves. During my time on the Executive Committee, at least six of my trustee colleagues died from HIV.”[2618]
(1) As Lord Owen accepted. Lord David Owen Transcript 22 September 2020 p170 INQY1000055
(2) Andy Burnham, Secretary of State for Health from June 2009 to May 2010. Glaziers and Window Breakers - The role of the Secretary of State for Health 2015 p73 RLIT0001140
(3) In 1988 the Department of Health and Social Security became the Department of Health, before being renamed the Department of Health and Social Care in 2018. This chapter, and this Report, endeavours to use the name of the Department at the relevant time.
(4) As Lord Fowler accepted in his evidence. Lord Norman Fowler Transcript 21 September 2021 p27 INQY1000144
(5) Lord Norman Fowler Transcript 21 September 2021 p28 INQY1000144
(6) Lord Kenneth Clarke Transcript 29 July 2021 pp116-120 INQY1000143
(7) See the chapter on Knowledge of Risk Before 1970.
(8) Namely the medical civil servants, reporting up to the CMO. Wales and Northern Ireland also had medical civil servants, although fewer in number, and each part of the UK had its own Chief Medical Officer.
(9) A medical branch within the DHSS, with responsibility (amongst other matters) for blood and blood products.
(10) Dr Diana Walford Transcript 19 July 2021 p104, p108 INQY1000136
(11) Memo from Dr Walford to John Harley 15 September 1980 p1 WITN0282008, Dr Diana Walford Transcript 19 July 2021 p109 INQY1000136
(12) John Harley then moved to the position of Assistant Secretary in HS2 in around late 1980.
(13) Dr Diana Walford Transcript 19 July 2021 pp111-113 INQY1000136
(14) Dr Diana Walford Transcript 19 July 2021 pp117-119 INQY1000136. Dr Walford told the Inquiry that the DHSS would have expected clinicians to know this in any event.
(15) John Moore took over as Secretary of State in June 1987; in July 1988 the DHSS was split into two Departments: the Department of Health and the Department for Social Security, at which point Kenneth Clarke became Secretary of State for Health.
(16) Tony Newton then became Minister of State for Health, succeeded by David Mellor in July 1988.
(17) As distinct from Social Security, which had its own Minister of State and Parliamentary Under-Secretary of State in the House of Commons. Lord Trefgarne and then Lord Glenarthur covered both health and social security in the House of Lords during their time in office.
(18) Lord Norman Fowler Transcript 21 September 2021 pp8-9 INQY1000144
(19) The pre-election period (“purdah”) is the term used to describe the period between the time an election is announced and the date the election is held. Civil servants are given official guidance by the Cabinet Office on the rules they must follow in relation to government business during this time.
(20) Written Statement of Lord Trefgarne paras 2.4-2.5 WITN7478001
(21) For England. Scotland, Wales and Northern Ireland each had their own CMO.
(22) Lord Norman Fowler Transcript 21 September 2021 pp34-35 INQY1000144
(23) “it was a huge, huge improvement when we got Donald Acheson in.” Lord Kenneth Clarke Transcript 27 July 2021 p36 INQY1000141. And see his remarks at the end of his testimony. Lord Kenneth Clarke Transcript 29 July 2021 pp124-125 INQY1000143
(24) The Permanent Secretary to the DHSS from 1975 to 1981 was Sir Patrick Nairne. He was followed by Sir Kenneth Stowe (1981-1987) then Sir Christopher France (1987-1992), who was the first Permanent Secretary of the Department of Health following the splitting of the DHSS into two Departments of State in 1988. Sir Graham Hart succeeded Sir Christopher as Permanent Secretary.
(25) Written Statement of John Canavan paras 1.4-1.5 WITN7115001
(26) See the handwritten note on The Daily Telegraph Alarm as lethal ‘plague’ spreads to non-homosexuals May 1983 DHSC0003824_093. This chapter inevitably refers extensively to the evidence of Dr Walford, because she was the only civil servant from the first half of the 1980s to give oral evidence to the Inquiry. It is an inevitable consequence of the fact that this Inquiry did not take place years earlier that many of the key witnesses are dead or in a state of ill health that made it unreasonable or impracticable to require them to give evidence. It is important to emphasise that, in relation to the issues which this chapter considers, there were a number of different civil servants, in particular from the administrative branch, involved in decision-making, as well as medical officers from Med IMCD and medical officers senior to Dr Walford in Med SEB.
(27) Minutes of UK Haemophilia Centre Directors meeting 30 September 1980 p4, p5, pp9-10, p11 PRSE0003946
(28) Dr Diana Walford Transcript 19 July 2021 pp84-85 INQY1000136, Written Statement of Dr Diana Walford para 44.4 WITN4461001
(29) This issue is addressed also in the chapter on Blood Services and Addressing Risk: Response.
(30) See the chapter Knowledge of Risk Before 1970.
(31) Dr William d’A Maycock was one of the editors and the guide was on behalf of the WHO, the International Society of Blood Transfusion and the League of Red Cross Societies.
(32) “Initial steps to form a panel of donors are best taken within such groups and communities as the armed forces, the police, large industrial or commercial undertakings, universities, prisons, and social or religious foundations.” Bowley et al (eds) Blood Transfusion - A Guide to the Formation and Operation of a Transfusion Service 1971 p14 PRSE0002035
(33) Minutes of Regional Transfusion Directors meeting 6 October 1971 pp4-5 NHBT0015758_001
(34) See for example Home Office Report on the work of the Prison Department 1974 p62 HMPP0000026, Home Office Report on the work of the Prison Department 1975 p69 HMPP0000027, Home Office Report on the work of the Prison Department 1976 p72 HMPP0000028, Home Office Report on the work of the Prison Department 1977 p67 HMPP0000029 and Home Office Report on the work of the Prison Department 1978 p62 HMPP0000030. The last mention of blood donor collection from prisons is in the 1983 report, published in 1984. Home Office Report on the work of the Prison Department 1983 p103 HMPP0000035
(35) “It is recorded that inmates donated 3,903 pints of blood and staff 229 pints during the periodic visits by the Blood Transfusion Service Mobile Units.” Prisons in Scotland Report for 1978 p4 PRSE0001508
(36) “Blood Transfusion Service mobile units visit most establishments at intervals and this year 2,851 pints of blood were donated by inmates and 249 pints by staff.” Prisons in Scotland Report for 1979 p4 PRSE0002834
(37) “Blood Transfusion Service Units continue to visit establishments and this year 1,676 pints were donated by inmates and 125 pints by staff.” Prisons in Scotland Report for 1980 p11 PRSE0003781
(38) ie the widespread presence of a particular antigen – in this case HBsAg – in the blood.
(39) Minutes of Regional Transfusion Directors meeting 26 September 1973 p8 NHBT0000086_002
(40) Hepatitis B Antigen 18 September 1973 DHSC0103253_079
(41) ie Australian antigen/Hepatitis B was present in the blood.
(42) Minutes of Regional Directors of the Scottish National Blood Transfusion Association meeting 4 October 1973 p6 PRSE0002693
(43) Minutes of Regional Transfusion Directors meeting 24 April 1974 pp4-5 PRSE0002186
(44) Table showing Frequency of HBAg and Anti-HBAg reported by RTCs July 1974 PRSE0004719
(45) 1:1,107 (0.09%)
(46) 1:214 (0.47%)
(47) Draft Second Report of the Advisory Group on Testing for the Presence of Hepatitis B Surface Antigen and its Antibody February 1975 pp27-28 PRSE0001879
(48) Second Report of the Advisory Group on Testing for the Presence of Hepatitis B Surface Antigen and its Antibody September 1975 PRSE0004381
(49) Letter from Dr Yellowlees to all regional medical officers 1 May 1975 p2 PRSE0000009
(50) Memo from Dr Scott to colleagues 8 May 1975 PRSE0003803, Letter from Dr McIntyre to Major-General Jeffrey PRSE0003502
(51) Memo from Dr Scott to colleagues 8 May PRSE0003803
(52) Medical officer at the SHHD.
(53) National Medical Director of SNBTS.
(54) Letter from Dr McIntyre to Major-General Jeffrey 16 May 1975 PRSE0003502
(55) Letter from Dr McIntyre to Major-General Jeffrey 16 May 1975 PRSE0003502
(56) Minutes of SNBTS Directors meeting 11 June 1975 p5 PRSE0003812
(57) Note on viral hepatitis 27 February 1980 p1 DHSC0000864
(58) Inspection Report on visit to blood transfusion centre Dundee 25 March 1982 pp1-2 ARCH0002306_002. Dr Ewa Brookes, who moved to become director at Dundee RTC in 1981, shared the concerns about prison donation. Written Statement of Dr Ewa Brookes for The Penrose Inquiry 26 January 2011 pp1-7 PRSE0001873
(59) Interim report on visit to Edinburgh and SE Scotland BTS 10-11 March 1982 and 10-12 May 1982 p2 SBTS0000407_007, Letter from David Haythornthwaite to Dr Cash 4 June 1982 p2 PRSE0000401
(60) Letter from Dr Cash to John Watt 5 July 1982 p1 PRSE0001345
(61) Minutes of SNBTS Directors meeting 29 March 1983 p5 PRSE0000193
(62) Letter from Dr Cash to David Haythornthwaite 12 April 1983 p1 PRSE0003038
(63) Minute from John Davies to John Mackay 6 May 1983 PRSE0004037
(64) Memo from Geoff Pearson to John Davies 9 May 1983 SCGV0000147_175
(65) Memo from J B Brown to John Parker 27 July 1983 PRSE0004345
(66) This was incorrect, save in relation to certain RTCs such as North London: see the chapter on Blood Services and Addressing Risk: Response.
(67) Note on Departmental Policy on Donor Sessions in Prisons and Borstals 16 August 1983 PRSE0003281
(68) Memo from Paul Winstanley to Mr J B Brown 23 August 1983 PRSE0004729
(69) Letter from Dr Brookes to Dr Cash 23 August 1983 PRSE0002981. This was not in fact correct: see the chapter on Blood Services and Addressing Risk: Response and Letter from Dr Gunson to Dr Cash 2 December 1983 NHBT0008624
(70) Minutes of SNBTS Directors meeting 13 September 1983 p6 PRSE0002617
(71) Extract from Hansard written answer by Edwina Currie to question from Alf Dubs 11 February 1987 NHBT0057149_087
(72) Minutes of SNBTS Directors meeting 8 December 1983 p4 PRSE0002899
(73) Written Statement of Professor John Cash to the Penrose Inquiry 25 January 2011 p2 PRSE0004484
(74) SNBTS Report: Penrose Inquiry – Collection of Blood in Prisons 2011 p8 PRSE0002164
(75) There is no reason to think that this would not also have been known to the Welsh Office and the DHSSNI in Northern Ireland.
(76) Lord Kenneth Clarke Transcript 28 July 2021 pp109-110 INQY1000142
(77) Save that Lord Owen had been made aware of the issue as a result of the CMO’s letter of 1 May 1975. Lord David Owen Transcript 22 September 2020 pp146-147 INQY1000055, Letter from Dr Yellowlees to all regional medical officers 1 May 1975 PRSE0000009
(78) In the Morbidity and Mortality Weekly Report (“MMWR”), the weekly publication of the Centers for Disease Control of the United States. Pneumocystis Pneumonia - Los Angeles Morbidity and Mortality Weekly Report 5 June 1981 p1 CGRA0000242
(79) As reported in the MMWR. Kaposi’s Sarcoma and Pneumocystis Pneumonia Among Homosexual Men - New York City and California Morbidity and Mortality Weekly Report 3 July 1981 p2 OXUH0002849, Follow-Up on Kaposi’s Sarcoma and Pneumocystis Pneumonia Morbidity and Mortality Weekly Report 28 August 1981 p1 PRSE0002908
(80) Durack Opportunistic Infections and Kaposi’s Sarcoma in Homosexual Men The New England Journal of Medicine 10 December 1981 p1 PRSE0000746
(81) Follow-Up on Kaposi’s Sarcoma and Pneumocystis Pneumonia Morbidity and Mortality Weekly Report 28 August 1981 p1 PRSE0002908
(82) Masur et al An outbreak of community-acquired Pneumocystis Carinii Pneumonia The New England Journal of Medicine 10 December 1981 PRSE0004831. The other article is Durack Opportunistic Infections and Kaposi’s Sarcoma in Homosexual Men The New England Journal of Medicine 10 December 1981 PRSE0000746. Interestingly, Hyland (the manufacturer of Hemofil) was prompted by these publications to start “closely monitoring” the AIDS issue: see an internal memo from Dr Henry Kingdon which recalls this. Memo from Dr Kingdon to Dr Sharon Northup 5 January 1983 CGRA0000668. The information it had about AIDS had led internally to a minute from Ed Cutter advising that his firm should include an AIDS warning in its product leaflets. Memo from Ed Cutter to Jack Ryan and others 29 December 1982 CGRA0000434. This demonstrates that it would not be unrealistic, nor a view simply of hindsight, to suggest that the DHSS might have done the same, though I do not make any criticism here of a failure to do so, since the DHSS might at this stage reasonably have expected the PHLS or CDSC to raise any alert of which they felt the DHSS should be aware.
(83) Letter from Dr Bruce Evatt to Professor Arthur Bloom 7 March 1983 p1 DHSC0001175
(84) The Centers for Disease Control Epidemiologic Aspects of the Current Outbreak of Kaposi’s Sarcoma and Opportunistic Infections The New England Journal of Medicine 28 January 1982 OXUH0002850
(85) The Centers for Disease Control Epidemiologic Notes and Reports Pneumocystis carinii Pneumonia among persons with Hemophilia A Morbidity and Mortality Weekly Report 16 July 1982 PRSE0000523. Dr Walford told the Inquiry that the MMWR would have been received in Med IMCD and if they related to blood or blood products she would have expected them to be brought to the attention of Med SEB. Dr Diana Walford Transcript 20 July 2021 pp111-113 INQY1000137. It is clear that Med IMCD had reasonable access to medical literature: a minute from Dr Sibellas to Dr Field drew to his attention in relation to AIDS an article in the British Medical Journal from 5 March 1983 and another British Medical Journal article from 23 April 1983. Minute from Dr Sibellas to Dr Field 26 April 1983 DHSC0003824_182. Dr Field received the MMWR and circulated, for example, the July 15 1983 MMWR to colleagues in Med IMCD, Med SEB and HS1 on 25 July 1983. The Centers for Disease Control An Evaluation of the Acquired Immunodeficiency Syndrome AIDS) Reported in Health-Care Personnel – United States Morbidity and Mortality Weekly Report 15 July 1983 DHSC0002229_093
(86) Memo from Stanley Godfrey to Dr Holgate 16 July 1982 DHSC0002219_009
(87) The principal in HS1A. The minute was copied to Dr Petronella Clarke, the medical officer who was standing in for Dr Walford during the latter’s maternity leave. Dr Diana Walford Transcript 20 July 2021 p113 INQY1000137
(88) The principal medical officer in the Medicines Division who dealt with biological products.
(89) It is noteworthy that Stanley Godfrey was keen “From the DHSS point of view” to “defend”NBTS’s “own record”: it is an unusual and arguably overly defensive reaction to having been notified of a serious potential public health concern. It is right to note that the Inquiry was not able to hear from Stanley Godfrey.
(90) Memo from Stanley Godfrey to Dr Holgate 16 July 1982 DHSC0002219_009
(91) The medical head of the Medicines Division.
(92) A senior medical officer in the Medicines Division.
(93) Memo from Dr Holgate to Stanley Godfrey 20 July 1982 DHSC0002219_012
(94) Letter on AIDS from the CDSC to the British Medical Journal 23 April 1983 p1 DHSC0003824_183
(95) This was requested in November 1982. CDSC Surveillance of the acquired immune deficiency syndrome in the United Kingdom, January 1982-July 1983 British Medical Journal 6 August 1983 p2 DHSC0002231_019
(96) This was requested in September 1982. CDSC Surveillance of the acquired immune deficiency syndrome in the United Kingdom, January 1982-July 1983 British Medical Journal 6 August 1983 p2 DHSC0002231_019
(97) Letter from Dr Galbraith September 1982 HSSG0010056_037. Also in September 1982 the MMWR reported that the epidemiology of AIDS suggested the involvement of an unidentified blood-borne agent, and the CDC provided an update on cases of AIDS in the US, emphasising the high mortality rate, the expectation that the mortality rate a few years after diagnosis might be far greater and the rapid increase in the reported incidence of AIDS. CDC Hepatitis B Virus Vaccine Safety: Report of an Inter-Agency Group MMWR 3 September 1982 p1 RLIT0000230 CDC Update on Acquired Immune Deficiency Syndrome (AIDS) - United States MMWR 24 September 1982 p1, pp3-4 OXUH0002848
(98) Minutes of UK Haemophilia Centre Directors meeting 13 September 1982 pp1-2, p10 CBLA0001619
(99) For a summary of the paper, see the chapter on Haemophilia Centres: Policies and Practice. By early November 1982 the MMWR was reporting people with haemophilia as one of the groups with apparently increased risks of AIDS (the others being homosexual males, intravenous drug users and Haitians). CDC Acquired Immune Deficiency Syndrome (AIDS): Precautions for Clinical and Laboratory Staffs MMWR 5 November 1982 p1 RLIT0000231
(100) Minutes of MRC Committee on the Development of Vaccines and Immunization Procedures meeting 12 November 1982 p1, pp6-7 MRCO0000036_006
(101) Assistant Secretary in HS1.
(102) Minutes of CBLA meeting 3 December 1982 CBLA0001644
(103) Dr Diana Walford Transcript 20 July 2021 pp121-123 INQY1000137. This case, and a number of further cases in haemophilia patients, had been reported in the MMWR on 10 December 1982, and were picked up by the journal Science in early January 1983. Update on Acquired Immune Deficiency Syndrome (AIDS) among Patients with Hemophilia A Morbidity and Mortality Weekly Report 10 December 1982 PRSE0003276, Marx Spread of AIDS sparks new health concern Science 7 January 1983 RLIT0000233
(104) Dr Diana Walford Transcript 20 July 2021 p123-124 INQY1000137
(105) Letter from Dr Craske to Dr Walford 10 January 1983 p1 DHSC0001104
(106) Minutes of Advisory Committee on the NBTS meeting 10 January 1983 CBLA0001659. Steven Green was a senior executive officer within HS1. Observers in attendance included Dr Bell (SHHD), Dr David Ferguson-Lewis (Welsh Office) and Dr Lawson (described as DHSS Northern Ireland).
(107) The Observer Mystery disease threat 16 January 1983 DHSC0002223_085. The Observer had previously reported in November 1982 about AIDS and the link with blood, noting that “A major speculation is that the AIDS ‘virus’ is carried in the blood and transmitted directly, either sexually or through syringes” and that AIDS had been identified in a small group of people with haemophilia treated with concentrates. The Observer No defence against gay disease 14 November 1982 MDIA0000010
(108) The Observer Mystery disease threat 16 January 1983 DHSC0002223_085. Dr Walford responded by noting that she had written to Professor Bloom for details of the meeting.
(109) Letter from Dr Walford to Professor Bloom 19 January 1983 BPLL0001351_047
(110) Memo from Dr T K Sweeney to S Fraenkel 18 January 1983 DHSC0002223_088
(111) Dr Diana Walford Transcript 20 July 2021 pp131-136 INQY1000137
(112) Minutes of CBLA meeting 26 January 1983 CBLA0004746
(113) Letter from Dr Gunson to Dr Walford 17 February 1983 NHBT0039762_031, AIDS Situation Stimulates Blood Banking Action AABB February 1983 NBHT0200068_001, Marx Spread of AIDS sparks new health concern Science 7 January 1983 RLIT0000233. Dr Walford’s reply 25 February 1983 set out her view that the most thought-provoking article about AIDS that she had read so far was one in The Lancet on 19 February describing an epidemic of acquired immunodeficiency in Rhesus monkeys. Letter from Dr Walford to Dr Gunson 25 February 1983 NHBT0039762_034, Henrickson et al Epidemic of Acquired Immunodeficiency in Rhesus Monkeys The Lancet 19 February 1983 NHBT0039762_033
(114) Acquired Immunodeficiency Syndrome The Lancet 22 January 1983 p2 SBTS0000315_021, Ragni et al Acquired-Immunodeficiency-Like Syndrome in Two Haemophiliacs The Lancet29 January 1983 RLIT0000201, AIDS: transfusion patients may be at risk The New Scientist3 February 1983 PRSE0000726, AIDS and preventive treatment in hemophilia New England Journal of Medicine 13 January 1983 PRSE0002410, “More than ever, AIDS appears to be infectious.”: West One Step Behind a Killer Science 1 March 1983 p9 BAYP0000028_004
(115) Other than Dr Joseph Smith deciding that the importation of factor concentrates should be considered by the CSM: see Letter from Dr Smith to Dr Fowler 28 March 1983 CBLA0000043_034 and the chapter on Regulation of Commercial Factor Concentrates. Stanley Godfrey and Dr Walford were aware that CSM(B) was proposing to consider this question. Memo from Stanley Godfrey to Miss Spencer 21 April 1983 WITN4461121, Written Statement of Dr Diana Walford para 83.8 WITN4461001. Unsurprisingly Dr Walford thought that Med SEB and Med ICMD would have had AIDS as one of its primary concerns in early 1983 but there is little documentary evidence to suggest that this was in fact the case. Dr Diana Walford Transcript 20 July 2021 p124 INQY1000137
(116) Minutes of CBLA meeting 23 March 1983 p4 CBLA0007769. Again with Dr Harris in attendance as a member and Stanley Godfrey as DHSS observer. The CBLA’s third meeting had taken place in February, with no discussion about AIDS. Minutes of CBLA meeting 23 February 1983 BPLL0003996
(117) Following this meeting Dr Lane wrote a memo to BPL colleagues, which provided a little more detail about what was discussed at the CBLA meeting. He explained that Professor Bloom had reported on the increasing incidence of AIDS cases, the high mortality rate, and “the American over-reaction to the problem.” It was understood that the Council of Europe’s panel of experts would determine the advice to be given to blood transfusionists and special interest groups. Meanwhile, Dr Lane wrote, “patients potentially at risk in the United Kingdom (notably haemophiliacs) are evidently concerned and resistance against the use of imported American coagulation factor concentrates is becoming apparent. Equally, there is a likelihood that a return to cryoprecipitate as a desirable form of treatment may become irresistible, whether logical or not.” Memo from Dr Lane to Gilbert Mallory 24 March 1983 CBLA0001691
(118) Letter from Dr Craske to Dr Walford 11 April 1983 DHSC0002353_024, enclosing The Acquired Immune Deficiency Syndrome (AIDS) 1 March 1983 HCDO0000517_002 and Spectrum of Disease Presentation in AIDS 1 March 1983 HCDO0000273_078
(119) Paul Winstanley and Stanley Godfrey; the former was succeeding the latter as the DHSS observer at CBLA meetings.
(120) Minutes of CBLA meeting 27 April 1983 pp3-4 BPLL0003987_002. The meeting also had a report from Dr Lane: Acquired Immune Deficiency Syndrome (AIDS) 22 April 1983 CBLA0001697
(121) Given the date, this is likely to be a reference to the broadcast by the BBC on 25 April 1983 of the documentary entitled Killer in the Village. This documentary prompted queries to the DHSS and Dr Sibellas briefed Dr Field that the CDSC was monitoring the situation closely and keeping the DHSS informed. Minute from Dr Sibellas to Dr Field 26 April 1983 DHSC0003824_182. Paul Winstanley reported back to the CBLA’s next meeting that he had rung the telephone number given at the end of the TV programme and that they were unable to say how many calls they had received but it had been “quite a lot”. Minutes of CBLA meeting 22 June 1983 p1 CBLA0004715. There was also, in late April 1983, discussion of the requirement to submit a national note setting out the position on AIDS, including information arising from consideration within the blood transfusion service, to the (European) Partial Agreement Public Health Committee. Memo from Dr Field to Dr Sibellas 28 April 1983 DHSC0002225_036
(122) Lord Norman Fowler Transcript 21 September 2021 pp126-127 INQY1000144
(123) It is clear that press reporting continued to be a trigger for ministerial interest or involvement. Thus later in May 1983 Mr Finsberg asked for a factual brief following a Daily Telegraph article on AIDS. The brief provided by Dr Walford on 20 May explained that it had been accepted by the medical profession for some time that the heterosexual partners of AIDS patients, and their children, might be at increased risk of contracting AIDS, and that the “general view” was that the transmission of AIDS seemed to follow the pattern seen with Hepatitis B: “that is, it may be transmitted by various types of sexual contact and by contact with blood and, possibly, other body fluids.” Brief from Dr Walford to Geoffrey Finsberg 20 May 1983 DHSC0002353_031. The article is at The Daily Telegraph Alarm as lethal ‘plague’ spreads to non-homosexuals May 1983 DHSC0003824_093. John Parker sent a minute to the private office of the Secretary of State in relation to a Guardian article of the same date which was highly critical of the Government. Memo from John Parker to George Godber 11 May 1983 DHSC0002227_037
(124) Mail on Sunday Hospitals Using Killer Blood 1 May 1983 PRSE0000199
(125) The Observer Killer disease alert over gay blood donors 1 May 1983 MDIA0000016, The Observer The epidemic spreads 1 May 1983 MDIA0000015
(126) Memo from John Parker to Janet Walden 3 May 1983 p1 DHSC0001651
(127) Memo from John Parker to Janet Walden 3 May 1983 p2 DHSC0001651. The question that was asked of the Prime Minister in Parliament on 3 May 1983 was “As the House of Commons’ favourite own-goal merchant, the Minister for Consumer Affairs [a reference to Gerard Vaughan] was warned two years ago by his own Department of the danger of contaminated blood supplies coming from the United States, will the Prime Minister rectify that deplorable and disgraceful mistake by immediately authorising the necessary expenditure within the National Health Service to make Britain independent in its blood supplies?” to which the Prime Minister responded by stating that “We first need to find out a good deal more about the incident and the causes that have been reported before coming to any conclusion.” Extract from Hansard 3 May 1983 p3 RLIT0000255
(128) The “suspect case” in Cardiff was by this stage a “probable” case of AIDS, rather than merely suspected. See the chapter on Haemophilia Centres: Policies and Practices. The case was reported in the CDSC’s weekly Communicable Disease Report; it is apparent from a handwritten note on the Report from Dr Sibellas to Steven Green that it had come to the attention of DHSS civil servants by 2 June 1983. Communicable Disease Report 6 May 1983 DHSC0002227_020
(129) While the note did refer to other at-risk groups (“homosexual males”, “mainline drug abusers” and “Haitian immigrants”, as did a later note on 20 May 1983: Brief from Dr Walford to Geoffrey Finsberg 20 May 1983 DHSC0002353_031), what the note did not do was to discuss the problems of AIDS transmissions in the population more generally, which were continuing to rise exponentially – for it must have seemed likely that whatever caused those infections also caused the very similar failures of the immune system in people with haemophilia. What might happen in the future to them was potentially to be known by seeing how from small beginnings cases of AIDS had rapidly mushroomed; that it had already killed at least half, if not more, of those who had AIDS; that it was not limited to homosexual men, nor to the US; and that there was likely to be a lengthy period between suffering whatever caused AIDS and first showing clear signs of it such that, if it was a virus, a person could be infected and infect others without knowing they were ill. A question might have been “If that is how it is happening to them, what reason have we to think it is not how it will happen to us?”and to plan accordingly to minimise the chances.
(130) AIDS Line to take 1983 pp2-4 DHSC0003824_173
(131) Lord Norman Fowler Transcript 21 September 2021 pp140-141 INQY1000144
(132) Memo from Dr Sibellas to Dr Ronald Oliver 6 May 1983 DHSC0002227_021
(133) Dr Field was senior principal medical officer in MED IMCD. Letter from Dr Galbraith to Dr Field 9 May 1983 p1 CBLA0000043_040
(134) Dr Galbraith referred to The Lancet reports of 30 April recording 11 cases of AIDS in people with haemophilia in the US receiving Factor 8 concentrates, three cases in Spain (which he had confirmed by a telephone call to the Ministry of Health in Madrid were users of US Factor 8 concentrates) and a case in a child following multiple transfusions. He also noted that Professor Bloom’s patient in Cardiff fitted the accepted criteria of AIDS and had received US concentrate. Ammann et al Acquired Immunodeficiency in an Infant: Possible Transmission by Means of Blood Products The Lancet 30 April 1983 PRSE0000317, Lissen et al AIDS in Haemophilia Patients in Spain The Lancet 30 April 1983 PRSE0002321
(135) According to a letter from Dr Craske to Dr Michael Whitehead (also of the PHLS), he and Dr Galbraith had discussed the problem of Factor 8 by phone on 9 May and had agreed that the latter would write to the DHSS suggesting that the DHSS consider the withdrawal of US commercial concentrates. Dr Craske’s recorded view was that whilst he was “not sure myself that we are at the stage when there is enough evidence to justify this step”, he thought that both the DHSS and haemophilia centre directors “will have to face this problem in the near future, and the earlier it is seriously considered the easier it will be to make a rational decision.” Letter from Dr Craske to Dr Whitehead 10 May 1983 p1 PHEN0001073
(136) Whether this is a reference to Dr Galbraith’s suggestion, in his letter of 9 May, of a top level meeting, or to some other communication from Dr Galbraith, is unclear.
(137) The consultant adviser in genito-urinary medicine.
(138) Memo from Dr Sibellas to Dr Field 12 May 1983 DHSC0002227_038
(139) Memo from Dr Walford to Dr Field 13 May 1983 DHSC0002227_047, Minutes of Haemophilia Reference Centre Directors meeting 13 May 1983 HCDO0000003_008. The meeting and its recommendations are considered in the chapter on Haemophilia Centres: Policies and Practices.
(140) Dr Walford did not think it could have occurred to her to share Dr Galbraith’s paper with the reference centre directors, which she found “a bit surprising”; she agreed it would have been “a good idea if they’d had that paper.” Dr Diana Walford Transcript 20 July 2021 pp170-171 INQY1000137
(141) Memo from Dr Walford to Dr Field 13 May 1983 DHSC0002227_047
(142) Memo from Dr Walford to Dr Field 13 May 1983 DHSC0002227_047
(143) Memo from Dr Walford to Dr Field 13 May 1983 DHSC0002227_047
(144) Memo from Dr Walford to Dr Field 23 May 2023 DHSC0002229_004
(145) Dr Walford thought that it would have been the responsibility of Med IMCD to make sure that the paper went to the Medicines Division. Dr Diana Walford Transcript 21 July 2021 pp1-2 INQY1000138
(146) Shortly after Lord Glenarthur became Parliamentary Under-Secretary of State on 13 June 1983 he asked the CMO for information on AIDS; this resulted in him being provided on 22 June with a paper that had been written by Dr Walford. Memo from Dr Oliver to Christopher Joyce 22 June 1983 DHSC0002309_123, Information page on AIDS DHSC0002309_124. Neither this paper nor any other material from civil servants referred to Dr Galbraith’s proposal, or to the fact that the CSM(B) would be looking at the question of imported concentrates the following month. Lord Glenarthur thought it “strange” and “quite odd” that he was not even informed that one of the country’s leading public health physicians had written to the DHSS arguing strongly for decisive action. Lord Simon Glenarthur Transcript 22 July 2021 pp169-170 INQY1000139
(147) Lord John Patten Transcript 20 May 2022 p89 INQY1000210
(148) The CSM(B)’s and CSM’s consideration of these matters is addressed in the chapter on Regulation of Commercial Factor Concentrates.
(149) Lord Glenarthur was “completely unaware” of the CSM’s decision and was not therefore in a position to comment on it at the time. He was surprised that there was not “a point at which … so many of these things were coming together and coalescing in the minds of officials … at least ministers ought to be aware of some of the competing elements and the real concerns that are being raised, even if it wasn’t to make a decision but to say, you ought to be aware, oh Ministers, that these are perilous times in some respects and therefore you ought to be aware of them.” Lord Simon Glenarthur Transcript 22 July 2021 pp172-173 INQY1000139. Lord Patten found it “very hard to understand” why this matter was not submitted to ministers. Lord John Patten Transcript 20 May 2022 pp93-94 INQY1000210
(150) Lord Norman Fowler Transcript 22 September 2021 pp20-21 INQY1000145
(151) Written Statement of Lord Simon Glenarthur para 29.2, para 36.1 WITN5282001
(152) Lord Simon Glenarthur Transcript 22 July 2021 pp177-178 INQY1000139
(153) Lord Simon Glenarthur Transcript 22 July 2021 pp180-181 INQY1000139
(154) Dr Diana Walford Transcript 20 July 2021 pp180-187 INQY1000137. Dr Walford qualified her answer by adding “consideration was given to whether we could change over to cryoprecipitate, consideration was given to whether BPL could produce small pool products and for each matter the view was no, we can’t on logistic grounds.”
(155) Agenda for meeting on AIDS 3 June 1983 p2 DHSC0002353_038. In relation to agenda item (8), it was said that “Haemophiliacs have been very worried by the recent media publicity”and that “Professor Bloom drafted a letter giving some reassurance which the Society sent to its members.”
(156) Background Papers on AIDS and blood products p1 DHSC0002229_019. One of the papers, referring to the “one suspect case in Cardiff”, stated that “the clinician in charge does not consider that it should be regarded as a confirmed case.” Background Papers on AIDS and blood products p2 DHSC0002229_019. This suggests that Professor Bloom expressed doubt to the DHSS as to whether his patient had AIDS. This was misleading on his part. Dr Walford confirmed in her oral evidence to the Inquiry that she was not aware that Professor Bloom had described it as a probable case in his notification to CDSC nor that he had notified CDSC, and agreed that “It seems to be the case that he was very reluctant to actually confirm that he agreed it was a case.” Dr Diana Walford Transcript 21 July 2021 p45 INQY1000138. Professor Bloom’s role is considered elsewhere in this chapter as well as in the chapter on Haemophilia Centres: Policies and Practice.
(157) Background Papers on AIDS and blood products p3 DHSC0002229_019. This was in fact an overstatement of the UKHCDO advice.
(158) Implications of AIDS for production of FVIII at BPL 31 May 1983 p2 DHSC0002229_020. It is right to note that Dr Walford thought that Dr Gunson would have fully reflected the views of his fellow transfusion directors. She also pointed to Dr Lane as a source. Dr Diana Walford Transcript 21 July 2021 pp48-49 INQY1000138
(159) Minutes of Acquired Immune Deficiency Syndrome (AIDS) meeting 3 June 1983 p1 DHSC0002229_030. As to the absence of ministerial involvement, the meeting took place a few days before the 1983 general election, although it does not follow that that was the reason for their non-involvement.
(160) This issue is considered further in the chapter on Regulation of Commercial Factor Concentrates.
(161) In this regard it was also agreed that if regions showed a continued reluctance to invest in plasma collection at the present time the provision of central funds should be considered.
(162) Minutes of Acquired Immune Deficiency Syndrome (AIDS) meeting 3 June 1983 DHSC0002229_030
(163) Minutes of Acquired Immune Deficiency Syndrome (AIDS) meeting 3 June 1983 p3 DHSC0002229_030
(164) Dr Diana Walford Transcript 21 July 2021 pp64-65 INQY1000138
(165) Committee of Experts on Blood Transfusion and Immunohaematology Informal Report on Proceedings held in Lisbon 16-19 May 19 May 1983 pp1-2 NHBT0017430
(166) Letter from Dr Gunson to Dr Walford 16 May 1983 DHSC0000716
(167) Letter from A T Cumming to Drs Field, Sibellas, Walford, Desmond Fanning and Paul Winstanley 7 June 1983 DHSC0002327_013
(168) Memo from Dr Walford to A T Cumming 13 June 1983 DHSC0002353_019
(169) The initial draft text of the resolution did not include the wording “wherever possible”.Letter from Council of Europe Public Health Division to DHSS International Relations Branch 3 June 1983 pp2-3 DHSC0105313. The final text did, as per the UK’s suggestion.
(170) Council of Europe Recommendation R(83)8 23 June 1982 p3 MACK0000307
(171) The DHSS’s position that large pool concentrates were unavoidable may have reflected the view from Dr Lane that it was impracticable for BPL to switch to producing small pool freeze-dried cryoprecipitate (see, for example, Acquired Immune Deficiency Syndrome (AIDS) 22 April 1983 CBLA0001697); it did not follow from that, however, that regional transfusion centres could not produce cryoprecipitate.
(172) Council of Europe Recommendation R(83)8 23 June 1982 p3 MACK0000307
(173) Dr Walford told the Inquiry that “it was not the role of the Department to inform physicians or recipients about a specific risk or hazard.”Dr Diana Walford Transcript 21 July 2021 pp131-134 INQY1000138
(174) Dr Diana Walford Transcript 21 July 2021 p137 INQY1000138
(175) Report from Committee of Experts on Blood Transfusion and Immunohaematology meeting 16-20 May 13 June 1983 CBLA0001710
(176) Dr Walford said that Dr Gunson would not have said anything that he did not believe to be true, but agreed that “he might have thought about it in some sort of general way as opposed to was every haemophilia clinician making sure they called up their patients and talked to them. That may be a difference. He was talking about the generality”. Dr Diana Walford Transcript 21 July 2021 pp140-141 INQY1000138
(177) Dr Diana Walford Transcript 21 July 2021 p144 INQY1000138
(178) Council of Europe Recommendation R(83)8 23 June 1982 p3 MACK0000307
(179) Memo from A Cumming to Geoffrey Lupton and Janet Walden July 1983 DHSC0002309_086
(180) Memo from Christopher Joyce to Stephen Alcock 22 July 1983 DHSC0002309_029
(181) Written Statement of Lord Simon Glenarthur para 31.4 WITN5282001
(182) Lord Simon Glenarthur Transcript 22 July 2021 pp159-161 INQY1000139
(183) Lord Simon Glenarthur Transcript 22 July 2021 pp162-3 INQY1000139
(184) Lord Simon Glenarthur Transcript 22 July 2021 pp164-5 INQY1000139
(185) Lord Simon Glenarthur Transcript 22 July 2021 p166 INQY1000139
(186) Lord Kenneth Clarke Transcript 27 July 2021 p181 INQY1000141
(187) Lord Kenneth Clarke Transcript 27 July 20201 pp189-192 INQY1000141
(188) See the chapter on People’s Experiences.
(189) See for example Dr Diana Walford Transcript 21 July 2021 pp24-25 INQY1000138
(190) Dr Gunson wrote to Sir Henry Yellowlees, the CMO, on 9 June 1983 setting out his view that there was no alternative to the continuation of the policy of using imported Factor 8 concentrate in the short term, but his letter did not address the availability of cryoprecipitate one way or another. Letter from Dr Gunson to Sir Henry Yellowlees 9 June 1983 NHBT0001067
(191) Dr Diana Walford Transcript 21 July 2021 pp27-28 INQY1000138
(192) Dr Diana Walford Transcript 21 July 2021 p56 INQY1000138
(193) Dr Diana Walford Transcript 21 July 2021 pp64-5 INQY1000138
(194) Hansard House of Lords AIDS: Incidence and Control 14 July 1983 DHSC0002229_085
(195) Memo from Christopher Joyce to Margaret Edwards 19 July 1983 DHSC0002229_095. A draft of the letter sent by Paul Winstanley to Lord Glenarthur’s Private Office on 26 August suggests that Paul Winstanley had added to the letter to give the up-to-date picture on publications from the CDSC. Memo from Paul Winstanley to Scott Ghagan 26 August 1983 WITN0771084
(196) Letter from Lord Glenarthur to Baroness Masham 30 August 1983 p3 DHSC0002231_037, Surveillance of the Acquired Immune Deficiency Syndrome (AIDS) in the United Kingdom, January 1982 - July 1983 29 July 1983 BART0000860, CDSC Surveillance of the Acquired Immune Deficiency Syndrome in the United Kingdom, January 1982 - July 1983 British Medical Journal 6 August 1983 DHSC0002231_019
(197) Memo from Tom Murray to Jane McKessack 21 August 1985 DHSC0002275_083. Outside of the AIDS context, in April 1984 John Patten gave advice to the public about avoiding typhoid by vaccination and consulting doctors about malarial risks. The Guardian Typhoid Warning 25 April 1984 JEVA0000121
(198) DHSS Press Release Increasing Number of Whooping Cough Cases Norman Fowler’s Statement 1 September 1982 WITN0771002
(199) Lord Norman Fowler Transcript 21 September 2021 pp65-67 INQY1000144
(200) There is no contemporaneous documentation relating to this meeting and no record of what was discussed. The date is identifiable only because of an entry Lord Glenarthur made in his personal diary. Lord Simon Glenarthur Transcript 22 July 2021 pp45-6 INQY1000139
(201) Memo from Dr Sibellas to Dr Field 9 September 1983 DHSC0001666
(202) Memo from Dr Walford to Paul Winstanley 19 September 1983 p1 DHSC0002231_059. Dr Walford took the opportunity at the meeting to mention to haemophilia centre directors that further consideration was to be given to rationalising the purchase of blood products and anticipated that this would face opposition (“It is clear that this is a fertile ground for almost wilful misunderstanding on their part!”).
(203) As Dr Walford accepted. Dr Diana Walford Transcript 21 July 2021 p189 INQY1000138
(204) Dr Mark Winter Transcript 1 October 2020 pp168-170 INQY1000059
(205) Dr Diana Walford Transcript 21 July 2021 p189 INQY1000138
(206) Memo from John Parker to Janet Walden 3 May 1983 p2 DHSC0001651. The underlining is added in this and other quotations of the line to take. It is not known who drafted this line to take: Dr Walford was clear that it was not her and thought it was most likely to have been drafted by someone within Med IMCD. Dr Diana Walford Transcript 20 July 2021 pp155-158 INQY1000137. In a paper authored by Dr Walford for a departmental meeting on 3 June 1983 it was said that “Although medical opinion is tending to favour a virus as the agent responsible, there is no proof that this is the case”.Acquired Immune Deficiency Syndrome (AIDS) Background Paper 1983 p1 DHSC0002229_019
(207) AIDS Line to take 1983 p3 DHSC0003824_173. Emphasis added.
(208) Letter from Lord Trefgarne to Nicholas Baker 31 May 1983 p1 HSOC0003451. Emphasis added. This was a response to a letter from Nicholas Baker to Kenneth Clarke which cannot now be found. Nor can the documents showing how and by whom the letter was drafted.
(209) Written Statement of Lord David Trefgarne para 2.20 WITN7478001
(210) Written Statement of Lord David Trefgarne para 2.22 WITN7478001. The briefing note of 3 May had not been copied to Lord Trefgarne’s private office so he was unaware of the caveat.
(211) See Memo from Dr Ronald Oliver to Christopher Joyce 22 June 1983 DHSC0002309_123 and Paper on Acquired Immune Deficiency Syndrome (AIDS) DHSC0002229_054. It was also sent to John Patten who had “expressed interest in AIDS” and asked for more information. Memo from Paul Winstanley to Janet Walden 28 June 1983 DHSC0002309_022
(212) Described as homosexuals, heroin addicts, Haitian immigrants and haemophiliacs.
(213) The factual basis for this assertion is unclear and it was wrong: there was not any uncertainty over Kevin Slater’s diagnosis.
(214) The paper added that no questions pertaining to donors’ sexual habits would be asked: “the Directors are adamant on this score.”
(215) Paper on Acquired Immune Deficiency Syndrome (AIDS) pp3-5 DHSC0002229_054
(216) Memo from John Parker to Christopher Joyce enclosing paper and leaflet on AIDS 1 July 1983 WITN4461134. Emphasis added. The qualification to the words “no conclusive proof” is no longer that the evidence was “suggestive” that a virus was the cause, but that this had now become “very likely”.
(217) Hansard House of Lords AIDS: Incidence and Control 14 July 1983 DHSC0002229_085. Emphasis added. The documents that would have contained the briefing for Lord Glenarthur in relation to this question have not been located. Lord Simon Glenarthur Transcript 22 July 2021 p42 INQY1000139, Written Statement of Lord Simon Glenarthur para 1.11 and para 25.6 WITN5282001. It is not known whether they were destroyed and if so when or in what circumstances. Lord Glenarthur’s answer also contained the assertion that the MRC had established a working party: this was inaccurate, as it had not at this point in time been established and only met for the first time in October 1983. Letter from James Gowans to Sir Henry Yellowlees 15 July 1983 MRCO0000439_158, Written Statement of Lord Simon Glenarthur paras 100.1-100.7 WITN5282001
(218) Memo from Christopher Joyce to John Parker 19 July 1983 DHSC0002229_096
(219) Letter from Dr Walford to John Parker 20 July 1983 DHSC0001109. Emphasis added.
(220) John Parker was Assistant Secretary in HS1. Memo from John Parker to Christopher Joyce 26 July 1983 p2 DHSC0002309_032. Emphasis added.
(221) Letter from Lord Glenarthur to Baroness Masham 30 August 1983 WITN4461147. Emphasis added. A minute from Lord Glenarthur’s office of 30 August recorded that he had “written as drafted”, in other words he sent the letter in the form drafted by officials. Memo from Scott Ghagan to Paul Winstanley 30 August 1983 DHSC0002231_037
(222) Dr Walford did not know why the qualifying clause which she had included was dropped. Dr Diana Walford Transcript 21 July 2021 pp149-152 INQY1000138
(223) Lord Simon Glenarthur Transcript 23 July 2021 pp19-20 INQY1000140. It also troubled Lord Fowler, who thought that the DHSS should have spotted the need to reflect the balance more precisely in the line that it took and acknowledged that it would have been better to have included a reference to the fact that the evidence suggested it was likely that AIDS could be transmitted by blood: “We should have seen the gap there … we should have spotted it.” Lord Norman Fowler Transcript 21 September 2021 pp149-150 INQY1000144
(224) Letter from Lord Glenarthur to Nicholas Baker 25 August 1983 HSOC0003452. Emphasis added. It is apparent from the letter that Nicholas Baker had written to the DHSS (to John Patten) with concerns from a constituent about the monitoring of AIDS cases and the supply of blood products. Neither the letter from Nicholas Baker nor any documents revealing the process of drafting Lord Glenarthur’s reply have been located.
(225) Letter from Lord Glenarthur to Clive Jenkins 26 August 1983 DHSC0002231_036. Emphasis added. Lord Glenarthur was responding to a letter of 7 July (which has not been located) from Clive Jenkins to Lord Trefgarne, his predecessor as Parliamentary Under-Secretary of State in the House of Lords.
(226) DHSS Press Release AIDS - and Blood Donation 1 September 1983 DHSC0006401_006. Emphasis added. The ministerial statement in the press release continued by saying “We must continue to minimise any possible risk of transmission of the disease by blood donation”. The use of the word “possible” further served to underplay the fact that there was a real, actual risk of transmission, which the DHSS well knew by this time, even if the precise agent was yet to be discovered.
(227) Memo from Robin Naysmith to Paul Winstanley enclosing DHSS Draft Press Release AIDS and Blood Donation 26 August 1983 DHSC0002309_034. The press release was approved, with minor amendments, by Kenneth Clarke. Memo from Robin Naysmith to Paul Winstanley 31 August 1983 DHSC0002321_034
(228) Note that the risk from not having enough Factor 8 is described as “obvious”, whilst the risk of infection from AIDS merely “possible”. DHSS Draft Press Release AIDS and Blood Donation 26 August 1983 pp4-5 DHSC0002309_034
(229) DHSS Draft Press Release AIDS and Blood Donation 26 August 1983 p6 DHSC0002309_034. As discussed elsewhere in this chapter, the DHSS’s belief that it was right that blood donors should be “fully informed about AIDS” was not matched by any action to ensure that the recipients of blood products and blood should be equally informed.
(230) Memo from John Parker to Dr Walford 2 August 1983 p2 DHSC0002321_031
(231) The Daily Telegraph Blood Donor Warning to AIDS Risk Groups, The Times Government Asks Victims of Aids Not to Give Blood, The Morning Star ‘No Blood’ Appeal to Aids Suspects 2 September 1983 SHTM0000566. The Morning Star reported the leaflet and the appeal for at-risk groups not to give blood but did not include reference to the “no conclusive proof” line.
(232) British Medical Journal Medical News AIDS and Blood Donation 17 September 1983 PMOS0000252_033. The Mail on Sunday on 2 October 1983, reporting on the death of the patient with haemophilia under the care of the Bristol Haemophilia Centre who was the first to die of AIDS in the UK in consequence of treatment with Factor 8 concentrates, did not reference the leaflet but recorded Kenneth Clarke as “still saying yesterday that there was little that could be done.” The Mail on Sunday The Scandal of Peter Palmer’s Death 2 October 1983 HSOC0016112
(233) Minutes of Advisory Committee on NBTS meeting 17 October 1983 p4 CBLA0001763. Emphasis added.
(234) The Guardian US Blood Caused Aids 1 November 1983 DHSC0002235_048. Dr Walford, in her oral evidence to the Inquiry, said that “This was a very shorthand bit of question and answer. Somebody scribbling on a journal … pointing out to me, as it were, what he thought to be a new development, but it wasn’t a new development and, therefore, I simply said yes, you know, nothing has changed.” Dr Diana Walford Transcript 21 July 2021 p155 INQY1000138
(235) Hansard Blood Products (Imports) 14 November 1983 PRSE0000886. Emphasis added. The briefing given to Kenneth Clarke in relation to this parliamentary answer is missing, and it is not therefore possible to know what information was provided to him about the availability of professional advice. Lord Clarke suggested in his written statement to the Inquiry that it could have been a reference to the Professor Bloom and Dr Rizza letter of 24 June 1983, but it was apparent from his oral evidence to the Inquiry that this suggestion emanated from the Department of Health and Social Care’s legal representatives for the purpose of drafting his statement and that he had no independent knowledge or recollection of the position. Written Statement of Lord Kenneth Clarke para 7.117 WITN0758001, Lord Kenneth Clarke Transcript 28 July 2021 pp14-19 INQY1000142. The reference to “professional advice” might be thought to be a reference from medical officials within the DHSS (such as the CMO) but according to a letter from Tony Newton to Frank Field MP in January 1988 it was in fact a reference to “discussions at the Haemophilia Centre Directors’ meeting in October 1983 when directors were given an expert view that consideration should be given to the possibility that Factor VIII from the USA might be contaminated with a putative infectious agent associated with the cause of AIDS.” Letter from Tony Newton to Frank Field MP 11 January 1988 p2 DHSC0001017. It is both surprising and in all likelihood incorrect to suggest that Kenneth Clarke’s parliamentary answer on 14 November 1983 was a reference to discussions at the UKHCDO meeting on 17 October 1983. This is for two reasons. First, neither Dr Walford (who sent her apologies) nor any other DHSS official attended the meeting (and the minutes from UKHCDO meetings tended to be sent out some significant time later). Second, what was actually said at the meeting regarding AIDS, as recorded in the minutes, was (courtesy of Professor Bloom and an echo of the DHSS line) “at present there was no proof that the commercial concentrates were the cause of AIDS” and “it was agreed that patients … should continue to receive the NHS or commercial concentrates in their usual way.” Minutes of UK Haemophilia Centre Directors meeting 17 October 1983 p10 PRSE0004440
(236) Letter from Lord Glenarthur to Jerry Wiggin 16 November 1983 pp4-5 HSOC000349. Emphasis added.
(237) Letter from Lord Glenarthur to John Maples 16 December 1983 ARCH0000679. Emphasis added. Mr Maples’ letter had been written following a visit from a constituent, John Grindley, who was very concerned about the spread of AIDS and risks from imported blood products. Letter from John Maples to Kenneth Clarke 2 November 1983 ARCH0001532. John Grindley was infected with HIV and died in June 1994. Written Statement of Mary Grindley WITN2336001
(238) Lord Simon Glenarthur Transcript 23 July 2021 pp41-44 INQY1000140
(239) The paper also suggested that it was “now clear” that recipients of blood and blood products could be affected and referred to cases in the US, UK, Spain, Germany, Austria and Canada as well as the baby who developed AIDS following transfusion from a donor who subsequently developed AIDS and a CDSC paper from June 1983 which identified the mode of transmission as follows “Thought to be blood-borne and by intimate direct contact of mucosal surfaces.” ACDP Report on Acquired Immune Deficiency Syndrome (AIDS) pp1-4 WITN5282009
(240) Letter from Clive Jenkins to Lord Glenarthur 27 October 1983 p1 DHSC0002235_041
(241) Written Statement of Lord Simon Glenarthur paras 27.2 and 27.3 WITN5282001
(242) Lord Simon Glenarthur Transcript 23 July 2021 pp37-39 INQY1000140
(243) Letter from Lord Glenarthur to Clive Jenkins 5 January 1984 PRSE0001727
(244) The Sunday Times New Aids Alarm Over Blood Link 25 March 1984 PRSE0001580
(245) Note from Steven Green to Alun Williams, Dr Smithies and E L Creagh 26 March 1984 DHSC0002239_089
(246) Lord Simon Glenarthur Transcript 23 July 2021 pp47-49 INQY1000140
(247) DHSS Chronology Leading to Acceptance of a Link between Factor VIII and AIDS 20 October 1987 p2 DHSC0002375_051
(248) DHSS Chronology Leading to Acceptance of a Link between Factor VIII and AIDS 20 October 1987 pp2-3 DHSC0002375_051. Though in fairness he may not have known this at the time, (though it does seem surprising if no-one in the DHSS were aware of it, given the importance of AIDS generally) on 20 May 1983 (as reported then in Science) a group at the Pasteur Institute in Paris, led by Dr Luc Montagnier reported that his team had isolated a virus which was associated with AIDS. In 2008 he and Dr Françoise Barré-Sinoussi from his team were awarded a Nobel Prize for this achievement. Dr James Smith, who was the head of Plasma Fractionation Laboratory in Oxford throughout and managed BPL factor production and development at Elstree from 1979-82, later observed that this group “had produced convincing evidence of a viral aetiology” (although there remained some suggestions that injection of foreign proteins could be a causal or contributory factor until early 1984). Written Statement of Dr James Smith para 43 WITN3433001. The following April, Dr Robert Gallo in the US identified the same viral particle as Dr Montagnier had done, and confirmed the causal association. In short, among scientists, HIV (though not called that until later) had been identified and isolated in May 1983; and if Dr Moore had known this he could not have said what he did.
(249) DHSS Chronology Leading to Acceptance of a Link between Factor VIII and AIDS 20 October 1987 p3 DHSC0002375_051. The December 1984 acknowledgement was a reference to a press release from the CMO on 20 December 1984 referring to heat treatment as a method by which the AIDS virus in Factor 8 might be inactivated. DHSS Press Release AIDS – Chief Medical Officer’s Statement 20 December 1984 pp2-3 BART0000814
(250) Memo from Dr Pickles to Dr Gwyneth Lewis 19 April 1988 p1 DHSC0001016. The minute of the CMO dated 7 April to which this is a response is missing.
(251) Brief from Dr Walford to Geoffrey Finsberg 20 May 1983 p2 DHSC0002353_031
(252) Committee of Experts on Blood Transfusion and Immunohaematology Informal Report on Proceedings held in Lisbon 16-19 May 19 May 1983 p1 NHBT0017430
(253) Letter from Dr Tedder to Dr Walford 20 May 1983 DHSC0003824_164
(254) NBTS AIDS and how it concerns blood donors 1983 p2 BPLL0007247
(255) Lord Simon Glenarthur Transcript 23 July 2021 pp50-51 INQY1000140
(256) The desire to avoid criticism and/or prevent matters in a positive light can be seen elsewhere in the DHSS’s thinking at this time. In a minute dated 30 November 1984 which reported to ministers three incidents of UK blood being given by donors found positive for HTLV-3, the information was accompanied by a “Defensive Press Briefing” to say that these incidents “reinforce the current policy of the Department” (that policy being the revision of the leaflet, developing a screening test and carrying out pilot studies and considering the use of heat-treatment of Factor 8). Memo from Alun Williams to Christopher Joyce 30 November 1984 DHSC0002309_057. As Lord Patten acknowledged, “Defensive Press Briefing” was “not a nice phrase”. He explained that the phrase made him “uneasy seeing it … the Department should have been on the front foot, not defensive” and also that “there may well be difficult questions to answer and therefore it would be right for civil servants to draft for ministers lines to use if pressed, because ministers don’t know everything”. Lord John Patten Transcript 20 May 2022 pp127-128 INQY1000210. However, when a press release was issued by the CMO on 20 December 1984 it set out the facts of the infections which had led to positive tests in three recipients. DHSS Press Release AIDS – Chief Medical Officer’s Statement 20 December 1984 pp2-3 BART0000814. In a similar vein to the minute of 30 November, in a minute dated 7 June 1985 concerning the arrangements for introduction of the screening test, the advice was to make the details public to “take presentational advantage of the extra funding for PHLS as well as stressing the importance attached to safeguarding the BTS”. Having such a statement on record, it was said, “could be helpful if a well publicised case of AIDS attributable to infected blood occurs.” Memo from Dr Malcolm Harris to Dr Hunt and Jane McKessack 7 June 1985 DHSC0002311_019. As Lord Patten observed, the DHSS should be “presenting things truthfully”, as opposed to “presenting things well.” Lord John Patten Transcript 20 May 2022 pp136-138 INQY1000210
(257) Note of Minister of State for Health meeting 6 July 1983 p1 DHSC0001511. The note of the 6 July meeting does not expressly indicate who said that Lord Glenarthur should emphasise that the risk to people with haemophilia was very small but the most natural reading of the note is that it was suggested by the Minister of State for Health and Lord Glenarthur thought the suggestion came from Kenneth Clarke. Lord Simon Glenarthur Transcript 22 July 2021 p70 INQY1000139. Lord Clarke said this was important to emphasise because “we didn’t want to cause mad panic.” Lord Kenneth Clarke Transcript 27 July 2021 pp82-83 INQY1000141
(258) Submissions on behalf of core participants represented by Thompsons Scotland 16 December 2022 para 4.50 SUBS0000064
(259) It is interesting to note that the director of Bristol Haemophilia Centre wrote to the parents of a patient in early October 1983, following the death of a patient from AIDS, using terminology that was very similar to the Government’s line to take: “The cause of this condition is still unknown but there is evidence to suggest that it is due to an infection which can be transmitted by blood or blood products. There is reason to believe that the source of infection in this case was imported Factor VIII concentrates but this is not proven and it cannot be said with certainty that these were the source of the infection.” The letter was expressly designed to allay patients’ fears. Letter from Dr Geoffrey Scott 3 October 1983 HSOC0003486
(260) Many will recall the “Tombstone” advert on TV, with the strap line “Don’t die of ignorance”. It emphasised the risks of contracting AIDS. It is credited with having saved lives. Had the same approach of emphasising rather than minimising risk been taken to those who might be considering transfusion or taking a blood product it too might have made a difference.
(261) See the section on The Context in this chapter. The UK had the advantage of having seen an epidemic take hold in the US, and those responsible for public safety would have realised that what happened there was likely to spread to other countries given the amount of social and business interaction between the US and other nations. It would have been wishful thinking to consider it purely an American phenomenon.
(262) Letter from Dr Gunson to Dr Walford 16 May 1983 DHSC0000716
(263) This was a meeting in which she recalled a “somewhat churlish reception … the Chair, Dr Wagstaff, introduced me with words to the effect: since Dr Walford has wished herself on us, I suppose we had better hear what she has to say!”Written Statement of Dr Diana Walford para 86.48 WITN4461001
(264) Written Statement of Dr Diana Walford para 86.49 WITN4461001
(265) Minutes of Regional Transfusion Directors meeting 18 May 1983 pp3-4 CBLA0001707
(266) Written Statement of Dr Diana Walford paras 86.50-86.52 WITN4461001. The possibility of regional transfusion directors also asking donors about symptoms such as night sweats, weight loss etc was raised by Dr Walford with Dr William Wagstaff in early June 1983. Memo from Dr Walford to Paul Winstanley 6 June 1983 p1 DHSC0002231_051
(267) Memo from Dr Walford to Paul Winstanley 17 June 1983 WITN4461131, DHSS Leaflet on AIDS WITN4461132
(268) Memo from Paul Winstanley to Mr Windsor 8 June 1983 DHSC0002321_018. See paragraph 5 in particular.
(269) Copied to the private offices of John Patten and Kenneth Clarke as well as to the Welsh Office, Northern Ireland Office and SHHD.
(270) Memo from John Parker to Christopher Joyce 1 July 1983 DHSC0002309_024
(271) Lord Glenarthur very much doubted that expenditure of the magnitude of £5,000 would ordinarily come to ministers for approval. Lord Simon Glenarthur Transcript 22 July 2021 p51 INQY1000139. It is clear from the submission to ministers that the reason for ministerial involvement was the “sensitivity” in relation to gay men, and Lord Glenarthur accepted that one concern was that of offending a cohort of potential donors. Lord Clarke told the Inquiry that he would probably have got involved because the leaflet was “a very big step … the handling of it was quite important. To say that we were actually going to – discouraging homosexuals -- concentrate on what it calls ‘promiscuous homosexuals’ -- from donating blood because they might be giving people AIDS, big stuff.” Lord Kenneth Clarke Transcript 27 July 2021 p75 INQY1000141
(272) Acquired Immune Deficiency Syndrome: Issue of an Information Leaflet through the National Blood Transfusion Service DHSC0002309_121, Why is a leaflet on AIDS necessary? 24 June 1983 DHSC0002309_122
(273) Memo from Christopher Joyce to John Parker 4 July 1983 DHSC0002309_025
(274) Memo from Janet Walden to Kenneth Clarke 1 July 1983 DHSC0002309_027
(275) Note of Minister of State for Health meeting 6 July 1983 DHSC0001511. An internal SSHD minute of the same date from Dr Bell to Dr Scott stated that “we are informed that Mr Fowler’s first reaction is that the terms of this leaflet are too strong, and that DHSS may therefore be making further amendments.” Memo from Dr Bell to Dr Scott 6 July 1983 SCGV0000147_159. There is no evidence that Norman Fowler expressed any view on this issue, and it seems plausible that this was a reference to the views, not of the Secretary of State, but of the Minister of State, Kenneth Clarke. Dr Bell expressed his own view that a single UK leaflet would be best, a proposal supported by Dr Cash.
(276) Note of Minister of State for Health meeting 6 July 1983 DHSC0001511
(277) Letter from Dr Gunson to Dr Oliver 14 July 1983 DHSC0002321_024. Lord Glenarthur told the Inquiry that this was not a concern he shared and that he “was perhaps not as sensitive as were some of my ministerial colleagues to any concerns about upsetting the homosexual community, and the adverse press coverage that could ensue. My greatest concern was to minimise the risk of donors passing on infection.” Written Statement of Lord Simon Glenarthur para 16.4 WITN5282001
(278) Memo from John Parker to Dr Oliver 19 July 1983 DHSC0002321_026
(279) Memo from Dr Oliver to John Parker 20 July 1983 DHSC0002321_027. This memo was not shared with ministers. Written Statement of Lord Kenneth Clarke para 7.17 WITN0758001
(280) Memo from John Bolitho to Dr Oliver 21 July 1983 DHSC0002321_028. Somewhat puzzlingly, John Bolitho also stated that the leaflet “cannot be seen as a leaflet which you read and then change your mind about giving blood.” That is exactly what the leaflet was intended to do, if read by someone in a high risk group, as pointed out by Dr Oliver in response to John Bolitho on 25 July 1983. Memo from Dr Oliver to John Bolitho 25 July 1983 DHSC0002321_029
(281) It was also, according to Dr Oliver, the view of Dr Gunson in his capacity as consultant adviser on blood transfusion. Memo from Dr Oliver to John Bolitho 25 July 1983 DHSC0002321_029
(282) Memo from John Parker to Stephen Alcock 29 July 1983 DHSC0002327_016
(283) In relation to the issue of the leaflet with the donor call-up cards, this could be expected to reach about 80% of the total donor population, including donors booked on factory sessions, although walk-in donors would not be covered; donors could read the leaflet in their own homes, thus avoiding embarrassment; and this was thought to be the most effective in keeping high-risk donors away from sessions, removing the temptation to proceed with donation in order to avoid embarrassment. The downside was that this would have administrative and resource implications. In relation to making the leaflet available at donor sessions, it would, said the submission, be difficult to ensure that all donors received a leaflet and there could be insufficient time for it to be read prior to donation; there were many circumstances besides the risks of AIDS which lead to a donor being rejected, and donors could be caused embarrassment if they felt fellow donors wrongly suspected the reason for their rejection; for the donor in a high-risk group reading the leaflet immediately prior to or during donation, they might well be tempted to proceed rather than risk the embarrassment of withdrawing at that stage. On the other hand, this presented very few administrative problems and had no obvious resource implications.
(284) Memo from Christopher Joyce to John Parker 3 August 1983 DHSC0002327_120. By “positive in our approach” Lord Glenarthur meant “proactive, perhaps more than positive ... let’s get on with it and do something … we were putting ourselves, in my view, in a degree of peril if we didn’t get a move on with it and alert people to the risks that might be there.”Dr Diana Walford Transcript 22 July 2021 p91 INQY1000138
(285) Underlining as in the original. Memo from Janet Walden to Stephen Alcock 2 August 1983 DHSC0002327_118
(286) Memo from Stephen Alcock to John Parker 2 August 1983 DHSC0002327_119
(287) Lord Kenneth Clarke Transcript 27 July 2021 p86 INQY1000141
(288) Memo from Robin Naysmith to Paul Winstanley 26 August 1983 DHSC0002309_034
(289) Memo from Robin Naysmith to Scott Ghagan 31 August 1983 DHSC0002309_035
(290) Memo from Scott Ghagan to Robin Naysmith 1 September 1983 DHSC0002309_036
(291) Lord Simon Glenarthur Transcript 22 July 2021 pp101-103 INQY1000139
(292) DHSS Press Release AIDS - and Blood Donation 1 September 1983 DHSC0006401_006
(293) From at least 16 July 1982, when information the CDSC had already passed through the hands of Dr Gunson to Stanley Godfrey, and from him on to Dr Petronella Clarke who was covering for Dr Walford whilst the latter was on maternity leave. Memo from Stanley Godfrey to Dr Holgate 16 July 1982 DHSC0002219_009
(294) For example by Paul Winstanley at the start of June: but it is indisputable that it was, given the context.
(295) Lord Simon Glenarthur Transcript 22 July 2021 p64 INQY1000139
(296) Lord Simon Glenarthur Transcript 22 July 2021 p103 INQY1000139
(297) Lord Kenneth Clarke Transcript 27 July 2021 pp76-77 INQY1000141
(298) Lord Kenneth Clarke Transcript 27 July 2021 pp102-103 INQY1000141. The possibility that the blood services might lose donors was, of course, a relevant matter to consider and was a concern shared by the blood services. However, the regional transfusion directors were experienced in adopting measures, such as local radio appeals, in order to address any drop in donor numbers. See Blood Services & Addressing Risk: Regional Transfusion Centres.
(299) Lord Kenneth Clarke Transcript 27 July 2021 p82 INQY1000141
(300) Lord Kenneth Clarke Transcript 27 July 2021 p86 INQY1000141. There was also a worry that the leaflets might fuel homophobia. See for example Written Statement of Lord Kenneth Clarke paras 7.7-7.8 WITN0758001
(301) Lord Kenneth Clarke Transcript 27 July 2021 pp96-97 INQY1000141
(302) This was in response to it being pointed out to Lord Clarke that there could be two to four years before an infected individual showed clinical signs of AIDS and that practising homosexuals might not themselves know that they were infected.
(303) Lord Kenneth Clarke Transcript 27 July 2021 pp121-122 INQY1000141
(304) For the Minister of State’s response see Memo from Robin Naysmith to Paul Winstanley
23 November 1983 WITN5282011. The Inquiry does not have a copy of the submission itself.
(305) Minutes of CBLA Working Group on AIDS meeting 14 October 1983 p5 PRSE0002573
(306) As opposed to leaving it to the discretion of the regional transfusion directors to make their own individual decision on distribution.
(307) This would have been consistent with the three month trial period agreed by ministers.
(308) Minutes of Advisory Committee on NBTS meeting 17 October 1983 p4 CBLA0001763. It is also unclear whose responsibility it was to raise these matters but it is reasonable to assume that it would have been Dr Gunson. He was the chair of the meeting of the Working Group on AIDS on 14 October 1983 (Minutes of CBLA Working Group on AIDS meeting 14 October 1983 p5 PRSE0002573) and attended the Advisory Committee meeting on 17 October. It is right to note however that Dr Ian Fraser (regional transfusion director, Bristol) and Dr Lane (BPL) also attended both meetings. Dr Gunson did raise “informally” with Dr Walford the suggestion of highlighting the message that high risk donors should not donate. Letter from Dr Gunson to Dr Wagstaff 30 November 1983 NHBT0039762_061
(309) Letter from J Emlyn-Jones to Paul Winstanley 23 November 1983 DHSC0002237_014. This is a letter from Cardiff RTC providing information about the use of the leaflets further to a memo from Paul Winstanley dated 18 August and a subsequent telephone call. Paul Winstanley’s letter to directors of 18 August had asked them to keep a note of numbers of leaflets used, rate of usage per month, method of distribution, effect on donor attendance and feedback from donors during the six month trial period (ministers having not, at that stage, decided that the trial period should be halved). Letter from Paul Winstanley to all transfusion directors 18 August 1983 DHSC0002231_026. However it is apparent from the Cardiff letter that directors were aware that the trial period was in fact three months.
(310) See for example Letter from Dr Gunson to Dr Wagstaff 30 November 1983 NHBT0039762_061, Summary of the activity at official level regarding the revised donor leaflet on AIDS: October 1983 - August 1984 p3 WITN5282008
(311) Letter from Dr Wagstaff to Paul Winstanley 3 January 1984 WITN5282008_002. Dr Wagstaff noted that “one or two people expressed a view that there should be a revision of content before reprinting” and that it would be wise to see Dr Brian McClelland’s new draft “before going to the printers.” He hoped to be able to communicate firm proposals following the next regional transfusion directors’ meeting on 25 January.
(312) From Dr P Rodin, who was the consultant adviser in genito-urinary medicine.
(313) Memo from Dr Sibellas to Dr Smithies 8 February 1984 DHSC0002239_010. Dr Smithies was a senior medical officer in Med SEB.
(314) It suggested that the position was being examined by Steven Green.
(315) A civil servant within the Health Services branch HS1.
(316) Memo from Dr Smithies to Alun Williams 14 February 1984 DHSC0002239_015. It is understood that Dr Smithies took up this role in late January/early February 1984.
(317) Memo from Dr Smithies to Dr Sibellas 6 March 1984 DHSC0002239_038
(318) It might have been more accurate to say overdue for review.
(319) This information had already been provided by Dr Wagstaff to the DHSS in January 1984 (as Dr Jack Darnborough, Cambridge regional transfusion director, pointed out. Letter from Dr Darnborough to Steven Green 15 March 1984 p2 WITN5282008_001); it is unclear why it was being requested again.
(320) Letter from Steven Green to all transfusion directors 12 March 1984 p1 WITN5282008_001
(321) Minutes of Advisory Committee on NBTS meeting 10 April 1984 p2 CBLA0001835. Dr Smithies told the regional transfusion directors’ meeting on 11 April that a revised and updated leaflet was in preparation. Minutes of Regional Transfusion Directors meeting 11 April 1984 p3 CBLA0001836
(322) Including the production of a more general leaflet, not specific to blood donation, but aimed at warning of the dangers of promiscuous sexual activity.
(323) It is unclear what measure was being applied to assess its success. The objective was to deter high risk donors from giving blood but the information that had been received from RTCs would not indicate whether that had been achieved or not.
(324) Memo from Margaret Edwards to Jane McKessack 17 April 1984 p2 DHSC0002321_044
(325) Memo from Christopher Joyce to Margaret Edwards 25 April 1984 DHSC0002309_041. John Patten also responded, but his response addressed only the other leaflet, not the donor leaflet. Memo from Jane McKessack to Roy Cunningham 18 April 1984 DHSC0002309_040
(326) Letter from Dr Smithies to Dr Sibellas 9 May 1984 WITN5282008_006
(327) Memo from Victoria Brown to Dr Smithies 16 May 1984 DHSC0002243_006
(328) Memo from Margaret Edwards to Dr Smithies 23 May 1984 DHSC0000178. This memo noted that “Ministers are very concerned about the sensitivities attached to links between AIDS and homosexual activity.”
(329) Letter from Dr Smithies to Dr Fraser 6 June 1984 DHSC0002243_021, Letters from Dr Smithies to Dr Wagstaff and Dr Keith Rogers 7 June 1984 WITN5282008_008, Letters from Dr Smithies to Dr Fraser, Dr Rogers and Dr Wagstaff 7 June 1984 WITN5282008_009
(330) Minutes of Regional Transfusion Directors meeting 11 July 1984 p3 DHSC0002245_002
(331) Memo from Dr Smithies to Alun Williams 18 July 1984 DHSC0002323_003, Draft leaflet on AIDS entitled AIDS and How it Concerns Blood Donors 18 July 1984 MACK0002635_043
(332) Memo from Dr Smithies to Dr Sibellas 23 July 1984 WITN5282008_011
(333) Memo from Dr Smithies to Alun Williams 31 July 1984 DHSC0002323_005
(334) This was described as having relatively minor cost implications for some RTCs: those centres whose volunteers were currently recalled by card would incur some cost “in that envelopes would have to be used, addressed and stamped.”
(335) Submission from John Parker to Christopher Joyce 10 August 1984 DHSC0002309_044. A handwritten note dated 13 August on the minute reads “MS(H) [ie Kenneth Clarke] to see.”
(336) Memo from S Ghagan to John Parker 21 August 1984 DHSC0002309_046
(337) Memo from Robin Naysmith to Alun Williams 16 October 1984 DHSC0002309_050
(338) Note from Dr Smithies to Steve Godber 19 November 1984 DHSC0002309_053
(339) Under-Secretary in the Health Services Division.
(340) The recent developments may have been the news that 13 people, including 3 babies, had died from AIDS after receiving a blood transfusion in Australia and a second AIDS-related death in the UK of a person with haemophilia. Note from Dr Smithies to George Godber 19 November 1984 p2 DHSC0002309_053
(341) The ministerial statements are likely to have been John Patten’s announcement in a press release on 19 November 1984 which referred to the leaflet being reprinted with a strengthened message and that the leaflet would be given to each known and new or unregistered donor. DHSS Press Release Britain to be self-sufficient in blood products by late 1986 19 November 1984 PRSE0002251, DHSS Press Release AIDS and Blood Products – John Patten Parliamentary Secretary for Health PRSE0003367. The Guardian reported on 20 November that homosexual donors had continued to donate blood, because they thought that the existing leaflet, asking promiscuous homosexuals not to donate, did not apply to them because they were not promiscuous. The Guardian Warning to gays still donating blood 20 November 1984 HSOC0016001
(342) Memo from Janet Hewlett-Davies to John Cashman 22 November 1984 p1 DHSC0002323_014. For reasons that are not clear, Janet Hewlett-Davies’ minute was copied to the Private Offices of John Patten and Kenneth Clarke, but not copied to the Private Office of the Minister with responsibility for blood, Lord Glenarthur. Lord Simon Glenarthur Transcript 22 July 2021 p124 INQY1000139
(343) Memo from Dr Abrams to Dr Smithies 23 November 1984 DHSC0000435. “at present” suggests the Advice leaflet without the alterations suggested by Janet Hewlett-Davies.
(344) Memo from Dr Abrams to Dr Harris 27 November 1984 p1 DHSC0002251_011
(345) Hansard written answer on AIDS (Blood Donors) 28 November 1984 DHSC0002251_017. A similar statement to Parliament (by means of a written answer) was made by Kenneth Clarke on 4 December. Hansard written answer on AIDS 4 December 1984 DHSC0002008
(346) Memo from M Nolan to Sarah Bateman and S Ghagan 30 November 1984 DHSC0002309_056
(347) Memo from Dr Abrams to Robin Naysmith 3 December 1984 DHSC0002309_058
(348) Memo from S Ghagan to Sarah Bateman 4 December 1984 DHSC0002309_059
(349) Memo from S Ghagan to Sarah Bateman 4 December 1984 p1 DHSC0002309_059
(350) Memo from Malcolm Harris to Sarah Bateman 14 December 1984 DHSC0002309_060
(351) Memo from Alun Williams to Sarah Bateman 20 December 1984 DHSC0002327_127
(352) The Guardian Blood donor passes Aids virus to baby 20 December 1984 HSOC0015996. Ministers had already been told, on 30 November, that there were incidents of blood being given by donors who were HTLV-3 positive: one donor who had subsequently developed AIDS had given donations which transmitted the virus to three recipients who were now seropositive. Memo from Alun Williams to Christopher Joyce 30 November 1984 DHSC0002309_057
(353) Memo from Robin Naysmith to Dr Abrams 20 December 1984 DHSC0002309_062
(354) Memo from R Windsor to Robin Naysmith 21 December 1984 DHSC0002309_063
(355) This was a reference to the text of the draft leaflet which, in answer to the question “Can patients get AIDS by transfusion of blood?” stated “Yes, but there is only a remote chance of this happening with ordinary blood transfusions given in hospital.”
(356) Memo from Sarah Bateman to R Windsor 31 December 1984 DHSC0002309_064
(357) Memo from Malcolm Harris to Alun Williams 2 January 1985 DHSC0001694. An additional impetus for speed was press coverage over Christmas in which a reporter had attended a donor session “where no attempt was made to impart information on the new ‘at risk’ group. The existing leaflet was not available because ‘DHSS is revising it’ and they were out of stock.”
(358) Memo from Alun Williams to Malcolm Harris and Christopher Joyce 3 January 1985 DHSC0002309_065
(359) Memo from Christopher Joyce to Alun Williams 15 January 1985 DHSC0002482_011
(360) Memo from Alun Williams to all regional transfusion directors 23 January 1985 p1 DHSC0002257_061
(361) Memo from Alun Williams to all regional transfusion directors 23 January 1985 p2 DHSC0002257_061
(362) Memo from Alun Williams to all regional transfusion directors 23 January 1985 p2 DHSC0002257_061
(363) Lord Simon Glenarthur Transcript 22 July 2021 p121 INQY1000139
(364) Lord Simon Glenarthur Transcript 22 July 2021 p132 INQY1000139
(365) Lord Simon Glenarthur Transcript 22 July 2021 p147 INQY1000139
(366) Lord John Patten Transcript 20 May 2022 pp120-121 INQY1000210
(367) Lord Kenneth Clarke Transcript 27 July 2021 p88 INQY1000141. “Even” Kenneth Clarke because he was loathe, in his evidence to the Inquiry, to accept criticism.
(368) Lord Kenneth Clarke Transcript 27 July 2021 p127 INQY1000141
(369) Guidance on AIDS and Blood Transfusion May 1983 PRSE0000984
(370) Guidance on AIDS and Blood Transfusion June 1983 PRSE0004850
(371) Dr Brian McClelland told the Inquiry that the thinking in initially defining the group as “Homosexual men” was that nobody really knew what was meant by “multiple partners” (“is two partners multiple? Over what time period?”) Dr Brian McClelland Transcript 28 January 2022 p5 INQY1000178
(372) The text explained that people with haemophilia “may be more susceptible or may become infected by their use of blood products which may have come from a blood donor with AIDS.”
(373) Minutes of SNBTS Directors meeting 14 June 1983 pp2-3 MACK0001960_001
(374) NBTS AIDS: And how it concerns blood donors 1983 p2 BPLL0007247
(375) NBTS AIDS: And how it concerns blood donors 1983 BPLL0007247
(376) The leaflet in bold print stated “Please remember, AIDS is a rare disease but a serious one.”
(377) At North London RTC it was found that donors in the high risk category “said that they had continued to donate despite the publicity about AIDS because the original (unrevised) leaflet had implied that homosexuals with stable partnerships were still eligible as donors.” Contreras et al Blood donors at high risk of transmitting the acquired immune deficiency syndrome British Medical Journal 9 March 1985 NHBT0000030_013
(378) Memo from Dr Smithies to Alun Williams 14 February 1984 DHSC0002239_015. In Scotland, SNBTS did not wait for the DHSS’s second leaflet but made its own amendments some time in 1984, using the phrases “sexually active homosexual men” instead of “many different partners”, and “present or past abusers of intravenous drugs”. Although “sexually active” was a better choice than “many different partners”, it remained problematic, because it would not capture those who had previously been sexually active (and might therefore unknowingly have been exposed to the virus) but who no longer were, perhaps out of fear of the virus itself. The reference to “present or past” in relation to IV drug use had the benefit of encompassing those who no longer used drugs, although “abusers” might still not include those who had used drugs intravenously but infrequently. SNBTS Important message to blood donors PRSE0000286
(379) As Dr Hewitt wrote in a letter dated 26 February 1985, it would be quite wrong to suggest that only those homosexual men who were promiscuous or who had promiscuous lovers were at risk of contracting AIDS: “Although promiscuous men are more likely to be infected, those who only have one partner are not immune. It is simply a matter that one encounter may be enough, and we are well aware of cases of AIDS in this country which have affected monogamous homosexual men who had no other risk factors. It is a fact of life in the United States … that any male homosexual (except possibly those celibate for many years) must be considered at risk.”Letter from Dr Hewitt to Anon 26 February 1985 NHBT0110979_001
(380) Underlining in the original. DHSS Press Release AIDS – Revised leaflet for blood donors published 1 February 1985 DHSC0004764_111
(381) NBTS AIDS: Important new advice for blood donors January 1985 NHBT0096480_022
(382) The third risk group – sexual contacts – was now defined as sexual contacts of people in the other risk groups, rather than as sexual contacts of those suffering from AIDS.
(383) A Q&A briefing dated 19 February 1985 identified the at-risk groups in the second leaflet and added that “If pressed: Practising means sexually active within the last five years.” This guidance was not, however, part of the leaflet and would not therefore have been understood by donors. Memo from Malcolm Harris to Mr Murray and Robin Naysmith 19 February 1985 DHSC0001598
(384) Minutes of EAGA meeting 29 January 1985 p5 PRSE0002734
(385) NBTS AIDS: Important information for blood donors September 1985 CBLA0002255. The leaflet was circulated by means of a letter dated 24 September 1985. Letter from Malcolm Harris to regional general managers and general managers of the Special Health Authorities for London Postgraduate Hospitals 24 September 1985 MACK0000052_001
(386) See Memo from Alun Williams to Dr Smithies 27 August 1985 DHSC0000497, Memo from Alun Williams to V Brown 28 August 1985 DHSC0002275_101, Memo from Malcolm Harris to M Fairey and M Ferguson 13 September 1985 DHSC0002277_089
(387) NBTS AIDS: What you must know before you give blood September 1986 p2 BPLL0007799_002. The date was changed to 1977 in July 1987. NBTS AIDS: Think before you give blood July 1987 p2 NHBT0007310
(388) Details of two of the transfusions appear in: Letter from John Buchanan to Dr Michael Barnes 30 October 1984 DHSC0004180_058, Letter from Dr Barnes to Dr Craske 5 November 1984 DHSC0001690, Report on donor and their donation history DHSC0004180_050. The third was confirmed in a response by Kenneth Clarke to a Parliamentary Question on 4 February 1985 when he said that “In 1984 monitoring was commenced of 3 recipients of blood transfusions given by a donor who subsequently had developed AIDS; the transfusions took place in 1983(2) and 1984(1).” Extract from Hansard on AIDS 4 February 1985 SCGV0000148_054
(389) Having been received at BPL on 6 April 1984, pooled for fractionation on 17 May and issued for clinical use on 10 August 1984. Note from Dr Smithies enclosing a summary report on the recall of Factor VIII batch HL3186 occasioned by probable diagnosis of AIDS in a contributing donor 26 October 1984 p5 DHSC0001111
(390) He was then chair of UKHCDO, and as such it was to be expected that he would be a central point of liaison and information for the DHSS.
(391) Lord Norman Fowler Transcript 22 September 2021 pp142-143 INQY1000145. Lord Clarke would expect medical officers to be drawing on the widest available relevant expertise in relation to something that was uncertain and new.
(392) Dr Diana Walford Transcript 20 July 2021 p167 INQY1000137
(393) Acheson One Doctor’s Odyssey: The Social Lesion 2007 p15 WITN0771088
(394) This is not “quibb[ling] about a few months”, as Lord Fowler suggested in his oral evidence. Lord Norman Fowler Transcript 22 September 2021 p52 INQY1000145
(395) Lord Glenarthur, for example, was appointed to the DHSS with no prior ministerial experience, no background in health or social security fields (he is a hereditary peer and his background was military/aviation). Lord Simon Glenarthur Transcript 22 July 2021 pp1-2 INQY1000139
(396) Written Statement of Lord Michael Forsyth para 22.1 WITN7126001
(397) Lord Simon Glenarthur Transcript 22 July 2021 p10 INQY1000139
(398) Lord John Patten Transcript 20 May 2022 pp16-17 INQY1000210
(399) Lord Norman Fowler Transcript 22 September 2021 pp152-153 INQY1000145
(400) Letter from Dr Gunson to Sir Henry Yellowlees 9 June 1983 NHBT0001067. Dr Gunson’s letter said that there was a “strong possibility” that AIDS was caused by a transmissible infectious agent and “it has been implicated in transfusion of blood and blood products.” He informed the CMO that in the US some patients with Haemophilia A had died and that in England “there is one patient with haemophilia who is suffering from a condition which fulfils the U.S.A. definition of AIDS”. Dr Gunson’s view was that there was no alternative to the continuation of treatment with imported concentrates “in the short term”. He asked for “a few minutes under Any Other Business to appraise members of the Committee [of Consultant Advisers to the CMO, who were due to meet on 17 June] of the problems of AIDS in relation to the transfusion of blood and blood products and the measures being undertaken to minimize the effects of this potentially fatal syndrome.” Letter from Dr Gunson to Sir Henry Yellowlees 9 June 1983 NHBT0001067
(401) There may have been a verbal conversation; a later letter refers to Sir Henry Yellowlees consulting Dr Gunson at “the meeting of the Consultant Advisers”in the summer of 1983. Letter from Dr Acheson to Dr Gunson 14 October 1983 p2 NHBT0001066
(402) Letter from Dr Acheson to Dr Gunson 14 October 1983 p2 NHBT0001066
(403) Memo from Dr Smithies to Dr Alderslade 19 October 1984 DHSC0002323_009
(404) Note from Dr Smithies to Mr Godber 19 November 1984 DHSC0002309_053
(405) Memo from Dr Smithies to Dr Sibellas 31 December 1984 DHSC0001693
(406) Lord Norman Fowler Transcript 22 September 2021 p50 INQY1000145
(407) Memo from Malcolm Harris to Sarah Bateman 2 August 1985 DHSC0002116
(408) Lord Norman Fowler Transcript 22 September 2021 p59 INQY1000145
(409) Memo from Dr Acheson to the Secretary of State 30 July 1985 DHSC0000514
(410) There is also little evidence of Sir Henry Yellowlees taking proactive steps in relation to the risks of hepatitis at any earlier stage.
(411) Written Statement of Dr Roger Moore para 29.3 WITN6919001. Dr Moore was a principal in HS1A from October 1985 to December 1988 and then deputy national director of NBTS’s National Directorate. The CMO’s statement was in the context of a response to a European Directive on self-sufficiency; having articulated the principle, the CMO continued “When therefore a doctor decides in the light of available clinical information, that a particular product is indicated for a particular patient, we believe that the decision should be respected even if that product has to be imported from outside the EC.”
(412) Dr Roger Moore Transcript 18 January 2022 pp45-46 INQY1000172
(413) Dr Diana Walford Transcript 19 July 2021 pp48-49 INQY1000136
(414) Written Statement of Lord Norman Fowler paras 8.14-8.15 WITN0771001
(415) Written Statement of Baroness Virginia Bottomley para 2.1(5) WITN5289001
(416) Written Statement of Dr James McKenna paras 7.1-7.2 WITN6983001
(417) Letter from Sir Henry Yellowlees to regional and area medical officers 31 December 1981 NHBT0000070_042
(418) Those interested in the reference to such a vaccine should know that until 2017 there was no programme of universal childhood vaccination against Hepatitis B. Certain groups at particular risk (including amongst others most health workers, and some people with haemophilia, were identified). It was not adopted as a universal vaccination in part because the early vaccines required frequent top-up injections, and because of resource implications.
(419) Letter from Dr Acheson to all doctors in England 15 May 1985 DHSC0105232; an equivalent letter was circulated in Scotland from DCMO Dr Graham Scott. Letter from Dr Scott to chief administrative medical officers 17 May 1985 LOTH0000267_019
(420) Letter from Dr Acheson to all doctors in England 15 May 1985 p4 DHSC0105232
(421) DHSS Press Release AIDS: Information for Doctors 15 May 1985 DHSC0002269_049
(422) Written Statement of Lord Kenneth Clarke para 8.5 WITN0758001
(423) Written Statement of Lord Norman Fowler para 8.19 WITN0771001
(424) Sheard and Donaldson The Nation’s Doctor: the role of the Chief Medical Officer 1855-1998 2018 p149 RLIT0002330
(425) There was an update on hepatitis infection figures in the 1980 report, published in 1982, although the focus was on Hepatitis A outbreaks and no mention of non-A non-B Hepatitis. DHSS On the State of the Public Health for the year 1980 DHSC0007003. The 1981 report, published in 1982, noted a rise in notifications of infective jaundice attributed to Hepatitis A; it was thought “unlikely that there has been much change in the incidence of hepatitis B or hepatitis non-A/non-B.” DHSS On the State of the Public Health for the year 1981 p49 DHSC0007002
(426) DHSS On the State of the Public Health for the year 1982 pp61 DHSC0007004
(427) DHSS On the State of the Public Health for the year 1983 p54, p66 DHSC0007005
(428) DHSS On the State of the Public Health for the year 1985 p12 DHSC0007007
(429) DHSS On the State of the Public Health for the year 1986 pp9-10 DHSC0007008
(430) DHSS On the State of the Public Health for the year 1987 pp15-16 DHSC0007009
(431) DHSS On the State of the Public Health for the year 1988 p18 DHSC0007010
(432) Lord Simon Glenarthur Transcript 22 July 2021 p6 INQY1000139
(433) Lord Simon Glenarthur Transcript 22 July 2021 pp11-12 INQY1000139. Ministers were not however in purdah: though busy they had exposure to the press, constituents and others, even if these were not “official” sources of information.
(434) Edwina Currie, who was Parliamentary Under-Secretary for Health from September 1986 to December 1988 described the process as “slightly arbitrary”: the black box of evening reading would be filled with what civil servants and more senior ministers felt the junior minister needed to know, as well as letters which required a signature. Written Statement of Edwina Currie Jones para 4.15 WITN5287001
(435) Dr Diana Walford Transcript 19 July 2021 p64 INQY1000136
(436) Lord Simon Glenarthur Transcript 22 July 2021 pp20-21 INQY1000139
(437) Written Statement of Lord John Patten para 2.8 WITN5297001, Lord John Patten Transcript 20 May 2022 pp13-15 INQY1000210
(438) Written Statement of Peter Wormald para 57.2 WITN6934001. He gave examples of the questions civil servants should ask themselves: (a) is it a matter of main policy or principle? (b) does it have major resource implications? (c) does it impact upon or conflict with other departmental policies or programmes? (d) is it a matter in which a particular minister has a close interest? (e) may the minister wish to inform any MP because of an impact on their constituency? (f) is there a possibility or likelihood of generating public or political interest or controversy, to which the minister may wish or be obliged to respond? (g) is there an actual or possible impact on the responsibilities or interests of any government colleagues? Peter Wormald added “If in doubt, an official should consult his superiors.”
(439) Lord Simon Glenarthur Transcript 22 July 2021 p22 INQY1000139. Or as Lord Clarke put it “You just plunged in.” Lord Kenneth Clarke Transcript 27 July 2021 p41 INQY1000141
(440) Other than at dinners or when visiting hospitals. Lord Kenneth Clarke Transcript 27 July 2021 pp47-48 INQY1000141
(441) Written Statement of Lord Simon Glenarthur para 1.7 WITN5282001, Directory of Civil Service Guidance Access by Ministers and Special Advisers to documents of a previous administration WITN5282002
(442) Lord Norman Fowler Transcript 21 September 2021 p19 INQY1000144
(443) Lord Kenneth Clarke Transcript 27 July 2021 p8 INQY1000141
(444) Lord Kenneth Clarke Transcript 27 July 2021 p12 INQY1000141
(445) Lord Kenneth Clarke Transcript 27 July 2021 p13 INQY1000141
(446) Lord Kenneth Clarke Transcript 27 July 2021 pp16-17 INQY1000141. This was clearly incorrect at least in relation to AIDS: see the section regarding the role of the CMO above.
(447) Lord Simon Glenarthur Transcript 23 July 2021 pp103-104 INQY1000140
(448) Written Statement of Lord Simon Glenarthur para 12.2 WITN5282001
(449) The particularly striking omissions are set out in the preceding text.
(450) When the criticisms were put to Lord Clarke under the Inquiry Rules 2006 the response on his behalf was: “Lord Clarke acknowledges that on occasion when giving oral evidence to the Inquiry he lost his composure and expressed his views more strongly than he ought to have done. He regrets that this was the case and wishes to offer his apologies to the Chair, Counsel to the Inquiry and those who were following his evidence. Lord Clarke felt the pressures of giving evidence over three days on a wide range of topics relating to events dating back forty years, by reference to very many documents. Lord Clarke was unable to speak to anyone throughout the course of his evidence about the difficulty he felt in giving evidence and this contributed to the way he presented. Lord Clarke came to the Inquiry wishing to assist it in its work to the extent he was able to do so. He has always felt and continues to feel great sympathy for those who suffered as a result of infected blood and blood products provided by the NHS. It was never his intention to cause any further distress or upset to those affected by the evidence he gave.”
(451) Lord Kenneth Clarke Transcript 27 July 2021 p10 INQY1000141
(452) Lord Kenneth Clarke Transcript 27 July 2021 pp121-122, p145, p187, p198 INQY1000141
(453) Lord Kenneth Clarke Transcript 28 July 2021 p16 INQY1000142
(454) Lord Kenneth Clarke Transcript 27 July 2021 pp154-155 INQY1000141
(455) Lord Kenneth Clarke Transcript 28 July 2021 p96 INQY1000142
(456) Lord Kenneth Clarke Transcript 28 July 2021 p16 INQY1000142
(457) Other less than helpful contributions included, in response to questions about the Government’s “no conclusive proof” line to take: “We’re not going to go long [sic] all day like this, are we? ... I mean, doesn’t this Inquiry wish to reach a conclusion? I don’t know how many years you’ve been going. Extraordinary.” Lord Kenneth Clarke Transcript 28 July 2021 p31 INQY1000142
(458) Lord Kenneth Clarke Transcript 27 July 2021 p207 INQY1000141
(459) Lord Kenneth Clarke Transcript 29 July 2021 pp126-127 INQY1000143
(460) This is not intended to be a comprehensive account of all the committees and working groups operating during this period.
(461) It was chaired by Dr Maycock.
(462) Report of the Advisory Group on Testing for the Presence of Australia Hepatitis Associated Antigen and its Antibody p3 PRSE0000190
(463) The report was originally produced in July 1971 but there was a request from the DHSS for further advice in September 1971 and a revised version of the first report was then published in May 1972. Hepatitis Advisory Group, Maycock Report July 1971 DHSC0103097_019, Report of the Advisory Group on Testing for the Presence of Australia Hepatitis Associated Antigen and its Antibody p24 PRSE0000190, Comments on the report of the group on which the Department would welcome further advice September 1971 DHSC0100021_035, Revised report of the Advisory Group on Testing for the Presence of Australia (hepatitis associated) Antigen and its Antibody p12 CBLA0000869
(464) Minute of Reconvened Advisory Group on Testing for the Presence of Australia (hepatitis associated) Antigen and its Antibody meeting 6 December 1973 DHSC0002357_014
(465) Second report of the Advisory Group on testing for the presence of Hepatitis B surface antigen October 1975 p12 DHSC0103109. The recommendation was that counter-immunoelectrophoresis should no longer be the recommended technique and should be replaced by reversed passive haemagglutination. The second report also, as discussed elsewhere in this report, contained advice regarding the practice of permanently excluding donors with a history of jaundice: the Group advised that this practice should be discontinued, provided that HBsAg was not detected by testing and the donor had not suffered from hepatitis or jaundice in the previous 12 months.
(466) Minutes of Reconvened Advisory Group on Testing for the Presence of HBsAG and its antibody meeting October 1979 p7 CBLA0001020
(467) Minutes of Advisory Group on Testing for the Presence of HBsAG and its Antibody meeting 6 March 1980 p2 CBLA0007195
(468) Third Report of the Advisory Group on Testing for the Presence of HBsAG and Its Antibody 1981 pp9-10 PRSE0000862
(469) Third Report of the Advisory Group on Testing for the Presence of HBsAG and Its Antibody 1981 p12 PRSE0000862
(470) Minutes of Advisory Group on Testing for the Presence of HBsAG and its Antibody meeting 6 March 1980 p2 CBLA0007195
(471) Dr Diana Walford Transcript 19 July 2021 pp132-133 INQY1000136
(472) Minutes of Advisory Group on Hepatitis B Testing meeting 17 September 1980 pp3-4 CBLA0001167
(473) Head of Med IMCD.
(474) Deputy CMO.
(475) It is possible that the genesis of the idea was a meeting chaired by the CMO, Sir Henry Yellowlees, in February 1979 to discuss the risks of transmission of Hepatitis B from healthcare staff to patients and vice versa. Dr Evans voiced the view at that meeting that “there was need for clear advice to the profession on all aspects of the problem of Hepatitis B.” Memo from Dr Wiliam Prentice to colleagues 16 February 1979 p2 SCGV0001180_234
(476) Memo from Dr Geffen to Dr Evans 5 July 1979 DHSC0003878_004
(477) See the handwritten note dated 13 July 1979 at the bottom of Memo from Dr Geffen to Dr Evans 5 July 1979 DHSC0003878_004
(478) Referred to in Memo from Dr Geffen to Dr Evans 24 July 1979 DHSC0002193_091; no minutes of this meeting have been located.
(479) Memo from Dr Sibellas to Dr Geffen 18 July 1979 p1 DHSC0002193_082. Noting that if they could not go ahead with an advisory group they would need to seek a consultant adviser in hepatitis, Dr Sibellas commented that “the current medical advice from specialists in the hepatitis field runs the whole spectrum from draconian measures (the ‘hepatitis leper’) to a much more conservative approach” and that an advisory group would assist in steering the best course between these points of view. Memo from Dr Sibellas to Dr Geffen 18 July 1979 p2 DHSC0002193_082
(480) Memo from Dr Geffen to Dr Evans 24 July 1979 DHSC0002193_091, Minute on Advisory Group on Viral Hepatitis pp1-2 DHSC0002193_092
(481) Memo from Dr Geffen to Dr Evans 6 November 1979 p1 DHSC0002195_062
(482) Memo from Dr Evans to Dr Geffen 13 February 1980 DHSC0000857
(483) Memo from Sir Henry Yellowlees to Mr Knight 13 June 1980 p1 DHSC0000880
(484) Proposed CMO’s Advisory Group on Hepatitis p1 DHSC0000870. A note from 1980 setting out the terms of reference and proposed members did refer in terms to “problems relating to the management and prevention of non-A non-B hepatitis.” Paper JKCCL(80)5 of the National Blood Transfusion Service Joint Management Committee for the Central Blood Laboratories 16 October 1980 p2 CBLA0001188
(485) Memo from Dr Phyllis Furnell to Dr Walford and Dr Oliver 27 June 1980 DHSC0000884, although it was agreed that the Advisory Group on Testing for Hepatitis B could continue with its work on redrafting its report and any other matters which were “its legitimate concern.” Memo from Dr Walford to Dr Furnell 1 July 1980 DHSC0000885
(486) Terms of reference of the Hepatitis Advisory Group p1 DHSC0002201_011
(487) Minutes of Advisory Group on Hepatitis meeting 3 October 1980 DHSC0002199_066. There was a summary given of the recommendations of the Third Report of the Advisory Group on Testing for Hepatitis B Surface Antigen and its Antibody, which included a reference to undertaking research into NANBH.
(488) Minutes of Advisory Group on Hepatitis meeting 5 December 1980 DHSC0002201_070. There was merely a passing reference under ‘Any other business’ to Dr Lane emphasising the need to make any tests for markers of NANBH available as soon as possible when developed.
(489) Minutes of Advisory Group on Hepatitis meeting 11 May 1981 DHSC0000128. The reference to a risk of transmission in renal units of NANBH from imported cadaveric kidneys does not amount to a discussion regarding NANBH.
(490) Minutes of Advisory Group on Hepatitis meeting 27 October 1981 NHBT0000068_048
(491) Minutes of Advisory Group on Hepatitis meeting 5 October 1982 pp2-5 NHBT0000068_021B
(492) Minutes of Advisory Group on Hepatitis meeting 18 October 1983 p1, pp3-4 BPLL0008168. The minutes of this meeting refer to there now being a working party on transfusion-associated hepatitis and a working party on AIDS.
(493) Minutes of Advisory Group on Hepatitis meeting 1 May 1984 CBLA0001840, Minutes of Advisory Group on Hepatitis meeting 9 October 1984 pp5-6 CBLA0001904. The October meeting included a short discussion on AIDS.
(494) Minutes of Advisory Group on Hepatitis meeting 31 October 1985 CBLA0002273. The minutes of its 1986 meeting (if there was one) have not been located.
(495) Minutes of Advisory Group on Hepatitis meeting (unconfirmed) 28 July 1987 NHBT0000069_010. There was no meeting in 1988.
(496) Minutes of Advisory Group on Hepatitis meeting 7 February 1989 p8 DHSC0002567_037
(497) The paper for the February 1989 meeting was brief and merely noted that the DHSS was planning to set up the ACVSB, which would “consider the many interests involved including the Health Departments, the Licensing Authority, NBTS, NIBSC and the commercial organisations.” Non A-Non B viruses in blood for transfusion – for information CBLA0002437
(498) Minutes of Advisory Group on Hepatitis meeting 6 December 1990 p5 NHBT0000190_055
(499) Dr Diana Walford Transcript 19 July 2021 p149 INQY1000136. She added that “it didn’t move with the speed of summer lightning, how shall I say” although “this was probably not slower than other working parties or other working groups would work”.
(500) Minutes of MRC Blood Transfusion Committee meeting July 1978 MRCO0005276_002, Membership of the MRC Blood Transfusion Research Committee and its Working Parties MRCO0005276_004. Working parties included the Working Party on Cryoprecipitate and the Working Party on Post-Transfusion Hepatitis, both established in 1967. Blood Transfusion Research Committee – Review of activities since 1967 MRCO0005276_003
(501) Minutes of Blood Transfusion Research Committee Working Party on Post-Transfusion Hepatitis meeting 16 October 1967 p1 MRCO0005069, Minutes of Blood Transfusion Research Committee Working Party on Post-Transfusion Hepatitis meeting 1 December 1969 MRCO0005076 and Minutes of Blood Transfusion Research Committee Working Party on Post-Transfusion Hepatitis meeting 14 December 1970 MRCO0000014_004
(502) Blood Transfusion Research Committee – Review of activities since 1967 p4 MRCO0005276_003
(503) Minutes of Blood Transfusion Research Committee meeting 17 December 1979 p2 CBLA0001040
(504) Minutes of Blood Transfusion Research Committee meeting 25 June 1981 pp2-3 CBLA0001396
(505) The Working Party had met on only two occasions since the Committee was reconstituted: February 1980 and June 1981. MRC Blood Transfusion Research Committee – Review of Activities 1979-82 June 1982 p5 MRCO0005282. At its February 1980 meeting the Working Party identified a number of problems relating to NANBH that needed investigation. Minutes of Blood Transfusion Research Committee Working Party on Post-Transfusion Hepatitis meeting 14 February 1980 pp2-3 MRCO0000029_003. At its June 1981 meeting the Working Party discussed the desirability of obtaining accurate data regarding the incidence of NANBH and whether ALT screening might be of value. Minutes of Blood Transfusion Research Committee Working Party on Post-Transfusion Hepatitis meeting 25 June 1981 p3 NHBT0000068_049
(506) Minutes of Blood Transfusion Research Committee meeting 8 March 1982 pp2-3 CBLA0001558
(507) Letter from Helen Duke to Dr Cash 19 July 1982 p1 PRSE0004746
(508) Letter from John Wastle to Secretaries of Health Boards 13 April 1983 SBTS0000680_069
(509) ACDP terms of reference DHSC0003880_030
(510) ACDP terms of reference and procedures May 1981 DHSC0003871_021
(511) Minutes of ACDP inaugural meeting 3 June 1981 p1 DHSC0003873_012
(512) Minutes of ACDP meeting 26 September 1983 p7 DHSC0102003_049
(513) Minutes of ACDP meeting 26 September 1983 pp11-12 DHSC0102003_049. The focus of the Working Group was to be the problems and risks of handling material from AIDS patients; a suggestion at the ACDP’s April 1984 meeting that its terms of reference should include blood products was met with the observation from Dr Smithies that the Blood Transfusion Service AIDS Working Party had a study of blood products well under way and from the chair that the ACDP was not equipped to do a detailed study of blood products as members did not have the know-how. Minutes of ACDP meeting 3 April 1984 p13 DHSC0102000_042
(514) Memo from Dr Walford to Dr Oliver and John Parker 16 August 1983 DHSC0001403. Dr Oliver agreed with Dr Walford. Memo from Dr Oliver to Dr Walford 22 August 1983 DHSC0001404
(515) Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 27 September 1982 p1 CBLA0001625. This was very much a Blood Transfusion Service working party, and there were no DHSS or SHHD observers.
(516) Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 27 September 1982 p1, p3 CBLA0001625
(517) In January, April and September 1983. Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 18 January 1983 NHBT0000023_002, Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 20 April 1983 NHBT0000023_003, Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 27 September 1983 PRSE0001299, Note of Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 3 October 1983 PRSE0002278. There were detailed discussions about AIDS in the latter meeting. The reconvened meeting of the Working Party is at Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 24 November 1986 NHBT0000023_007; on this occasion there was a DHSS representative (Dr Smithies) and an SHHD representative (Dr John Forrester).
(518) Letter from Dr Forrester to Dr McIntyre 1 December 1986 p1 PRSE0003801
(519) Minutes of MRC Working Party on AIDS meeting 10 October 1983 p2 CBLA0001749
(520) Minutes of MRC Working Party on AIDS meeting 10 October 1983 p6 CBLA0001749
(521) Minutes of MRC Working Party on AIDS meeting 20 December 1983 p3 DHSC0002239_079
(522) The Possibilities for Research on Acquired Immune Deficiency Syndrome in the UK April 1984 p4 MACK0000945. “Cases of AIDS have occurred already in haemophiliacs and more are likely. Because of the specially high standard of record-keeping in the UK, it is possible to trace which batches of factor VIII cryoprecipitate etc., any patient has received and also all others in the country who have received the same batches, with their family contacts. A study is planned at the Public Health Laboratory in Manchester, in co-operation with the Haemophilia Centre Directors. We support this as it offers a special opportunity to study attack rates, incubation periods and other important factors.”
(523) Minutes of MRC Working Party on AIDS meeting 17 April 1984 p4 MRCO0000541_061
(524) Minutes of MRC Working Party on AIDS meeting 25 October 1984 p2 MRCO0000541_047
(525) Minutes of MRC Working Party on AIDS meeting 25 October 1984 p2 MRCO0000541_047
(526) DHSS On the State of the Public Health for the year 1983 1984 p55 DHSC0007005
(527) Minutes of Central Committee for Research and Development in Blood Transfusion meeting 21 June 1983 pp1-2 PRSE0002741
(528) Minutes of CBLA Working Group on AIDS meeting 14 October 1983 CBLA0001755. It was chaired by Dr Gunson and members included Drs Craske, Lane, Philip Mortimer and Tedder. There was no DHSS or SHHD observer.
(529) Minutes of CBLA Working Group on AIDS meeting 14 October 1983 p1 CBLA0001755
(530) See further the chapters on Surrogate Screening for Hepatitis C and Surrogate Screening for HIV.
(531) Minutes of CBLA Working Group on AIDS meeting 27 January 1984 CBLA0001799. No further minutes have been located.
(532) Minutes of ACVSB meeting 4 April 1989 NHBT0000041_003
(533) ACVSB terms of reference p1 PRSE0001189
(534) Letter from Dr Harris to Dr Gunson 8 March 1989 p8 WITN4486049
(535) Memo from Dr Pickles to Dr Harris 9 June 1988 DHSC0003597_144
(536) Memo from Dr Pickles to Dr Harris 11 July 1988 DHSC0002429_132
(537) Memo from Dr Harris to CMO 14 July 1988 DHSC0003597_133
(538) A reference to the Health Services Division.
(539) Memo from Dr Moore to John Cashman 2 September 1988 DHSC0003597_115
(540) Memo from Dr Pickles to Dr McInnes 3 January 1989 DHSC0002429_076
(541) Memo from Dr Pickles to Dr Williams 30 September 1988 DHSC0002429_106
(542) Dr Hillary Pickles Transcript 12 May 2022 pp124-127 INQY1000205, Memo from Dr Pickles to Dr McInnes 3 January 1989 DHSC0002429_076, Memo from Dr Moore to Malcolm Harris and Meg Kirk 6 December 1988 WITN0758013, Submission on ACVSB PRSE0003956. The then Parliamentary Under-Secretary of State for Health, Edwina Currie, agreed to the establishment of the committee in December, but due to changes to the proposed membership a further submission was sent to the new Parliamentary Under-Secretary of State for Health, Roger Freeman, on 12 January 1989. Memo from Dr Harris to Meg Kirk 12 January 1989 DHSC0003597_069
(543) Submission on ACVSB p1 PRSE0003956
(544) Memo from John Canavan to Dr Harris 21 February 1989 DHSC0003597_056, Letter from Michael Forsyth to Roger Freeman 8 February 1989 PRSE0000967, Letter from Richard Needham to Roger Freeman January 1989 WITN0758015, Letter from Ian Grist to Roger Freeman 24 January 1989 WITN0758016
(545) Malcolm Harris, writing to the SHHD, Welsh Office and Northern Ireland Office in October 1988, said that “We would like to get the committee established as soon as possible.”Letter from Malcolm Harris to Duncan Macniven 25 October 1988 PRSE0000216
(546) Note on the virological safety of blood DHSC0002429_107
(547) Dr Diana Walford Transcript 19 July 2021 p57 INQY1000136
(548) Memo from Dr Walford to John Harley 15 September 1980 p1 WITN0282008
(549) Although the redevelopment of BPL was underway in the 1980s.
(550) See the chapter on Surrogate Screening for Hepatitis C.
(551) See the chapter on Viral Inactivation.
(552) See the chapter on People’s Experiences.
(553) See the Expert Report to the Infected Blood Inquiry: Hepatitis January 2020 pp51-52 EXPG0000001. This chapter is about addressing risk, so government cannot be judged on what became clear as reality only later: but the fact that the risk was reality underscores the importance of taking risks seriously.
(554) Minutes of EAGA meeting 29 January 1985 PRSE0002734
(555) Professor Ian Hann Penrose Inquiry Transcript 6 May 2011 pp53-55 PRSE0006021
(556) Public Health Agency Four decades of public health: Northern Ireland’s health boards 1973-2009
p8 WITN3449008
(557) Public Health Agency Four decades of public health: Northern Ireland’s health boards 1973-2009 p12 WITN3449008
(558) Written Statement of Dr James McKenna WITN6983001
(559) Written Statement of Lord John Patten para 8.3 WITN5297001. See also the statement of Sir Richard Needham para 20 WITN5595001. “Security issues dominated the role and function of the Northern Ireland Office given that my tenure was during the height of ‘the Troubles’.” Also the statement of Lord King (Tom King) to the effect that his main responsibilities as Secretary of State had been to “combat the serious terrorist campaign that was threatening the orderly life of the people of Northern Ireland.” Written Statement of Lord Thomas King para 13 WITN5598001
(560) As explained by Dr Andrzej Rejman, senior medical officer in the DH (London) from 1989 to 1998, the departments in Northern Ireland, Wales and Scotland were “smaller than DH by a significant margin, and so the relevant doctors in their departments would have had a much wider role. So, for example, there would not have been an SMO [senior medical officer] dealing just with haematology. You know, they’d be dealing with haematology and other matters as well. And because of that, I think they did, to a certain extent, rely upon work done within DH. And particularly a lot of the policy decisions would be -- would come from DH.” Dr Andrzej Rejman Transcript 10 May 2022 p42 INQY1000203
(561) Lord David Owen Transcript 22 September 2020 p153 INQY1000055
(562) Written Statement of Lord John Patten para 8.4 WITN5297001
(563) Written Statement of Lord John Patten para 2.12 WITN5297001
(564) Written Statement of Lord Norman Fowler para 2.17 WITN0771001, Lord Norman Fowler Transcript 21 September 2021 pp22-23 INQY1000144
(565) Written Statement of Dr Morris McClelland para 7a WITN0892001
(566) Dr Hillary Pickles Transcript 12 May 2022 p58 INQY1000205
(567) Written Statement of Dr Robert McQuiston para 7.2 WITN5572001
(568) Minutes of Scottish Home and Health Department, Department of Health and Social Services, Northern Ireland and the Welsh Office meeting 1 December 1980 p3 DHSC0000064
(569) Letter from N I Kells to Eastern Health and Social Services Board 20 April 1977 DHSC0002183_028. It is of note, however, that the DHSSNI did not simply ratify unquestioningly the recommendations of the Maycock Group’s second report. At the date of issue of the circular in April 1977 asking that certain of the recommendations be implemented, the DHSSNI was still considering its position on some of the other recommendations. Letter from N I Kells to Eastern Health and Social Services Board 20 April 1977 p2 DHSC0002183_028
(570) Letter from Dr Harris to Dr Logan 7 July 1980 DHSC0003878_156. Dr Logan attended the first but not the second meeting.
(571) Minutes of ACVSB meeting 21 November 1990 CBCA0000080_008. The Northern Ireland Minister (Richard Needham) had earlier been asked to agree to the establishment of the ACVSB. Letter from Richard Needham to Roger Freeman January 1989 WITN0758015
(572) Memo from John Parker to Janet Walden 3 May 1983 DHSC0001651
(573) Letter to N Lunn 16 August 1985 RHSC0000042_080
(574) From 1985 until 1992 Richard Needham was Parliamentary Under-Secretary of State for Northern Ireland.
(575) Thus, for example, there were discussions in 1986 between the health ministers of Northern Ireland and the Republic of Ireland regarding a campaign of public education, and a ministerial submission noted that the measures taken in Northern Ireland to prevent the spread of infection “mirrored initiatives which have been introduced at national level” and included the introduction of HIV screening within the Northern Ireland Blood Transfusion Service and participation in national AIDS committees such as EAGA. A local initiative involved the setting up of an informal group with representatives of the DHSSNI, the four health boards, and clinicians most closely involved with AIDS, the aim of which was “to provide a co-ordinated approach to publicity and education in the Province.” Note on AIDS – the position in Northern Ireland 18 November 1986 p1 DHSC0046919_006
(576) Written Statement of Sir Richard Needham para 42 WITN5595001
(577) Written Statement of Sir Richard Needham para 16, para 31 WITN5595001
(578) Written Statement of Lord Norman Fowler paras 2.16-2.17 WITN0771001
(579) Written Statement of Lord Norman Fowler para 2.20 WITN0771001
(580) Written Statement of Lord Barry Jones paras 37-39 WITN5708001
(581) Dr Andrzej Rejman Transcript 10 May 2022 p41 INQY1000203
(582) Dr Hillary Pickles Transcript 12 May 2022 p58 INQY1000205
(583) Letter from Michael Abrams to Dr Crompton 6 September 1984 HSSG0010054_009
(584) Letter from J D H Evans to Jayant Desai 16 January 1990 p3 DHSC0044895
(585) Letter from A J Beale Solicitors to Jayant Desai 25 October 1989 pp1-2 DHSC0019634_001, Appendix A Legal Framework of Health Services in Wales DHSC0019634_002
(586) Letter from Dr Crompton to Chief Administrative Medical Officers 23 November 1984 HSSG0010056_009
(587) Letter from A J Beale Solicitors to Jayant Desai 25 October 1989 DHSC0019634_001
(588) Which was copied to the Welsh Office. Memo from John Parker to Janet Walden 3 May 1983 DHSC0001651. According to a later letter produced for the purposes of the HIV litigation, this was the Welsh Office’s first consideration of the risk of infection from AIDS. Letter from J D H Evans to Jayant Desai 16 January 1990 p3 DHSC0044895. For the reasons discussed earlier in this chapter, this was too late: the risks should have been appreciated and considered by the beginning of 1983.
(589) This is a more fulsome account of Dr Napier’s views, since the article in the Western Mail records him as saying “The disease certainly exists but there is no proof as to how it is transmitted. All the evidence so far is circumstantial and I feel there is a need for people receiving transfusions to be reassured that they are only one of tens of thousands of people who can expect to receive complication-free treatment.” He was also reported in the newspaper as saying “We have been aware of this disease for some time and it has not caught us unaware” Western Mail Blood virus assurance 3 May 1983 DHSC0001652
(590) Memo from Dr Ferguson-Lewis to Dr Donald Lovett 3 May 1983 HSSG0010055_004
(591) Minutes of Medical Services Health Professional Group meeting 4 May 1983 pp1-3 HSSG0010055_001. Following the meeting Dr Skone wrote to chief administrative medical officers referring to the Cardiff case and to the need to acquaint all clinicians with the system of surveillance through CDSC. It was said also that Dr Crompton intended to write personally to consultants. Letter from Dr Skone to Chief Administrative Medical Officers 4 May 1983 HSSG0010056_032
(592) Dr Bloom misled the Haemophilia Society and others when he wrote on 4 May 1983 that he was unaware of any proven case “in our own haemophilic population” (Letter from Reverend Tanner to members of the Haemophilia Society 4 May 1983 DHSC0001228); he misled UKHCDO directors when he and Dr Rizza wrote that “one possible case” had been reported which “cannot be considered as a definite case” (Letter from Drs Bloom and Rizza 24 June 1983 p1 HCDO0000270_004); and when he told Dr Walford that he did not consider this suspected case should be regarded as a confirmed case (see her memo of 20 May 1983 at DHSC0002227_060). He had reported it to CDSC as a “probable” case of AIDS, as incontrovertibly it showed itself to be when Kevin Slater died of the disease. Surveillance of possible cases of AIDS case report 26 April 1983 p5 WITN3408009, Letter from C Lush to Dr Busby 9 July 1985 WITN3408024
(593) In relation to this matter, the minutes go on, somewhat curiously, to refer to “the associated consequences of lost jobs with implications for social services as well as for the health service.” Minutes of Medical Services Health Professional Group meeting 4 May 1983 p3 HSSG0010055_001
(594) The view that the risk of AIDS was greatly outweighed by the benefits of treatment with concentrates was still being maintained by the Welsh Office in late 1984: a statement to be used in response to requests on reports of AIDS deaths in South Glamorgan, dated 10 December 1984, asserted that “While this treatment [with imported concentrates] is now recognised to have carried some risk of the transmission of A.I.D.S., it is a very small risk compared with that of withholding such essential life-saving treatment in this group of patients, many of whom would undoubtedly have died from uncontrolled internal haemorrhage had it not been available or had it been withheld.” Statement to be used in response to requests on reports of AIDS deaths in South Glamorgan 10 December 1984 HSSG0010053_009. As discussed earlier in this chapter in relation to the DHSS’s decision-making, this both understated the risks of AIDS and overstated the benefits of concentrate treatment, and fell into the same error as the DHSS: seeing this as a binary, all-or-nothing issue. A meeting on 4 December 1984 involving Dr Ferguson-Lewis of the Welsh Office, Professor Bloom, Dr Napier and others had discussed the wording for the draft press statement. Minutes of South Glamorgan District Health Authority meeting 4 December 1984 p1 HSSG0010054_004
(595) Minutes of CMO and others meeting 4 May 1983 HSSG0010055_002
(596) Minutes of CMO Welsh Office meeting 19 November 1984 p1 HSSG0010054_008
(597) Minutes of CMO Welsh Office meeting 19 November 1984 p1 HSSG0010054_008. This was a reference to the Wessex donor.
(598) Minutes of CMO Welsh Office meeting 19 November 1984 p3 HSSG0010054_008
(599) Memo from Alan Dredge to the Parliamentary Under-Secretary of State 19 November 1984 HSSG0010054_005
(600) Memo from Alan Dredge to the Parliamentary Under-Secretary of State 19 November 1984 p1 HSSG0010054_005
(601) Memo from Alan Dredge to the Parliamentary Under-Secretary of State 19 November 1984 p1 HSSG0010054_005. This was in fact inaccurate, given what was known about the use of the donations from a donor in Wessex with AIDS, but the Welsh Office may not have known at the time the full picture in that regard. Letter from Dr Barnes to Dr Craske 5 November 1984 DHSC0001690
(602) Letter from Dr Galbraith to Dr Crompton 20 November 1984 HSSG0010054_002
(603) See the chapter on Self-Sufficiency.
(604) This point is made in Thompsons Scotland Submissions to the Infected Blood Inquiry 16 December 2022 p889 SUBS0000064, and is well founded.
(605) Penrose Inquiry SHHD Structure – 1980 to 1991 PRSE0000358. Lord Forsyth became Secretary of State for Scotland in 1990.
(606) Lord Norman Fowler Transcript 21 September 2021 p23 INQY1000144
(607) Written Statement of Lord Michael Forsyth para 27.2 WITN7126001. Commenting on the decision-making regarding the introduction of surrogate testing for non-A non-B Hepatitis, Lord Forsyth suggested that the DHSS was taking the lead, with SHHD and SNBTS represented at any meeting and ministers consulted before any decision was taken, and that he “would have been content with that.”Written Statement of Lord Michael Forsyth para 42.1 WITN7126001
(608) Penrose Inquiry SHHD Structure - 1980 to 1991 PRSE0000358
(609) Dr Macdonald’s statement to the Penrose Inquiry recorded that “It was expected that DHSS … would take the lead and that they and the ‘territorial departments’ would then implement a common policy, subject only to a modest degree of adaptation by the latter departments if required by local circumstances … DHSS had significantly larger numbers of both administrative and medical staff who could give their attention to health matters than SHHD. Consequently individual members of staff in DHSS could handle in greater depth a smaller number of issues than their opposite numbers in SHHD who had to spread their attention more widely.” Written Statement of Dr Iain MacDonald for Penrose Inquiry para 7 PRSE0002766
(610) For example, Dr Bell’s notes of such meetings in February 1978 and in February 1979. Notes on English and Welsh Regional Transfusion Directors meeting 22 February 1978 SCGV0000072_021, Notes on Regional Transfusion Directors meeting at DHSS 3 October 1979 SCGV0000072_005
(611) Written Statement of Duncan Macniven para 11.1 WITN7064001
(612) Written Statement of Duncan Macniven para 13.1 WITN7064001
(613) Lord Michael Forsyth Transcript 20 July 2022 p23 INQY1000231
(614) Professor Richard Tedder and Dr Graham Scott Penrose Inquiry Transcript 28 September 2011 pp130-131 PRSE0006049
(615) Written Statement of Duncan Macniven para 24.1 WITN7064001
(616) Duncan Macniven Transcript 19 July 2022 p6 INQY1000230
(617) Letter from Dr Bell to Mr Finnie 7 October 1981 SCGV0000132_182
(618) Senior medical officer in the SHHD with responsibility for blood services.
(619) Notes for Scottish Health Service Haemophilia Centre/Transfusion Service Directors meeting January 1983 p7 PRSE0001991
(620) The Observer Mystery disease threat 16 January 1983 DHSC0002223_085
(621) Jones et al Altered immunology in haemophilia The Lancet 1983 DHSC0002351_004
(622) The MMWR edition reported on the growth of the AIDS epidemic in the US, mentioned that recent victims included some children under 10, and carried the headnote to a report of the San Francisco baby case.
(623) Minutes of SNBTS Directors and Haemophilia Directors meeting 21 January 1983 p7 PRSE0001736
(624) Note on AIDS Lines to take DHSC0003824_173
(625) Memo from John Parker to Janet Walden 3 May 1983 DHSC0001651
(626) Memo from Dr Prentice to Dr Scott and others 5 May 1983 SCGV0000147_177
(627) Memo from Scottish Office to Dr Prentice 5 May 1983 SCGV0000147_180
(628) Letter from Dr McIntyre to John Davies 6 May 1983 p1 SCGV0000147_181
(629) Letter from Dr McIntyre to John Davies 6 May 1983 p2 SCGV0000147_181
(630) Memo from John Davies to John Mackay 6 May 1983 PRSE0004037
(631) On 14 November in The Observer which reported that people with haemophilia had AIDS in the US and that there was a “major speculation” that the AIDS virus was “carried in the blood”. The Observer No defence against gay disease 14 November 1982 MDIA0000010. Followed by, on 7 January 1983, Science in an article entitled Spread of AIDS Sparks New Health Concern reporting on the San Francisco baby case, andthat there were concerns that some 22 children were suspected of having AIDS, 3 daughters of the same mother, a sex worker with AIDS (but different fathers), and 7 confirmed cases in heterosexual males with haemophilia, 2 of whom were less than 10 years old, and one case in a homosexual male with haemophilia.Marx Spread of AIDS Sparks New Health Concern Science 7 January 1983 NHBT0015767. There were said to be 827 cases of AIDS identified in the US; and on 13 January 1983 the New England Journal of Medicine’s editorial suggested that such was the risk that cryoprecipitate might now be the treatment of choice. Desforges AIDS and preventive treatment in hemophilia New England Journal of Medicine 13 January 1983 PRSE0002410
(632) Minutes of SNBTS Directors and Haemophilia Directors meeting 21 January 1983 p7 PRSE0001736
(633) To (a) producing a leaflet, and (b) stopping accepting donations from prisons.
(634) Letter from Dr McIntyre to John Davies 6 May 1983 p2 SCGV0000147_181
(635) Dr Brian McClelland Transcript 27 January 2022 p156 INQY1000177
(636) Minutes of BTS Co-ordinating Group meeting 24 May 1983 p5 SBTS0003966_085, Guidance on AIDS and Blood Transfusion June 1983 PRSE0004850
(637) Minutes of SNBTS Directors meeting 14 June 1983 p3 MACK0001960_001
(638) Letter from Dr Bell to Dr McIntyre 15 June 1983 PRSE0002473
(639) Letter from Dr Bell to John Wastle 15 June 1983 PRSE0004396
(640) Gay Scotland AIDS IN SCOTLAND Mystery virus claims two July/August 1983PRSE0003358
(641) AIDS Guidelines for handling blood and blood products 30 June 1983 PRSE0001552
(642) File note of SHHD official on AIDS 28 June 1983 p3 SCGV0000147_171
(643) File note of SHHD official on AIDS 28 June 1983 p2 SCGV0000147_171
(644) Memo from John Parker to Christopher Joyce 1 July 1983 DHSC0002309_024. It was also sent to the Welsh Office and Northern Ireland Office.
(645) Acquired Immune Deficiency Syndrome: Issue of an Information Leaflet through the National Blood Transfusion Service p1 DHSC0002309_121
(646) AIDS leaflet p2 DHSC0002309_122
(647) Memo from John Parker to Christopher Joyce 4 July 1983 DHSC0002309_026
(648) Memo from SHHD to Dr Bell p1 SCGV0000147_161
(649) Memo from Dr Bell to Dr Scott 6 July 1983 PRSE0000049
(650) Memo from John Davies to John Mackay 11 July 1983 SCGV0000147_157
(651) Memo from John Davies to John Mackay 11 July 1983 SCGV0000147_157, AIDS leaflet SCGV0000147_158
(652) Letter from Dr Cash to Dr Brian McClelland 11 July 1983 SBTS0004433_052, AIDS leaflet SBTS0004433_053
(653) Memo from John Parker to Stephen Alcock 29 July 1983 DHSC0002327_016
(654) File note on AIDS leaflet 5 August 1983 SCGV0000147_142
(655) Letter from Dr Cash to Dr Brian McClelland 19 August 1983 PRSE0001400
(656) Scottish Office Press Release Information Leaflet on AIDS Issued 1 September 1983 PRSE0002778
(657) Written Statement of Dr Brian McClelland para 325 WITN6666001, Dr Brian McClelland Transcript 28 January 2022 p21 INQY1000178
(658) Note of Advisory Committee on NBTS meeting 17 October 1983 p2 SCGV0000083_048
(659) Minutes of Advisory Committee on NBTS meeting 17 October 1983 p4 CBLA0001763
(660) Minutes of Advisory Group on Hepatitis meeting 18 October p3 BPLL0008168
(661) The Scotsman 50pc rise in number of AIDS victims 31 October 1983 SCGV0000147_098
(662) “A few donors had responded by declaring that they were homosexual but the problem of how to screen out those who might present as donors in spite of the leaflet remains.” Minutes of Haemophilia and Blood Transfusion Working Group meeting 14 November 1983 pp1-2 PRSE0002581
(663) Memo from Dr Bell to Drs Scott and McIntyre 10 November 1983 pp3-4 SCGV0000052_086
(664) Minutes of SNBTS Directors meeting 8 December 1983 p2 PRSE0002899
(665) Minutes of SNBTS Directors and Haemophilia Directors meeting 2 February 1984 p3 PRSE0001556
(666) This article, which was noted in SHHD files and brought to Dr Bell’s attention, stated that it was the first diagnosed case in Scotland: Daily Record Victim of Gay Plague 17 February 1984 SCGV0000147_089
(667) Minutes of SNBTS Directors meeting 13 March 1984 p2 PRSE0003405
(668) Blood Transfusion Service Giving a donation of blood March 1984 SCGV0000147_088. What this might have been referring to from within the body of the document were the words “It will not be possible to accept your blood on this occasion if you have had symptoms which could suggest AIDS (Acquired Immune Deficiency Syndrome) or if you are in a group with an increased risk of AIDS.” It did not itself set out the symptoms, nor did it say what groups had increased risk of AIDS: for this purpose it referred people to a leaflet which would be available at donor sessions or that they could telephone the Blood Transfusion Service. The note is not clear as to whether the stronger tone met with his approval or the opposite.
(669) The mistake as to the length of trial approved by ministers is discussed above. It was meant to be three not six months long, but more than six months had now passed in any event.
(670) Minutes of Advisory Committee on the NBTS meeting 10 April 1984 pp2-3 WITN5282008_005
(671) Note of Advisory Committee on NBTS meeting 10 April 1984 p2 SCGV0000083_020
(672) Minutes of SNBTS Directors meeting 12 June 1984 PRSE0002709
(673) Memo from John Parker to Christopher Joyce 10 August 1984 DHSC0002309_044
(674) Letter from Dr Cash to Dr Bell 15 February 1984 PRSE0003911
(675) Note of CBLA Central Committee for Research and Development in Blood Transfusion meeting 28 February 1984 p2 SCGV0000052_073
(676) It is also unclear when this information was communicated to the DHSS.
(677) Memo from Hugh Morison to John Mackay 20 November 1984 SCGV0000147_058
(678) Memo from Hugh Morison to Mr Hoy 20 November 1984 SCGV0001147_139
(679) Memo from Hugh Morison to John Mackay 20 November 1984 SCGV0000147_058
(680) Memo from Miss Teale to Hugh Morison 21 November 1984 PRSE0002945
(681) Hansard written answer on AIDS SCGV0000148_082, Newspaper article titled AIDS leaflet 29 November 1984 HSOC0016013_001
(682) Note of Haemophilia Directors and SNBTS Representatives meeting 29 November 1984 PRSE0002066
(683) Scottish Information Office.
(684) Note of Haemophilia Directors and SNBTS Representatives meeting 29 November 1984 p2 PRSE0002066
(685) Memo from John Davies to John Mackay 5 December 1984 p1 PRSE0003032
(686) Professor Christopher Ludlam attended the meeting on 29 November 1984 and told the Inquiry: “I was waiting for the [UKHCDO] meeting on 10 December to happen to get the view of my colleagues and for a full discussion about the issues … I went to the meeting on 10 December in London at Elstree. It was a big meeting, we discussed it, it was important. It was a stressful meeting and I was keen to get other people’s views. I turned up at work the following morning to receive a phone call from the Yorkshire Post … he told me he would publish it on I think it was 20 December, which left me a handful of days to decide what to do.” Professor Christopher Ludlam Transcript 2 December 2020 pp83-85, pp89-90 INQY1000078
(687) As Lord Owen accepted. Lord David Owen Transcript 22 September 2020 p170 INQY1000055. And as implicit in Lord Fowler’s comments and those of Lord Clarke quoted in the opening paragraphs.
(688) On the contrary, the CMO through his May 1975 Dear Doctor letter effectively endorsed its continuance. Letter from Dr Yellowlees to all regional medical officers 1 May 1975 PRSE0000009
(689) Steps began to be taken to set up a surveillance scheme, but that was on the initiative of the CDSC and Dr Galbraith. O’Connor et al Correspondence discussing Acquired immune deficiency syndrome British Medical Journal23 April 1983 DHSC0003824_183
(690) This comment relates to the first four months of 1983, and to the growing media interest. Neither junior minister (John Patten; Lord Glenarthur) was then in post. The comment does not apply to them.
(691) May 1983 was also when there was some (limited) consideration by the Welsh Office and the SHHD; the evidence in relation to Northern Ireland is lacking but the likelihood is that no action was being taken by the DHSSNI, which looked to take its lead entirely from the DHSS.
(692) It was the subject of comment from Dr Walford internally, but that is all. Memo from Dr Sibellas to Dr Field 12 May 1983 DHSC0002227_038
(693) Or none that survives, or is referred to in any of the documents, or was recalled by any witness.
(694) Lord Simon Glenarthur Transcript 22 July 2021 pp169-170 INQY1000139, Lord John Patten Transcript 20 May 2022 pp87-90 INQY1000210, Lord Kenneth Clarke Transcript 27 July 2021 pp145-154 INQY1000141, Lord Norman Fowler Transcript 21 September 2021 pp152-158 INQY1000144
(695) Nor was any consideration given to using fresh frozen plasma in place of Factor 9, on a temporary basis, for the treatment of Haemophilia B.
(696) The word “them” is deliberate – it should have been a matter for both, acting together, in light of the patient’s wishes and the clinician’s medical knowledge, including the knowledge of alternatives. But the “them” would too often be seen by many at the time as referring just to the clinicians.
(697) Council of Europe Recommendation R(83)8 23 June 1983 p3 MACK0000307
(698) Council of Europe Recommendation R(83)8 23 June 1983 p3 MACK0000307
(699) This is despite the fact that an association between the same viral particle and the development of AIDS had been reported in Science by French researchers in May 1983.
(700) At the time, believed to be viral, but which also had not been identified at a microbiological level, and could not be directly tested for. World Health Organization Expert Committee on Hepatitis First Report March 1953 pp18-19 RLIT0000215
(701) And, indeed, despite it being known that from March 1983 that the Food and Drug Administration had recommended to all US commercial producers of factor concentrates that they should not prepare factor concentrates from the plasma of people who were homosexual, IV drug users, or from Haiti.
(702) The belief among some that there had been a six-month trial period was due to poor communication of what was being undertaken and for how long.
(703) Donald Acheson was only recently in post by this stage, and became pro-active in respect of AIDS a short while later.
(704) Government stands in a different position to the well-meaning friend who is the speaker in the familiar quote: the latter’s words may be understood as intending to be supportive, when the listener knows they have no basis other than friendship for using the phrase. Government is expected to be objective.
(705) Later the UK Haemophilia Centre Doctors’ Organisation. Individuals’ titles have also changed over time. This Report generally uses the title which the individual held at the time (eg Dr) when referring to contemporaneous materials or events, and the individual’s later or current title (eg Professor) when referring to their evidence to the Inquiry.
(706) See the account given in section 9 (History of Organisation of Haemophilia Care in the United Kingdom) of Dr Charles Rizza’s report for the HIV Haemophilia Litigation. Health Authority Defendants Report by Dr Charles Rizza pp38-44 HCDO0000394
(707) Arrangements for the Care of Persons Suffering from Haemophilia and Related Diseases HM 68 (8) 5 March 1968 OXUH0003712_002
(708) See, for example, a meeting chaired by Dr Henry Yellowlees (then Deputy Chief Medical Officer) at which Dr Rosemary Biggs recommended the establishment of a three-tier system. Meeting Notes regarding Haemophilia Centres 4 September 1969 p1 DHSC0100025_112
(709) This was not replaced until 1993 when HSG (93)(30) was published.
(710) The Oxford Centre was based at the Churchill Hospital; the Manchester Centre at Manchester Royal Infirmary; the Newcastle Centre at the Royal Victoria Infirmary; the Cardiff Centre at the University Hospital of Wales; and the Sheffield Centre at the Hallamshire Hospital.
(711) Memo of Health Services Development from Department of Health and Social Security February 1976 p4 DHSC0002179_070
(712) Minutes of Haemophilia Centre Directors meeting 1 October 1968 p4 HCDO0001013
(713) R Hughes and Dr D Ower from the Ministry of Health attended the 1 October 1968 meeting. Minutes of Haemophilia Centre Directors meeting 1 October 1968 p1 HCDO0001013. Dr W Obank from the DHSS attended the 1971 meeting. Minutes of Haemophilia Centre Directors meeting 5 April 1971 p1 HCDO0001014. From 1974 Dr Sheila Waiter from the DHSS was in attendance; she was replaced in due course by Dr Diana Walford, who in turn was replaced by Dr Alison Smithies. BPL was represented by Dr William d’A Maycock and then by Dr Richard Lane.
(714) The minutes of the meetings of the working parties were not, however, disseminated to all directors.
(715) Professor Christopher Ludlam Transcript 3 December 2020 p60 INQY1000079
(716) Professor Liakat Parapia Transcript 29 October 2020 p168 INQY1000070
(717) Rizza The Management of Haemophilia in the United Kingdom Thrombosis and Haemostasis 1976 p2 DHSC0000301
(718) Minutes of Reference Centre Directors meeting 27 January 1978 pp1-2 HCDO0000400
(719) Minutes of Haemophilia Reference Centre Directors meeting 23 February 1976 p1 HCDO0000395
(720) At a reference centre directors meeting in February 1984 consideration was given to whether the draft minutes should be provided to other persons and it was agreed that DHSS representatives who were invited to attend the meetings for specific purposes should not receive the minutes of the routine business of the meeting but only the part of the minutes which related to “the items for which they had been invited to attend and to which they had made a contribution”. Minutes of Haemophilia Reference Centre Directors meeting 13 February 1984 p2 HCDO0000415
(721) Professor Edward Tuddenham Transcript 22 October 2020 pp82-85 INQY1000067
(722) Minutes of Haemophilia Centre Directors meeting 13 January 1977 pp25-27 PRSE0002268
(723) According to the Haemophilia Centre Handbook 1980 p7 HSOC0000600
(724) Haemophilia Centre Handbook 1980 p8 HSOC0000600
(725) Haemophilia Centre Handbook 1980 p8 HSOC0000600
(726) Minutes of SNBTS Directors and Haemophilia Directors meeting 30 January 1981 p4 PRSE0000144
(727) The British Society for Haematology.
(728) This was Professor Savidge’s description of the group of reference centre directors.
(729) Written Statement of Professor Geoffrey Savidge for Archer Inquiry 17 September 2007 pp3-4 ARCH0002508_002
(730) See the chapter Treatment of Bleeding Disorders.
(731) For Haemophilia B the shift took place earlier, towards the beginning of the 1970s, when fresh frozen plasma was replaced with Factor 9 concentrates; this is considered later in this chapter.
(732) Minutes of Haemophilia Centre Directors Meeting 27 October 1972 pp8-9 HCDO0001015
(733) Professor Ingram was director of St Thomas’ Haemophilia Centre. Minutes of Haemophilia Reference Centre Directors meeting 23 February 1976 p4 HCDO0000395. That there should be any doubt over the need to explain the risks and advantages of home therapy is a matter of concern. Unfortunately, and as explored later in this chapter and elsewhere in this Report, most patients did not have the risks of therapy (whether at home or in hospital) explained to them, at least insofar as those risks involved increased use of factor concentrates and the consequential increased risk of viral transmission.
(734) Minutes of Haemophilia Centre Directors and Blood Transfusion Directors joint meeting 31 January 1974 p8 CBLA0000187
(735) Minutes of Haemophilia Centre Directors meeting 18 September 1975 p11 OXUH0003735
(736) Minutes of Haemophilia Centre Directors meeting 24 October 1977 p17 PRSE0001002
(737) Minutes of Reference Centre Directors meeting 27 January 1978 p8 HCDO0000400
(738) “Patients collecting supplies of cryoprecipitate for home treatment will bring a polystyrene box into which the cryoprecipitate is packed with some crushed Cardice [dry ice]. Patients are expected to take the cryoprecipitate straight home as the Cardice may not last for more than a couple of hours if the day is warm and the box is not air-tight.” The cryoprecipitate should then be placed in a deep-freeze at home. Haemophilia Centre Handbook 1980 p12 HSOC0000600
(739) Haemophilia Centre Handbook 1980 p51 HSOC0000600
(740) Minutes of Haemophilia Centre Directors meeting 1 October 1968 p4 HCDO0001013
(741) Minutes of Haemophilia Centre Directors meeting 5 April 1971 p11 HCDO0001014
(742) Minutes of Haemophilia Centre Directors meeting 27 October 1972 p5 HCDO0001015
(743) Minutes of Haemophilia Centre Directors meeting 13 January 1977 pp9-10 PRSE0002268
(744) Centre director at the Middlesex Hospital.
(745) Home Treatment Working Party 15 October 1979 p1 LOTH0000012_135
(746) See further the chapter on Self-Sufficiency.
(747) Minutes of Haemophilia Centre Directors meeting 27 October 1972 p10 HCDO0001015
(748) Minutes of Haemophilia Centre Directors and Blood Transfusion Directors joint meeting 31 January 1974 pp5-6 CBLA0000187
(749) Minutes of Haemophilia Reference Centre Directors meeting 23 February 1976 p3 HCDO0000395
(750) It is relevant to note that this conclusion was not based on the availability of screening for Hepatitis B; the report merely expressed the hope that “Perhaps now that the virus associated Australian antigen can be studied a method will be found to remove the antigen from concentrated materials, though of course its removal may not necessarily remove the virus.” Jaundice and Factor VIII Antibodies in Treated Patients with Haemophilia and Christmas Disease 5 April 1971 p11 DHSC0002173_048
(751) Jaundice and Factor VIII Antibodies in Treated Patients with Haemophilia and Christmas Disease 5 April 1971 p1, pp9-10 DHSC0002173_048
(752) See the chapter on Hepatitis Risks 1970 and After which addresses the Bournemouth outbreak and Dr John Craske’s reporting of it.
(753) See further the article published by Craske et al An outbreak of hepatitis associated with intravenous injection of Factor VIII concentrate The Lancet 2 August 1975 PRSE0001794
(754) Elsewhere in this report the approach of dismissing threats which are suspected but “not yet proved” or for which there is “no conclusive proof” is condemned as an inadequate response to threat: the absence of greater knowledge should not prevent action on the basis of credible material suggesting there is good reason to think there is a risk. Dr Biggs’ suggestion that commercial concentrates should not be given too bad a reputation probably came because she had recently published a study comparing hepatitis infection rates following the receipt of factor concentrates with those following the administration of cryoprecipitate. She found the advantage of cryoprecipitate was minimal. Although the concentrates did include some commercial, they were largely domestic, prepared from pool sizes with a mean of fewer than 200 donations. Despite being happy to use commercial products, as her comments suggest, she nonetheless continued to express enthusiasm for achieving self-sufficiency.
(755) Minutes of Haemophilia Centre Directors meeting 1 November 1974 p6 HCDO0001017
(756) Minutes of Haemophilia Centre Directors meeting 18 September 1975 pp4-5 OXUH0003735. “Anicteric” cases are those in which the skin does not yellow – there is no frank jaundice. The description is apt to cover cases in the acute phase in which there is no jaundice, and cases where the infection is chronic (ie has lasted over six months).
(757) Professor Gordon Lowe Transcript 9 December 2020 pp68-70 INQY1000083, Agenda of Symposium on Haemophilia 19 September 1975 PRSE0004632
(758) See the chapter Hepatitis Risks 1970 and After.
(759) Minutes of Haemophilia Reference Centre Directors meeting 23 February 1976 p4 HCDO0000395
(760) In fact the next meeting of haemophilia centre directors did not take place until January 1977 and there was no discussion of this issue. Minutes of Haemophilia Centre Directors meeting 13 January 1977 PRSE0002268. However, the reference centre directors returned to this topic in their second meeting in June 1976, in which Professor Edward Blackburn, reporting on his study of the relationship between doctors and the mass media, observed that “It seems that the Radio and Television authorities have the right to edit and comment on their presentations as they think fit.” Minutes of Haemophilia Centre Directors meeting 29 June 1976 p2 HCDO0000396. Remarkably there was still no discussion about the substance of the matters raised in the Blood Money documentary.
(761) Appendix C to Haemophilia Directors Hepatitis Working Party Hepatitis study 22 September 1977 p6 CBLA0000681_009
(762) Minutes of Haemophilia Centre Directors meeting 24 October 1977 p19 PRSE0001002
(763) Report of Haemophilia Centre Directors Hepatitis Working Party 20 August 1978 p1 CBLA0000831
(764) Dr Brian Colvin Transcript 6 October 2020 p49, pp132-133 INQY1000061
(765) Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 14 December 1977 pp1-3 HCDO0000544
(766) According to the next Working Party meeting in March 1978, studies of NHS Factor 8 associated patients were to begin in June 1978 with a number of centres interested in participating. Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 14 March 1978 p2 HCDO0000545
(767) In the same meeting, in making his report for the Hepatitis Working Party, Dr Craske reported that the DHSS had asked him to raise with the directors the suggestion that patients should be kept on one type (or preferably one batch) of concentrate for long periods. The directors “agreed that in principle this was a good idea which they tried to practise in any event, but it was extremely difficult to achieve this goal.” Minutes of Haemophilia Reference Centre Directors meeting 15 September 1978 p2, p5 HCDO0000401. The DHSS’ suggestion was not based on reducing the exposure of the recipient to donors, however; rather the reason for the suggestion, which was made by the Small Grants Committee, was to simplify analysis and presentation of results, increase the chances of identifying icterogenic material and permit the withdrawal of icterogenic bottles. Letter from R A Kingham to Dr Craske 27 July 1978 p1 DHSC0038713_065. In a letter to the Small Grants Secretariat in November 1978 Dr Craske, referring to the reference centre directors’ meeting, recorded that there was unanimous agreement that in theory maintaining patients on single batches or brands was a good method of reducing the risk of hepatitis, but that “factors such as the shortage of Factor VIII, the large numbers of patients under treatment and particularly the cost of maintaining large stocks of Factor VIII such a policy would involve meant that they did not consider it to be a practical policy to stick rigidly to this regime.” Letter from Dr Craske to R Kingham 9 November 1978 DHSC0038713_052
(768) Minutes of Haemophilia Reference Centre Directors meeting 15 September 1978 pp4-5 HCDO0000401
(769) Report of Haemophilia Centre Directors Hepatitis Working Party 20 August 1978 pp1-2 CBLA0000831
(770) Report of Haemophilia Centre Directors Hepatitis Working Party 20 August 1978 p4, pp5-6 CBLA0000831
(771) Report of Haemophilia Centre Directors Hepatitis Working Party 20 August 1978 p8 CBLA0000831
(772) Minutes of Haemophilia Centre Directors meeting 13 November 1978 pp11-12 HSOC0010549
(773) Minutes of Haemophilia Centre Directors meeting 20 August 1979 pp1-2 HCDO0000549
(774) Minutes of Haemophilia Reference Centre Directors meeting 15 October 1979 pp11-12 PRSE0000539
(775) Minutes of Haemophilia Centre Directors meeting 20-21 November 1979 p18 CBLA0001028
(776) In percentage terms it is 28.6%. Haemophilia Centre Directors Hepatitis Working Party 1979 Report p2, p6 HCDO0000135_023
(777) Minutes of Haemophilia Centre Directors meeting 20 February 1980 p1 HCDO0000550
(778) See, for example, Written Statement of Dr Olive Baugh, director of the associate centre at Chelmsford paras 5.1.2-5.1.3, para 9.1, paras 9.7-9.8, para 11.1 WITN5316001, Written Statement of Dr David Newsome, director of the associate centre at Blackburn para 19, paras 44-46 WITN3080002, Written Statement of Dr Diana Samson, director of the centre at the Charing Cross Hospital para 24 WITN4673001
(779) The focus for most of this chapter is on treatment policy and practice with regard to patients with Haemophilia A. That reflects the fact that almost all treatment for Haemophilia B was, in the relevant period, with NHS Factor 9 concentrates. Haemophilia B treatment is addressed later in this chapter. Treatment for von Willebrand disorder varied a little more between centres, but was predominantly with cryoprecipitate and NHS concentrate. Again the position in relation to von Willebrand disorder is addressed later in this chapter.
(780) Draft Personal Record for Dr Jones p1 WITN0841007
(781) Written Statement of Dr Peter Hamilton para 2.2 WITN4197005
(782) Draft Personal Record for Dr Jones p1 WITN0841007
(783) Jones Guidelines for the Organisation of a Haemophilia Centre CLOT September-December 1982 p4 WITN0841010. Further information regarding Newcastle Haemophilia Centre is set out in the Inquiry’s written and oral presentations: see Newcastle Haemophilia Centre Presentation Note INQY0000306 and the transcripts for 2, 3 and 9 February 2021 INQY1000092, INQY1000093, INQY1000094
(784) By August 1974, 23 patients were on home therapy using Hemofil. Letter from Dr Jones to Dr Sackwood 16 August 1974 p2 TYWE0000029. By November 1975 there were 43 patients on home therapy, with a mean Factor 8 usage of 18,796 units per patient per year. Draft Personal Record for Dr Jones p2 WITN0841007
(785) Written Statement of Dr Peter Jones para 15 WITN0841005. Dr Jones had, however, been an early fan of cryoprecipitate: see his 1967 letter to The Lancet and his 1972 article in Community Medicine. Letters to the Editor 8 April 1967 PJON0000136_001, Jones Answering the needs of haemophilic children and their families Community Medicine 28 July 1972 HSOC0022656
(786) Optimum Use of Factor VIII Preparations at Present Available in the United Kingdom September 1974 p1 OXUH0000757. There was no reference to NHS concentrate. The use of cryoprecipitate to cover bleeds, surgery and dental extraction, as a matter of choice despite the availability of commercial concentrate, shows that cryoprecipitate was not, as some later comment came to suggest, of little utility for those purposes.
(787) There is some evidence to suggest that it was under four: the recommendation in the February 1985 publication AIDS and the Blood was to give cryoprecipitate to children under the age of four. Dr Jones could not explain the disparity. Jones AIDS and the Blood A Practical Guide 1985 p45 RLIT0000046, Written Statement of Dr Peter Jones para 20 WITN0841038
(788) Written Statement of Dr Peter Jones para 17 WITN0841005, World Federation of Hemophilia 3rd European Regional Congress Programme 27-29 April 1976 pp26-29 WITN0841011
(789) Draft Personal Record for Dr Jones p12 WITN0841007
(790) Written Statement of Dr Peter Jones para 16 WITN0841005
(791) Figures from 1969 to 1974 related to the Newcastle Centre and the associate centre in Carlisle; figures from 1975 included other associate centres in the region as well.
(792) Letter from Dr Jones to Dr Liam Donaldson 23 February 1988 pp6-7 BPLL0002848_001
(793) According to the 1976 return, Hemofil was the main product used for the treatment of Haemophilia A. Annual Returns for Newcastle Haemophilia Centre 1976 p1 HCDO0001103. The 1977 annual return records a very substantial increase in the use of Hemofil (2.3 million units, compared to 1.6 million units of NHS product). Annual Returns for Newcastle Haemophilia Centre 1977 p1 HCDO0001188. In 1978 Hemofil, Factorate and Koate were all in use, along with NHS concentrate. Annual Returns for Newcastle Haemophilia Centre 1978 p1 HCDO0001285. The 1979 return shows Koate as the most used product, followed by Hemofil. Both NHS concentrates and Factorate were also used. The individual records enclosed with the 1979 return demonstrate that a number of individuals were treated with multiple products rather than kept on a single product. Annual Returns for Newcastle Haemophilia Centre 1979 p1, pp3-4 HCDO0001354
(794) Written Statement of Dr Peter Jones para 24 WITN0841005, Written Statement of Dr Peter Jones paras 7g, 7n, 8h, 9b, 9d, 27, 56a and 70 WITN0841038. There is certainly some contemporaneous evidence of shortfall: see for example the November 1975 report to the regional health authority stating that approximately 180,000 units of commercial concentrate had been bought in the past year to make up “the deficit in BTS supplied VIII products for in-patient use.” The use of anti-haemophilic globulin within the Northern Regional Haemophilia Service November 1975 p4 PJON0000099_001
(795) Letter from Dr Jones to Dr Maycock 3 February 1976 p2 CBLA0008631
(796) Written Statement of Anne Kirkman Collins answering HIV/Haemophiliacs Litigation Questionnaire p5 TYWE0000022. In his written evidence to the Inquiry Dr Jones asserted that the commercial concentrates were characterised by low volume, ease of preparation and ease of administration and that “if the NHS concentrates had been manufactured to the same general standards of the commercial concentrates, they would have been used exclusively for home therapy in the UK.”Written Statement of Dr Peter Jones para 27 WITN0841038
(797) In addition, Dr Peter Hamilton had a particular interest in liver disease. Following his appointment he wrote to Dr Craske on 21 June 1978 explaining that he intended to “make a special clinical study of the problems of liver disease in our haemophiliacs.” He would be observing them regularly for evidence of liver disease and would “take off enough serum for sending to you”(enclosed with the letter was the first batch of samples from approximately 40 home therapy patients). Letter from Dr Hamilton to Dr Craske 21 June 1978 PJON0000053_001
(798) Note on The Factor VIII Concentrates and Hepatitis June 1975 PJON0000047_001
(799) Jones Developments and Problems in the Management of Hemophilia Seminars in Hematology October 1977 p8 PJON0000147_001
(800) Jones Haemophilia Management A physician’s guide to the treatment of haemophilia 1979 p32 PJON0000002
(801) Haemophilia Society Northumbrian Branch Newsletter – Spring 1976 p3 HSOC0021641
(802) Haemophilia Society Northumbrian Branch Newsletter – Spring 1976 pp3-4 HSOC0021641. Underlining as in the original. These risks are as stated. It is an unorthodox way of expressing risk. To those used to odds of success, for example in placing bets, 3 to 1 seems the likeliest to result in infection, and a 3,000 to 1 chance the least. What was intended was that by comparison with a typical prescription of 3 packs of plasma to a patient (3 donors, 1 patient), an administration of what comes from 3,000 donors (who have contributed to the manufacturing pool) is 1,000 times as likely to carry infection. The Inquiry has no information on how, exactly, Dr Jones’ description was understood.
(803) Haemophilia Society Northumbrian Branch Newsletter – Autumn 1980 pp1-2 HSOC0021600
(804) Haemophilia Society Northumbrian Branch Newsletter – Autumn 1980 pp2-3 HSOC0021600. Underlining as in the original.
(805) Haemophilia and Home Therapy The Lancet 14 July 1979 p2 PRSE0003848
(806) Draft Personal Record for Dr Jones p26 WITN0841007
(807) See below and the chapter on People’s Experiences.
(808) Further information regarding Cardiff Haemophilia Centre is set out in the Inquiry’s written and oral presentations: see Counsel Presentation on Professor Bloom and the Cardiff Haemophilia Centre September 2020 INQY0000320 and the transcripts for 24 and 30 September 2020 and 8 October 2020 INQY1000057, INQY1000058 and INQY1000063
(809) This chapter considers treatment practices and policies at Cardiff, as well as the influence of the UKHCDO, and in particular the reference centre directors, Professor Bloom being the chair of UKHCDO between 1979 and 1985. His role in advising the DHSS, the Haemophilia Society and other bodies, committees or working groups is considered in other chapters of this Report.
(810) Letter from Professor Bloom to Dr Maycock 27 November 1972 CBLA0000098
(811) Minutes of Blood Transfusion Directors and Haemophilia Reference Centre Directors meeting 22 October 1976 p4 CBLA0000473
(812) ie NHS product from BPL at Elstree.
(813) File Note of Meeting between David Williams and Professor Bloom 24 August 1978 p1 IPSN0000334_019
(814) The figures are: cryoprecipitate 909,020 units; NHS concentrate 23,750; commercial 485,825. Annual Returns for Cardiff Haemophilia Centre 1976 p1 HCDO0001065
(815) The figures (for the treatment of 65 patients) are: cryoprecipitate 864,780 units; NHS concentrate 255,059; commercial 532,442. Annual Returns for Cardiff Haemophilia Centre 1977 p1 HCDO0001146
(816) The figures (for the treatment of 54 patients) are: cryoprecipitate 516,250 units; NHS concentrate 306,970; commercial 699,287. Annual Returns for Cardiff Haemophlilia Centre 1978 p1 HCDO0001241
(817) The figures (for the treatment of 55 patients) are: cryoprecipitate 830,620 units; NHS concentrate 328,528; commercial 1,122,705. Annual Returns for Cardiff Haemophlilia Centre 1979 p12 HCDO0001310
(818) Letter from Professor Bloom to GP 10 February 1975 WITN0047002. By way of comment, it is clear that Professor Bloom believed in early 1975 (ie after Hepatitis B could be tested for, albeit not very effectively when used as a screen, and the central risk was that of NANBH) first that freeze-dried concentrate was potentially “dangerous”; second that there was real danger of cross-infection from its use, and third that this was “unavoidable” if Factor 8 were to be used. The fact that Bloom had in the back of his mind the question whether the risk could be avoided or lessened is shown by the fact that he chose to mention unavoidability: it is a real pity that this thought did not lead him to look for ways of lessening the risk, and encouraging others to do so too. What he said speaks more of complacent resignation than of a call to arms.
(819) Professor Christopher Ludlam Transcript 1 December 2020 pp12-13 INQY1000077
(820) Dr Saad Al-Ismail Transcript 17 November 2020 p72 INQY1000074
(821) Haemophilia Litigation Report June 1990 p57 DHSC0001297. As explored in the chapter on Hepatitis Risks 1970 and After, this view of NANBH in the 1970s was wrong.
(822) Haemophilia Litigation Report June 1990 p59 DHSC0001297
(823) Report from Professor Bloom in Haemophilia Litigation 19 September 1991 pp1-2 DHSC0045373_049. The mid 1980s might be the time when the potentially serious nature of chronic hepatitis in haemophilia was “fully recognised”, but the potential seriousness of NANBH (Hepatitis C) should have been both “recognised” and acted upon by haemophilia centre directors in the second half of the 1970s.
(824) Further information regarding Manchester Haemophilia Centre is set out in the Inquiry’s written and oral presentations: see Counsel Presentation on Manchester Royal Infirmary Haemophilia Centre January 2021 INQY0000322 and Counsel Presentation on Manchester Royal Infirmary Haemophilia Centre Transcript 13 January 2021 INQY1000087
(825) Minutes of Haemophilia Society Executive Committee meeting 15 February 1973 p3 HSOC0029671_012
(826) Manchester Evening News A desperate choice 22 January 1970 HSOC0006206
(827) Factor VIII Concentrate for the treatment of Haemophilia CBLA0000121, Letter from Dr Delamore to Dr Maycock 4 December 1972 CBLA0000104
(828) Minutes of Reference Centre Directors meeting 27 January 1978 p8 HCDO0000400
(829) Statement of Dr Douglas Lee pp7-8 NHBT0096558_009. Dr Douglas Lee was also the regional transfusion director in Lancaster.
(830) The quantities were: 850,560 cryoprecipitate; 450,295 NHS concentrate; 325,087 Kryobulin and smaller amounts of Hemofil and Profiliate. A substantial volume of FEIBA was used: 564,420. Annual Returns for Manchester Haemophilia Centre 1976 p1 HCDO0001099
(831) The quantities were: 600,000 cryoprecipitate; 822,210 NHS concentrate; 404,855 Kryobulin; 402,459 Hemofil; 170,870 Koate and a small amount of Profilate. Annual Returns for Manchester Haemophilia Centre 1977 p1 HCDO0001184
(832) The quantities were: 477,180 cryoprecipitate; 961,284 NHS concentrate; 350,684 Kryobulin; 245,148 Factorate; 101,499 Profilate. Annual Returns for Manchester Haemophilia Centre 1978 p1 HCDO0001281
(833) The quantities were: 376,800 cryoprecipitate; 1,176,261 NHS concentrate; 200,450 Kryobulin; 336,620 Koate; 103,294 Factorate; and 82,175 Hemofil. Annual Returns for Manchester Haemophilia Centre 1979 p1 HCDO0001350. Dr Gunson’s statement (prepared for the purpose of litigation) observed that usage of cryoprecipitate in the North West region remained high in comparison with the national position, because of the policies adopted by the regional haemophilia service. Statement of Dr Gunson for HIV Litigation 11 January 1989 p13 NHBT0020196_001
(834) File Note of Meeting between David Williams and Dr Wensley 28 November 1978 IPSN0000338_011. An October 1981 letter from Dr Wensley noted that in the North West almost all Elstree Factor 8 was used for home treatment. Letters between Dr Wensley and Dr James Smith and Dr Gunson 28 October 1981 NHBT0089538
(835) Letter from Dr Gunson to G Oates 5 February 1986 p4 NHBT0096549. The purpose of Dr Gunson’s letter was to query whether, as at 1986, there was still a need for Dr Wensley’s role with the Blood Transfusion Service (as opposed to his duties at the haemophilia centre).
(836) Letter from Dr Delamore to Dr Rizza 9 March 1977 pp2-3 OXUH0000499
(837) The Haemophilia Society Haemophilia Today Seminar Report Manchester 1978 p5 PRSE0000421
(838) Emphasis added. Stevens et al Liver disease in haemophiliacs: An overstated problem? British Journal of Haematology 12 January 1983 p1 PRSE0002564
(839) Further information regarding St Thomas’ Haemophilia Centre is set out in the Inquiry’s written and oral presentations: see Counsel Presentation on St Thomas’ Haemophilia Centre 2 October 2020 INQY0000324 and Counsel Presentation on Haemophilia Centres Transcript 8 October 2020 INQY1000063
(840) Letter from Dr Ingram to Dr Maycock 10 October 1972 p1 CBLA0006658
(841) The Haemophilia Society News Bulletin August 1974 p6 HSOC0022702
(842) Letter from Professor Ingram to Dr Maycock 5 April 1976 BPLL0003662. This was a study involving two centres: St Thomas’ was using Elstree concentrate; Oxford was using concentrates produced by Dr Ethel Bidwell: Ingram et al Home treatment in haemophilia: clinical, social and economic advantages Clinical and Laboratory Haematology 4 January 1979 p4 DHSC0002191_019
(843) Letter from Professor Ingram to Dr Maycock 9 February 1978 pp1-2 CBLA0000728
(844) Minutes of Haemophilia Reference Centre Directors meeting 22 September 1980 p11 HCDO0000406
(845) Professor Geoffrey Savidge Archer Inquiry Transcript 19 September 2007 pp115-116 ARCH0000011
(846) Written Statement of Professor Geoffrey Savidge for Archer Inquiry 17 September 2007 p3 ARCH0002508_002
(847) The 1976 annual return showed: 432,135 units of cryoprecipitate; 758,500 units of NHS concentrate; and 343,712 units of commercial (Profilate, Hemofil, Kryobulin). Annual Returns for St Thomas’ Hospital Haemophilia Centre 1976 p1 HCDO0001119. The figures on the 1977 return are not easy to follow in terms of units but suggest that most treatment was with NHS concentrate or cryoprecipitate. Annual Returns for St Thomas’ Hospital Haemophilia Centre 1977 p10 HCDO0001206
(848) The cryoprecipitate use is similar to preceding years (7,408 bags) but commercial concentrates far outstripped NHS: 866,000 commercial (mostly Factorate and Hemofil) compared to 386,300 NHS. Annual Returns for St Thomas’ Hospital Haemophilia Centre 1978 p3 HCDO0001293
(849) This showed reduced usage of cryoprecipitate (2,736 bags), a reduced use of NHS Factor 8 (260,300 units) and over a million units of commercial (mostly Kryobulin and Factorate). Annual Returns for St Thomas’ Hospital Haemophilia Centre 1979 p1 HCDO0001374
(850) Written Statement of Professor Edward Tuddenham paras 6-8 WITN3435002. Professor Tuddenham left in 1986. Dr Kernoff remained director until 1991 when he was succeeded by Professor Christine Lee.
(851) Annual Returns for Royal Free Hospital Haemophilia Centre 1973 p1 RFLT0000356
(852) The return shows 978,950 units of cryoprecipitate, 361,804 units of commercial concentrate (Profilate, Factorate, Koate, Hemofil, and Kryobulin) and 305,930 units of NHS Factor 8 concentrate. Annual Returns for Royal Free Hospital Haemophilia Centre 1976 p1 HCDO0001111
(853) The return shows 2,102,310 units of cryoprecipitate, 601,681 units of commercial concentrates (Profilate, Koate, Hemofil, Kryobulin) and 510,200 units of NHS Factor 8. Annual Returns for Royal Free Hospital Haemophilia Centre 1977 p20 HCDO0001198
(854) Letter from Dr Dormandy and Dr Jenkins to Dr Lane 26 January 1978 CBLA0000722
(855) Dr Dormandy had been a pioneer of home therapy with cryoprecipitate, arranging for families to have freezers in their own homes for that purpose. Professor Christine Lee Lindsay Tribunal Transcript 25 July 2001 pp4-5 LIND0000326, Wellcome Witnesses to Twentieth Century Medicine Haemophilia: Recent History of Clinical Management September 1999 p45 RLIT0000022, Professor Christine Lee Transcript 20 October 2020 pp38-40 INQY1000065
(856) 1,630,552 units of commercial concentrates (Profilate, Factorate, Koate, Hemofil), 889,250 units of cryoprecipitate and 744,630 units of NHS Factor 8 concentrates. Annual Returns for Royal Free Hospital Haemophilia Centre 1978 p4 RFLT0000361
(857) 2,077,507 units of commercial concentrates (Profilate, Factorate, Koate, Hemofil), 655,850 units of cryoprecipitate and 593,165 units of NHS Factor 8 concentrates. Annual Returns for Royal Free Hospital Haemophilia Centre 1979 p12 RFLT0000362
(858) Professor Christine Lee Lindsay Tribunal Transcript 25 July 2001 p5 LIND0000326
(859) Minutes of Haemophilia Centre Directors and Blood Transfusion Centre Directors meeting 1 September 1978 p5 CBLA0000838
(860) Professor Edward Tuddenham Transcript 22 October 2020 pp19-23 INQY1000067
(861) Professor Edward Tuddenham Transcript 22 October 2020 pp137-138 INQY1000067
(862) Professor Edward Tuddenham Transcript 22 October 2020 p72 INQY1000067
(863) Letter from Dr Kernoff to Dr Colvin 27 April 1979 p2 BART0002487. The returns show that multiple products were purchased for the Royal Free. However there is some evidence that Dr Kernoff’s policy was to attempt to maintain individual patients on particular brands to minimise the risk of hepatitis. Letter from Dr Kernoff to Mr Jones 23 June 1980 p1 BART0000913. Professor Lee said that there was also a policy of keeping patients on the same batch until it ran out. Professor Christine Lee Transcript 20 October 2020 pp59-60 INQY1000065
(864) Minutes of Haemophilia Working Party NETR meeting 4 July 1979 p2 BART0000685. It was agreed that there would be developed a regional policy for investigation of home treatment patients for treatment-induced liver disease, a regional policy outlining the indication for liver disease and a regional proforma to follow up patients new to Factor 8 or 9 concentrate therapy.
(865) Minutes of Haemophilia Working Party NETR meeting 5 December 1979 p3 BART0000683. The “situations” to be investigated were: recognised clinical hepatitis; subclinical hepatitis; home treatment patients (for risks to family members); prophylactic treatment (for assessment of the possible increased risk of hepatitis); and monitoring of patients changing from cryoprecipitate to concentrate.
(866) Minutes of Haemophilia Working Party NETR meeting 5 December 1979 p2 BART0000683
(867) Professor Edward Tuddenham Transcript 22 October 2020 p18 INQY1000067
(868) Two patients were treated in 1981: by 1985 33 were treated with DDAVP. Annual Returns for Royal Free Haemophilia Centre 1981 p19 HCDO0001563, Annual Returns for Royal Free Haemophilia Centre 1985 HCDO0001946
(869) Professor Christine Lee Transcript 20 October 2020 pp42-45 INQY1000065
(870) Professor Christine Lee Transcript 20 October 2020 pp42-44 INQY1000065
(871) Levine et al Health of the Intensively Treated Hemophiliac, With Special Reference to Abnormal Liver Chemistries and Splenomegaly Journal of the American Society of Hematology July 1977 p7 RLIT0001221, Professor Christine Lee Transcript 20 October 2020 p43 INQY1000065
(872) See footnote 863.
(873) Forbes and Lowe Unresolved Problems in Haemophilia 1982 p33 RLIT0001242, Biggs et al at the International Forum Can Hemophilic Patients be Adequately Maintained with Cryoprecipitates? Vox Sanguinis 1972 p7 BAYP0000022_050
(874) Professor Edward Tuddenham Transcript 22 October 2020 p21 INQY1000067
(875) Craske An Outbreak of Hepatitis Associated with Intravenous Injection of Factor-VIII Concentrate The Lancet 2 August 1975 p5 PRSE0001794
(876) Further information regarding Oxford Haemophilia Centre is set out in the Inquiry’s written and oral presentations: see Counsel Presentation on Oxford Haemophilia Centre September 2020 INQY0000323 and the Counsel Presentation on Oxford Haemophilia Centre Transcript 9 October 2020 INQY1000064
(877) Biggs Haemophilia Treatment in the United Kingdom from 1969 to 1974 British Journal of Haematology 1977 (received 1976) p6, p10 PRSE0004645
(878) Biggs Haemophilia Treatment in the United Kingdom from 1969 to 1974 British Journal of Haematology 1977 (received 1976) p8 PRSE0004645
(879) Memo from Jean Spooner to Dr Biggs and Dr Rizza 28 August 1978 OXUH0003775_005, Memo from Jean Spooner to Dr Biggs and Dr Rizza 1 September 1976 OXUH0003775_080
(880) Letter from Dr Rizza to Dr R H Cowdell 12 July 1977 p2 OXUH0003761_052
(881) Wellcome Witnesses to Twentieth Century Medicine Haemophilia: Recent History of Clinical Management September 1999 p44 RLIT0000022
(882) Biggs Haemophilia Treatment in the United Kingdom from 1969 to 1974 British Journal of Haematology 1977 (received 1976) p11 PRSE0004645
(883) Letter from Dr Rizza to Dr Taylor 13 May 1977 OXUH0003761_036
(884) 1,577,162 units of NHS concentrate; 794,927 Profilate; 553,960 Factorate; 890,880 Koate; 347,428 Hemofil – totalling over 2.5 million units of commercial concentrates. Annual Returns for Oxford Haemophilia Centre 1977 p32 HCDO0001193
(885) Annual Returns for Oxford Haemophilia Centre 1978 HCDO0001290. The 1978 returns contain individual data but not the overall figures.
(886) Annual Returns for Oxford Haemophilia Centre 1979 p29 HCDO0001360
(887) Letter from Dr Rizza 5 December 1984 COLL0000002
(888) Health Authority Defendants Report by Dr Rizza p62 HCDO0000394. Citing Mannucci Asymptomatic Liver Disease in Haemophiliacs Journal of Clinical Pathology 1975 PRSE0000240, Spero et al Asymptomatic Structural Liver Disease in Hemophilia The New England Journal of Medicine 22 June 1978 PRSE0002523, and Preston et al Percutaneous Liver Biopsy and Chronic Liver Disease in Haemophiliacs The Lancet 16 September 1978 PRSE0003622. The report further observed (correctly) that from the first meeting in 1968 of haemophilia centre directors there was considerable interest in collecting information on the incidence of hepatitis in people with haemophilia following transfusion with different products, that surveys were carried out at regular intervals and the results discussed at most AGMs from 1971 onwards. “From its inception the UK Haemophilia Centre Directors’ Organisation was aware of post transfusion hepatitis in haemophiliacs and took steps to study the problem and to be involved in the surveillance of blood products in particular the heat treated materials when they became available in the early 1980’s. Little was known about non A non B hepatitis in 1972 when commercial Factor VIII concentrate became widely available and at first the condition was thought to be mild with little in the way of long term damage. The studies carried out on haemophiliacs in this country and abroad showed that this was not the case and that significant numbers of haemophiliacs in time went on to develop chronic liver disease.”Health Authority Defendants Report by Dr Rizza p74 HCDO0000394
(889) Professor Christopher Ludlam Transcript 1 December 2020 pp41-42 INQY1000077
(890) Professor Christopher Ludlam Transcript 1 December 2020 pp61-69 INQY1000077
(891) Penrose Inquiry Transcript of Professor Ian Hann and Dr Brian McClelland 6 May 2011 pp153-154 PRSE0006021, Penrose Inquiry Transcript of Professor Christopher Ludlam 17 June 2011 pp10-11 PRSE0006035, Medical Ethics Expert Panel Transcript 27 January 2021 pp79-80 INQY1000091
(892) The annual return shows 697,760 units of cryoprecipitate, 481,139 units of Edinburgh concentrate (ie that manufactured at the PFC) and a small amount of Oxford Factor 8. Annual Returns for Edinburgh Haemophilia Centre 1976 p1 HCDO0002459. The 1977 return records 636,510 units of cryoprecipitate and 271,396 units of Edinburgh concentrate. Annual Returns for Edinburgh Haemophilia Centre 1977 p1 HCDO0002460. The 1978 return records 644,325 units of cryoprecipitate and 272,249 units of Edinburgh concentrate. Annual Returns for Edinburgh Haemophilia Centre 1978 p1 HCDO0002461. The 1979 return shows 694,190 units of cryoprecipitate, and 200,826 units of NHS concentrate. Annual Returns for Edinburgh Haemophilia Centre 1979 p1 HCDO0002462
(893) The annual return for 1980 records for the treatment of Haemophilia A: 1,190,000 units of cryoprecipitate; 1,644,750 units of NHS concentrate; and what is probably (the return is not entirely legible) 164,000 units of Factorate. Annual Returns for Edinburgh Haemophilia Centre 1980 HCDO0002463. That was for the treatment of 51 Haemophilia A patients. The number of patients treated in the previous years were 57 (1976), 53 (1977), 51 (1978) and 45 (1979).
(894) Professor Gordon Lowe Transcript 9 December 2020 pp18-19 INQY1000083
(895) National Haemophilia Database Bleeding Disorder Statistics for the Penrose Inquiry p20 April 2012 PRSE0002887
(896) The return showed 488,055 units of cryoprecipitate, 562,003 units of NHS concentrate and 174,774 units of commercial. Annual Returns for Glasgow Royal Infirmary 1976 p1 HCDO0002488
(897) The return showed 416,550 units of cryoprecipitate, 742,098 units of NHS concentrate and 178,562 units of commercial. Annual Returns for Glasgow Royal Infirmary 1977 p1 HCDO0002489
(898) The return showed 559,210 units of cryoprecipitate, 828,889 units of NHS concentrate and 196,870 units of commercial. Annual Returns for Glasgow Royal Infirmary 1978 p1 HCDO0002490
(899) The return showed 350,990 units of cryoprecipitate, 992,776 units of NHS and 389,232 units of commercial. Annual Returns for Glasgow Royal Infirmary 1979 p1 HCDO0002491
(900) Professor Charles Forbes Penrose Inquiry Transcript 28 April 2011 p30 PRSE0006017
(901) Professor Charles Forbes Penrose Inquiry Transcript 28 April 2011 p47 PRSE0006017
(902) Professor Charles Forbes Penrose Inquiry Transcript 28 April 2011 p51 PRSE0006017
(903) Professor Charles Forbes Penrose Inquiry Transcript 28 April 2011 p58 PRSE0006017
(904) Professor Charles Forbes Penrose Inquiry Transcript 28 April 2011 p65 PRSE0006017
(905) Further information regarding Belfast Haemophilia Centre is set out in the Inquiry’s written and oral presentations: see INQY0000246 and the transcripts for 30 and 31 March 2021 INQY1000115 and INQY1000116
(906) Minutes of Haemophilia Reference Centre Directors meeting 14 September 1981 pp1-2 LOTH0000012_122
(907) Written Statement of Dr Elizabeth Mayne p1 WITN0736001
(908) A Profile of the Management of Haemophilia in Northern Ireland 25 March 1988 p2 RHSC0000067_002
(909) Expert Witness Report of Dr Elizabeth Mayne May 1990 p7 CBLA0000072_024. Relative safety is not emphasised – though “low donor exposure” probably had lower risk in mind.
(910) There is some evidence that it may have been in 1970. Patient discharge summary from Dr Mayne to Dr Wallace 12 February 1970 BHCT0000784
(911) Sixth Written Statement of Dr Elizabeth Mayne para 10.3 WITN0736009. This must have been on a named patient basis, given that the product was not yet licensed.
(912) Minutes of Haemophilia Centre Directors and Blood Transfusion Directors joint meeting 31 January 1974 p6 CBLA0000187
(913) Fourth Written Statement of Dr Elizabeth Mayne para 5 WITN0736006
(914) Fourth Written Statement of Dr Elizabeth Mayne para 7 WITN0736006
(915) Note of meeting between Dr Mayne and David Williams on 10 October 1978 IPSN0000332_021
(916) Letter from Dr Mayne to David Williams 12 January 1979 IPSN0000332_017
(917) Annual Returns for Belfast Haemophilia Centre 1976 p1 HCDO0000054_006
(918) The return showed substantial cryoprecipitate use (350,000), some NHS concentrate (36,690) and substantial commercial concentrates (Hemofil: 322,210, Kryobulin: 199,627). Annual Returns for Belfast Haemophilia Centre 1977 p1 HCDO0001137
(919) The return showed the use of cryoprecipitate (250,646), NHS concentrate (186,992), Hemofil (290,599) and Kryobulin (334,390). Annual Returns for Belfast Haemophilia Centre 1978 p7 HCDO0001231
(920) Less cryoprecipitate was used than previously (120,000 units) and some NHS concentrate was used (135,483 units). Annual Returns for Belfast Haemophilia Centre 1979 HCDO0001300
(921) Written Statement of Dr Elizabeth Mayne para 2 WITN0736007
(922) Written Statement of Dr Elizabeth Mayne para 26.4 WITN0736009
(923) Written Statement of Dr Elizabeth Mayne para 22.3 WITN0736009
(924) Expert Witness Report of Dr Elizabeth Mayne May 1990 p18 CBLA0000072_024, Spero et al Asymptomatic Structural Liver Disease in Hemophilia The New England Journal of Medicine 22 June 1978 PRSE0002523
(925) HIV Haemophilia Litigation Report by Dr Mayne p2 WITN0736011
(926) Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 p15 LIND0000323
(927) Professor Blackburn was also the chair of UKHCDO until 1979.
(928) Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 p1 LIND0000323
(929) See the chapter on Hepatitis Risks 1970 and After.
(930) Preston et al Percutaneous Liver Biopsy and Chronic Liver Disease in Haemophiliacs The Lancet 16 September 1978 PRSE0003622, Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 p3 LIND0000323. Dr Preston’s take on the 1978 study, as reported in 1999, was that “in 1978 we showed quite definitely that non-A, non-B was a very serious disorder. The Department of Health should have responded by pushing for ways to inactivate the virus in the blood, or given patients the choice of an alternative.” The Observer Whitehall in cover-up on tainted blood risk 21 November 1999 p1 HSOC0009730. He told the Inquiry that this accurately reflected his views. Professor Eric Preston Transcript 2 November 2020 pp37-38 INQY1000071
(931) Minutes of the Haemophilia Centre Directors Hepatitis Working Party meeting 15 December 1980 p2 HCDO0000554, Professor Eric Preston Transcript 2 November 2020 pp38-40 INQY1000071
(932) Preston et al Blood Product Concentrates and Chronic Liver Disease The Lancet 6 March 1982 PRSE0000384
(933) Cryoprecipitate 90,090 units; NHS concentrate 28,500 units; and commercial concentrates (Factorate, Hemofil, Kryobulin) 123,166 units. Annual Returns for Sheffield Haemophilia Centre 1976 p1 HCDO0001114
(934) Cryoprecipitate 4,970 units; NHS 248,705 units; commercial concentrates (Factorate, Koate, Kryobulin) 353,490 units in hospital. Annual Returns for Sheffield Haemophilia Centre 1977 p10 HCDO0001200. It is not entirely clear whether these figures on p10 of the return include the home treatment figures shown on p7 or whether the latter represent additional usage. A handwritten note records that “At this centre, ‘home treatment packs’ from ARMOUR have been used most of the time for home therapy.” Annual Returns for Sheffield Haemophilia Centre 1977 p7 HCDO0001200
(935) NHS concentrate 488,135 units; commercial concentrates (Factorate, Koate, Kryobulin) 491,614 units. Annual Returns for Sheffield Haemophilia Centre 1979 p1 HCDO0001368. The 1978 return is missing.
(936) 4,690 units of cryoprecipitate; 141,775 units of NHS concentrate; 800,852 units of commercial concentrates (Factorate, Hemofil, Kryobulin). Annual Returns for Sheffield Haemophilia Centre 1980 p1 HCDO0001466
(937) Written Statement of Professor Eric Preston para 14 WITN4002001
(938) Written Statement of Professor Eric Preston para 22 WITN4002001, Professor Eric Preston Transcript 2 November 2020 p18 INQY1000071
(939) Professor Eric Preston Transcript 2 November 2020 p17 INQY1000071
(940) This description was provided by Professor Michael Makris, who worked at the Royal Hallamshire from 1987, becoming its director in 2000 on Professor Preston’s retirement, and was confirmed by the latter to be correct. Written Statement of Professor Michael Makris para 9.10 WITN4033001, Professor Eric Preston Transcript 2 November 2020 pp20-21 INQY1000071
(941) Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 p46 LIND0000323, Professor Eric Preston Transcript 2 November 2020 pp23-24 INQY1000071
(942) Minutes of West Midlands Regional Health Authority Working Party on Treatment of Haemophiliacs meeting 13 May 1976 p2 SHIN0000044
(943) Further information regarding Birmingham Haemophilia Centre is set out in the Inquiry’s written and oral presentations: see Counsel Presentation on Birmingham Haemophilia Centre 21 October 2020 INQY0000319 and Professor Ian Franklin Transcript 27 October 2020 INQY1000068
(944) The working party was made up of haemophilia directors from the regional centres, including from both Birmingham hospitals, Hereford, North Staffordshire (Dr Ibbotson), Shrewsbury (Dr O’Shea and Dr Mann), Worcester (Dr Payne) and Wolverhampton (Dr Allan). The meetings were chaired by Dr Shinton, the director of the Coventry Centre. A representative from the West Midlands Blood Transfusion Centre also attended (initially Dr Bird and then Dr Ala).
(945) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 18 December 1975 pp1-2 SHIN0000045
(946) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 23 May 1977 p2 SHIN0000042
(947) Annual Returns for Birmingham Haemophilia Centre 1976 p8 HCDO0000028_002
(948) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 21 November 1977 p3 SHIN0000041
(949) Agenda for Working Party on the Treatment of Haemophiliacs meeting 14 May 1979 p5 CBLA0000940, Annual Returns for Birmingham Haemophilia Centre 1977 p1 HCDO0001139. At a meeting of the Working Party in May 1978 it was reported that Factor 8 usage for the region had increased slightly but cryoprecipitate use had fallen dramatically from what had been estimated for the year. Dr Stuart of QEH stated that only a third of QEH’s Factor 8 product was received from the Lister, meaning the two-thirds shortfall had to be made up with commercial concentrates. Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 15 May 1978 p2 SHIN0000040
(950) Agenda for Working Party on the Treatment of Haemophiliacs meeting 14 May 1979 p6 CBLA0000940, Annual Returns for Birmingham Haemophilia Centre 1978 p1 HCDO0001233
(951) Annual Returns for Birmingham Haemophilia Centre 1979 p1 HCDO0001302
(952) Written Statement of Professor Frank Hill para 2.5 WITN3087001
(953) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 22 November 1976 p2 SHIN0000043
(954) Minutes of Haemophilia Centre Directors meeting 20-21 November 1979 pp17-18 CBLA0001028
(955) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 3 December 1979 p3 SHIN0000037
(956) Dr Brian Colvin Archer Inquiry Transcript 12 June 2008 p140 ARCH0000012, Dr Brian Colvin Transcript 6 October 2020 pp39-40 INQY1000061
(957) Dr Brian Colvin Transcript 6 October 2020 p42 INQY1000061
(958) Craske An Outbreak of Hepatitis Associated with Intravenous Injections of Factor-VIII Concentrate The Lancet 2 August 1975 PRSE0001794, Dr Brian Colvin Transcript 6 October 2020 pp47-48 INQY1000061
(959) Preston et al Percutaneous Liver Biopsy and Chronic Liver Disease in Haemophiliacs The Lancet 16 September 1978 PRSE0003622, Dr Brian Colvin Transcript 6 October 2020 pp62-65 INQY1000061
(960) Letter from Dr Kernoff to Dr Colvin 27 April 1979 p2 BART0002487, Dr Brian Colvin Transcript 6 October 2020 pp69-70 INQY1000061
(961) Guidelines from NETR Association of Haematologists 16 May 1979 p1 BART0000684
(962) Minutes of Association of Haematologists NETR Haemophilia Working Party meeting 12 December 1979 p2 BART0000682
(963) Dr Brian Colvin Transcript 6 October 2020 p97, p143, pp147-148 INQY1000061. DDAVP would be attempted for patients with mild haemophilia and those with von Willebrand disorder. Patients with moderate haemophilia would be treated with concentrates.
(964) Dr Brian Colvin Transcript 6 October 2020 pp124-133 INQY1000061
(965) Dr Brian Colvin Transcript 6 October 2020 p133, p161 INQY1000061
(966) Further information regarding Leeds Haemophilia Centre is set out in the Inquiry’s Counsel Presentation on Smaller Haemophilia Centres: St James’ Hospital, Leeds June 2021 INQY0000259
(967) The annual return for 1977 shows 76 patients with Haemophilia A treated during the year, with Factorate, Koate and Kryobulin all in use (and exceeding the amount of NHS concentrate used). Annual Returns for Leeds Haemophilia Centre 1977 p9 HCDO0001174
(968) The annual return for 1978 showed the use of 5,000 units of cryoprecipitate, as against 590,335 units of NHS concentrate and 978,034 units of commercial concentrate (Factorate and Kryobulin) for the treatment of 74 patients with Haemophilia A. Annual Returns for Leeds Haemophilia Centre 1978 HCDO0001271
(969) The annual return for 1979 showed the use of 472,540 units of NHS concentrate but 1,242,198 units of Factorate. Annual Returns for Leeds Haemophilia Centre 1979 p1 HCDO0001340
(970) Those returns which contain individual patient data show patients often being treated with more than one type of commercial concentrate during the year. See for example Annual Returns for Leeds Haemophilia Centre 1977 p1 HCDO0001174, Annual Returns for Leeds Haemophilia Centre 1978 p2 HCDO0001271
(971) Minutes of Haemophilia Centre Directors meeting 5 April 1971 pp2-4 HCDO0001014, Minutes of Haemophilia Centre Directors meeting 1 November 1974 pp2-4 HCDO0001017
(972) Minutes of Haemophilia Centre Directors meeting 1 November 1974 p5 HCDO0001017
(973) Minutes of Haemophilia Centre Directors meeting 18 September 1975 pp4-5 OXUH0003735
(974) Minutes of Haemophilia Centre Directors meeting 13 January 1977 pp10-11 PRSE0002268
(975) Minutes of Haemophilia Centre Directors meeting 20-21 November 1979 pp18-19 CBLA0001028
(976) See the chapter on Self-Sufficiency.
(977) Written Statement of Dr David Bevan pp23-24 WITN4106001, Dr David Bevan Transcript 12 January 2021 pp103-106 INQY1000086. Dr Bevan described it as “this myth of harmlessness”.
(978) As, for instance, in Edinburgh at the start of the 1970s when death was caused not just to patients but to staff.
(979) The papers and the discussions were published in 1982, edited by Dr Forbes and Dr Lowe of the Royal Infirmary, Glasgow. Forbes and Lowe Unresolved Problems in Haemophilia 1982 RLIT0001242
(980) Minutes of Haemophilia Reference Centre Directors meeting 22 September 1980 pp5-6 HCDO0000406. The minutes also record it being said that “The patients who were thought to have suffered from Non-A and Non-B hepatitis had very mild clinical symptoms.”
(981) Minutes of Haemophilia Reference Centre Directors meeting 22 September 1980 p11 HCDO0000406
(982) Minutes of Haemophilia Centre Directors meeting 30 September 1980 p6 PRSE0003946
(983) Minutes of Haemophilia Centre Directors meeting 30 September 1980 p10 PRSE0003946
(984) Minutes of Haemophilia Centre Directors meeting 30 September 1980 p15 PRSE0003946
(985) Forbes and Lowe Unresolved Problems in Haemophilia 1982 p7 RLIT0001242
(986) From the Department of Pathology, Western Infirmary, Glasgow.
(987) Forbes and Lowe Unresolved Problems in Haemophilia 1982 p11 RLIT0001242
(988) Forbes and Lowe Unresolved Problems in Haemophilia 1982 pp19-20 RLIT0001242
(989) All of the Royal Free Hospital.
(990) Forbes and Lowe Unresolved Problems in Haemophilia 1982 pp37-38, p42 RLIT0001242
(991) Of the Department of Histopathology at the Royal Free Hospital. Forbes and Lowe Unresolved Problems in Haemophilia 1982 p44 RLIT0001242
(992) All of the Royal Hallamshire Hospital, Sheffield.
(993) Chronic persistent hepatitis was described by them as typically a benign disorder that rarely proceeds to cirrhosis, whereas chronic active (aggressive) hepatitis carries a significant risk of progression to cirrhosis. Forbes and Lowe Unresolved Problems in Haemophilia 1982 p48 RLIT0001242
(994) Forbes and Lowe Unresolved Problems in Haemophilia 1982 p52-53, p58 RLIT0001242
(995) Professor Howard Thomas Transcript 24 March 2021 pp100-102 INQY1000112. Professor Thomas published in August 1981 further information regarding the liver biopsies that had been carried out, which showed that in a group of eight patients with haemophilia the biopsies indicated four with chronic active hepatitis and four with chronic persistent hepatitis. Bamber et al Ultrastructural Features in Chronic Non-A, Non-B (NANB) Hepatitis: A Controlled Blind Study Journal of Medical Virology 1981 RLIT0000497
(996) Dr Mark Winter Transcript 1 October 2020 pp41-42 INQY1000059
(997) Dr Mark Winter Transcript 1 October 2020 p52 INQY1000059
(998) Dr Mark Winter Transcript 1 October 2020 p58 INQY1000059
(999) Dr Mark Winter Transcript 1 October 2020 p59 INQY1000059
(1000) The Hepatitis Working Party met on 15 December 1980 and discussed the Sheffield/Royal Free biopsy work that had been presented at the symposium. Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 15 December 1980 HCDO0000554. In September 1981 the Working Party considered the hepatitis surveillance data and recorded that an application had been made to the MRC with a view to a prospective study of patients with mild defects undergoing treatment requiring concentrate cover. Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 11 September 1981 pp1-2 PRSE0003474
(1001) This issue was raised at the reference centre directors’ meeting on 23 February 1981 and it was decided to ask the Hepatitis Working Party to consider and advise. Meeting of Haemophilia Reference Centre Directors meeting 23 February 1981 p10 HCDO0000407
(1002) Minutes of Haemophilia Reference Centre Directors meeting 14 September 1981 p5 LOTH0000012_122
(1003) Minutes of Haemophilia Centre Directors meeting 9 October 1981 pp20-22 DHSC0001312, Haemophilia Centre Directors Hepatitis Working Party Report for 1980-81 p4 HCDO0000135_017
(1004) Product usage is in international units, unless otherwise stated.
(1005) Annual Returns for Newcastle Haemophilia Centre 1980 p1 HCDO0001451, Annual Returns for Newcastle Haemophilia Centre 1981 p15 HCDO0001552, Annual Returns for Newcastle Haemophilia Centre 1982 p1 HCDO0001651
(1006) Annual Returns for Free Haemophilia Centre 1980 p1 RFLT0000363, Annual Returns for Free Haemophilia Centre 1981 p1 HCDO0001563, Annual Returns for Free Haemophilia Centre 1982 p1 HCDO0001662
(1007) Annual Returns for Cardiff Haemophilia Centre 1980 p1 HCDO0001405, Annual Returns for Cardiff Haemophilia Centre 1981 p1 HCDO0001503, Annual Returns for Cardiff Haemophilia Centre 1982 p1 HCDO0001606
(1008) Annual Returns for Belfast Haemophilia Centre 1980 p1 HCDO0001394, Annual Returns for Cardiff Haemophilia Centre 1981 p1 HCDO0001493 (figures barely legible), Annual Returns for Cardiff Haemophilia Centre 1982 p1 HCDO0001596
(1009) Annual Returns for Glasgow Haemophilia Centre 1980 p1 HCDO0002492, Annual Returns for Glasgow Haemophilia Centre 1981 p1 HCDO0002493, Annual Returns for Glasgow Haemophilia Centre 1982 p1 HCDO0002494
(1010) Annual Returns for Edinburgh Haemophilia Centre 1980 p1 HCDO0002463, Annual Returns for Edinburgh Haemophilia Centre 1981 p1 HCDO0002464, National Haemophilia Database (“NHD”) and UKHCDO Pivot Table: Annual consumption of CFC 1976 to 1994 18 March 2022 WITN3826017, Annual Returns for Edinburgh Haemophilia Centre 1982 p1 HCDO0002465.
(1011) Annual Returns for Sheffield Haemophilia Centre 1980 p1 HCDO0001466, Annual Returns for Sheffield Haemophilia Centre 1981 p1 HCDO0001567, Annual Returns for Sheffield Haemophilia Centre 1982 p1 HCDO0001665
(1012) Annual Returns for St Thomas’ Haemophilia Centre 1980 p1 HCDO0001471, Annual Returns for St Thomas’ Haemophilia Centre 1981 p1 HCDO0001575, Annual Returns for St Thomas’ Haemophilia Centre 1982 p1 HCDO0001671
(1013) Annual Returns for Manchester Haemophilia Centre 1980 p1 HCDO0001447, Annual Returns for Manchester Haemophilia Centre 1981 p1 HCDO0001548, Annual Returns for Manchester Haemophilia Centre 1982 p3 HCDO0001645
(1014) Annual Returns for Oxford Haemophilia Centre 1980 OXUH0003430_003, Annual Returns for Oxford Haemophilia Centre 1981 OXUH0003451_001, Annual Returns for Oxford Haemophilia Centre 1982 p1 HCDO0001657. One person was treated with cryoprecipitate in 1981. NHD and UKHCDO Pivot Table: Annual consumption of CFC 1976 to 1994 18 March 2022 WITN3826017
(1015) Annual Returns for Birmingham Haemophilia Centre 1980 p1 HCDO0001396, Annual Returns for Birmingham Haemophilia Centre 1981 p1 HCDO0001495, Annual Returns for Birmingham Haemophilia Centre 1982 p1 HCDO0001598
(1016) Annual Returns for Bristol Haemophilia Centre 1980 p1 HCDO0001402, Annual Returns for Bristol Haemophilia Centre 1981 p1 HCDO0001500, Annual Returns for Bristol Haemophilia Centre 1982 p1 HCDO0001603
(1017) Annual Returns for Leeds Haemophilia Centre 1980 p1 HCDO0001435, Annual Returns for Leeds Haemophilia Centre 1981 p1 HCDO0001536, Annual Returns for Leeds Haemophilia Centre 1982 p1 HCDO0001635
(1018) Annual Returns for Liverpool Haemophilia Centre 1980 p1 HCDO0001440, Annual Returns for Liverpool Haemophilia Centre 1981 p1 HCDO0001542, Annual Returns for Liverpool Haemophilia Centre 1982 p1 HCDO0001640
(1019) Annual Returns for London Haemophilia Centre 1980 p1 HCDO0001442, Annual Returns for London Haemophilia Centre 1981 p1 HCDO0001564, Annual Returns for London Haemophilia Centre 1982 p1 HCDO0001642
(1020) Annual Returns for Lewisham Haemophilia Centre 1980 p1 HCDO0001438, Annual Returns for Lewisham Haemophilia Centre 1981 p1 HCDO0001539, NHD and UKHCDO Pivot Table: Annual consumption of CFC 1976 to 1994 18 March 2022 WITN3826017, Annual Returns for Lewisham Haemophilia Centre 1982 p1 HCDO0001637
(1021) Annual Returns for Cambridge Haemophilia Centre 1980 p1 HCDO0001404, Annual Returns for Cambridge Haemophilia Centre 1981 p1 HCDO0001502, Annual Returns for Cambridge Haemophilia Centre 1982 p1 HCDO0001605
(1022) Annual Returns for Coventry Haemophilia Centre 1980 p1 HCDO0001414, Annual Returns for Coventry Haemophilia Centre 1981 p1 HCDO0001512, Annual Returns for Coventry Haemophilia Centre 1982 p1 HCDO0001614
(1023) Annual Returns for Kent Haemophilia Centre 1980 p1 HCDO0001448, Annual Returns for Kent Haemophilia Centre 1981 p1 HCDO0001549, Annual Returns for Kent Haemophilia Centre 1982 p1 HCDO0001647
(1024) Emphasis added. Letter from Dr Colvin to David Watters 8 October 1986 p1 HSOC0003432
(1025) Dr Mark Winter Transcript 1 October 2020 p70 INQY1000059
(1026) Present at this meeting at St Thomas’ were Professor Bloom (Chair), Dr Rizza (Oxford), Dr Forbes (Glasgow), Dr Jones (Newcastle), Dr Kernoff (Royal Free), Dr Ludlam (Edinburgh), Dr Matthews (Oxford), Dr Mayne (Belfast), Dr Prentice (Glasgow), Dr Preston (Sheffield), Dr Savidge (St Thomas’), Dr Tuddenham (Royal Free), Dr Wensley (Manchester), Dr Craske, Dr Stevens (representing Dr Delamore) and Dr Aronstam (Treloar’s). Minutes of Haemophilia Reference Centre Directors meeting 6 September 1982 p11 HCDO0000410
(1027) Dr Rizza reported that there had been an increased amount of NHS concentrate used by centres during 1981; he felt that “this was an encouraging sign and hoped that the increased supplies would continue to be available to Centres.” Minutes of Haemophilia Reference Centre Directors meeting 6 September 1982 p7 HCDO0000410, Annual Returns for Haemophilia Centres summary 1981 1 September 1982 CBLA0001612
(1028) It was agreed that it was not necessary for the estimated requirements for Factor 8 to be revised at the present time but that the matter would be reviewed the following year. Minutes of Haemophilia Reference Centre Directors meeting 6 September 1982 p8 HCDO0000410
(1029) Minutes of Haemophilia Reference Centre Directors meeting 6 September 1982 pp8-11 HCDO0000410
(1030) Minutes of Haemophilia Reference Centre Directors meeting 6 September 1982 p11 HCDO0000410
(1031) Minutes of Haemophilia Centre Directors meeting 13 September 1982 p10 CBLA0001619. A report from Ken Milne of the Haemophilia Society, setting out items that he thought were of particular interest from the meeting on 13 September, made no mention of AIDS at all, reinforcing the impression given by the minutes that AIDS was barely discussed. Report on Haemophilia Centre Directors meeting 13 September 1982 DHSC0001313. Professor Ludlam said that he could not defend the word “remote”. Professor Christopher Ludlam Transcript 3 December 2020 p65 INQY1000079
(1032) It was minuted that an application to the MRC for prospective study funding had been refused and the DHSS no longer had any funds available. The preliminary study of 28 previously untreated or minimally treated patients at Oxford with mild coagulation defects was discussed. Nine previously untreated patients had developed NANBH. Some had received NHS Factor 8, one US commercial and one NHS Factor 9. Dr Craske proposed to extend the project to other centres to compare attack rates of NANBH after transfusion with different brands and to follow up patients to determine long-term sequelae. He also hoped to collect sera to develop tests. There was a discussion about new “hepatitis reduced” concentrates and a reference to pasteurisation by heat. The only way to evaluate preparations for freedom from NANBH was, it was suggested, by chimpanzee inoculation or prospective study in “susceptible human subjects”.
Dr Kernoff proposed to follow up patient records at the Royal Free to see if further information was available to evaluate comparative risks of NANBH after transfusion with NHS Factor 8 and NHS Factor 9. Dr Craske agreed to revise and circulate the prospective study protocol. It would be open to any haemophilia centre directors to use the protocol when evaluating any new concentrate products; directors would be invited to report the results in a standardised way to the Working Party and to retain serial samples of each patient’s serum so a collection would be available to evaluate any new marker tests for NANBH. Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 13 September 1982 pp2-4 HCDO0000556
(1033) Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 13 September 1982 p5 HCDO0000556. On the following day, 14 September, a symposium was held in Manchester on “Current Topics in Haemophilia”. Professor Bloom wrote a foreword to the publication of the proceedings of the symposium, which began by announcing that “These are exciting times in the haemophilia world” and concluded by observing that “Unfortunately, true to form, new hazards are appearing on the horizon including the acquired immune deficiency syndrome. The impact of these will no doubt feature in our next Symposium.” Wensley Current topics in haemophilia: proceedings of the symposium held in Manchester 14 September 1982 p4 DHSC0002221_003
(1034) See the chapter on Knowledge of the Risks of AIDS.
(1035) That Dr Craske wrote to CDC on this date and had spoken to Dr Kernoff is apparent from a later letter. Letter from Dr Dale Lawrence to Dr Craske 22 November 1982 HCDO0000003_111. The Inquiry does not have a copy of the letter of 4 October 1982.
(1036) Letter from Dr Rizza to Dr Craske 8 October 1982 OXUH0001617_001
(1037) Report on The Acquired Immune Deficiency Syndrome (AIDS) 5 November 1982 pp2-3 CBLA0001653_003
(1038) Letter from Dr Craske to Dr Rizza 11 November 1982 HCDO0000392_074, Letter from Dr Craske to Dr Ludlam 11 November 1982 HCDO0000273_079. Dr Craske also sent a copy to Dr Lane on 22 December 1982. Letter from Dr Craske to Dr Lane 22 December 1982 CBLA0001653_001
(1039) Letter from Dr Craske to Dr Rizza 11 November 1982 HCDO0000392_074
(1040) Letter from Dr Lawrence to Dr Craske 22 November 1982 HCDO0000003_111
(1041) Dr Lane’s agenda for the meeting makes no reference to AIDS; nor does the letter written by Dr Cash to Dr Lane two days later. Letter from Dr Rizza to Dr Lane 10 December 1982 CBLA0003258, Letter from Dr Cash to Dr Lane 17 December 1982 CBLA0001650
(1042) Letter from Dr Craske to Dr Lane 22 December 1982 p1 CBLA0001653_001
(1043) According to Professor Lee in her evidence to the Lindsay Tribunal. Professor Christine Lee Lindsay Tribunal Transcript 25 July 2001 p6 LIND0000326
(1044) Letter from I D Marshall of Alpha Therapeutic UK Ltd to Professor Bloom 16 March 1983 p2 CBLA0000060_067
(1045) Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 19 January 1983 pp2-3 HCDO0000558
(1046) Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 19 January 1983 pp3-4 HCDO0000558
(1047) Letter from Dr Craske to Dr Rizza 11 November 1982 HCDO0000392_074, Letter from Dr Craske to Dr Ludlam 11 November 1982 HCDO0000273_079
(1048) Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 19 January 1983 p3 HCDO0000558
(1049) Also in January (on the 21 January) was a meeting of SNBTS directors and Scottish haemophilia directors at which the minutes recorded Dr Cash drawing to members’ attention recent articles in the US, The Observer and The Lancet about “this problem” and circulating a Morbidity and Mortality Weekly Report (“MMWR”) extract. Minutes of SNBTS Directors and Haemophilia Directors meeting 21 January 1983 p7 PRSE0001736
(1050) Desforges AIDS and Preventive Treatment in Hemophilia The New England Journal of Medicine 13 January 1983 p2 PRSE0002410. See the chapter on Knowledge of the Risks of AIDS.
(1051) Those haemophilia clinicians present included Dr David Evans (Manchester), Professor Roger Hardisty (Great Ormond Street), Dr Rizza (Oxford), Dr Hamilton (Newcastle), Dr Ludlam (Edinburgh), Dr Colvin (London), Dr Preston (Sheffield), Dr Mayne (Belfast), Dr Aronstam (Treloar’s), Dr Hill (Birmingham), Dr Prentice (Glasgow), Dr Savidge (St Thomas’), Dr Kernoff (Royal Free), Dr Wensley (Manchester) and Professor Bloom (Cardiff).
(1052) Notes of meeting with Immuno 24 January 1983 pp3-4 PRSE0002647. See the chapter on Knowledge of Risks of AIDS.
(1053) The letter is dated 11 January 1982 but it is clear from the context and other documents that the year has been erroneously recorded and that it was produced on 11 January 1983.
(1054) Letter from Dr Bloom and Dr Rizza to all Haemophilia Centre Directors 11 January 1982 p1 HCDO0000252_042
(1055) This meeting was attended by Professor Bloom, Dr Rizza, Dr Forbes, Dr Kernoff, Dr Ludlam, Dr Matthews, Dr Preston, Dr Savidge, Dr Tuddenham, Dr Wensley, Dr Craske, Dr Aronstam and Dr David Winfield.
(1056) Minutes of Haemophilia Reference Centre Directors meeting 14 January 1983 p5 HCDO0000411
(1057) Professor Tuddenham described the reference centre directors at this meeting as being “on full alert. Anxious, worried and, like everyone else, still highly puzzled as to what could be causing this syndrome, presumed by now to be transmissible by direct contact means and therefore likely to be a virus, and looking for advice on how to move forward, given that it was clear by then that the haemophilia population was at risk.” Professor Edward Tuddenham Transcript 22 October 2020 p89 INQY1000067. That is not, however, the sense that emerges from the minutes, or from the action (or rather lack of action) which resulted from the meeting.
(1058) The Haemostasis Club was run at St Thomas’ by Professor Ingram; it was described by Dr Bevan (St George’s Hospital) as being run “on the British model of genteel academia where enthusiasts for a certain subject would gather and hear presentations and chat and discuss the presentations and generally form a community.” Dr David Bevan Transcript 12 January 2021 p22 INQY1000086
(1059) Professor Luscher was a specialist in paediatric haematology, with a particular interest in haemophilia, at the Children’s Hospital of Michigan.
(1060) Haemostasis Club note on AIDS distribution and defects 8 March 1983 PARA0000013
(1061) Letter from Drs Craske, Rizza and Bloom to Director 22 March 1983 HCDO0000517_001
(1062) The Acquired Immune Deficiency Syndrome (AIDS) 1 March 1983 p4 HCDO0000517_002
(1063) Guidance on UKHCDO Hepatitis Working Party AIDS Survey 1 March 1983 HCDO0000273_078
(1064) Surveillance of Possible Cases of the Acquired Immune Deficiency Syndrome HCDO0000517_004
(1065) Minutes of special meeting of Haemophilia Reference Centre Directors 13 May 1983 HCDO0000003_008
(1066) What happened to Kevin Slater is described in more detail in the Counsel Note on the First Cardiff AIDS Patient January 2021 INQY0000321, Counsel Presentation Transcript 2 February 2021 INQY1000092
(1067) Haemophilia Society The Bulletin No2 December 1983 p5 PRSE0000411
(1068) Completed survey form Surveillance of possible cases of the Acquired Immune Deficiency Syndrome (AIDS) 26 April 1983 p5 WITN3408009
(1069) On 3 May 1983, Professor Bloom provided the Haemophilia Society with a statement concerning AIDS, circulated to Society members on 4 May. He stated that he was “unaware of any proven case”of AIDS among people with haemophilia in the UK. The significance of Professor Bloom’s actions at this time and more generally are considered in the chapters Role of Government: Response to Risk and Haemophilia Society. Letter from Professor Bloom to Reverend Tanner 3 May 1983 p2 CBLA0000060_158
(1070) Communicable Disease Report Weekly Edition CDR 83/18 6 May 1983 p1 PRSE0000353
(1071) Memo from Mary Sibellas to Dr Oliver 6 May 1983 DHSC0002227_021
(1072) The typed text of the draft minutes used the phrase “have up until now restricted their use of National Health Service concentrates to children and mildly affected haemophiliacs” but there is a handwritten amendment which revised it to the phrase used in the final version. Minutes of special meeting of Haemophilia Reference Centre Directors 13 May 1983 p2 HCDO0000003_008
(1073) Minutes of special meeting of Haemophilia Reference Centre Directors 13 May 1983 pp1-3 HCDO0000003_008
(1074) Letter from Dr Galbraith to Dr Ian Field 9 May 1983 CBLA0000043_040. Professor Franklin, when giving oral evidence, considered that Dr Galbraith’s paper should have led to some form of high-level advice to haemophilia clinicians; he was never made aware of it. Professor Ian Franklin Transcript 28 October 2020 p2 INQY1000068
(1075) Dr Walford, who attended the reference centre directors’ meeting, was certainly aware of the letter by 13 May since she wrote a minute to Dr Field about it later that day after the reference centre directors’ meeting. Memo from Dr Walford to Dr Field 13 May 1983 DHSC0002227_047. She may well have seen it by 10 May 1983, as she and Paul Winstanley wrote a note on the imports of blood products on that date. Memo from Paul Winstanley to Dr Walford and Mrs Walden 10 May 1983 DHSC0002227_035. In any event someone within the DHSS should have ensured that the Dr Galbraith letter was shared with the reference centre directors and UKHCDO.
(1076) Letter from Dr Evatt to Professor Bloom 7 March 1983 p1 CBLA0000060_017
(1077) Letter from Professor Bloom and Dr Rizza 24 June 1983 p1 HCDO0000270_004
(1078) Letter from Professor Bloom and Dr Rizza 24 June 1983 p1 HCDO0000270_004
(1079) Letter from Professor Bloom and Dr Rizza 24 June 1983 p1 HCDO0000270_004
(1080) See Letter from Professor Bloom to Dr Walford 17 May 1983 HCDO0000003_122. Having set out these concerns and welcomed Dr Walford’s intention to raise the matter, Professor Bloom said “I hope that it will be possible rapidly to vary the Product Licence for relevant imported products to take account of these recent developments.”
(1081) Dr Brian Colvin Transcript 6 October 2020 p191 INQY1000061
(1082) Letter from Professor Bloom and Dr Rizza 24 June 1983 p1 HCDO0000270_004
(1083) As things turned out, the viral inactivation to which the products had been subjected would not have eliminated hepatitis, but could be effective vis-à-vis AIDS.
(1084) Professor Tuddenham accepted that this fell short of any kind of firm steer or recommendation: it was “just a polite suggestion.” Professor Edward Tuddenham Transcript 22 October 2020 pp96-97 INQY1000067. Professor Ludlam thought it reflected “the sort of people that Professor Bloom and Dr Rizza were … they were both very polite individuals, and I think this was a sort of turn of phrase, and it was a way of encouraging people along … both Dr Rizza and Professor Bloom promoted haemophilia care by encouragement, rather than directive”. Professor Christopher Ludlam Transcript 3 December 2020 pp77-78 INQY1000079
(1085) Council of Europe Committee of Ministers recommendations on Preventing the Possible Transmission of Acquired Immune Deficiency Syndrome (AIDS) from Affected Blood Donors to Patients Receiving Blood or Blood Products 23 June 1983 PRSE0000372
(1086) Professor Christopher Ludlam Transcript 2 December 2020 pp42-44 INQY1000078
(1087) Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 14 September 1983 PRSE0000879
(1088) Minutes of Haemophilia Reference Centre Directors meeting 19 September 1983 p1, pp3-4 HCDO0000413, Appendix B Surveillance of AIDS cases in patients with blood coagulation disorders 10 September 1983 CBLA0001758
(1089) Professor Edward Tuddenham Transcript 22 October 2020 pp102-104 INQY1000067
(1090) Draft minutes of Haemophilia Centre Directors meeting 17 October 1983 p10 PRSE0004440. By early October 1983 the President of the British Society for Haematology had decided that a Working Party should be formed “to investigate the problem of Aids in relation to the practice of Haematology in the Diagnostic Laboratory” and the Working Party, which included Professor Bloom and Dr Rizza, had already met. Minutes of the British Society for Haematology Committee meeting 4 October 1983 p6 BSHA0000005_049. No AIDS-focused working party was formed by UKHCDO until 1985.
(1091) This was the paper that had been discussed by reference centre directors a month earlier. Appendix B Surveillance of AIDS cases in patients with blood coagulation disorders 10 September 1983 CBLA0001758
(1092) Draft minutes of Haemophilia Centre Directors meeting 17 October 1983 p11 PRSE0004440
(1093) Draft minutes of Haemophilia Centre Directors meeting 17 October 1983 p10 PRSE0004440
(1094) At the very least the word “proof” should have been preceded by the word “absolute” and followed by some such words as “but it is certainly likely”. Professor Bloom had by now attended a meeting of the Biological Sub-Committee of the Committee on the Safety of Medicines on 13 July 1983 which had concluded that an infectious aetiology was likely. Minutes of Sub-Committee on Biological Products 13 July 1983 meeting p2 ARCH0001710
(1095) Dr Brian Colvin Transcript 7 October 2020 p20 INQY1000062
(1096) Minutes of Reference Centre Directors meeting 13 February 1984 pp4-5 HCDO0000415, Haemophilia Centre Directors AIDS Investigation 16 January 1984 HCDO0000846. Dr Craske’s report also noted that there had been a study of seven patients with AIDS associated with blood transfusion.
(1097) Dr Craske had reported that the number of cases had increased “exponentially” since 1981. He also explained that there was a “possibility” that transmission by blood and blood products may become “a serious problem”and that in the UK “widespread transmission could occur … unless precautions are taken to exclude donors from the already identified high risk group for AIDS”. Research Proposal for Epidemiological study of AIDS pp1-2 HCDO0000273_075
(1098) Minutes of Reference Centre Directors meeting 13 February 1984 p5 HCDO0000415
(1099) Minutes of Haemophilia Reference Centre Directors meeting 10 September 1984 p8 HCDO0000416
(1100) Minutes of Haemophilia Centre Directors meeting 27 September 1984 p5 PRSE0003659
(1101) Minutes of Haemophilia Centre Directors meeting 27 September 1984 pp12-13 PRSE0003659, Current Situation Regarding AIDS 10 September 1984 CBLA0001884_007
(1102) A note of the meeting was taken by Norman Pettet of BPL. Minutes of Haemophilia Reference Centre Directors meeting 10 December 1984 HCDO0000394_117. A further account of the meeting appears from the internal DHSS minute from Dr Smithies to Dr Abrams 12 December 1984 DHSC0001117
(1103) Minutes of Haemophilia Reference Centre Directors meeting 10 December 1984 p1 HCDO0000394_117. A letter from Dr Lane to the reference centre directors and others (including Drs Gunson, Cash and Tedder) dated 15 November 1984 said the meeting was “to discuss AIDS in relation to the management of haemophiliacs and the implications for treatment with factor VIII concentrates” and that 10 December was the first date suitable for the majority of participants. Letter from Dr Lane to Professor Bloom and others 15 November 1984 p1 BPLL0010494. A reply from Professor Bloom on 19 November 1984 stated that “clearly the matter is of great importance and has certainly come to a head with the Australian experience and with the unfortunate death of the Newcastle patient. I am only glad that we had decided in advance of these events to take some action”. Letter from Professor Bloom to Dr Lane 19 November 1984 p1 BPLL0010493. Dr Rizza’s report for the HIV litigation suggested that the meeting was called “In view of the increasing numbers of reports of AIDS in haemophiliacs in USA and in Europe, the evidence that heating factor concentrate may render them safe and the development of tests for HTLV3 antibody”. Health Authority Defendants Report by Dr Charles Rizza p139 HCDO0000394
(1104) These matters are considered later in this chapter.
(1105) On 23 November 1984 Dr Rizza wrote to Dr Lane suggesting a number of questions which he thought needed to be considered at the meeting, including whether directors should now switch to using only heat-treated Factor 8 concentrates. Letter from Dr Rizza to Dr Lane 23 November 1984 OXUH0000429_002. An agenda was produced by Dr Lane on 4 December 1984. Agenda for Haemophilia Centre Directors meeting 4 December 1984 OXUH0000428
(1106) Minutes of Haemophilia Reference Centre Directors meeting 10 December 1984 p7 HCDO0000394_117
(1107) Minutes of Haemophilia Reference Centre Directors meeting 10 December 1984 p10 HCDO0000394_117
(1108) Minutes of Haemophilia Reference Centre Directors meeting 10 December 1984 p11 HCDO0000394_117
(1109) The final version of the document sent to directors appears in: AIDS Advisory Document 14 December 1984 HCDO0000270_007. A first draft was produced by Professor Bloom. Notes of Reference Centre Directors meeting 14 December 1984 p1 HCDO0000273_053 and sent to Dr Ludlam and Dr Lane in a letter for comment on 18 December 1984 HCDO0000273_052, Letter from Professor Bloom to Dr Lane 18 December 1984 BPLL0010479_001. The handwritten notes on HCDO0000273_053 are Professor Ludlam’s. Professor Christopher Ludlam Transcript 2 December 2020 pp55-56 INQY1000078
(1110) AIDS Advisory Document 14 December 1984 p2 HCDO0000270_007
(1111) AIDS Advisory Document 14 December 1984 pp2-3 HCDO0000270_007
(1112) AIDS Advisory Document 14 December 1984 p3 HCDO0000270_007
(1113) Health Authority Defendants Report by Dr Charles Rizza p139 HCDO0000394
(1114) Minutes of AIDS Group of Haemophilia Centre Directors meeting 11 January 1985 p1 HCDO0000521. Professor Bloom’s report for the HIV litigation stated that the advisory document should have been received by haemophilia centre directors in the first week of January 1985. Haemophilia Litigation Report June 1990 p151 DHSC0001297
(1115) Professor Savidge Statement for Archer Inquiry 17 September 2007 p8 ARCH0002508_002
(1116) See the chapter on Role of Government: Response to Risk.
(1117) Dr Janet Shirley Transcript 14 January 2021 pp7-8 INQY1000088
(1118) By way of example, the 1983 annual return showed four patients with Haemophilia A being treated during the year and one patient with von Willebrand disorder and two patients with Haemophilia B, although there might have been additional patients seen who were not provided with treatment (and thus not included in the return) or were treated with DDAVP (which Dr Shirley indicated would not be included in the return). Annual Returns for Frimley Park Haemophilia Centre 1983 HCDO0001700, Dr Janet Shirley Transcript 14 January 2021 pp20-22 INQY1000088
(1119) Guidance should also have been forthcoming from the DHSS and/or Chief Medical Officer and was not. This is addressed in the chapter on Role of Government: Response to Risk.
(1120) Dr Janet Shirley Transcript 14 January 2021 p16 INQY1000088
(1121) Dr Janet Shirley Transcript 14 January 2021 pp51-52 INQY1000088
(1122) Dr Janet Shirley Transcript 14 January 2021 pp50-51 INQY1000088
(1123) Mrs AJ gave powerful evidence about her husband’s infection and death from HIV. ANON Transcript 11 October 2019 pp68-151 INQY1000040
(1124) Although Dr Shirley thought that he might have moderate haemophilia because his Factor 8 levels tended to be lower than would be expected. Dr Janet Shirley Transcript 14 January 2021 p63 INQY1000088
(1125) Dr Janet Shirley Transcript 14 January 2021 p66 INQY1000088. The failures of clinicians to advise patients about the risks of AIDS is discussed later in this chapter.
(1126) Dr Janet Shirley Transcript 14 January 2021 pp50-51, p68, p77 INQY1000088
(1127) Professor Liakat Parapia, director of Bradford Haemophilia Centre from 1982, Professor Liakat Parapia Transcript 29 October 2020 p62 INQY1000070
(1128) Dr Bevan was based at St George’s Hospital from 1977, initially as a registrar, then as lecturer and honorary senior registrar, before becoming a consultant haematologist in 1984 and taking over as haemophilia centre director from Professor Peter Flute in 1985. Dr David Bevan Transcript 12 January 2021 pp8-12 INQY1000086
(1129) Written Statement of Dr David Bevan 9 November 2020 p23 WITN4106001
(1130) Dr David Bevan Transcript 12 January 2021 pp96-100 INQY1000086
(1131) See the chapter on Knowledge of the Risks of AIDS.
(1132) Dr Stanley Dempsey Transcript 11 February 2022 p59 INQY1000278
(1133) Dr Stanley Dempsey Transcript 11 February 2022 p101 INQY1000278
(1134) Professor Ian Franklin Transcript 27 October 2020 pp163-164 INQY1000068
(1135) Dr Brian Colvin Transcript 6 October 2020 p169 INQY1000061
(1136) Epidemiologic Notes and Reports Pneumocystis carinii Pneumonia among Persons with Hemophilia A Morbidity and Mortality Weekly Report 16 July 1982 PRSE0000523
(1137) Dr Mayne recalls that Dr Craske did make the connection. See footnote 1231.
(1138) Dr Mark Winter Transcript 1 October 2020 pp73-77 INQY1000059
(1139) Dr Mark Winter Transcript 1 October 2020 p76 INQY1000059, Dr Mark Winter Penrose Inquiry Transcript 27 April 2011 p8 PRSE0006016
(1140) Dr Mark Winter Transcript 1 October 2020 p77 INQY1000059
(1141) Dr Mark Winter Transcript 1 October 2020 p80 INQY1000059. Dr Winter also questioned why alarm bells were not ringing at the DHSS: “this alarm bells question, of course, isn’t just for clinicians; it’s for politicians and people who plan the supplies of the concentrates that we were using”. Dr Mark Winter Transcript 1 October 2020 p81 INQY1000059
(1142) Professor Ian Hann Transcript 8 December 2020 pp62-64 INQY1000082, Second International Symposium on Infections in the Immunocompromised Host 1983 p18 PRSE0002220
(1143) Professor Ian Hann Transcript 8 December 2020 p66 INQY1000082
(1144) Draft Personal Record for Peter Jones pp34-35 WITN0841007
(1145) In his written statement to the Inquiry, in response to the question of whether he took any action at this point in time, Dr Jones stated that he “stepped up surveillance and initiated testing as it became available”. Written Statement of Dr Peter Jones 6 June 2021 para 44b WITN0841038
(1146) Dr Jones could not recall discussion about the Heathrow meeting with Dr Hamilton but it is implausible to think that there would not have been communication about such a significant meeting. Written Statement of Dr Peter Jones 6 June 2021 para 44e WITN0841038
(1147) It is right to note that Dr Jones’ letter in The Lancet dated 15 January 1983, having referred to suggestions that “transfusion is immunosuppressive in an as yet unidentified way”, recommended continued careful surveillance of patients with severe haemophilia. It made no mention of a virus as an infective agent. Jones et al Altered Immunology in Haemophilia The Lancet 15 January 1983 DHSC0002351_004
(1148) Letter from Dr Jones to The Press Council 6 May 1983 p1 PJON0000001_100
(1149) Letter from Dr Jones to colleagues 26 May 1983 p1 PJON0000057_001. Dr Jones referred to the “present state of publicity”. He referred to the “British case” (a reference to Kevin Slater), recorded that he was “getting better” and suggested that it was “somewhat suspect” that this was said by Colindale to be a “confirmed” case. He emphasised how few cases there were. He suggested that one would expect to see more cases among the haemophiliac populations had the transmissible agent been introduced via Factor 8 concentrates from the suspect areas. Withdrawing Factor 8 concentrates would mean the cessation of home therapy, prophylaxis and elective surgery, the effects of which would be “obvious”. Referring to the reference centre directors’ meeting in May (at which Dr Hamilton again represented Newcastle), he explained that it was decided that there were no indications for special measures in the UK population of people with haemophilia apart from the need for very small children (under the age of four) to be treated with cryoprecipitate where possible, which did not represent a change in policy. He enclosed a copy of a recent Haemophilia Society statement, which was likely to be the 4 May 1983 statement authored by Professor Bloom. The overall tone and effect of the letter was that there was nothing much to worry about and no different course that needed to be taken.
(1150) Acquired Immunodeficiency in Haemophilia The Lancet 2 April 1983 p1 PRSE0002723
(1151) Written Statement of Dr Peter Jones para 44c WITN0841038. In his evidence to the Lindsay Tribunal Dr Jones was asked about the priority, in terms of safety, of the treatment options from the first half of the 1980s. He stated that “We considered that the safest material available to us locally was our cryoprecipitate … It was less likely to be associated with hepatitis than the pooled products … It was also thought to be safer because of the population from the northern region that it was drawn from.” The next product, in safety terms, was the NHS product, “But we were not given the luxury of being able to use that because there was insufficient material.” Even after 1983 children from around the age of six would be transferred from cryoprecipitate to concentrate for home therapy. Dr Peter Jones Lindsay Tribunal Transcript 11 July 2001 p74, p91 LIND0000312
(1152) Dr Boulton in his evidence to the Penrose Inquiry stated that: “I think at this time, 1982/1983, there was still a reluctance by some haemophilia directors to – and I think this is typified by my dear friend Peter Jones of Newcastle, who was really anxious to get the balance right, as I said earlier, between relieving the immediate problems of haemophilia bleeding against the remote – I put that in inverted commas – risk of some infectious disease later so … I would like to put this in the context of my correspondence and telephone calls with Peter Jones … But at that time, 1982/1983, Peter, who was a paediatrician by training and largely dealing with boys with haemophilia in the Newcastle area, really wanted to test the thinking about the nature of this epidemic, or looming epidemic, that seemed to be focused in America, particularly the west coast, and how relevant that was to England. I think he was reluctant in drawing too much of a conclusion that would reduce significantly the amount of therapy he could give to his patients … although there were legitimate concerns about the safety of those products, Peter and many like him were reluctant to abandon the treatment; in other words, go back ten years or so to the style of treatments usually only cryoprecipitate or small pooled products which would reduce the dosage that children could get and return them to a risk of getting permanent joint damage from their early years”.Dr Frank Boulton Penrose Inquiry Transcript 12 May 2011 pp35-38 PRSE0006024
(1153) Memo from Dr Boulton to Dr McClelland 30 May 1983 PRSE0003709
(1154) Written Statement of Anne Collins HIV/Haemophilia Litigation TYWE0000022
(1155) See the 1983 and 1984 annual returns. Annual Returns for Newcastle Haemophilia Centre 1983 HCDO0000149_002, Annual Returns for Newcastle Haemophilia Centre 1984 HCDO0001842
(1156) In his statement to the Inquiry Dr Jones suggested that one step taken in response to the risk of AIDS was to put off non-urgent surgery. Written Statement of Dr Peter Jones para 45 WITN0841038. That is not consistent with the stance taken by Dr Jones in contemporaneous documents and there is no documentary evidence from Newcastle to demonstrate that surgery was deferred or curtailed.
(1157) See for example Letter from Dr Jones to Barry Dowdeswell 22 November 1984 PJON0000063_001, Letter from Dr Jones to Professor Bloom 29 November 1984 PJON0000069_001
(1158) Letter from Dr Jones to colleagues 30 November 1984 PJON0000067_001
(1159) Letter from Dr Jones to Barry Dowdeswell 27 November 1984 PJON0000061_001, Report of Ad-Hoc Group to Consider the use of Heat-Treated Factor VIII Concentrate TYWE0000048
(1160) Written Statement of John McDougall paras 8-11 WITN2850001, Daily Mail Seven-month hell of man dying from AIDS 20 November 1984 WITN2850002, The Guardian Haemophiliac’s death from Aids after transfusion 19 November 1984 DHSC0002249_029, Melbye et al HTLV-III Seropositivity in European Haemophiliacs Exposed to Factor VIII Concentrate Imported from the USA The Lancet December 1984 PRSE0001630
(1161) The UKHCDO data provided to the Inquiry gives a figure of 88. NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1162) Jones et al AIDS and haemophilia: morbidity and mortality in a well defined population British Medical Journal 14 September 1985 p1 WITN3901009
(1163) The Birmingham Children’s Hospital is considered separately later in this chapter.
(1164) As Professor Franklin accepted in his evidence to the Inquiry: he could recall no new measures taken in response to the risk of AIDS in 1983-1984 other than the maintenance of batch dedication, nor any discussion about the possibility of a complete or partial reversion to cryoprecipitate. Professor Ian Franklin Transcript 28 October 2020 p9 INQY1000069
(1165) Letter from Reverend Tanner to members of the Haemophilia Society 4 May 1983 DHSC0001228
(1166) Draft minutes of Haemophilia Centre Directors meeting 17 October 1983 PRSE0004440. Professor Franklin said he thought the advice from the October 1983 meeting was “taken not by vote but by the sapiential authority of the senior figures and a lack of organised alternative opinion”. Written Statement of Professor Ian Franklin para 101d WITN4032001
(1167) Professor Ian Franklin Transcript 27 October 2020 pp165-166 INQY1000068
(1168) Letter from Professor Franklin to Adrian Whittington 9 April 1991 UBFT0000156
(1169) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 27 June 1983 p2 SHIN0000030
(1170) Professor Ian Franklin Transcript 28 October 2020 pp5-6 INQY1000069
(1171) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 5 December 1983 SHIN0000029, Professor Ian Franklin Transcript 28 October 2020 p7 INQY1000069
(1172) For the treatment of 83 patients with Haemophilia A, the return showed 97,090 units of cryoprecipitate in hospital (none for home treatment), a total of 907,475 units of NHS Factor 8 (for home and hospital) and a total of 1,331,105 units of Factorate (for home and hospital). Annual Returns for Queen Elizabeth Hospital Haemophilia Centre 1983 HCDO0001694
(1173) For the treatment of 90 patients with Haemophilia A, the return showed 86,000 units of cryoprecipitate in hospital (none for home treatment), a total of 1,709,890 units of NHS Factor 8 (for home and hospital) and a total of 1,667,720 of Factorate (for home and hospital). Annual Returns for Queen Elizabeth Hospital Haemophilia Centre 1984 HCDO0001791
(1174) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 14 May 1984 p2 SHIN0000028
(1175) Letter from Dr Franklin to Dr Lane 24 May 1984 BPLL0000853_002. Professor Franklin wrote that “This situation is particularly regrettable given the current interest amongst haemophiliacs in the acquired immune deficiency syndrome. Almost every adult patient at our clinic asks about this syndrome and a significant number of patients have requested to receive only NHS material. Our efforts to reassure patients have included maintaining them on a single product so as to limit the pool of donors to which they are exposed as much as possible. Not only will this sudden and unexpected short-fall in NHS material mean that we will have to change this policy but it will also make epidemiological studies of hepatitis and AIDS meaningless.”
(1176) Professor Ian Franklin Transcript 27 October 2020 pp172-173 INQY1000068
(1177) Minutes of the West Midlands Regional Health Authority meeting 17 December 1984 SHIN0000026_002
(1178) Professor Edward Tuddenham Transcript 22 October 2020 p62 INQY1000067
(1179) Haemophilia Society The Bulletin No2 December 1983 p12 PRSE0000411. The title of the talk was Innovative Alternatives to Human Factor VIII.
(1180) Professor Edward Tuddenham Transcript 22 October 2020 pp66-71 INQY1000067
(1181) Professor Edward Tuddenham Transcript 22 October 2020 pp71-72 INQY1000067, Professor Christine Lee Lindsay Tribunal Transcript 25 July 2001 pp15-17, pp37-38 LIND0000326, Professor Christine Lee Transcript 20 October 2020 p75, pp78-79 INQY1000065, Professor Christine Lee Transcript 21 October 2020 pp30-31 INQY1000066. Annual returns do show a steady increase in the use of DDAVP at the Royal Free Hospital between 1981 and 1985 from two patients in 1981 to 33 patients by 1985. Annual Returns for Royal Free Haemophilia Centre 1981 HCDO0001563, Annual Returns for Royal Free Haemophilia Centre 1982 HCDO0001662, Annual Returns for Royal Free Haemophilia Centre 1983 HCDO0001758, Annual Returns for Royal Free Haemophilia Centre 1984 HCDO0001851, Annual Returns for Royal Free Haemophilia Centre 1985 HCDO0001946
(1182) Minutes of an Association of Haematologists NETR Haemophilia Working Party meeting 13 December 1984 pp2-3 BART0000676, Professor Edward Tuddenham Transcript 22 October 2020 pp74-75 INQY1000067, Professor Lee thought the policy of deferring elective surgery commenced in 1984 but could not say when. Professor Christine Lee Lindsay Tribunal Transcript 25 July 2001 p17 LIND0000326
(1183) Commercial concentrates (Factorate, Koate, Hemofil, Kryobulin) totalled nearly 5 million units (4,924,485); NHS Factor 8 concentrate totalled 1,410,900 units; and cryoprecipitate 101,010 units (in hospital only). Annual Returns for Royal Free Hospital Haemophilia Centre 1983 p1 HCDO0001758
(1184) Annual Returns for Royal Free Hospital Haemophilia Centre 1984 p1 HCDO0001851
(1185) Letter from Dr Kernoff to patients 17 January 1985 BART0000819_002. Professor Tuddenham accepted in his evidence that this was “obviously illogical.”Professor Edward Tuddenham Transcript 22 October 2020 pp77-79 INQY1000067
(1186) Professor Christopher Ludlam Transcript 1 December 2020 pp69-75 INQY1000077, Letter from Dr Boulton to John Watt 1 February 1980 PRSE0000492. Professor Ludlam did not use cryoprecipitate for home treatment principally, he said, because of the risk of allergic reactions. He accepted that cryoprecipitate had transformed the treatment of patients with Haemophilia A and allowed most bleeds in non-inhibitor patients to be treated effectively. Written Statement of Professor Christopher Ludlam para 100 WITN3428001
(1187) Professor Christopher Ludlam Transcript 1 December 2020 pp77-78 INQY1000077, Written Statement of Professor Christopher Ludlam para 93 WITN3428001
(1188) Letter from Dr Boulton to Dr Ludlam 10 May 1982 p1, p3 PRSE0003044. Dr Boulton asked that: maximum use be made of the cryoprecipitate programme; no more patients be put on home therapy; no patients be put on the cold operating lists; some of the heaviest users be counselled to use less.
(1189) Letter from Dr Boulton to Dr Ludlam 20 August 1982 PRSE0003294
(1190) Note of meeting between Dr Boulton and Dr Ludlam 23 August 1982 p3 PRSE0001840
(1191) Lothian Health Board Area Executive Group Agendas and Papers 7 December 1982 p5 LOTH0000216, Professor Christopher Ludlam Transcript 1 December 2020 pp56-61 INQY1000077, Letter from Dr Boulton to Dr Ludlam 29 December 1982 p1 PRSE0003269, Letter from Dr Boulton to John Watt 7 December 1982 PRSE0001487. Dr Ludlam, however, felt that he was not getting the supply of PFC material that had been agreed. Letter from Dr Cash to John Watt 28 October 1982 PRSE0000028, Professor Christopher Ludlam Transcript 1 December 2020 pp91-93 INQY1000077
(1192) Annual Returns for Edinburgh Haemophilia Centre 1981 HCDO0002464
(1193) 528,000 units of cryoprecipitate; 1,574,000 units of NHS concentrate for the treatment of patients with Haemophilia A. The commercial concentrate usage is slight in comparison: 2,300 units of Factorate and 5,000 units of Koate. Annual Returns for Edinburgh Haemophilia Centre 1982 p1 HCDO0002465
(1194) 295,000 units of cryoprecipitate; 1,730,000 units of NHS concentrate; 64,000 units of Factorate and 87,000 units of Koate. Annual Returns for Edinburgh Haemophilia Centre 1983 p1 HCDO0002466
(1195) 91,120 units of cryoprecipitate; 2,471,940 units of NHS concentrate; and 35,850 units of Factorate. Annual Returns for Edinburgh Haemophilia Centre 1984 p1 HCDO0002467
(1196) Professor Christopher Ludlam Transcript 1 December 2020 pp99-100 INQY1000077
(1197) Professor Christopher Ludlam Transcript 1 December 2020 pp102-105 INQY1000077. Professor Ludlam suggested that it might have been because the supply of PFC concentrate improved in 1984; a plausible reason, however, might be that it was a belated response to the discovery that a batch of PFC Factor 8 had infected a number of patients with HIV.
(1198) When discussing, with the Head of Healthcare Policy Division, Deputy Chief Medical Officer, Professor Lowe (and others), assistance for the Scottish Executive investigation about the safety of blood products from Hepatitis C. Minutes of Scottish Haemophilia Centres and Royal Hospital for Sick Children meeting 10 February 2000 pp2-3 ARCH0003312_020. See the chapter on Scotland for this meeting.
(1199) See Professor Christopher Ludlam Transcript 1 December 2020 p116 INQY1000077
(1200) See generally his evidence on the topic of knowledge of the seriousness of NANBH in evidence. Professor Christopher Ludlam Transcript 1 December 2020 pp116-132 INQY1000077
(1201) Professor Christopher Ludlam Transcript 2 December 2020 p3 INQY1000078
(1202) Professor Christopher Ludlam Transcript 2 December 2020 pp8-30 INQY1000078
(1203) Minutes of Haemophilia Centre Directors Hepatitis Working Party meeting 19 January 1983 pp3-4 HCDO0000558
(1204) Professor Christopher Ludlam Transcript 2 December 2020 pp15-16 INQY1000078. Commenting on the San Francisco baby report, he said “I’m not a paediatrician but I do know that there are a range of immune deficient – congenital immune deficiencies that can arise in small children, which makes them very susceptible to opportunistic infections and they would present, I think, in a similar way to a patient who had been infected with an AIDS virus.” As it happens, the treating paediatricians of the San Francisco baby did publish a report in 1983, showing that the only possible alternative cause might be a primary immunodeficiency disorder and setting out why the clinical and laboratory findings suggested that a transmissible infectious agent had resulted in AIDS. Ammann et al Acquired Immunodeficiency in an infant: possible transmission by means of blood products The Lancet 30 April 1983 PRSE0000317.
By way of comment, Koch’s postulates have little to do with the position. They usually apply to establish a causal relationship between a microbe (or known agent) and a disease ie when asking “Does this cause that disease” and both ‘this’ and ‘that’ are known but what is uncertain is the link. They are: (1) the microorganism must be found in diseased but not healthy individuals; (2) the microorganism must be cultured from the diseased individual; (3) inoculation of a healthy individual with the cultured microorganism must cause the disease; and finally (4) the microorganism must be reisolated from the inoculated, diseased individual and matched to the original microorganism.
It is obvious that the disease could not be “found” unless identifiable, which in the case of NANBH was by exclusion; and that without knowing the precise configuration of the supposed virus, it could not be cultured, nor could it be inoculated as a virus into a human being without ethical breaches, nor could it be isolated from the individual reinfected.
(1205) Minutes of SNBTS Directors and Haemophilia Directors meeting 21 January 1983 p3, p7 PRSE0001736
(1206) Notes of meeting with Immuno 24 January 1983 p4 PRSE0002647
(1207) Professor Christopher Ludlam Transcript 2 December 2020 pp19-24 INQY1000078
(1208) Professor Christopher Ludlam Transcript 4 December pp86-87 INQY1000080. He went on to say at the end of his evidence that HIV and the third problem might be linked: this appeared a possibility to him which had been recognised, he thought, by the virologist Professor Tedder in February 1984: that it was a possibility that AIDS could occur in people with haemophilia as a result of the side-effects of impurities in the concentrate so as to predispose them to AIDS: “they were pre-disposed in two ways. One is – well, they would – if they got a lot of Factor VIII in general, not from the implicated batch, but over the years, if they were big users, when they were exposed to the virus, they were more likely to get infected.” Professor Christopher Ludlam Transcript 4 December 2020 p162 INQY1000080
(1209) Though PFC concentrate nonetheless had contributions from those in prison, and Edinburgh with its international festival connections was on its way to becoming a hot spot for AIDS.
(1210) Professor Christopher Ludlam Transcript 2 December 2020 pp29-32 INQY1000078
(1211) Minutes of SNBTS Directors and Haemophilia Directors meeting 2 February 1984 p2 PRSE0001556
(1212) Professor Christopher Ludlam Transcript 2 December 2020 pp31-39 INQY1000078
(1213) Professor Christopher Ludlam Transcript 2 December 2020 pp67-68 INQY1000078
(1214) Professor Richard Tedder Lindsay Tribunal Transcript 9 July 2001 p14 LIND0000310
(1215) Professor Christopher Ludlam Transcript 2 December 2020 pp69-74, p85 INQY1000078. Some 18 months earlier (March 1983) Professor Ludlam had received the first results from an AIDS study of his. He described the effect these had on him as making him surprised, perplexed, and puzzled. It came as a bit of a shock because he had expected no problem with those who had been on Scottish PFC concentrate. Professor Christopher Ludlam Transcript 4 December 2020 pp75-79, pp157-162 INQY1000080. He knew that the abnormalities he found were known to exist in those who were later diagnosed as suffering from AIDS (though in this latter group the order of magnitude was greater). I would be surprised if this was not in the back of his mind when he sent samples to Dr Tedder, and therefore have difficulty in accepting that he had no prior inkling that the patients, whose samples they were, might be suffering. Dr Tedder’s insight is more likely to be right. Moreover, though this was not explored with him in oral evidence, he must have been aware of the British Medical Journal article on 15 October 1983 written by Forbes et al from Glasgow (Immunological abnormalities in haemophilia: are they caused by American factor VIII concentrate?), to the effect that Scottish patients had immunological abnormalities similar to those in their American counterparts. See Professor Gordon Lowe Transcript 10 December 2020 p4 INQY1000084, Written Statement of Professor Charles Forbes to the Penrose Inquiry PRSE0004259,Forbes et al Immunological abnormalities in haemophilia: are they caused by American factor VIII concentrate? British Medical Journal 15 October 1983 PRSE0001121. If he had no prior inkling, as he now thinks, he should have had some. However, I am prepared to accept that he did indeed expect the results to be negative, and was shocked when he found they were not. Whether, given his understanding on the threefold risk to people receiving concentrates, and some degree of abnormality in those patients in his study, this expectation was justified is another question. Nonetheless, the fact of the expectation is a sign of overconfidence in the safety of PFC concentrates.
(1216) Memo from Dr McClelland to Dr Robert Perry 20 November 1984 PRSE0000828
(1217) Letter from Dr Ludlam to Dr I B Sutherland 16 November 1984 LOTH0000097_007
(1218) Note of Haemophilia Directors and SNBTS Representatives meeting 29 November 1984 p1 PRSE0002066
(1219) Note of Haemophilia Directors and SNBTS Representatives meeting 29 November 1984 p2 PRSE0002066
(1220) Professor Christopher Ludlam Transcript 2 December 2020 pp81-96 INQY1000078
(1221) The Penrose Inquiry Final Report, March 2015 pp105-107 PRSE0007002, Professor Christopher Ludlam Transcript 3 December 2020 pp29-35 INQY1000079, Written Statement of Professor Pratima Chowdary p2 WITN3826030
(1222) Annual Returns for Glasgow Haemophilia Centre 1982 p1 HCDO0002494. The data provided to the Inquiry by UKHCDO indicates 25 patients tested positive for HIV at Glasgow Royal Infirmary. NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1223) 45,550 units of cryoprecipitate; 1,914,100 units of NHS. Annual Returns for Glasgow Haemophilia Centre1983 p1 HCDO0002495
(1224) 29,700 cryoprecipitate; 2,206,404 NHS; 5,500 commercial (Hemofil). Annual Returns for Glasgow Haemophilia Centre 1984 p1 HCDO0002496
(1225) Professor Charles Forbes Penrose Inquiry Transcript 28 April 2011 pp103-104 PRSE0006017
(1226) Professor Charles Forbes Penrose Inquiry Transcript 28 April 2011 p110 PRSE0006017
(1227) That was Professor Lowe’s understanding, but he was not directly involved at the time. Professor Gordon Lowe Transcript 9 December 2020 pp49-51 INQY1000083
(1228) Professor Gordon Lowe Transcript 10 December 2020 p4 INQY1000084, Written Statement of Professor Charles Forbes to the Penrose Inquiry PRSE0004259,Forbes et al Immunological abnormalities in haemophilia: are they caused by American factor VIII concentrate? British Medical Journal 15 October 1983 PRSE0001121
(1229) Melbye et al HTLV-III Seropositivity in European Haemophiliacs Exposed to Factor VIII Concentrate Imported from the USA The Lancet 1984 PRSE0001630. Taking both Scottish and Danish patients together, 7% of those who had received only domestic concentrates were seropositive; whereas 40% of those who had received commercial factor concentrate either alone or in combination with local products were. If the UK had been self-sufficient in factor concentrates, and these (statistically significant) results had been replicated generally they suggest that over 80% of the infections which occurred would have been spared.
(1230) Professor Gordon Lowe Transcript 10 December 2020 p20 INQY1000084
(1231) She recalled enquiring as to the relevance to haemophilia and that Dr Craske “reminded us that the individuals cited in the paper were known to maintain their lifestyle by being paid blood donors, as was documented in the World in Action (1975) programme.” Written Statement of Dr Elizabeth Mayne para 30.2 WITN0736009; Immunocompromised Homosexuals The Lancet 12 December 1981 BPLL0002571_098. The New England Journal of Medicine published three articles two days earlier about the same topic; and homosexual males in San Francisco had been the subject of reports of immunocompromise since 5 June 1981 in the MMWR.
(1232) Although not present at the meeting, this was her discussion of it (although she erroneously dated the special meeting as being February 1983) in the report she produced during the HIV Haemophilia Litigation: “At the meeting it was agreed that there was insufficient concrete evidence to warrant changing the type of concentrate used to treat severely affected patients. The decision was taken after prolonged discussion; it was felt that the immense benefits of treatment precluded change.” Expert Witness Report of Dr Elizabeth Mayne May 1990 p34 CBLA0000072_024
(1233) Letter from Dr Mayne to the Editor of The Lancet 4 August 1993 LOTH0000080_007
(1234) Annual Returns for Belfast Haemophilia Centre 1982 p1 HCDO0001596, 1983 p1 HCDO0001692, 1984 p1 HCDO0001789
(1235) Northern Ireland Haemophilia Reference Centre Factor VIII Usage 1 August 1985 p2 BHCT0000503
(1236) Northern Ireland Haemophilia Reference Centre Factor VIII Usage 1 August 1985 p1 BHCT0000503
(1237) Expert Witness Report of Dr Elizabeth Mayne May 1990 p40 CBLA0000072_024
(1238) Written Statement of Dr Elizabeth Mayne para 36.1 WITN0736009
(1239) Written Statement of Dr Elizabeth Mayne para 58.1 WITN0736009, NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1240) Notes for Scottish Health Service Haemophilia Centre – Transfusion Service Directors meeting January 1983 p7, p15 PRSE0001991
(1241) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 19 January 1983 pp3-4 HCDO0000558
(1242) Notes of meeting with Immuno 24 January 1983 PRSE0002647. And four days later a patient being reviewed in his clinic was described as follows: “Being a well-read man, he is somewhat concerned about the possibility of acquiring the acquired immunodeficiency syndrome, although of course there is no grounds for suspecting the diagnosis in him.” Letter from Dr Malcolm Liddell to ANON 28 January 1983 p2 WITN0047004
(1243) Letter from Professor Bloom to David Watters 20 January 1983 HCDO0000003_066
(1244) Letter from Dr Evatt to Professor Bloom 7 March 1983 p1 BPLL0001351_021
(1245) Letter from Mr Ian David Marshall to Professor Bloom 16 March 1983 CBLA0000060_067
(1246) See the chapter on The Haemophilia Society.
(1247) Haemophilia Treatment Policy Guidelines 18 May 1983 WITN4029002
(1248) 92,740 units of cryoprecipitate, compared to 178,640 in 1982 p1 HCDO0001606. In relation to concentrates, this represented an increase in the use of NHS concentrates since 1982 and a roughly equivalent decrease in the use of commercial concentrates, although the latter were still the product most in use. Roughly half of the concentrates used were for home treatment. These figures do not include the usage of FEIBA and NHS Factor 9 used in the treatment of people with inhibitors. The total number of people with Haemophilia A treated during the year was 64. Annual Returns for Cardiff Haemophilia Centre 1983 p1 HCDO0001702
(1249) 123,900 units of cryoprecipitate. The total number of patients with Haemophilia A treated in 1984 was 77. The figures do not include usage of FEIBA and NHS Factor 9 for inhibitors. Annual Returns for Cardiff Haemophilia Centre 1984 p1 HCDO0001798
(1250) The main 1983 return made no reference to DDAVP. Annual Returns for Cardiff Haemophilia Centre 1983 p1 HCDO0001702. The 1983 individual patient data records the use of DDAVP for a single person with Haemophilia A and three people with von Willebrand disorder.
(1251) Letter from Professor Bloom to Dr Boulton 23 May 1983 PRSE0003701
(1252) This child, with inhibitors, was also treated with FEIBA and with Factor 9. Annual Returns for Cardiff Haemophilia Centre 1984 p8 HCDO0001798
(1253) Annual Returns for Cardiff Haemophilia Centre 1984 pp7-13 HCDO0001798
(1254) Draft minutes of Haemophilia Centre Directors meeting 17 October 1983 p10 PRSE0004440
(1255) NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1256) Letter from Dr Rizza to Dr Craske 8 October 1982 OXUH0001617_001
(1257) Letter from Dr Rizza to Dr Rosemary Rue 11 May 1983 OXUH0002245_007
(1258) The precise figure is 4,655,053. Profilate, Factorate, Koate and Hemofil were all used. Annual Returns for Oxford Haemophilia Centre 1983 p1 HCDO0001753
(1259) And inconsistent with the suggestion in Dr Rizza’s letter to the regional medical officer that the system of treatment was such that large numbers of patients were treated only with NHS or only with commercial concentrates.
(1260) Annual Returns for Oxford Haemophilia Centre 1984 p1 HCDO0001847
(1261) Annual Returns for Oxford Haemophilia Centre 1984 pp6-31 HCDO0001847
(1262) Letter from Dr Rizza to Mr C R Jones 13 December 1984 OXUH0003761_020
(1263) Written Statement of Professor Pratima Chowdary p2 WITN3826030
(1264) Professor Liakat Parapia Transcript 29 October 2020 pp5-6 INQY1000070. The previous director, Professor Robert Turner, became unexpectedly ill, which led to Dr Parapia taking over.
(1265) Professor Liakat Parapia Transcript 29 October 2020 pp30-35 INQY1000070
(1266) Professor Liakat Parapia Transcript 29 October 2020 p38 INQY1000070. The 1982 return showed no cryoprecipitate being used at all, only concentrates (NHS, Factorate and Kryobulin). Annual Returns for Bradford Haemophilia Centre 1982 p1 PARA0000003
(1267) Again, no cryoprecipitate was used for the treatment of patients with Haemophilia A; all treatment was with concentrates (NHS, Factorate and Kryobulin). Annual Returns for Bradford Haemophilia Centre 1983 HCDO0000228_002
(1268) Professor Liakat Parapia Transcript 29 October 2020 pp43-44 INQY1000070
(1269) Professor Liakat Parapia Transcript 29 October 2020 pp57-60 INQY1000070
(1270) Professor Liakat Parapia Transcript 29 October 2020 p62 INQY1000070
(1271) Desforges AIDS and Preventive Treatment in Hemophilia The New England Journal of Medicine 13 January 1983 PRSE0002410
(1272) Professor Liakat Parapia Transcript 29 October 2020 p87 INQY1000070
(1273) Professor Liakat Parapia Transcript 29 October 2020 p110 INQY1000070. A meeting of the Yorkshire haemophilia centre directors took place on 7 June 1983 to discuss the supply position with regard to Factor 8 concentrates. A record of the meeting prepared by Dr Swinburne referred to NHS supply amounting to about one third of the total and continued “There would be no objection to using more than are commercial supplies, although from the AIDS point of view there might be an advantage in limiting the batches of materials to which any patient was exposed. This might be done by ear-marking certain batches for particular hospitals. Further discussion with the B.T.S. would be needed to see if this was possible.” On the issue of cryoprecipitate, the only discussion was to the effect that “The Directors were concerned at the volume of the current cryoprecipitate, which includes so much plasma that the risk of reaction is very great.” It was noted that “Heat treated material may be available soon.” Note of Yorkshire Haemophilia Centre Directors meeting 7 June 1983 PARA0000048
(1274) Minutes of Blood Transfusion Service meeting 4 December 1984 PARA0000008
(1275) Letter from Dr Swinburne to Dr Tovey 7 February 1985 PARA0000018
(1276) Professor Liakat Parapia Transcript 29 October 2020 pp131-132 INQY1000070
(1277) NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1278) The 1976 annual return showed predominantly cryoprecipitate use, with some NHS concentrate HCDO0000024_004. A comparison with 1983’s annual return shows a significant shift to commercial concentrate (Armour) for both hospital and home treatment, with very little cryoprecipitate and some NHS concentrate. Survey of patients treated at Haemoophilia Centres in the UK 1983 HCDO0000143_003
(1279) Dr David Bevan Transcript 12 January 2021 pp28-29 INQY1000086
(1280) Dr David Bevan Transcript 12 January 2021 p31 INQY1000086
(1281) Dr David Bevan Transcript 12 January 2021 pp69-70 INQY1000086
(1282) Dr David Bevan Transcript 12 January 2021 p66 INQY1000086
(1283) Dr David Bevan Transcript 12 January 2021 p67 INQY1000086
(1284) Dr Bevan could not avoid the suspicion that there were some non-heat-treated batches used up to the middle of 1985 but did not think that there was unheated product used from July onwards. Dr David Bevan Transcript 12 January 2021 pp72-73 INQY1000086
(1285) Dr David Bevan Transcript 12 January 2021 pp75-77 INQY1000086. The UKHCDO data provided to the Inquiry suggested that 20 patients were infected. NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1286) Dr Mark Winter Transcript 1 October 2020 p8 INQY1000059
(1287) Dr Mark Winter Transcript 1 October 2020 p9 INQY1000059
(1288) Dr Mark Winter Transcript 1 October 2020 p10 INQY1000059
(1289) Dr Mark Winter Transcript 1 October 2020 p17 INQY1000059
(1290) Dr Mark Winter Transcript 1 October 2020 pp18-19 INQY1000059
(1291) Dr Mark Winter Transcript 1 October 2020 p20 INQY1000059
(1292) Dr Mark Winter Transcript 1 October 2020 pp24-26 INQY1000059
(1293) Dr Mark Winter Transcript 1 October 2020 p82 INQY1000059. It is not possible to determine from the annual returns the impact of this message. The annual return for Guy’s for 1982 shows that 229,675 units of concentrate were used in the treatment of 21 patients with Haemophilia A. Annual Returns for Guy’s Hospital 1982 p1 HCDO0001623. This comprised NHS concentrate and two commercial concentrates: Factorate and Koate. The annual return for 1983 shows that 160,575 units of concentrate were used in the treatment of 17 patients with Haemophilia A: a greater proportion of that concentrate was NHS compared to the previous year, but Factorate was still in use (although not Koate). Annual Returns for Guy’s Hospital 1983 p1 HCDO0000146_003. In both years cryoprecipitate was only used for the treatment of patients with von Willebrand disorder. In 1984, cryoprecipitate was used for the treatment of Haemophilia A to an extent, but most treatment was with NHS concentrate (Factorate and Koate were both used as well, although in smaller quantities than NHS). Annual Returns for Guy’s Hospital 1984 p1 HCDO0001814
(1294) Dr Mark Winter Transcript 1 October 2020 pp90-92 INQY1000059
(1295) He had not been director of a centre previously.
(1296) The director had been Dr Harold Sterndale. Dr Mark Winter Transcript 1 October 2020 p116 INQY1000059
(1297) Dr Mark Winter Transcript 1 October 2020 pp120-121 INQY1000059
(1298) Dr Mark Winter Transcript 1 October 2020 pp134-140 INQY1000059
(1299) Dr Mark Winter Transcript 2 October 2020 p9 INQY1000060
(1300) Dr Mark Winter Transcript 1 October 2020 p140 INQY1000059
(1301) Dr Mark Winter Transcript 2 October 2020 p154 INQY1000060
(1302) Dr Mark Winter Transcript 1 October 2020 pp112-114 INQY1000059
(1303) Dr Mark Winter Transcript 1 October 2020 pp168-170 INQY1000059
(1304) Notes of meeting with Immuno 24 January 1983 PRSE0002647
(1305) Dr Brian Colvin Transcript 6 October 2020 pp164-166 INQY1000061
(1306) Dr Brian Colvin Transcript 6 October 2020 p169 INQY1000061
(1307) Dr Brian Colvin Transcript 6 October 2020 p174 INQY1000061
(1308) Minutes of Association of Haematologists NETR Working Party in Haemophilia meeting 9 February 1983 BART0000679. Attendees at the meeting included, in addition to Dr Colvin, Dr Kernoff (Royal Free), Dr Baugh (director of the Chelmsford Haemophilia Centre), Dr Samuel Machin (Middlesex Hospital) and Dr Jean Harrison (director of the RTC at Brentwood).
(1309) Dr Brian Colvin Transcript 6 October 2020 pp181-182 INQY1000061. The 1983 annual return for The London shows that Dr Colvin did use substantial quantities of NHS Factor 8 (1,100,392 units) as well as 148,540 units of cryoprecipitate and 388,654 units of commercial concentrate (Koate, Factorate, Hemofil and Kryobulin) for the treatment of 78 patients with Haemophilia A. Annual Returns for The London Hospital 1983 HCDO0000177_003. A broadly similar approach appears from the 1982 return. Annual Returns for The London Hospital 1982 p1 HCDO0001642. Dr Colvin observed that “inevitably”, because of the shortfall in NHS Factor 8, “we were using a significant quantity of commercial concentrate in the hospital.” Dr Brian Colvin Transcript 6 October 2020 pp180-182 INQY1000061. A reduction in the purchase of commercial concentrate in 1983 was due to an increase in supply of NHS material. Letter from Dr Colvin to Miss A Paterson 23 March 1984 BART0000517. Dr Colvin also pointed to a study of patients with mild Haemophilia A or von Willebrand disorder who were treated with cryoprecipitate between October 1982 and July 1984 as an indication that he was trying to avoid the use of concentrates due to the risks of viral infection. Colvin et al A Prospective Study of Cryoprecipitate Administration: Absence of Evidence of Virus Infection Clinical & Laboratory Haematology 1 March 1987PRSE0003838; Dr Brian Colvin Transcript 6 October 2020 pp183-185 INQY1000061. A publication in 1987 shows he did offer cryoprecipitate (which he described as “widely used as the safest form of treatment for patients with mild coagulation defects who were unsuitable for DDAVP injection”) to six patients treated between October 1982 and July 1984 in an attempt to establish the risk of transfusion hepatitis, none of whom had ever received concentrates. None was infected either with hepatitis or with HIV, despite one having been treated for a severe knee bleed, and the others having elective surgery, which in many centres would have been “covered” by the use of concentrates. Colvin et al A prospective study of cryoprecipitate administration: absence of evidence of virus infection Clinical and Laboratory Haematology 1987 PRSE0003838. A publication in 1986 records that he had arranged treatment of three patients (who had not previously had concentrate) who needed treatment for which factor concentrate would normally then be used, with 8CRV, an NHS product from Oxford made from selected donors and heat treated. This was in 1984 before heat treated product became generally available. Colvin et al Heat-treated NHS factor VIII concentrate in the United Kingdom – a preliminary study Clinical and Laboratory Haematology 1986 PRSE0000608. Though other studies at that time showed that all patients receiving concentrate (whether NHS or commercial) would be likely to be infected with hepatitis, his patients were not. This was an early use of heat treated NHS material with an eye on patient safety.
(1310) Report on Haemophilia Services in the NETR: 1983 p4, p9 BART0002284, Dr Brian Colvin Transcript 7 October 2020 pp13-16 INQY1000062
(1311) Letter from Dr Colvin to David Watters 22 February 1984 p2 BART0002310. Dr Colvin did not accept that he was suggesting that there was no increased risk from commercial material as at February 1984. Rather he was not recommending “that we don’t buy commercial concentrate at all.” Dr Brian Colvin Transcript 7 October 2020 pp28-30 INQY1000062
(1312) Minutes of Association of Haematologists NETR Haemophilia Working Party meeting 9 May 1984 p2 BART0000677
(1313) Dr Brian Colvin Transcript 7 October 2020 pp30-32 INQY1000062
(1314) Minutes of Association of Haematologists NETR Haemophilia Working Party meeting 13 December 1984 pp2-3 BART0000676. The deferral of elective surgery was also agreed. The reference to small pool concentrate was to “tiny amounts of an NHS small pool heat-treated concentrate available at around that time.” Dr Brian Colvin Transcript 7 October 2020 p43 INQY1000062. The meeting decided that the associate centres in the NETR should exchange their emergency stocks of commercial concentrates for heat-treated products, via the Royal Free, but did not address what should be done with stocks of unheated commercial concentrates which patients on home treatment might hold at home. Dr Colvin could not recall what if any process was put in place at The London to try to get back any stocks of unheated commercial concentrates. Dr Brian Colvin Transcript 7 October 2020 p46 INQY1000062
(1315) Written Statement of Dr Brian Colvin para 63 WITN3343007. There were three other children who had been to Treloar’s and treated there: Dr Colvin observed that he did not have any influence on the treatment they received. Dr Brian Colvin Transcript 7 October 2020 pp79-80 INQY1000062. The UKHCDO data provided to the Inquiry gave a figure of 34 patients infected with HIV and not resident abroad. Written Statement of Professor Pratima Chowdary p2 WITN3826030
(1316) Based on experience in Vellore, India reported by Dr Alok Srivastava. Dr Brian Colvin Transcript 6 October 2020 p97 INQY1000061; Dr Brian Colvin Transcript 7 October 2020 pp9-10 INQY1000062
(1317) He was speaking generally about the UK, rather than the London Hospital in particular. Dr Brian Colvin Transcript 6 October 2020 pp146-147 INQY1000061
(1318) Informed by his views of Dr Srivastava’s experience in Vellore and summarised by his saying “you might have got away with it.” Dr Brian Colvin Transcript 7 October 2020 pp7-11 INQY1000062. As part of this, he said: “if you had abandoned all surgery except for the most life-saving and if you had abandoned the home treatment programme and if you had cut back on dosage … the consequences of the temporary withdrawal of all blood products in the way that Dr Galbraith perfectly understandably recommended was a probable, I think, significant reduction in anti-HIV positivity and a significant, and probably very significant, reduction in the quality of haemophilia care.”
(1319) No cryoprecipitate was used; 404,955 units of NHS Factor 8 were used; 2,357,275 units of commercial (Factorate) were used. Annual Returns for Leeds Haemophilia Centre 1982 p1 HCDO0001635
(1320) NHS Factor 8 increased to 1,449,960; 1,686,689 units of commercial concentrates were recorded. Annual Returns for Leeds Haemophilia Centre 1983 p1 HCDO0001734. In 1984, 1,497,585 units of NHS Factor 8 and 1,715,894 units of commercial concentrates were used. Annual Returns for Leeds Haemophilia Centre 1984 p1 HCDO0001826. No cryoprecipitate usage was recorded in 1983 or 1984 for the treatment of Haemophilia A.
(1321) Annual Returns for Leeds Haemophilia Centre 1985 p1 HCDO0001920
(1322) Minutes of Regional Haematologist Group meeting 16 November 1983 NHBT0100235_002
(1323) The precise figures on the 1981 return are faint but do show commercial concentrates as the predominant treatment. Annual Returns for Liverpool Haemophilia Centre 1981 p1 HCDO0001542
(1324) The use of cryoprecipitate dropped from around 330,000 in 1981 to 29,260 in 1982. NHS Factor 8 use in 1982 was 1,156,340 units, compared to 2,704,134 units of commercial concentrates. Annual Returns for Liverpool Haemophilia Centre 1982 p1 HCDO0001640
(1325) Cryoprecipitate use dropped still further in 1983 to 17,780 and to a tiny 6,090 units in 1984. The amount of NHS Factor 8 in 1983 was 1,945,060, with commercial concentrates at 1,976,520; in 1984 NHS Factor 8 usage increased to 2,302,140 and commercial concentrates fell slightly to 1,788,280. However, there may be some doubt about these figures, as the amounts given for some concentrates are identical as between hospital and home treatment use, which seems unlikely (for example, the 1984 return records 150,340 units of Koate in hospital and exactly the same figure for home treatment with Koate). Annual Returns for Liverpool Haemophilia Centre 1983 p2 HCDO0000145_003; Annual Returns for Liverpool Haemophilia Centre 1984 p1 HCDO0001832
(1326) Written Statement of Dr Bernard McVerry para 20.3 WITN3502007
(1327) Written Statement of Dr Bernard McVerry para 24.1 WITN3502007
(1328) Mersey Regional Haemophilia Centre Response to Questionnaire: HIV Litigation Main Statement of Claim p8, p10 NHBT0085908
(1329) HIV Medical Negligence Cases Status Report 5 September 1991 p4 DHSC0045721_051
(1330) Written Statement of Dr Bernard McVerry paras 55.1, 56.2, 63.1 WITN3502007 and see footnotes 1323-1325.
(1331) 219 bags of cryoprecipitate were used. The return has a handwritten figure of 18,330 in the plasma column, but it may be that that was a calculation of the number of units of cryoprecipitate used, rather than indicating the use of plasma. 419,213 units of NHS Factor 8 were used and 430,863 units of commercial concentrates (Factorate, Hemofil and Kryobulin). Annual Returns for Sheffield Haemophilia Centre 1981 p1 HCDO0001567
(1332) 5,250 units of cryoprecipitate, 413,220 units of NHS concentrate and 550,790 units of commercial concentrates (Factorate, Hemofil, Kryobulin). Annual Returns for Sheffield Haemophilia Centre 1982 p1 HCDO0001665
(1333) 409,165 units of NHS Factor 8 concentrate were used and 475,486 units of commercial (Factorate, Hemofil, Kryobulin). A small amount (3,080 units) of cryoprecipitate was used. Annual Returns for Sheffield Haemophilia Centre 1983 p1 HCDO0001761
(1334) 122 bags of cryoprecipitate. 626,075 units of NHS Factor 8 were recorded and 372,240 units of commercial (Factorate, Kryobulin). Annual Returns for Sheffield Haemophilia Centre 1984 p1 HCDO0001853
(1335) Sheffield participated in a formal trial of an Armour heat-treated concentrate, beginning in April 1984, but the two patients became ill with hepatitis. Dr Preston’s recollection was that they withdrew from that study and moved to a study with colleagues in other centres, using an Alpha product. Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 pp6-7 LIND0000323. Dr Preston published an article in The Lancet about the two patients treated with Armour heat-treated and a third treated with BPL’s small pool heat-treated product. Non-A, Non-B Hepatitis and Heat-treated Factor VIII Concentrates WITN3289189. Dr Winter also recalled that Sheffield was one of four centres that started to use heat-treated products at the end of May 1984. Written Statement of Dr Mark Winter para 35.9 WITN3437002
(1336) Annual Returns for Sheffield Haemophilia Centre 1985 HCDO0001949. Professor Preston told the Lindsay Tribunal that at the beginning of 1985 he moved over completely to heat-treated products, discontinuing the use of non heat-treated NHS products in February/March 1985. Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 p8, p21 LIND0000323
(1337) Professor Francis Eric Preston Transcript 2 November 2020 pp73-75 INQY1000071
(1338) Professor Francis Eric Preston Transcript 2 November 2020 p74 INQY1000071
(1339) Professor Francis Eric Preston Transcript 2 November 2020 p76 INQY1000071; Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 p10 LIND0000323
(1340) NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1341) Professor Eric Preston Lindsay Tribunal Transcript 23 July 2001 p24 LIND0000323. Professor Makris’ evidence was that a total of 38 individuals were infected (28 with severe Haemophilia A, 1 with moderate Haemophilia A, 5 with mild Haemophilia A, 4 with Haemophilia B). However, he also indicated that eight of these individuals were infected prior to their transfer to the adult service. It is not clear why this figure differs from the UKHCDO data. Written Statement of Professor Michael Makris para 43.1 WITN4033001
(1342) Dr Vivian Mitchell Transcript 18 November 2020 p8 INQY1000075
(1343) Dr Vivian Mitchell Transcript 18 November 2020 p15 INQY1000075
(1344) Dr Vivian Mitchell Transcript 18 November 2020 p16 INQY1000075
(1345) Dr Vivian Mitchell Transcript 18 November 2020 pp17-18 INQY1000075
(1346) Dr Vivian Mitchell Transcript 18 November 2020 p19 INQY1000075. Dr Mitchell acknowledged that reactions could occur but did not recall it being a major problem. He also recalled that Leicester was fortunate in being in the middle of the county so nobody was further away than 20 miles and most did not have to travel far to get to the Centre – and so maintaining patients with mild or moderate haemophilia and children under ten on cryoprecipitate at the hospital was not difficult. Dr Vivian Mitchell Transcript 18 November 2020 pp19-20 INQY1000075
(1347) Dr Vivian Mitchell Transcript 18 November 2020 p20 INQY1000075
(1348) Dr Vivian Mitchell Transcript 18 November 2020 p21 INQY1000075
(1349) Dr Vivian Mitchell Transcript 18 November 2020 p27 INQY1000075
(1350) Dr Vivian Mitchell Transcript 18 November 2020 pp22-24 INQY1000075
(1351) Even with Dr Mitchell’s approach, some patients were infected with Hepatitis C and HIV. To prevent such infections, national measures (such as self-sufficiency, earlier achievement of viral inactivation, better donor screening and selection) would have been required. These are considered elsewhere in this Report.
(1352) Letter from Dr Mitchell to British Medical Journal 20 July 1985 PRSE0001555
(1353) Transcript 18 November 2020 pp50-51 INQY1000075. The UKHCDO data supplied to the Inquiry gives a figure of ten patients who tested positive for HIV at Leicester. NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1354) Wellcome Witnesses to Twentieth Century Medicine Haemophilia: Recent History of Clinical Management 1999 p86 RLIT0000022, Professor Edward Tuddenham Transcript 22 October 2020 pp143-144 INQY1000067
(1355) It is also relevant to recognise that, except for those in the largest centres, haemophilia clinicians spent little more than one session out of ten per week (half a day), if that, on haemophilia care, a factor which reinforced the need for clear guidance, whether from the reference centre directors or from Government or both, which prioritised patient safety and the minimisation of risk.
(1356) According to an article by Dr Rosemary Biggs and others, the condition was to be called “Christmas disease” after the name of the first patient whose condition was examined in detail. Christmas Disease: A Condition Previously Mistaken for Haemophilia British Medical Journal 27 December 1952 HSOC0022584
(1357) Expert Report to the Infected Blood Inquiry: Bleeding Disorders and Blood Disorders January 2020 p19 EXPG0000002
(1358) According to the Expert Bleeding Disorders and Blood Disorders Report, “the National Haemophilia Database has 1,836 reported cases of haemophilia B of whom 360 are severe, compared to 8,410 cases of haemophilia A of whom 2,060 are severe.” Expert Report to the Infected Blood Inquiry: Bleeding Disorders and Blood Disorders January 2020 p19 EXPG0000002
(1359) There was a return to its use recommended by clinicians for children, patients with mild Haemophilia B, and newly treated patients after the AIDS epidemic began. See below. It was thus not entirely superseded, though the volumes with which it had to be infused to have any significant effect on clotting were often challenging.
(1360) DDAVP enables the Factor 8 in the bloodstream to produce between two and four times the clotting efficacy; it has no similar effect for Factor 9.
(1361) Several intermediate Factor 9 products were subsequently licensed in the UK during the mid to late 1970s, including Baxter’s/Hyland’s ‘Proplex Factor IX Complex’ (licence PL 0116/0049 granted on 15 October 1976) MHRA0033316_007, MHRA0033317_054, MHRA0033317_067; BPL/PFL’s ‘Dried Human Factor IX Fraction’ (licence PL 0134/0009 granted on 3 February 1977) CBLA0000569; and PFC’s ‘Human Factor IX Concentrate DEFIX’ (licence PL 3473/0008 granted on 16 July 1979)SBTS0004085_029
(1362) Health Authority Defendants Report by Dr Rizza p34 HCDO0000394
(1363) Minutes of Haemophilia Centre Directors meeting 5 April 1971 p11 HCDO0001014
(1364) A witness to the Inquiry who received Factor 9 treatment in the mid 1970s recalls that at the time “There was a massive push for people to go on to home treatment.” Written Statement of Peter Brierly para 5 WITN1105001
(1365) Biggs Haemophilia Treatment in the United Kingdom from 1969 to 1974 British Journal of Haematology 1977 PRSE0004645
(1366) Minutes of Haemophilia Centre Directors meeting 13 January 1977 p22 PRSE0002268
(1367) The 1976 annual returns recorded that 396 patients were treated with a total of 5,561,834 Factor 9 units in the UK. Of those, 17,680 units came from FFP; 11,500 units of commercial concentrates were used; and the remaining 5,532,654 units were NHS concentrates. The average per patient was 18,790 units. 60 patients were on home treatment. Dr Rizza and Rosemary Spooner Annual Returns from Haemophilia Centres 18 October 1978 pp4-5 CBLA0000863
(1368) Minutes of Haemophilia Centre Directors meeting 24 October 1977 p15 PRSE0001002
(1369) In 1978, 337 patients (including 7 carriers of Haemophilia B) were treated with 6,840,000 units of Factor 9, comprising 31,000 units of FFP, 11,000 units of commercial concentrates, and 6,799,000 units of NHS Factor 9. The average amount used per patient was 21,000 units. This was an increase from 1976, but said to be a decrease from 1977 when the annual figure was 23,000. Annual Returns for 1978 pp1-2, p4 OXUH0000212_002. These figures were based on the returns from 103 centres; some centres had not yet sent their returns. A graph shows the steep rise in Factor 9 concentrate usage since 1969. Annual Returns for 1978 p13 OXUH0000212_002. In 1979, 342 patients (including 11 carriers) were treated with 6,933,500 units of Factor 9. Only 1,500 units were FFP, used exclusively for the treatment of Haemophilia B carriers. No commercial concentrates were recorded, and the vast majority of the treatment therefore was with NHS Factor 9 concentrates. The average amount used per Haemophilia B patient was 20,273 units. Annual Returns for 1979 5 September 1980 p3 CBLA0001160. The table also shows usage of Factor 9 in the treatment of Haemophilia A patients with Factor 8 antibodies: those figures have not been included in the text above. The annual returns referred to in this and the following footnotes were based on the returns that had been submitted to Oxford; there may have been some outstanding returns and the figures given are therefore not necessarily comprehensive.
(1370) Minutes of Haemophilia Centre Directors meeting 13 November 1978 p18 HSOC0010549
(1371) Peter Jones Home Treatment Working Party 15 October 1979 p1 LOTH0000012_135
(1372) Annual Returns for 1980 p3, p8 BART0002484. The table also shows usage of Factor 9 in the treatment of Haemophilia A patients with Factor 8 antibodies: those figures have not been included in the text above. A graph shows the increase in treatment since 1969. Annual Returns for 1980 p14 BART0002484
(1373) Annual Returns for 1981 p3, p8 CBLA0001612. The table also shows usage of Factor 9 in the treatment of Haemophilia A patients with Factor 8 antibodies: those figures have not been included in the text above.
(1374) Annual Returns for 1982 p9, p11 CBLA0001757. The table also shows usage of Factor 9 in the treatment of Haemophilia A patients with Factor 8 antibodies: those figures have not been included in the text above.
(1375) Annual Returns for 1983 p11, p13 CBLA0001884_002. The table also shows usage of Factor 9 in the treatment of Haemophilia A patients with Factor 8 antibodies: those figures have not been included in the text above.
(1376) Annual Returns for 1984 p10, p12 CBLA0002279_002. The table also shows usage of Factor 9 in the treatment of Haemophilia A patients with Factor 8 antibodies: those figures have not been included in the text above.
(1377) Annual Returns for 1985 p5, p10, p12 BART0002267. The table also shows usage of Factor 9 in the treatment of Haemophilia A patients with Factor 8 antibodies: those figures have not been included in the text above.
(1378) Notes for Scottish Health Service Haemophilia Centre Transfusion Service Directors meeting January 1981 p11 CBLA0001252
(1379) Notes for Scottish Health Service Haemophilia Centre Transfusion Service Directors meeting January 1981 p11 CBLA0001252
(1380) Notes for Scottish Health Service Haemophilia Centre Transfusion Service Directors meeting January 1981 p12 CBLA0001252
(1381) Note of Haemophilia and Blood Transfusion Working Group meeting 4 March 1981 p3 SBTS0000382_008
(1382) Minutes of Scottish National Blood Transfusion Service Directors and Haemophilia Directors meeting 21 January 1983 p5 PRSE0001736
(1383) Involving Dr Craske, Dr Rizza, Rosemary Spooner, Dr Ghosh, Dr Joan Trowell, Dr Ludlam and Dr Lane. Second Annual Report on Project Number J/S240/78/7: Studies of the Epidemiology and Chronic Sequelae of Factor VIII and IX Associated Hepatitis in the United Kingdom November 1980 p2 HCDO0000135_021
(1384) The upper range of normal for this study was taken to be 35 IU/L. Second Annual Report on Project Number J/S240/78/7: Studies of the Epidemiology and Chronic Sequelae of Factor VIII and IX Associated Hepatitis in the United Kingdom November 1980 p39 HCDO0000135_021
(1385) Self Sufficiency – Pool Sizes at the Blood Product Laboratory March 2022 p21 INQY0000345
(1386) Letter from Dr Rainsford to Dr Judith Chessells 8 May 1975 TREL0000169_033
(1387) Manuscript note by Dr Bidwell: Limitations on number of plasma donations in a bath of concentrate 4 March 1976 CBLA0000341, Memo from Dr Maycock to Dr Bidwell 19 March 1976 CBLA0000346. See also Self Sufficiency – Pool Sizes at the Blood Product Laboratory March 2022 pp19-23 INQY0000345
(1388) This would have been the theoretical assumption at the time. In practice, it seems that there was most likely a plateauing of risk once a certain level of exposure had been reached – a “threshold” effect.
(1389) When an Expert Committee on Hepatitis of the WHO considered the protective measures that could be taken against hepatitis. See the chapter on Blood Services and Addressing Risk: Response.
(1390) It may theoretically be possible to envisage that if pools had been smaller, that a consequence might have been less production, opening a gap between what was available from the NHS and what was desired by treating clinicians; and theoretically possible that if such a gap had emerged, commercial concentrate might have been bought to fill it. However, there is no hint of this theoretical possibility being raised in any contemporaneous document of which the Inquiry is aware.
(1391) Minutes of Haemophilia Reference Centre Directors special meeting 13 May 1983 HCDO0000003_008
(1392) Letter from Professor Bloom and Dr Rizza 24 June 1983 p1 HCDO0000270_004
(1393) The meeting on 10 December 1984 appears to have focused primarily on the use of Factor 8. The note taken by Mr Pettet of BPL recorded that: “Some discussion took place on the use of Factor IX. It was felt that the main problem was in balancing the risk of HTLV III against the risk of increased thrombogenicity associated with HT – Factor IX.” Minutes of the Haemophilia Reference Centre Directors meeting 10 December 1984 p5 HCDO0000394_117
(1394) The history of some of this controversy is relevant. In 1975, Professor Garrott Allen warned Dr Maycock about Konyne and Dr David Aronson (of the FDA) wrote an article in 1979 noting a “surprisingly high” incidence of icteric hepatitis. Letter from Professor Joseph Garrott Allen to Dr Maycock 6 January 1975 CBLA0000249; Aronson Factor IX Complex Seminars in Thrombosis and Hemostasis 1979 p12 MHRA0008115_041. Professor Bloom’s report for the HIV litigation however says that “In the early 1980’s several observers noted that there appeared to be a reduced risk of HIV infection and/or immunological abnormalities in patients with haemophilia B compared to those with haemophilia A.” His first reference is late 1983. Haemophilia Litigation Report June 1990 p123 DHSC0001297
(1395) Emphasis in the original. AIDS Advisory Document 14 December 1984 p3 HCDO0000270_007
(1396) Minutes of AIDS Group of Haemophilia Centre Directors meeting 11 January 1985 p4 HCDO0000521
(1397) Minutes of AIDS Group of Haemophilia Centre Directors meeting 17 June 1985 p4 HCDO0000523
(1398) Haemophilia Litigation Report June 1990 p125 DHSC0001297
(1399) See also NHD and UKHCDO Pivot Table 5.3.1 showing Annual consumption of CFC 1976 to 1994 18 March 2022 WITN3826017
(1400) Written Statement of Dr Terence Snape 8 February 2022 para 191 WITN3431001. See also Written Statement of Dr James Smith 27 July 2020 paras 71-73 WITN3433001
(1401) Written Statement of Dr Terence Snape 8 February 2022 paras 192-193 WITN3431001
(1402) Bleeding Disorders Statistics for the Infected Blood Inquiry 2022 p40 WITN3826016. Written Statement of Professor Pratima Chowdary p1 WITN3826030
(1403) Some also with Hepatitis B and other viruses.
(1404) 941 people with severe Haemophilia A were infected, compared to 18 with severe Haemophilia B. Expert Report to the Infected Blood Inquiry: Statistics September 2022 p16 EXPG0000049. Given that there are around six times as many people with Haemophilia A, multiplying 18 by 6 = 108. 941 divided by 108 = 8.7. It follows that people with Haemophilia A were 8.7 times more likely to be infected. The relative infectivity of commercial as opposed to NHS concentrate suggested by the crude ratio may well be even greater, when it is considered that most of those receiving Factor 8 concentrates had a substantial proportion of their treatment from NHS products. The extent of the effect of this in numerical terms is impossible to determine with any certainty.
(1405) Garrott Allen The Advantages of the Single Transfusion Annals of Surgery September 1966 p2 RLIT0000218
(1406) The raw figures have some uncertainties about them, which are not capable of precise quantification. The US also saw more cases in Haemophilia A than B. This was without being able to explain the difference being that a voluntary donor source for the plasma used as the basis of treatment of Haemophilia B patients but not Haemophilia A cases. An article co-authored by Dr Evatt (of the CDC) suggested that the reason could be because less treatment was needed for Haemophilia B, and because one manufacturing method used ethanol, citing CDC work with Hyland and Travenol that demonstrated that ethanol can reduce HIV activity in plasma. Stehr-Green et al Hemophilia-Associated AIDS in the United States, 1981 to September 1987 American Journal of Public Health April 1988 p3 MULL0002894, Piszkiewicz et al Inactivation of HTLV-III/LAV during plasma fractionation The Lancet 23 November 1985 CBLA0000011_052. Italy is a contrast to the US experience: it had more cases in people with Haemophilia B than Haemophilia A, having treated with Konyne and Immuno Bebulin. Schinaia et al Clinical Factors Associated With Progression to AIDS in the Italian Cohort of HIV-Positive Hemophiliacs Thrombosis and Haemostasis 24 March 1994 p5 MULL0003137. The uncertainties thus need to be acknowledged, but the overall assessment holds good that NHS products resulted in significantly less infectivity.
(1407) According to the Haemophilia Society, it is thought that around 10,000 people in the UK are registered with VWD, but many more have low levels of VWF that may contribute to bleeding problems.
(1408) Expert Report to the Infected Blood Inquiry: Bleeding Disorders and Blood Disorders January 2020 p23 EXPG0000002
(1409) The Haemophilia Society Understanding VWD 2023 pp6-8 RLIT0002359
(1410) Minutes of Haemophilia Centre Directors meeting 13 January 1977 p13 PRSE0002268
(1411) The 1976 annual returns recorded that 186 patients were treated with a total of 796,468 Factor 8 units in the UK. Of those, 674,045 units came from cryoprecipitate; 72,358 came from commercial concentrates; 41,025 units used were of NHS concentrates; and FFP totalled 9,040 units. The average per patient was 4,282 units. Dr Rizza and Rosemary Spooner Annual Returns from Haemophilia Centres 1976 18 October 1978 pp10-11 CBLA0000863
(1412) DDAVP is a synthetic drug modelled on a hormone naturally found in the body, and works to stimulate the release of a patient’s own clotting factors (Factor 8 and VWF) from storage sites in the body into the blood. Levels of the clotting factors are increased by three to six times the patient’s baseline level for 12-24 hours. Most but not all patients respond to DDAVP. If a patient is responsive to DDAVP, it can be used as the treatment of choice for all procedures and bleeding episodes except major surgery or injury. If a patient is partially responsive, DDAVP may be used for minor procedures and minor bleeding episodes, but an alternative may be required for major procedures and episodes. If there is no response when a patient is administered DDAVP, an alternative treatment is required. See: The Haemophilia Society Understanding VWD 2023 p12 RLIT0002359, Manucci Desmopressin (DDAVP) in the Treatment of Bleeding Disorders: The First 20 Years Journal of the American Society of Hematology 1 October 1997 RLIT0002365
(1413) Manucci et al 1-Deamino-8-Arginine Vasopressin: A New Pharmacological Approach to the Management of Haemophilia and Von Willebrand’s Disease The Lancet 23 April 1977 p1 PRSE0000638
(1414) Written Statement of Professor Charles Hay para 17.1, para 17.2 WITN3289039
(1415) The total number of units used to treat VWD patients was 1,296,000. Cryoprecipitate made up 1,030,000 units; 16,000 units of FFP; 171,000 units of NHS concentrate; and 79,000 units of commercial concentrate were used. Annual Returns for 1978 p3 1 November 1979 OXUH0000212_002
(1416) A total of 1,223,000 Factor 8 units were used to treat 233 patients with VWD, where cryoprecipitate accounted for 673,500 units; commercial concentrate accounted for 334,000 units; 209,000 units of NHS concentrate and 6,500 units of FFP were used. Annual Returns for 1979 p2 CBLA0001160
(1417) Minutes of Haemophilia Centre Directors meeting 20-21 November 1979 pp16-17 CBLA0001028
(1418) Annual Returns for 1980 p9 BART0002484
(1419) Annual Returns for 1981 CBLA0001612
(1420) Letter from Professor Bloom to Stan Godfrey 22 October 1981 DHSC0103196
(1421) Annual Returns for 1982 p6, p12 CBLA0001757
(1422) Annual Returns for 1983 pp2-3, pp7-8, p14 CBLA0001884_002
(1423) Written Statement of Professor Charles Hay paras 23.2-23.3 WITN3289039
(1424) Written Statement of Professor Charles Hay para 17.3 WITN3289039. He had been at Sheffield 1976-1978 and then returned as a senior registrar.
(1425) Minutes of Haemophilia Centre Directors meeting 30 September 1980 pp10-13 PRSE0003946. The von Willebrand’s Working Party was reported to be considering the criteria for diagnosis of the condition and the undertaking of a new survey with the collaboration of haemophilia centre directors.
(1426) Minutes of Haemophilia Centre Directors meeting 13 September 1982 pp5-6, p12 CBLA0001619
(1427) Letter from Professor Bloom and Dr Rizza 24 June 1983 p1 HCDO0000270_004
(1428) Haemophilia Treatment Policy Guidelines 18 May 1983 p1 WITN4029002
(1429) Draft minutes of Haemophilia Centre Directors meeting 17 October 1983 pp6-7 PRSE0004440. The discussion regarding the von Willebrand Working Party merely recorded that Dr Tuddenham presented a written report, saying that “the analysis was proving most interesting and he hoped that a paper would be prepared in the not too distant future for publication.” Draft minutes of Haemophilia Centre Directors meeting 17 October 1983 p12 PRSE0004440
(1430) AIDS Advisory Document 14 December 1984 p2 HCDO0000270_007
(1431) Annual Returns for 1983 pp2-3, p15 CBLA0001884_002
(1432) Annual Returns for 1984 p7, p13 CBLA0002279_002
(1433) Annual Returns for 1985 p1, p13 BART0002267
(1434) Over the following months her blood was repeatedly tested (“I have not got a clue what they were doing these tests for”); only in 1997 did she learn, from her GP, that the treatment in November 1983 had infected her with Hepatitis C. Written Statement of Pauline Nicholson paras 2-11 WITN0079001
(1435) Letter from Harrogate General Hospital 1 May 1979 p2 WITN3118003
(1436) Written Statement of ANON paras 2-8 WITN3118001
(1437) Written Statement of Catherine Slater paras 5-7 WITN1732001
(1438) Written Statement of Beryl Partington paras 1-6 WITN3545001. They learned of his infection by letter from Royal Manchester Children’s Hospital in September 1985. Nick died in 2012 at the age of 42.
(1439) Letter from S Sadek to Dr G Caithness 4 October 1984 WITN2175002, Written Statement of Ian Joy paras 5-6 WITN2175001
(1440) Written Statement of Frances Joy para 4, paras 10-11 WITN3098001
(1441) Written Statement of ANON paras 7-8 WITN0140001. Each time she questioned the decision to treat her prophylactically with cryoprecipitate as she felt she did not need it. As a blood product, she presumed it had been heat treated – which cryoprecipitate was not.
(1442) Written Statement of Melanie Richmond paras 3-7 WITN2254001
(1443) Written Statement of Professor Pratima Chowdary on behalf of UKHCDO p1 WITN3826030
(1444) Written Statement of William Wright paras 7-13 WITN2287001, Written Statement of William Wright paras 2-3 WITN2287002, William Wright Transcript 5 July 2019 pp10-22 INQY1000028. Responsibility for these failures rests with the Edinburgh Royal Infirmary. As for Professor Ludlam’s responsibility, he did not personally administer the treatment, but he was responsible for the unit. In that capacity he was responsible for there being no gatekeeping to ensure appropriate treatment on this occasion. Though there is no evidence that there was a policy in place to ensure that previously untreated patients (such as Bill Wright) or people whose haemophilia was mild were not treated with factor concentrate except as a last resort; and there was no arrangement as yet to obtain 8Y though it was likely to be safer. Professor Ludlam’s understanding was that the duty doctor should have phoned the registrar to let her know that there was no record held at the centre relating to Bill Wright. He did not do so. Had he done so, Professor Ludlam explains that he would have contacted the Glasgow centre to acquire details of Bill Wright’s previous investigations. He describes that the duty doctor took it on himself to consider that Bill Wright had haemophilia, without seeking the appropriate clotting screen which would have been available on a 24-hour basis. Written Statement of Professor Christopher Ludlam WITN3428049. In any event, DDAVP or cryoprecipitate could have been given, or the option of no treatment (Bill Wright would have had to be consulted about his options and was not) and the unit should have made aware of this and should in any event have discussed the options and hepatitis risks with the patient. Professor Ludlam is not personally responsible if a member of staff disobeys instructions and treats a patient with possible haemophilia without investigation and without a diagnosis with a clotting factor concentrate. What seriously compounds the failings in this particular case is that Professor Ludlam did not reveal any details of what had happened, as he should have done, to his patient until the exigencies of litigation brought them to light some ten years later. At the time he said to Bill Wright only that he had been given factor concentrate, there was a 50% chance he would get hepatitis, but that he would be ok, and gave false reassurance that any hepatitis that resulted would be of little or no significance. He offered no apology or explanation for what had happened even though the contemporaneous documents show that he knew that what had happened should not have been done.
(1445) The issue explored in the main text here is whether this could and should have been avoided if someone had had the foresight to obtain a supply of 8Y. However, the treatment which Bill Wright received illustrates many of the wider failures which have already been discussed in this chapter: the misplaced confidence in concentrates, the failure to have safety at the forefront of the clinician’s mind (even after so many had been infected with HIV), the failure to consider and offer alternative, safer treatments (such as DDAVP for someone like Bill with a mild haemophilia, or even the option of no treatment), the failure to advise as to the risks of the treatment being offered. As put in the submissions on behalf of core participants represented by Thompsons Scotland: “The case is clearly demonstrative of the fact that, despite the horrors of the HIV years and the multiple AIDS infections in Edinburgh, no effective change from the previous treatment regime had occurred. Bleeding was simply equated with treatment with a factor concentrate. No consideration of the necessity of that treatment took place. No consideration or discussions of the inevitable infection with a potentially fatal disease took place either.” Written Submissions on behalf of Core Participants Represented by Thompsons Scotland 16 December 2022 para 4.257, p710 SUBS0000064
(1446) This “minimal” is a weasel word. He had had no treatment with concentrate. If he had been asked, and his answer had been listened to, he would have told the doctors that.
(1447) Letter from Dr Boulton to Dr Perry 27 June 1986 PRSE0003845. Professor Ludlam told the Inquiry that he was ruthful because he had not been informed about the patient and he was disappointed and cross that he had not been consulted, so as to help make the decision about what treatment would be appropriate. Professor Christopher Ludlam Transcript 4 December 200 pp17-18 INQY1000080
(1448) At the meeting of the CBLA’s Central Committee for Research and Development in Blood Transfusion on 9 July 1985 it was reported that “several patients have already safely passed the point at which the first evidence of NANBH transmission would have been expected.”Dr Forrester, of the SHHD, and Dr Brian McClelland did not attend and sent their apologies, but would presumably have received the minutes in due course. Minutes of the CBLA Central Committee for Research and Development in Blood Transfusion meeting 9 July 1985 p3 PRSE0002420
(1449) Dr Robert Perry Penrose Inquiry Transcript 7 December 2011 p27 PRSE0006074
(1450) Letter from BPL to Haemophilia Centre Directors and Regional Transfusion Directors 24 July 1985 p2 CBLA0002224
(1451) Professor Christopher Ludlam Transcript 4 December 2020 pp24-25 INQY1000080
(1452) Minutes of CBLA Central Committee for Research and Development in Blood Transfusion meeting 19 December 1985 p2 CBLA0002287
(1453) PFC Report for SHS Haemophilia and SNBTS Directors Meeting March 1986 p4 PRSE0003457. There was no express discussion of this issue recorded in the minutes of the meeting on 5 March 1986. Minutes of SNBTS Directors and Haemophilia Directors meeting 5 March 1986 PRSE0001081
(1454) Note of a meeting held at PFC 17 March 1986 p3 PRSE0003764
(1455) Dr Robert Perry Transcript 1 April 2022 p109 INQY1000184
(1456) Professor Christopher Ludlam Transcript 4 December 2020 pp26-28 INQY1000080
(1457) On 27 June 1986 Dr Boulton wrote to Dr Cash stating that “Apparently a few weeks ago [Dr Ludlam] was asking Brian McClelland if VIIIY could be made available in the event of a ‘virgin’ haemophiliac being presented. He tells me that he would be happy to treat such patients with a product prepared by the SNBTS that has been subjected to an ‘equivalent’ heat-treatment regime.” Letter from Dr Boulton to Dr Cash 27 June 1986 PRSE0002000
(1458) Professor Christopher Ludlam Transcript 4 December 2020 p22 INQY1000080. Dr Boulton wrote to Dr Perry asking if the latter could obtain some vials of BPL’s 8Y for use by Dr Ludlam “if a previously untreated haemophilic presented for replacement therapy.” Letter from Dr Boulton to Dr Perry 7 July 1986 PRSE0004097. Dr Perry wrote on the same day (in response to an earlier letter from Dr Boulton dated 4 July) saying that “we could probably get supplies of 8Y for special cases.” Letter from Dr Perry to Dr Boulton 7 July 1986 PRSE0003814. By “special cases” he was referring to minimally or previously untreated patients. Dr Robert Perry Transcript 1 April 2022 p114 INQY1000184. On 10 July 1986 Dr Perry wrote to Mr Pettet of BPL, referring to the case of the “virgin” patient who had recently been treated with the PFC’s product and had developed markers for non-A non-B Hepatitis, and asking BPL to supply “a very modest quantity of 8Y” to cover the treatment of “similar virgin patients who may appear.” Letter from Dr Perry to Mr Pettet 10 July 1986 PRSE0004383. On 1 August 1986 Dr Smith sent Dr Perry the requested vials of 8Y. Letter from Dr Smith to Dr Perry 1 August 1986 PRSE0002616. The correspondence revealed that there were in fact two routes to getting a small supply of 8Y for Scotland: the first was that any Scottish or Northern Irish patient who might need it could be entered in the trial and be treated with 8Y that way; the second was that BPL would in any event send a supply to PFC. Dr Robert Perry Transcript 1 April 2022 pp117-118 INQY1000184
(1459) Professor Christopher Ludlam Transcript 4 December 2020 p32 INQY1000080
(1460) Letter from Dr Boulton to Dr Perry 4 July 1986 PRSE0001784, Note showing Phase II and Phase III Production PRSE0002783
(1461) There is no reason to think that an earlier request for a supply of 8Y would have been unsuccessful: both Mr Pettet and Dr Smith responded positively to the request that was eventually made in July 1986.
(1462) Dr Perry’s view, as expressed to the Inquiry and with hindsight, was that UKHCDO should have discussed the matter, involving as appropriate BPL and PFC, and should have come up with a policy for identifying any patients that were previously untreated, whether in Scotland, Northern Ireland, Wales or England, for whom 8Y would be appropriate, and that an operational arrangement could then have been made to enable that to happen. Dr Robert Perry Transcript 1 April 2022 pp122-124 INQY1000184
(1463) It is not a justification that the effect of providing 8Y to Scotland would have diminished the supply of 8Y available in England, since there would almost certainly have been plenty to treat previously untreated (or only lightly treated) patients in both countries.
(1464) Dr Robert Perry Transcript 1 April 2022 p123 INQY1000184
(1465) See for example the letter from Dr Perry dated 6 December 1984 which set out the arrangements for the supply of NY to regional transfusion centres, including Belfast. Letter from Dr Perry to Transfusion Directors 6 December 1984 PRSE0002675
(1466) Letter from Dr Mayne to Dr Perry 18 February 1988 p39 PRSE0000129
(1467) Correspondence within Submission for a Product Licence Variation for SNBTS Factor VIII Z8 pp33-39 PRSE0000129. The chain of correspondence between Drs Mayne, Perry and Dempsey is at NIBS0001965. Dr Mayne expressed “delight” with the information it was the older product which had transmitted the hepatitis, and not the new Z8: but she did not expressly recognise, at the same time, that this child should never have been given NY when Z8 was available. Correspondence within Submission for a Product Licence Variation for SNBTS Factor VIII Z8 p42 PRSE0000129. Her comment was inapposite in this context.
(1468) Correspondence within Submission for a Product Licence Variation for SNBTS Factor VIII Z8 p34 PRSE0000129. Dr Dempsey’s statement to the Inquiry states that Z8 was introduced at the hospital in July 1987 and that this was an isolated error which arose from a failure to return two vials of NY to the blood bank for disposal. The vials were subsequently reconstituted for issue to the ward where they were administered by medical staff. The contemporaneous documents refer to the patient being infected with non-A non-B Hepatitis; Dr Demsey’s statement says that the patient made a full recovery and did not seroconvert to Hepatitis C. Written Statement of Dr Stanley Dempsey paras 32.1-32.5 WITN5560001
(1469) Correspondence within Submission for a Product Licence Variation for SNBTS Factor VIII Z8 p33 PRSE0000129
(1470) Correspondence within Submission for a Product Licence Variation for SNBTS Factor VIII Z8 p35 PRSE0000129
(1471) This is based on an analysis in the Penrose Inquiry preliminary report, coupled with a letter from Dr Cacchia, director at Dundee, which speaks of the Dundee experience over a slightly longer time period until December 1987. The Penrose Inquiry Preliminary Report September 2010 para 9.326 PRSE0007003, Letter from Dr Cachia to Dr Keel 17 March 2000 PRSE0000295, Written Submissions on behalf of Core Participants Represented by Thompsons Scotland 16 December 2022 paras 4.303-4.304, pp739-741 SUBS0000064
(1472) It is important to bear in mind that the purpose of these visits was, from the perspective of the pharmaceutical company, to make sales, and that these companies were in competition with one another for increased shares of the UK market. An internal memo from Christopher Bishop of Armour in March 1986 gives a flavour of this. Referring to a forthcoming meeting of the “Haemostasis Club”, the memo described Professor Savidge, Dr Kernoff and Dr Preston as “the leading advocates for the ‘safer wet heat treated’ Alpha factor VIII (Profilate). I suspect that this could be a very cleverly connived Meeting at the instigation of either these three Clinicians or Alpha themselves to convert all Directors to a product/s which can be shown to have a better track record with regard to the elimination of NANB hepatitis.” Christopher Bishop urged attendance by Armour colleagues, “particularly as it relates to our market position in the U.K.” He noted that “Geoff Savidge has kindly agreed to put questions on our behalf to the Panel … I would suggest that one or two very carefully constructed questions be discussed between us and put to Geoff in advance.” Emphasis in original. Memo from Christopher Bishop to Peter Harris 6 March 1986 p1 ARMO0000505_001
(1473) Dr Colvin added that he was “not aware of any particular reason that I would use any particular commercial product that wasn’t related to price, because I regarded them as, frankly, equivalent in both efficacy and safety.” Dr Brian Colvin Transcript 7 October 2020 p136, p138 INQY1000062. Linda Frith, who worked for Cutter, described how she would generally meet haemophilia centre directors by appointment once every three months. Written Statement of Linda Frith para 215 WITN6407001. Christopher Bishop, of Armour, expected that sales representatives would visit a centre at least once a month. Christopher Bishop Transcript 4 November 2021 pp52-53 INQY1000158
(1474) These could be gifts for clinical staff, or gifts for patients. An example of the former is the set of white leather suitcases seen at Birmingham Children’s Hospital and understood to be a gift from a pharmaceutical company. Written Statement of Elisabeth Buggins para 59 WITN1021001. Christopher Bishop, of Armour, recalled gifts such as calculators and paperweights. Christopher Bishop Transcript 4 November 2021 pp14-15 INQY1000158. An example of gifts for patients is the evidence of Adrian Goodyear, regarding Treloar’s. He recalled pharmaceutical companies leaving gifts for the pupils: “watches, backpacks, stationery … there was a couple of genuinely special gifts. One was again this pyramid watch. It looked expensive. It was heavy and there was a box of those. But the ultimate prize, if you like, in that time-frame was a chronograph watch … everybody wanted one of those.” Adrian Goodyear Transcript 5 June 2019 pp72-73 INQY1000014
(1475) Professor Savidge, in his evidence to the Archer Inquiry, discussed funding for research as follows: “Generally speaking, if one had dealings with a commercial company -- and I have probably had more dealings with commercial companies than most -- the rules are very simple: they pay for everything to do with the research that they expect you to do … One is expected, as part and parcel of being involved with the research project for a commercial company, to actually present one’s data … So you have to go where you are requested to go and give a presentation. You may be offered an honorarium or you may not, but that really covers the fact you are up until 2.30 doing a report or something similar and you expect perhaps to at least have a few shekels to keep your eyes open. So I think it depends very much upon the individuals of what happens.” Professor Geoffrey Savidge Archer Inquiry Transcript 19 September 2007 pp145-146 ARCH0000011
(1476) Letter from Dr D Lott to Dr Jones 23 December 1980 HHFT0001201_003
(1477) Letter from Christopher Bishop to Dr Rizza 6 August 1981 OXUH0001624_004. This letter also addressed a direct request made by Dr Rizza for “financial support to enable us to continue employing a Health Visitor in our Hepatitis Studies”, with a similar request being made to the MRC and the Haemophilia Society. Letter from Dr Rizza to Christopher Bishop 27 August 1981 OXUH0001624_003. Armour’s response was to suggest waiting until Dr Rizza knew the outcome of his applications to the MRC and the Haemophilia Society, before making any application to its Grants and Donations Committee.
(1478) The request was mainly for a year’s salary for a senior technician, with Dr Kernoff adding that: “Any help Armour is able to give us would be greatly appreciated.” Letter from Dr Kernoff to Christopher Bishop 15th March 1983 ARMO0000236. Armour’s response is at: Letter from Christopher Bishop to Dr Kernoff 7 April 1983 ARMO0000238
(1479) See Armour’s letter to Dr Preston: Letter from Christopher Bishop to Dr Preston 21 April 1983 ARMO0000239. Details of the proposal for which funding was being sought: Commitment approval and cost breakdown for Factorate study 9 May 1983 ARMO0000246. Later correspondence demonstrates that funding was made available: Letter from Dr Preston to Christopher Bishop 22 June 1983 ARMO0000268, Letter from Christopher Bishop to Dr Preston 19 July 1983 ARMO0000272, Letter from Robert Christie to Dr Preston 29 July 1983 ARMO0000282, Letter from Dr Preston to Robert Christie 11 August 1983 ARMO0000286
(1480) “I have paid our first 1985 donation to your research fund to the Finance Department of the Central Birmingham Health Authority. We continue to be very interested in the progress of this project.” Letter from Robert Christie to Dr Hill 27 March 1985 ARMO0000370
(1481) 1981 Koate Marketing Notes p9, p13 BAYP0000021_016. Dr Muriel Tillyer, who was director of the haemophilia centre at the Lewisham Hospital from 1997, recalled pharmaceutical companies providing “help to patients on home treatment, delivering supplies and providing some training”, and grants to assist clinical staff to attend conferences. The question of influence was “an important one that I was alive to. I tried to ensure that I offered the same access (limited) to all the companies”, adding that the relationships did not influence the choice of products. Written Statement of Dr Muriel Tillyer para 13 WITN3298005
(1482) Minutes of Cutter Laboratories Limited Board meeting 16 December 1980 p5 BAYP0000021_063
(1483) Cutter December Monthly Report: Area 2 – The North and Wales p1 BAYP0000025_088. In a letter of 2 November 1984 to Cutter, Dr Wensley referred to his request for financial support “as our local research fund grant has not been renewed” and indicated that “The direction of our future work has not been settled, but it could certainly be further slanted towards problems of mutual relevance.” Letter from Dr Wensley to Mr Marzouk 2 November 1984 BAYP0000025_062
(1484) Letter from Linda Frith to Dr Kernoff 11 April 1985 BAYP0000024_172. Cutter also provided funding for expenses of a meeting of the Haemostasis and Thrombosis Club in November 1986 and offered £5,000 to the haematology department at the Middlesex Hospital, asking for “a letter saying what the funds would be used for, e.g. to help support a research project or to a researcher, etc.” Letter from Linda Frith to Dr Machin 14 November 1986 p2 BAYP0000009_063
(1485) Cutter Laboratories Situation Report April 1986 16 May 1986 p3 BAYP0000008_189
(1486) Memo from Brian Dyos to Pete DeHart regarding meeting with Professor Bloom 14 May 1985 BAYP0000024_225
(1487) The funding may have been in relation to overseas speakers who had been invited. Minutes of Haemophilia Reference Centre Directors meeting 14 April 1986 p6 HCDO0000420. Professor Ludlam’s evidence to the Inquiry was that pharmaceutical representatives did not attend the haemophilia centre directors’ annual general meetings, but that there could be an associated educational day which might involve extra expense (such as speakers from abroad) and where “the relevant pharmaceutical companies were keen to have an opportunity to meet with haemophilia directors.” Professor Christopher Ludlam Transcript 3 December 2020 p61 INQY1000079. Peter Coombes, of Immuno, confirmed that pharmaceutical companies were not allowed to attend the actual meeting but were invited to attend the educational presentations and allowed to put up a promotional stand. Written Statement of Peter Coombes para 56.1 WITN6409001. See further the statement of Robert Nicholson, also of Immuno. Written Statement of Robert Nicholson paras 35.2-35.3 WITN7595001. An international symposium was organised in Manchester in September 1982, to follow the haemophilia centre directors’ meeting, with Armour “making a generous financial contribution towards the cost of the symposium”and the publication of the proceedings of the symposium. University of Manchester Department of Clinical Haematology Current Topics in Haemophilia 1983 p2 DHSC0002221_003
(1488) £6,500 from Alpha 1986/87, £1,000 from each of Alpha, Armour and Immuno in 1997/78 and £1,000 from Armour in 1989/90. The donations of £1,000 may have been “to help staff get to scientific meetings.” Note by Dr Ludlam regarding funding by pharmaceutical companies 1970s and 1980s STHB0000220
(1489) Letter from Dr Kernoff to L Jones 23 June 1980 p3 BART0000913
(1490) Letter from Dr Kernoff to L Jones 23 June 1980 p3 BART0000913
(1491) Professor Edward Tuddenham Interview Transcript 29 September 2016 pp3-4 JEVA0000011
(1492) ie pharmaceutical companies.
(1493) Professor Edward Tuddenham Interview Transcript 29 September 2016 p4 JEVA0000011. Although Professor Tuddenham was less exposed to this hospitality because he “took a very academic route” he said that he could see how it could influence people. He confirmed in his oral evidence to the Inquiry that this account of lavish hospitality was based on his direct knowledge of the way in which the pharmaceutical companies acted. Professor Edward Tuddenham Transcript 22 October 2020 pp134-135 INQY1000067
(1494) Written Statement of Professor Liakat Parapia para 9a WITN0785003
(1495) Professor Liakat Parapia Transcript 29 October 2020 pp162-163 INQY1000070. A Royal College of Physicians Working Party on the Ethics of the Relationship between Physicians and the Pharmaceutical Industry was held on 18 October 1984. The chairman of the Association of British Pharmaceutical Industry Code of Practice Committee reported to the Working Party that he “had heard of a few cases of excessive hospitality and gifts but felt that what he was seeing on the Committee was the tip of a very large iceberg; due to the reticence of the people receiving these rewards, the view was limited.” He believed that the medical profession “had to be tougher generally” and hoped that the Working Party “would adopt a strict attitude.” Agenda and Minutes of College Working Party on the Ethics of the Relationship between Physicians and the Pharmaceutical Industry meeting 18 October 1984 p3 RCPH0000299
(1496) Professor Liakat Parapia Transcript 29 October 2020 p164 INQY1000070. Other clinicians, such as Dr Bevan, confirmed that support from pharmaceutical companies was necessary in order for medical staff to be able to attend the major international conferences, often in the US, “where you are likely to see state of the art research discussed and also to be able to discuss with peers in other countries various approaches.” There was, he said, “No way” that any NHS clinician could fund that out of any NHS funds. Whilst acknowledging that “the company’s motive is always profit, always”, Dr Bevan also recalled that there would be funding for booklets and educational facilities for patients, which he described as “a range of activities which would seem to be completely blameless or to have no ulterior motive really.” Dr David Bevan Transcript 12 January 2021 pp112-116 INQY1000086. Dr Mayne, from the Belfast Haemophilia Centre, would accept funding for travel to scientific meetings, but was “unreceptive to gifts”, such that it became known that any gifts sent or left with her staff would be returned. Educational gifts to the centre and accessories for patients were, however, regarded as acceptable. Written Statement of Dr Elizabeth Mayne paras 118.1-118.3 WITN0736009
(1497) Professor Edward Tuddenham Interview Transcript 29 September 2016 p3 JEVA0000011
(1498) Letter from Dr Biggs to Dr Jones 8 November 1976 p1 PJON0000050_001
(1499) Letter from Dr Jones to Dr Biggs 19 November 1976 PJON0000051_001. At the meeting of directors in January 1977, Dr Jones did declare an interest as a temporary paid consultant to Hyland and volunteered to withdraw from the meeting whilst the question of supplies was discussed, but it was agreed that he could stay. Minutes of Haemophilia Centre Directors meeting 13 January 1977 pp14-15 PRSE0002268. In 1980 Dr Jones visited and reported on plasmapheresis centres managed by Plasma Alliance, which had been acquired by Armour Pharmaceuticals. Memo from Dr Jones regarding Paris trip 17 September 1979 WITN0841028, Revlon Health Care Group A Report on Plasmapheresis in the United States June 1980 PJON0000040_001. Dr Jones also appeared on behalf of Speywood before the Committee on Safety of Medicines in 1981, saying that he had come to the hearing “as an independent consultant (unpaid) to advise the Committee that in his capacity as director of a haemophilia centre, he had satisfactorily treated patients with Humante.” Appendix C to Minutes of Committee on Safety of Medicines meeting p4 MHRA0036365_018
(1500) At that time Professor Rawlins was professor of clinical pharmacology at the University of Newcastle upon Tyne. He was quoted in a newspaper article in March 1981 as saying that: “There is a certain amount of covert bribery. One drug company recently flew a lot of consultants to Spain to hear about their drugs. They invited me to go. If they were introducing their drugs to people in Newcastle, they wouldn’t get such a good turnout, whereas going to Spain could whet appetites. When you talk to doctors, they always say ‘I go along and have their drink and I am not influenced by it,’ but sub-consciously they must be. The companies are not idiots. They would not do it if it was not worthwhile … Education gets mixed up with financial rewards or other substitutes.” The Sunday People Bribery 29 March 1981 JEVA0000125
(1501) Agenda and Minutes of College Working Party on the Ethics of the Relationship between Physicians and the Pharmaceutical Industry meeting 18 October 1984 p6 RCPH0000299
(1502) Rawlins Evidence to the Royal College of Physicians Working Party on Ethics of the Relationship between Physicians and the Pharmaceutical Industry p7 RCPH0000310
(1503) Working Party of the Royal College of Physicians Report on the Relationship Between Physicians and the Pharmaceutical Industry March 1986 p10 RCPH0000105
(1504) This begs the question who is to make the judgement. The “may be” does not suggest doubt as used in this context – it is effectively saying “is, unless specifically justified”. The guidance notes that: “No objection can, however, be taken to grants of money or equipment by firms to institutions such as hospitals, health care centres and university departments, when they are donated specifically for purposes of research.” General Medical Council Professional Conduct and Discipline: Fitness to Practise April 1985 pp33-34 GMCO0001696_011
(1505) Expert Report to the Infected Blood Inquiry: Medical Ethics April 2020 p112 INQY0000241
(1506) Closing submissions on behalf of the Saunders Law core participants 16 December 2022 para 81 SUBS0000060
(1507) Written submissions on behalf of the core participants represented by Watkins & Gunn 16 December 2022 paras 156-165 SUBS0000061
(1508) Submissions on behalf of the core participants represented by Collins Solicitors 16 December 2022 para 676 SUBS0000063
(1509) See also the chapter on Viral Inactivation where it deals with the withdrawal of Armour HT from the UK market. It is disturbing to note that when a serious infection (HIV) was identified in patients as a consequence of having a particular product (Armour HT), with implications for public health, because others might in turn have been infected by that patient, the first port of call of the clinician concerned should not have been the DHSS, but was instead the manufacturer. It is difficult to understand quite why Armour was then offered “participation” in any article about the matter, rather than being told of the form of the publication and permitted to comment if they wished. It also appears that it was an employee of Armour who reported the findings to the DHSS, and not the clinician concerned. In overview, the matter was reported to the DHSS; and it may be appropriate that if (for instance) a consumer has concerns about the safety of a product they have purchased they should raise it in the first place with the supplier, before raising any concern more widely – but the aspects mentioned above, in the particular field of healthcare, against a background in which money may have been influential, lead to the observation that more needed to be done to avoid any appearance of bias in relation to the treatment of patients.
(1510) Minutes of Haemophilia Centre Directors meeting 1 October 1968 p4 HCDO0001013
(1511) Letter from Dr Biggs to Mr Guthrie 14 December 1970 AMRE0000012_004. See further the discussion of the research undertaken on pupils at the school in the chapter entitled Treloar’s.
(1512) Letter from Dr Ludlam to Dr Craske 28 April 1980 p1 LOTH0000031_027
(1513) Letter from Professor Bloom and Dr Rizza to all Haemophilia Centre Directors 11 January 1982 p1 HCDO0000252_042. The letter is misdated 11 January 1982 but it is clear from its context and from other documents that it was a letter sent in January 1983.
(1514) Bruce Norval Transcript 9 June 2021 p111 INQY1000126
(1515) Expert Report to the Infected Blood Inquiry: Medical Ethics April 2020 p91 INQY0000241. As explained in the BMA’s 1993 publication Medical Ethics Today “In principle, a general need for research is usually conceded to be beyond argument. Nevertheless criticism is rightly levelled at particular research projects which ignore patient rights or whose methodology, execution or utility is suspect.” BMA Medical Ethics Today: Its Practice and Philosophy 1993 p227 BMAL0000089
(1516) Medical Ethics Expert Panel Transcript 27 January 2021 p61 INQY1000091
(1517) Written Statement of Professor Edward Tuddenham para 93 WITN3435002. By way of comment, it is almost impossible to avoid side effects when administering modern treatments, and some may be harmful, so the statement is not an absolute principle but nonetheless a useful starting point.
(1518) Expert Report to the Infected Blood Inquiry: Medical Ethics April 2020 p93 INQY0000241
(1519) The Nuremberg Code 1947 stemmed from the international concern that arose following the atrocities, conducted in the name of scientific experimentation, in concentration camps. Writing in 1993 the BMA observed that “Most people will strongly refute the existence of even the ghost of a connection between the criminal acts of wartime and present-day research and see no analogy between the two. Nevertheless, this is clearly not an issue for complacency. As a 1991 Lancet editorial indicated: ‘Like other self-evident truths, the need for informed consent has not been universally recognised, even after the Nuremberg judges stated it so plainly. The columns of the Lancet bear witness to research by fraud and research verging on common assault in which patients participated in pure research disguised as clinical investigation or treatment.’ ” BMA Medical Ethics Today: Its Practice and Philosophy 1993 pp230-231 BMAL0000089
(1520) British Medical Journal The Nuremberg Code 1947 Permissible Medical Experiments 7 December 1996 p1 RLIT0000372. This means that the person involved should, amongst other matters, “have sufficient knowledge and comprehension of the elements of the subject matter involved as to enable him to make an understanding and enlightened decision. This latter element requires that before the acceptance of an affirmative decision by the experimental subject there should be made known to him the nature, duration, and purpose of the experiment; the method and means by which it is to be conducted; all inconveniences and hazards reasonably to be expected; and the effects upon his health or person which may possibly come from his participation in the experiment.”
(1521) World Medical Assembly Declaration of Helsinki: Recommendations guiding doctors in clinical research June 1964 p2 RLIT0001505. Such consent should “as a rule” be obtained in writing.
(1522) Counsel Presentation on Ethical and Clinical Guidance for Clinicians and Other Healthcare Practitioners May 2021 pp32-39 INQY0000249
(1523) Convention for the Protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine (Oviedo Convention) 1997 RLIT0002356
(1524) BMA Medical Ethics Today: Its Practice and Philosophy 1993 pp229-230 BMAL0000089
(1525) BMA Medical Ethics Today: Its Practice and Philosophy 1993 p231 BMAL0000089. See also the oral evidence of the medical ethics expert group: “people need to know what the alternatives are to participation and what the risks and benefits of participation and non-participation are and what their probabilities are. So they need to be able to understand what will happen to them or what is likely to happen to them or what could happen to them, both in terms of the risks and benefits, both of taking part and not taking part. They also will need to be informed of the broader context of the research.” (Professor Julian Savulescu) Medical Ethics Expert Panel Transcript 27 January pp63-64 INQY1000091
(1526) A study of patients with antibodies by Dr Rizza and Dr Biggs, reported in the British Journal of Haematology in 1973, appears to be an example of a genuinely retrospective assessment. Rizza and Biggs The Treatment of Patients who have Factor-VIII Antibodies British Journal of Haematology 1973 IPSN0000343_015
(1527) Professor Charles Hay Transcript 5 November 2020 p116 INQY1000073
(1528) Medical Ethics Expert Panel Transcript 27 January 2021 pp119-120 INQY1000091
(1529) For an account of some of the work undertaken by the Blood Coagulation Research Unit see Biggs Thirty Years of Haemophilia Treatment in Oxford British Journal of Haematology 1967 RLIT0000043_021
(1530) Progress Report 1967-1970 of the External Staff at the Oxford Haemophilia Centre 1971 p5, p7 OXUH0003647_002
(1531) Blumberg A Study of the Occurence of Various Inherited and Acquired Antigens and Antibodies in the Blood of Patients with Haemophilia Who have Been Seen at the Oxford Haemophilia Centre 1972 p3, p22 JEVA0000006. This related to patients treated at Oxford: indeed, there is a sample punch card which makes this clear, since it contains a record of “Date First seen in Oxford”. This particular dataset is thus not directly related to any national database. However, from the mid 1950s diagnoses of haemophilia in the UK were notified to a Central Haemophilia Register, initially kept at Oxford for the MRC but discontinued in 1967. The UK Haemophilia Centre Doctors’ Organisation (“UKHCDO”) then started collecting data about patient numbers, product usage, inhibitors and jaundice. UKHCDO census data was standardised in 1975. The start of this process is recorded in: Letter from Dr Margaret Gorrill to Dr Macfarlane 2 November 1955 OXUH0003509_017. There were said to be concerns about confidentiality of the data; and that there was no evidence to suggest that the limited information in the register had been, or was likely to be, useful for research purposes. Minutes of Ministry of Health meeting 28 October 1966 MRCO0005298_001. The Ministry of Health wrote on 19 June 1967 to haemophilia directors to tell them it was no longer necessary to notify new cases to a central register, but each individual centre should keep a record of all patients to whom haemophilia cards were issued, with the essential information previously noted in the central register. Letter from R Hughes to Haemophilia Centre Directors 19 June 1967 DHSC0100025_056. Haemophilia centre directors at their meeting 1 October 1968 recorded that they felt there was no need at present to have a central register, though they would collect information about inhibitors. Minutes of Haemophilia Centre Directors meeting 1 October 1968 p4 HCDO0001013. In parallel the MRC Cryoprecipitate Working Party agreed that haemophilia centre directors should also collect information about jaundice. Minutes of MRC Cryoprecipitate Working Party meeting 1 October 1968 p3 DHSC0103189. At a meeting on 5 April 1971 it was agreed that records should be kept and sent to Oxford at the end of each year. These would include the full list of names of patients treated, to prevent duplication where someone attended more than one centre during the year. Minutes of Haemophilia Centre Directors meeting 5 April 1971 p3 HCDO0001014. New forms were prepared for returns from 1972 onwards. Minutes of Haemophilia Centre Directors meeting 27 October 1972 pp2-4 HCDO0001015. In 1975 the forms were simplified. Three sets would be returned: (a) annual returns of therapeutic materials used, deaths, lists of patients with haemophilia treated in the year; (b) new cases of Haemophilia A or B and new cases of inhibitors; (c) a hepatitis survey, noting the material used in the six months prior to the development of jaundice, details of symptoms and history, and a Hemofil return for all centres using Hemofil which “should be completed for all Centres using Hemofil and will be forwarded to Dr Craske so that he can complete his study.” Minutes of Haemophilia Centre Directors meeting 18 September 1975 pp5-6 OXUH0003735. The history is summarised in Bleeding Disorders Statistics for the Infected Blood Inquiry 2022 pp9-11 WITN3826016
(1532) Craske et al Commercial factor VIII associated hepatitis, 1974-75, in the United Kingdom: a retrospective survey Journal of Hygiene 1978 p1 1978 HSOC0000009
(1533) Alton was the haemophilia centre at which boys from Treloar’s were then treated.
(1534) Minutes of Haemophilia Centre Directors meeting 18 September 1975 pp5-6 OXUH0003735
(1535) Minutes of Haemophilia Centre Directors meeting 13 January 1977 pp10-11 PRSE0002268
(1536) Three patients had died from illnesses not related to transfusion hepatitis and so were excluded from the survey.
(1537) Hemofil Associated Hepatitis – 1974-75 in the United Kingdom:A Retrospective Survey pp1-2, p7 CBLA0000566
(1538) Craske et al Commercial factor VIII associated hepatitis, 1974-75, in the United Kingdom: a retrospective survey Journal of Hygiene 1978 HSOC0000009
(1539) A study which must have involved the sharing of personal medical data about them without their knowledge and consent.
(1540) A matter of considerable concern, since if they had been told they should also then have been told of Dr Craske’s conclusion that if they had been treated with another product they might not have become infected.
(1541) Hemofil Associated Hepatitis – 1974-75 in the United Kingdom:A Retrospective Survey p8 CBLA0000566
(1542) Haemophilia Directors Hepatitis Working Party Hepatitis Associated Commercial Factor VIII 1976 22 September 1977 p1 CBLA0000681_009
(1543) Further Survey of Factor VIII Associated Hepatitis 1976-7 January 1977 p1 HCDO0000392_057. The protocol proposed that the survey would also include NHS Factor 8, but Dr Craske’s subsequent report was limited to Hemofil and Kryobulin. Haemophilia Directors Hepatitis Working Party Hepatitis Associated Commercial Factor VIII 1976 22 September 1977 CBLA0000681_009
(1544) Minutes of UK Haemophilia Centre Directors meeting 24 October 1977 p7, p19 PRSE0001002, Haemophilia Directors Hepatitis Working Party Hepatitis Associated Commercial Factor VIII 1976 22 September 1977 CBLA0000681_009
(1545) Haemophilia Directors Hepatitis Working Party Hepatitis Associated Commercial Factor VIII 1976 22 September 1977 pp1-2 CBLA0000681_009
(1546) Haemophilia Directors Hepatitis Working Party Hepatitis Associated Commercial Factor VIII 1976 22 September 1977 p3 CBLA0000681_009, Minutes of UK Haemophilia Centre Directors meeting 24 October 1977 p19 PRSE0001002
(1547) Written Statement of Lee Stay para 6 WITN1541001, UKHCDO record of Lee Stay’s registered haemophilia centres 26 October 2018 WITN1541002, NHD record of Lee Stay 26 October 2018 p4 WITN1541004
(1548) Written Statement of Neil Weller para 9 WITN1598005, NHD record of Neil Weller 24 October 2018 WITN1598007
(1549) Written Statement of Ruth Major para 4 WITN2506001, NHD record of Peter Major 27 April 2018 p3 WITN2506002, University Hospital of Wales medical record of Peter Major 27 February 1979 WITN2506003
(1550) Written Statement of Robert Hodgkins para 15 WITN0009001
(1551) Written Statement of Patricia Crowe para 12 WITN1176001. The NHD records show treatment with Hemofil and with cryoprecipitate in 1976 for “Dr Craske’s research work”. NHD record of David Gill 22 August 2018 p3, p6 WITN1176002
(1552) NHD record of Rosamund Cooper 29 November 2017 p3, p7 p10 WITN1168002. The records of testing include “Dr Craske’s research work”. Written Statement of Rosamund Cooper para 27 WITN1168001. Rosamund Cooper Transcript 18 October 2019 pp89-90 INQY1000044
(1553) NHD record of Hadyn Lewis 15 July 2019 p2 WITN2368004
(1554) Letter from Dr Hay to Haydn Lewis 8 August 2006 p1 WITN2368015. Dr Hay added that the issue of consent to receive that concentrate was between Haydn and his centre “and is nothing to do with the database” (which is clearly correct), but that “it would not have been normal to have asked for consent at that time, and this treatment anti-dates the first description of non-A, non-B hepatitis in patients with haemophilia by 12 months.” It may not have been normal to ask for consent at that time in relation to this kind of study, but it does not follow that this was the ethically correct approach. Furthermore, whilst non-A non-B Hepatitis may not have been at the forefront of a treating clinician’s thinking in 1974, any such clinician should have known that at the time of this treatment concentrates might transmit Hepatitis B.
(1555) Jason Evans Transcript 11 June 2021 pp144-145 INQY1000128, Written Statement of Jason Evans para 91 WITN1210008
(1556) Email from Professor Hay to Jason Evans 14 July 2016 and Fletcher et al Non-A non-B hepatitis after transfusion of factor VIII in infrequently treated patients British Medical Journal 10 December 1983 p2, p4 WITN1210029
(1557) Craske et al Commercial factor VIII associated hepatitis, 1974-75, in the United Kingdom: a retrospective survey Journal of Hygiene 1978 HSOC0000009
(1558) Written Statement of Professor Charles Hay para 35, para 26 WITN3289187
(1559) Except that, as explained in the main text above, it is not clear that the Kryobulin study was entirely retrospective.
(1560) This is apparent from records of the National Haemophilia Database. See for example:
(a) in respect of 1974: NHD record of Perry Evans 23 January 2018 p4 WITN1212002, NHD record of Colin Scott 30 August 2018 p4 WITN1595002, NHD record of Neil Weller 24 October 2018 p2 WITN1598007, NHD record of Paul Slater 6 June 2019 p6 WITN3408004, NHD record of Kevin Slater 6 June 2019 p6 WITN3408005, NHD record of Leigh Peach August 2022 p8 WITN7128002
(b) in respect of 1975: NHD record of ANON 10 October 2018 p8 WITN1339002, NHD record of Lee Stay 26 October 2018 p4 WITN1541004, NHD record of Colin Scott 30 August 2018 p4 WITN1595002, NHD record of Perry Evans 23 October 2018 p4 WITN1212002, NHD record of Lee Stay 26 October 2018 p4 WITN1541004, NHD record of John Dinkel 16 October 2018 p3 WITN2855002, NHD record of Paul Slater 6 June 2019 p6 WITN3408004, NHD record of Kevin Slater p6 6 June 2019 WITN3408005, NHD record of Leigh Peach August 2022 p8 WITN7128002
(c) in respect of 1976: NHD record of David Gill 22 August 2018 p6 WITN1176002, NHD record of ANON 10 October 2018 p8 WITN1339002, NHD record of Lee Stay 26 October 2018 p4 WITN1541004, NHD record of John Dinkel 16 October 2018 p3 WITN2855002, NHD record of Victor Budgen 1 July 2019 p5 WITN3315003, NHD record of Lee Stay 26 October 2018 p2 WITN1541002, NHD record of Neil Weller 24 October 2018 p2 WITN1598007
These are examples only from a larger number of similar entries.
(1561) See for instance the comments below by Dr Biggs and Dr Rizza on 22 May 1975. Minutes of Oxford Haemophilia Centre meeting 22 May 1975 p2 OXUH0001103_004
(1562) Minutes of Oxford Haemophilia Centre meeting 22 May 1975 p3 OXUH0001103_004
(1563) Minutes of Haemophilia Centre Directors meeting 18 September 1975 pp9-10 OXUH0003735. The documents make clear that the study was led by Dr Kirk. He introduced the protocol at the meeting and the protocol provided that test results would be sent to him, and the forms to be completed were described as relating to Dr Kirk’s “Hepatitis Survey”. Prospective study: Hepatitis in Haemophilia associated with the use of Factor VIII concentrates September 1975 p3, p9 CBLA0000312
(1564) Prospective study: Hepatitis in Haemophilia associated with the use of Factor VIII concentrates September 1975 pp1-2 CBLA0000312. This study is also discussed in the chapter on Treloar’s. Other centres were invited to participate; it is not clear whether or not they did.
(1565) Although it was said that mild haemophiliacs not on regular replacement therapy would be excluded.
(1566) Prospective study: Hepatitis in Haemophilia associated with the use of Factor VIII concentrates September 1975 p2 CBLA0000312
(1567) It should be noted that if this was desirable (as it was) it should have been a feature of general clinical practice rather than a hallmark of a study. The fact that it was singled out for mention shows that clinicians were aware of risks from giving patients factor concentrates, knew that limiting those patients to batches of the same product would probably be less harmful, yet recognised nonetheless that this measure was not generally being taken.
(1568) Prospective study: Hepatitis in Haemophilia associated with the use of Factor VIII concentrates September 1975 p3 CBLA0000312
(1569) The basis seems to have been “We think this product may create more likelihood of disease in your child (or yourself) than other products – and we want to try it out to see if we are right.” It seems inconceivable that any parent should agree if that were the way the choice had been put to them.
(1570) Letter from Dr Kirk to Dr David Magrath 1 April 1977 CBLA0000590. While Dr Kirk did not say so expressly, given his role in leading the study, it seems likely that his letter referred to results from all of the participating centres. The letter was copied to Drs Biggs, Rizza, Craske and William d’A Maycock. Dr Magrath of the National Institute for Biological Standards and Control replied on 20 April 1977, agreeing with the proposal. Letter from Dr Magrath to Dr Kirk 20 April 1977 HHFT0000925_002
(1571) Letter from Dr Craske to Dr Anthony Aronstam 7 October 1977 HHFT0000925_001. Dr Craske wrote that Dr Kirk was writing up his results and proposed to Dr Aronstam that their collaboration continue: “I think it will be valuable to take serial serum samples from these boys with the idea of trying new tests, particularly those thought to give a good correlation with chronic liver damage.”
(1572) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 14 December 1977 p1 HCDO0000544
(1573) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 14 March 1978 p2 HCDO0000545. The minutes note that it had been decided “to continue the study on transaminase levels after single infusions of Factor VIII”, with Dr Trowell suggesting that collection of samples should take place before infusion and at 3 and 7 days following infusion (rather than 48 hours and 7 days). They also state that the participating centres were Treloar’s (“Alton”), Oxford and Edinburgh, though the 7 November 1978 minutes refer to Treloar’s), Oxford and Newcastle. It is unclear whether this is the same study or two separate studies. Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 7 November 1978 HCDO0000546
(1574) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 7 November 1978 p2 HCDO0000546
(1575) Funding was sought from the DHSS because hepatitis surveillance had hitherto been funded by the MRC and an anonymous private donation to Dr Biggs but this “private hepatitis fund” would be exhausted by August 1978. Letter from Roger Buxton to Dr Maycock 19 April 1978 p3, p10 CBLA0000756. Additional detail was set out in a protocol for the chronic sequelae study, prepared by Dr Craske in February 1978. Study of the Incidence of Chronic Sequelae of Factor VIII – Associated B and Non-B Hepatitis February 1978 OXUH0000316. The protocol was presented at the 14 March 1978 meeting of Haemophilia Centre Directors Hepatitis Working Party, which also discussed the Hepatitis Surveillance study. Dr Peter Jones had expressed interest in a similar project at Newcastle and a study along similar lines might be undertaken at Manchester. The Bournemouth patients treated with Hemofil would be followed from Oxford. Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 14 March 1978 p1 HCDO0000545
(1576) Letter from Roger Buxton to Dr Maycock 19 April 1978 p7 CBLA0000756
(1577) If possible, a third group transfused with other batches of Hemofil would also be studied.
(1578) Letter from Roger Buxton to Dr Maycock 19 April 1978 p8 CBLA0000756
(1579) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 7 November 1978 p1 HCDO0000546. By this time an application had been made to the North West Regional Health Authority for a grant to enable a follow up of chronic liver disease to be undertaken at Manchester. Dr Craske also provided an update on the two studies in an annual report on the work of the Haemophilia Centre Directors Hepatitis Working Party in 1978. Report of Haemophilia Centre Directors Hepatitis Working Party 20 August 1978 CBLA0000831
(1580) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 29 January 1979 p1 HCDO0000547_001. Before confirming funding, the DHSS asked whether informed consent would be obtained from the patients in their study of chronic sequelae and their family members. Dr Craske’s response was: “The physician responsible for the clinical care of haemophiliac patients usually has a very close relationship with his patients and their families. The purpose of this project will be carefully explained to any patient or member of his family and their consent obtained prior to their inclusion in this project.” Letter from R Kingham to Dr Craske 27 July 1978 p2 DHSC0038713_065, Letter from Dr Craske to R Kingham 8 August 1978 p3 DHSC0038713_064
(1581) Study of the Effect of Intravenous Infusions of Factor VIII on Serum Enzyme Levels in Haemophiliacs 19 January 1979 HCDO0000547_002, Draft protocol: An assessment of the value of serum bile acid measurements in the investigation of haemophiliacs thought to have Chronic Hepatitis 19 January 1979 OXUH0000314
(1582) Study of the Effect of Intravenous Infusions of Factor VIII on Serum Enzyme Levels in Haemophiliacs 19 January 1979 p1 HCDO0000547_002
(1583) Draft protocol: An assessment of the value of serum bile acid measurements in the investigation of haemophiliacs thought to have Chronic Hepatitis 19 January 1979 p2 OXUH0000314
(1584) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting p1 HCDO0000549. Additional detail on this and other studies was provided in a report, prepared by Dr Craske, on the work of the Haemophilia Centre Directors’ Working Party in 1979. In relation to the Hepatitis Surveillance study, this recorded that so far 112 out of 122 Oxford patients had been found to have evidence of past infection with Hepatitis B virus. Report of the Haemophilia Centre Directors Hepatitis Working Party 1979 p3 HCDO0000135_023
(1585) Report of the Haemophilia Centre Directors Hepatitis Working Party 1979 p2, p11 HCDO0000135_023
(1586) First Annual Report on Project Number J/S240/78/7 3 December 1979 p7 HCDO0000270_089. Dr Craske also provided an update at the Haemophilia Centre Directors Hepatitis Working Party as noted in Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 20 February 1980 HCDO0000550
(1587) First Annual Report on Project Number J/S240/78/7 3 December 1979 p3, pp19-22 HCDO0000270_089
(1588) Second Annual Report on Project Number J/S240/78/7 HCDO0000270_065, Third Annual Report on Project Number J/S240/78/7 HCDO0000270_054
(1589) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 3 September 1980 pp1-2 HCDO0000553
(1590) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 11 September 1981 pp1-2 PRSE0003474
(1591) Minutes of UK Haemophilia Centre Directors meeting 9 October 1981 pp20-22 DHSC0001312, Haemophilia Centre Directors Hepatitis Working Party Report 1980-1981 24 October 1981 HCDO0000135_017
(1592) Haemophilia Centre Directors Hepatitis Working Party Report 1980-1981 24 October 1981 pp2-3 HCDO0000135_017
(1593) It was recorded that some work on commercial concentrate had been carried out at the Royal Free Hospital, and that an application for a project grant had been made to the MRC “to support a multicentre study in patients coming to operation.” A feasibility study had so far shown that “4 out of 4 patients studied who had had no previous transfusion of concentrate developed non-A, non-B hepatitis.”
(1594) Haemophilia Centre Directors Hepatitis Working Party Report 1980-1981 24 October 1981 pp4-5 HCDO0000135_017
(1595) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 20 February 1980 p1 HCDO0000550. Some of the patients at the Royal Free had undergone a liver biopsy, which “showed changes ranging from acute hepatitis to chronic persistent hepatitis with some suggestion of early progression to chronic active hepatitis. Eight of these patients had had no overt evidence of acute hepatitis.” See below for a discussion of the research undertaken at the Royal Free.
(1596) Prospective Study of the Incidence of Acute and Chronic Hepatitis in Haemophiliacs as a Result of First Exposure to Factor VIII Concentrate or Cryoprecipitate 2 July 1980 pp2-3 HCDO0000552. A study of household contacts was also proposed. Specimens for Hepatitis A, Hepatitis B and liver function tests would be obtained from adult household contacts of haemophilia patients, “subject to informed consent on entry of each patient to the project.” The tests would be repeated at three and six months after the index patient received their transfusion of concentrate, to be increased to monthly for three months if the patient contracted hepatitis.
(1597) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 20 February 1980 pp2-3 HCDO0000553. This preliminary data was also discussed at the 22 September 1980 meeting of Haemophilia Reference Centre Directors. Dr Craske informed the meeting that he was proposing to apply to the DHSS for a further grant for the prospective study of mildly affected patients and patients receiving concentrates for the first time. Minutes of Haemophilia Reference Centre Directors meeting 22 September 1980 p5 HCDO0000406
(1598) Application for a Research Grant for Prospective Study of the Incidence of Acute and Chronic Hepatitis in Haemophiliacs as a Result of First Exposure to Factor VIII Concentrate or Cryoprecipitate 3 February 1981 p2, pp5-6, p8 OXUH0001613_002
(1599) The study also proposed to investigate household contacts prospectively, though it was said that children would only be investigated “where clinically justifiable.” Application for a Research Grant for Prospective Study of the Incidence of Acute and Chronic Hepatitis in Haemophiliacs as a Result of First Exposure to Factor VIII Concentrate or Cryoprecipitate 3 February 1981 p8 OXUH0001613_002
(1600) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 11 September 1981 pp1-2 PRSE0003474. In June 1981, Dr Craske wrote to the Haemophilia Society to seek financial support for a preliminary pilot study at the Oxford Centre to take place because it was expected that it would take around a year to obtain the funding for and arrange a multi-centre study. Letter from Dr Craske to Kenneth Polton 11 June 1981 OXUH0001633_005. An update on the study was also given by Dr Craske at the 14 September 1981 meeting of haemophilia reference centre directors. Minutes of Haemophilia Reference Centre Directors meeting 14 September 1981 p8 LOTH0000012_122
(1601) Minutes of UK Haemophilia Centre Directors meeting 9 October 1981 pp20-21 DHSC0001312
(1602) Minutes of Haemophilia Reference Centre Directors meeting 6 September 1982 p9 HCDO0000410
(1603) The MRC’s refusal was said to be due to its withdrawal from support of projects in the applied clinical research field, and the DHSS was said no longer to have funds available owing to the reallocation of monies to the MRC.
(1604) See the chapter on Pool Sizes.
(1605) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 13 September 1982 p2 HCDO0000556
(1606) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 13 September 1982 pp2-4 HCDO0000556
(1607) Craske A prospective study of the incidence of acute and chronic hepatitis in haemophiliacs as a result of first exposure to factor VIII and IX concentrate or cryoprecipitate 23 September 1982 p1 HCDO0000135_015
(1608) Craske A prospective study of the incidence of acute and chronic hepatitis in haemophiliacs as a result of first exposure to factor VIII and IX concentrate or cryoprecipitate 23 September 1982 p1 HCDO0000135_015. One difference involved greater clarity on the categories of patient who would be considered for the study: these included both patients who would be undergoing “an elective treatment requiring cover with concentrate or cryoprecipitate” and patients seen in the centre who were “seen in the Haemophilia Centre as an emergency and require immediate treatment with concentrate”.
(1609) The proposed procedure was to seek an exemption from a clinical trial certificate by the Licensing Authority, which was said to be less costly and lengthy than obtaining a clinical trial certificate.
(1610) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 19 July 1983 pp1-3 HCDO0000558. Following this, the meeting included a discussion of recent developments concerning AIDS. Professor Bloom and Dr Rizza had already sent the letter at the start of this chapter on 11 January 1982. Letter from Professor Bloom and Dr Rizza to all Haemophilia Centre Directors 11 January 1982 HCDO0000252_042
(1611) UK Haemophilia Hepatitis Working Party Annual Report 1982-1983 28 September 1983 pp3-5 PRSE0001160
(1612) Fletcher et al Non-A non-B hepatitis after transfusion of factor VIII in infrequently treated patients British Medical Journal 10 December 1983 p1 CBLA0001772
(1613) It is right to note that Dr Joan Trowell, who was involved in the study in her capacity as a hepatologist, told the Inquiry that the research studies were all submitted to and approved by the local research ethics committee, and that all patients or parents were given a full verbal explanation and also a written sheet detailing the background and purpose of the study and what would be involved for them. Written Statement of Dr Joan Trowell para 73.1 WITN3740003. However, it is also right to note that Dr Trowell’s involvement came after patients had been treated, when she was assessing their liver function, and her statement makes clear that she had no involvement in decisions regarding haemophilia treatment. No documentation relating to ethics committee approval for this particular study has been found; nor has any form of written sheet describing the study.
(1614) Prior to that he had had no Factor 8 replacement therapy since 1974. Letter from Dr Rizza to David Tibbs 27 October 1971 p1 WITN0599007
(1615) Written Statement of Malcolm Slater paras 18-20, para 32 WITN0599001
(1616) Malcolm and Violet Slater Transcript 29 October 2019 pp51-53 INQY1000046
(1617) Malcolm Slater’s involvement in this study is confirmed by the appearance of his name in a list entitled “Patients included in Prospective Post Transfusion Hepatitis Study Oxford Haemophilia Centre up to November 1981”, where he was described as having “Nil” previous transfusion and the date of his “present transfusion” (ie that relevant to the study) being given as November 1981. Patients included in Prospective Post Transfusion Hepatitis Study OXUH0001610_002
(1618) There is an echo of this in the minutes of the first meeting of the MRC Working Party on AIDS in 1983 which emphasised “the need to ensure that the best use be made of the special combination of suitable patients for study and the clinical, immunological, virological and other expertise available in the United Kingdom.” The UK system for haemophilia treatment and blood product organisation would “allow detailed study of haemophilia associated cases which has not been possible in the USA due to their system of record keeping and organisation.” Minutes of UK Working Party on Transfusion-Associated Hepatitis meeting 27 September 1983p4 CBLA0001749
(1619) Submissions on behalf of core participants represented by Thompsons Scotland 16 December 2022 p765 SUBS0000064
(1620) Letter from Peter Jones to Mr and Mrs Longstaff 12 April 1973 WITN1055172
(1621) Carol Grayson Transcript 8 July 2022 p40 INQY1000223, Written Statement of Carol Grayson paras 567-571 WITN1055004
(1622) Minutes of Haemophilia Centre Directors meeting 20-21 November 1979 p18 CBLA0001028
(1623) But in fact this was a misdiagnosis. Written Statement of ANON para 3 WITN1103001
(1624) Patient medical record 27 November 1978 WITN1103011
(1625) Written Statement of ANON para 10 WITN1103007, Closing Submission of Milners Solicitors 16 December 2022 p114 SUBS0000055
(1626) Letter from Dr Craske to Dr Aronstam 10 May 1979 HHFT0000916_003. A handwritten footnote to the letter says “I realise that the above suggestion does not apply to the LMT boys”, but it was not a suggestion that should have been made in respect of any patients.
(1627) Letter from Dr Aronstam to Dr Craske 14 May 1979 HHFT0000916_002
(1628) Dr Craske wrote back to Dr Aronstam seeking to clarify his suggestion. He said he meant to suggest using NHS concentrate to cover such operations “where other concentrates such as commercial material would be indicated. Some occasions are bound to arise in these circumstances where concentrate is given to a patient who has not had previous concentrate.” Letter from Dr Craske to Dr Aronstam 16 May 1979 HHFT0000916_001
(1629) Professor Christine Lee Lindsay Tribunal Transcript 25 July 2001 p5 LIND0000326
(1630) Professor Edward Tuddenham Transcript 22 October 2020 pp20-22 INQY1000067
(1631) Closing Submission of Milners Solicitors 16 December 2022 pp28-29 SUBS0000055
(1632) Letter from Dr Kernoff to Christopher Bishop 15 March 1983 p2 ARMO0000236
(1633) Four Factor 8 concentrates were used: BPL’s product and concentrate “bought from three manufacturers, the source of plasma in the latter case being exclusively of U.S.A. origin”. NHS Factor 9 concentrate was used. Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p3 HSOC0021398
(1634) Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p2 HSOC0021398
(1635) Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p2 HSOC0021398
(1636) Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p2 HSOC0021398
(1637) Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p2 HSOC0021398
(1638) Emphasis added. Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p3 HSOC0021398
(1639) Professor Lee confirmed that this was the position in her evidence to the Inquiry. Professor Christine Lee Transcript 21 October 2020 pp140-141 INQY1000066
(1640) This is consistent with a grant application co-authored by Dr Kernoff in November 1981. This was not concerned with the study described in the main text of this chapter but with other possible studies which were regarded as “components of routine patient management and surveillance” and as such no application to the ethical practices committee had been made. Application for a Grant to Action Research for the Crippled Child November 1981 p7 WITN0644062
(1641) They received NHS concentrates. A 22-month-old baby treated with NHS Factor 9 concentrate also developed hepatitis.
(1642) Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 pp3-4 HSOC0021398
(1643) The paper did note: “These policies changed over the period of the study, as it became appreciated that the risk of NANB hepatitis after concentrate was very high.” Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p5, p2 HSOC0021398. By way of comment, however, this was a change after the research had begun.
(1644) Kernoff et al High risk of non-A non-B hepatitis after a first exposure to volunteer or commercial clotting factor concentrates: effects of prophylactic immune serum globulin British Journal of Haematology 1985 p5, p2 HSOC0021398
(1645) Professor Christine Lee Transcript 20 October 2020 p16 INQY1000065
(1646) Professor Lee did not, according to her oral evidence to the Inquiry, start work until January 1983, by which time most of the patients studied had been treated: “most of them had been treated actually before I even set foot in the centre”. Professor Christine Lee Transcript 20 October 2020 p8 INQY1000065. Her own work may have been retrospective, in the sense that she was gathering together and analysing the results of the liver function tests, but it does not follow that this was a genuine retrospective study.
(1647) Milners Solicitors submitted that Mark, his brother and his father were, respectively, patients 11, 19 and 18 in the table in the report. Closing Submission of Milners Solicitors 16 December 2022 p29 SUBS0000055. There is no reason to doubt this.
(1648) Written Statement of Kathleen Stewart para 10 WITN1002001
(1649) Closing Submission of Milners Solicitors 16 December 2022 p30 SUBS0000055
(1650) Mark Stewart Transcript 9 October 2019 p68 INQY1000038
(1651) Mark Stewart Transcript 9 October 2019 pp124-141 INQY1000038
(1652) Mark Stewart Transcript 9 October 2019 p98 INQY1000038
(1653) Mark Stewart Transcript 9 October 2019 pp85-86 INQY1000038
(1654) In fact DDAVP was available from around 1978. Expert Report to the Infected Blood Inquiry: Bleeding Disorders and Blood Disorders January 2020 p33 EXPG0000002
(1655) She does not explain why he was so treated, noting that this was before her involvement in his care. Written Statement of Professor Christine Lee para 10 WITN0644004
(1656) Written Statement of Professor Christine Lee para 32 WITN0644004
(1657) Although Professor Lee was involved in this study and sought to defend it, it should be made clear that the treatment decisions were not hers to make, and that the responsibility for those decisions rested with Dr Peter Kernoff. Professor Lee was at that time a research senior registrar who began her work at the Royal Free in January 1983. Professor Christine Lee Transcript 20 October 2020 p3, p19 INQY1000065. It may also be that for some of the patients, because of their particular circumstances, concentrates may exceptionally have been an acceptable treatment: however, this does not detract from the overall conclusion to which the Inquiry is driven.
(1658) Minutes of Haemophilia and Blood Transfusion Working Group meeting 14 November 1983 p1 PRSE0002581. A sense of the patient being used at the will of the clinician for research purposes is clear also from other correspondence. Thus Dr Cash’s letter to Dr Forbes on 28 March 1984 spoke of planning ahead “with regard to getting our product into SHS ‘virgin’ haemophilia a patients … I believe it is important that we obtain from your good self the promised data you have on serial liver function tests in haemophilia A patients who have received only PFC material (and/or local cryoppt.) … The importance of this work, in the context of the proposed heat treated product studies, lies in the fact that we need to know whether your patients can be used as adequate retrospective controls.” Letter from Dr Cash to Dr Forbes 28 March 1984 PRSE0003749. In April 1984 Dr Cash wrote to Dr Robert Crawford at Law Hospital, “most anxious that we look at the incidence of hepatitis and transaminitis in ‘virgin’ haemophiliacs who receive our heat treated factor VIII concentrate.” Letter from Dr Cash to Dr Crawford 25 April 1984 PRSE0000909
(1659) Stirling et al Liver function in Edinburgh haemophiliacs: a five-year follow-up Journal of Clinical Pathology 1981 p2, p5 PRSE0000013. The authors of the study thanked Dr Samuel Davies (Professor Ludlam’s predecessor as centre director) “for permission to study these patients.” It does not appear to have occurred to them to seek permission from the patients for this purpose (or at least inform them that their sera was being tested, analysed and compared). See also a 1986 study of 139 people with haemophilia in Glasgow where the authors thanked Dr Michael Willoughby, formerly of the Royal Hospital for Sick Children, “for permission to study his patients”. Steven et al Liver Dysfunction in Haemophilia Scottish Medical Journal 1986 p5 NHBT0000094_043
(1660) Letter from Dr Lee to Professor Francis Preston 1 July 1996 p1 HCDO0000268_036, Professor Christopher Ludlam Transcript 4 December 2020 pp70-71 INQY1000080
(1661) Professor Christopher Ludlam Transcript 4 December 2020 p65 INQY1000080
(1662) Professor Christopher Ludlam Transcript 4 December 2020 p65 INQY1000080
(1663) For reasons discussed elsewhere in this Report, it should, by this stage, have been appreciated that this was more than a possibility.
(1664) T cells are explained in the chapter on Blood and Transfusion. When there is an infection by HIV, there are more killer (suppressor, “CD8”) cells and less helper (“CD4”) cells, such that the ratio of one to the other changes from that which would be within a normal range.
(1665) Minutes of UK Haemophilia Centre Directors Hepatitis Working Party meeting 19 July 1983 p4 HCDO0000558. On 13 January 1983 the New England Journal of Medicine had carried an article on this topic. Lederman et al Impaired Cell-Mediated Immunity in Patients with Classic Hemophilia New England Journal of Medicine 13 January 1983 PRSE0004470
(1666) See for example Patient medical record 25 March 1984 p60, p63 WITN2232036 and Robert Mackie medical records WITN2190010
(1667) Professor Christopher Ludlam Transcript 4 December 2020 pp75-77 INQY1000080, Professor Christopher Ludlam Penrose Inquiry Transcript 17 June 2011 pp19-20, pp32-98 PRSE0006035
(1668) Gordon Factor VIII Products and Disordered Immune Regulation The Lancet 30 April 1983 CBLA0000059_031
(1669) “Two thirds of our patients had helper/suppressor rations below the lower limit of our normal range”.
(1670) On the basis that there were no known cases of AIDS in the Scottish blood donor population – which rather overlooks the possibility that there might be cases that were not yet known, but were nonetheless present.
(1671) Ludlam et al Disordered Immune Regulation in Haemophiliacs not exposed to commercial Factor VIII The Lancet 28 May 1983 PRSE0001303
(1672) Submissions on behalf of core participants represented by Thompsons Scotland 16 December 2022 p794 SUBS0000064. Professor Ludlam indeed accepted in evidence that “at the start of 1983, early 1983, [he] realised that factor concentrates not only gave rise to a potential risk of non-A, non-B infection and a real risk of HIV infection, but there was a third problem, which was neither hepatitis or HIV, but that was the problem that it might, in any event, separately, give rise to a deterioration in the immune system”. Professor Christopher Ludlam Transcript 4 December 2020 p86-87 INQY1000080
(1673) Carr et al Abnormalities of Circulating Lymphocyte Subsets in Haemophiliacs in an AIDS-free Population The Lancet 30 June 1984 OXUH0002842
(1674) Professor Ludlam confirmed in his evidence to the Inquiry that patients were not advised of the results of what the analysis showed. Professor Christopher Ludlam Transcript 4 December 2020 p78 INQY1000080
(1675) Ludlam et al Human T-Lymphotropic Virus Type III (HTLV-III) Infection in Seronegative Haemophiliacs after Transfusion of Factor VIII The Lancet 3 August 1985 p2 PRSE0004177. At the Penrose Inquiry he described the process in this way: “to make sure that they were correctly carried out in the laboratory, I labelled the blood forms ‘AIDS study’. These would be forms that would be handed to the patients to get their blood taken and, you know, patients could read it. So I must have explained something about AIDS because I wouldn’t write ‘AIDS study’ on a form, which I then either handed to the patient or was sitting in front of the patient while they were having their blood taken, without some explanation.”Professor Christopher Ludlam Penrose Inquiry Transcript 17 June 2011 p19 PRSE0006035. He did not say what he explained: and a reconciliation of this with the evidence given by his patients is dependent on the terms of this – were they, for instance, given to understand that the “study” was simply to confirm that AIDS was an American problem?
(1676) As Professor Ludlam accepted in his evidence. Professor Christopher Ludlam Transcript 4 December 2020 p79 INQY1000080
(1677) As submitted on behalf of the core participants represented by Thompsons: “It seems reasonable to think that if a person was specifically told that blood was being taken from him with a view to carrying out a study of his immune system in relation to the new threat posed by AIDS he would remember and would have reacted with some alarm about the possibility.”Submissions on behalf of core participants represented by Thompsons Scotland 16 December 2022 p775 SUBS0000064
(1678) Professor Christopher Ludlam Transcript 4 December 2020 pp80-81 INQY1000080
(1679) He did, however, accept that “I could have applied for ethical approval for doing the lymphocyte subset”. Professor Christopher Ludlam Transcript 4 December 2020 pp80-81 INQY1000080
(1680) Professor Ludlam sought to suggest that the skin tests were different and required ethical approval, because they were invasive. However this is an artificial distinction: the testing was for the same purpose, namely measurement and analysis of immune function for possible publication.
(1681) Professor Christopher Ludlam Transcript 4 December 2020 pp79-81 INQY1000080. In fairness to Professor Ludlam, he maintains in an answer on his behalf when the criticism was put to him under the Inquiry Rules 2006 that what is said here “appears to be based on a misunderstanding of the nature and practice of clinical research and of the quite separate and distinct practice of publishing data; … [that] even by present day national guidelines, much of the immune investigation undertaken in the 1980s to understand the impact of blood products on patients would not then have been classified as research, but as ‘service evaluation’ and would not have required ethical approval … Nevertheless, Professor Ludlam scrupulously sought ethical approval wherever appropriate, e.g. for the skin tests and HIV virology investigations, (and even on some cases when it was not necessary) Results of immune tests were routinely given to patients when these indicated that a change of therapy was recommended … as drafted, the text reads as if there had been no evidence of the investigation and management of patients with haemophilia in Edinburgh in the early and mid-1980s, let alone the response made by the clinical team to the threat of AIDS … a great deal of evidence was provided but is not referenced.” He (rightly in my view) pointed out he was employed in a teaching hospital, and “although his principal responsibility was the welfare of his patients, he was expected to be curious about and to research aspects of haemophilia and its treatment.” However he also says that patients understood and readily agreed with their supplying an additional small aliquot of blood for further research and storage; that although the results of recently introduced investigations were not necessarily reported to patients this was because the results were uncertain, but anyone who inquired was given the information. He suggests that “evidence provided to the Inquiry has been used selectively to support apparent preconceptions by the Inquiry”, and what is said about Edinburgh research does “a gross disservice to a group of patients and their families who have already suffered considerably and waited too long for their distress to be recognised by the state. What survivors of those with heritable bleeding disorders and their families seek is a balanced and reasoned assessment of the history of this traumatic and challenging period.”
(1682) Case examiner decision form complaint against Professor Christopher Ludlam pp42-43 WITN3365031_001
(1683) Case examiner decision form complaint against Professor Christopher Ludlam p191 WITN3365029_001
(1684) Case examiner decision form complaint against Professor Christopher Ludlam p193 WITN3365029_001
(1685) The Edinburgh Haemophiliac Cohort MRC News MACK0002138. See for example the publication in the Clinical Research section of the British Medical Journal in February 1988 of the results of retrospective testing of stored sera samples, which were compared with the clinical state of the patients to determine whether progression to AIDS or AIDS-related complex correlated with any of the serological measurements. This study was supported by the MRC and Scottish Home and Health Department (“SHHD”), and the authors thanked “the staff of the hepatitis and AIDS reference laboratory, Edinburgh, for making available stored serum samples from the haemophiliac patients.” The patients (who were not thanked) remained unaware. Simmonds et al HIV antigen and antibody detection: variable responses to infection in the Edinburgh haemophilic cohort British Medical Journal 27 February 1988 PRSE0000836. There is evidence that blood was also taken from family members and used for research purposes, the nature of which remains unclear, with no explanation being given as to the purpose of the blood testing: see the evidence of Alice Mackie. Alice Mackie Transcript 4 July 2019 pp55-56 INQY1000027. It is conceivable that this was pursuant to the proposal, in a letter from Dr Forbes, asking centre directors if they wished to “participate in a study to assess the anti-HTLVIII status of household and sexual contacts of haemophilic patients.” Dr Forbes’ letter cautioned that it “may” be important to discuss the nature of the study and the possible implications of results with families before seeking their permission to participate and that it “might” be appropriate to seek approval from the local ethical committee. Letter from Dr Forbes to Director 7 October 1985 HCDO0000019_023. It should be noted that Dr Peter Jones considered the proposed questionnaire for this study, which was drawn up by Dr Ludlam, was unethical and could be construed as a breach of human rights and that central collection of this data could do “untold harm.” Letter from Peter Jones to Dr Forbes 22 October 1985 HCDO0000271_088
(1686) Froebel Immunological abnormalities in haemophilia: are they caused by American factor VIII concentrate? British Medical Journal 15 October 1983 p1 PRSE0001121
(1687) Professor Lowe was not at that stage directly involved in the study. Professor Lowe Transcript 11 December 2020 p44 INQY1000085
(1688) Professor Lowe did not know as a matter of fact what was said to patients (if anything) but agreed as a matter of principle that they should have been told of their prospective involvement. Professor Gordon Lowe Transcript 11 December 2020 pp46-47 INQY1000085
(1689) Professor Charles Forbes Penrose Inquiry Transcript 15 June 2011 p110 PRSE0006033
(1690) Professor Charles Forbes Penrose Inquiry Transcript 15 June 2011 p111 PRSE0006033
(1691) Froebel Immunological abnormalities in haemophilia: are they caused by American factor VIII concentrate? British Medical Journal 15 October 1983 p2 PRSE0001121
(1692) Melbye et al HTLV-III seropositivity in European haemophiliacs exposed to Factor VIII concentrate imported from the USA The Lancet 29 December 1984 PRSE0001630
(1693) Letter from Dr Froebel to Dr Perry 29 October 1984 PRSE0000259, Professor Gordon Lowe Transcript 10 December 2020 p23, pp65-67 INQY1000084
(1694) This patient had been admitted to Glasgow Royal Infirmary in mid 1984 (around May and/or July). Professor Gordon Lowe Transcript 10 December 2020 p14 INQY1000084. Patients at the Glasgow Royal Infirmary were invited for HIV testing in the course of 1985. Professor Gordon Lowe Transcript 10 December 2020 pp24-97 INQY1000084
(1695) HP011 was a pharmacokinetic study comparing HPVIII with the existing SNBTS product (Z8); HP012 was a clinical trial to assess the tolerability of HPVIII in non-HIV-infected patients with Haemophilia A and was a PUP study; HP013 was a clinical trial to assess the tolerability of HPVIII in patients with Haemophilia A who were HIV positive; HP014 was a clinical trial comparing HPVIII with Z8 in the treatment of patients with Haemophilia A. The clinical trial protocols for these trials were dated November 1991 and are at: SNBTS pharmacokinetic study HP011 protocol 13 January 1992 SBTS0004605_005, SNBTS clinical trial HP012 protocol 25 November 1991 SCGV0000220_005, SNBTS clinical trial HP013 protocol 25 November 1991 SCGV0000220_004, SNBTS clinical trial HP014 protocol 28 November 1991 SCGV0000219_017. A protocol for HP016, assessing the tolerability of HPVIII in patients with Haemophilia A, was produced in the second half of 1992: SNBTS clinical trial HP016 protocol 14 September 1992 SCGV0000220_145, SNBTS clinical trial HP016 amended protocol 30 November 1992 SBTS0004605_055. These clinical trials were approved by the Medicines Control Agency, and by the independent ethics committees geographically based around Scotland and Northern Ireland in respect of each Principal Investigator/Haemophilia Centre. An independent data safety monitoring committee was also established with Sir Patrick Forrest as its chair.
(1696) HP014 required that the patients should be at least 12 years of age; the others had no age exclusion. SNBTS clinical trial HP014 protocol 28 November 1991 p5 SCGV0000219_017
(1697) SNBTS clinical trial HP012 protocol 25 November 1991 pp23-25 SCGV0000220_005, SNBTS clinical trial HP013 protocol 25 November 1991 pp17-19 SCGV0000220_004. Solvent detergent viral inactivation destroys viruses with a lipid envelope, because lipids are dissolved by detergent. For viruses with no such envelope other means had to be selected. Parvovirus was known to have no lipid (fatty) coating.
(1698) SNBTS clinical trial HP016 protocol 14 September 1992 pp15-16 SCGV0000220_145
(1699) SNBTS clinical trial certificate exemption for SNBTS high potency Factor VIII concentrate application November 1991 p28 JGSM0000006_120. See the further discussion regarding enveloped viruses: evidence was referred to which suggested “a high margin of safety for the SNBTS process using a virus inactivation method which has previously been shown to inactivate the major viruses potentially transmitted by plasma products ie. HIV-1, Hepatitis B and Hepatitis C.” SNBTS clinical trial certificate exemption for SNBTS high potency Factor VIII concentrate application November 1991 pp54-57 JGSM0000006_120
(1700) The unpublished data relating to these seroconversions was prepared for the Coagulation Factor Working Party meeting in November 1994. SNBTS Product Service Department B19 Parovirus Seroconversions on High Purity Factor VIII Trials p1 LOTH0000051_005. This provoked “interest in whether those B19 seroconversions noted in Liberate recipients … could be linked to B19 titre in the product.” Minutes of Coagulation Factor Working Party meeting 3 November 1994 p3 LOTH0000051_002. The data was published in the interim and final reports. SNBTS Report on Clinical Trials to Assess the Efficacy and Tolerability of a New High Purity Factor VIII Concentrate (Liberate) in Patients With Haemophilia A 1 February 1995 p75, p216 SBTS0003795_062
(1701) Minutes of Annual Haemophilia, SNBTS Directors and SOHHD meeting 12 May 1994 p2 SBTS0003825_008. Haemophilia directors were “particularly hopeful that viral inactivation step[s] to eliminate these notes might become available.”
(1702) Hydrops fetalis is life-threatening: it occurs when either in an unborn or newborn baby large amounts of fluid build up in a baby’s tissue and organs, causing extensive swelling.
(1703) Joint disease.
(1704) Written Statement of Professor Christopher Ludlam pp52-53 WITN3428001. He added that the infection was difficult to study in adults with haemophilia, because many children get infected in their normal environment.
(1705) Written Statement of ANON para 6 WITN2239001
(1706) The horror of watching his son die of AIDS and the devastation wrought upon the family was powerfully described in Mr AB’s written and oral evidence to the Inquiry. Written Statement of ANON paras 27-33 WITN2239001, ANON Transcript 11 July 2019 pp30-39 INQY1000032
(1707) Written Statement of ANON para 25 WITN2239001
(1708) ANON Transcript 11 July 2019 pp39-41 INQY1000032
(1709) Written Statement of ANON para 7 WITN2239012
(1710) Written Statement of ANON para 11 WITN2239012
(1711) Written Statement of ANON para 5 WITN2239012
(1712) Written Statement of ANON para 11 WITN2239012
(1713) See Written Statement of Dr James McMenamin WITN3495001, Written Statement of Dr James McMenamin WITN3495003, Written Statement of Dr Dermot Kennedy WITN3363001 and Written Statement of Dr Dermot Kennedy WITN3363004
(1714) Written Statement of ANON paras 7-9 WITN2239013
(1715) Written Submission of ANON 16 December 2022 SUBS0000066
(1716) The failure here is a systemic, rather than personal one.
(1717) Written Statement of ANON para 16 WITN2239012
(1718) Though not decided.
(1719) This will be the case in most congenital conditions such as haemophilia, for treatment usually begins for the first time after birth. It may be then, as a very young child, that the results of a particular treatment can be seen most clearly, rather than have to be disentangled from outcomes in adults who have had several years of various different treatments which may cloud the picture.
(1720) It should be emphasised that this is not a finding of legal liability, for that is a finding which it is beyond the powers of the Inquiry to make.
(1721) See the chapter on Treloar’s.
(1722) Letter from the warden of Lord Mayor Treloar College to Mr and Mrs Cuffley September 1967 p2 WITN7547002
(1723) Minutes of Wessex Regional Health Authority meeting 28 March 1979 p1 HHFT0001066_002
(1724) Submissions on behalf of core participants represented by Thompsons Scotland 16 December 2022 p767 SUBS0000064
(1725) Submissions on behalf of core participants represented by Thompsons Scotland 16 December 2022 p767 SUBS0000064
(1726) Note from Counsel to the Infected Blood Inquiry on the number of children with bleeding disorders who were infected with HIV November 2022 INQY0000387
(1727) Some died before Hepatitis C testing was a possibility, but it is inevitable that those children infected with HIV from blood products would also have been infected with Hepatitis C.
(1728) The Haemophilia Society The Bulletin 1990 No1 March 1990 p4 HCDO0000276_001. The oral evidence of Dr Boulton, who was in practice the director of the Royal Liverpool Centre from 1975 to 1980 (Professor Bellingham had nominal responsibility but in practice delegated haemophilia care to Dr Boulton), was that a boy would transition from Alder Hey to the Royal Liverpool between the ages of 14 and 18. Dr Frank Boulton Transcript 4 February 2022 pp13-14 INQY1000181
(1729) The focus of his work was paediatric oncology. Counsel Presentation on Smaller Haemophilia Centres: Alder Hey, Liverpool June 2021 para 2 INQY0000260
(1730) Annual Returns for Alder Hey Children’s Hospital 1977 HCDO0001177. Dr Boulton explained to the Inquiry that the care of boys with haemophilia was shared with Dr Martin. Written Statement of Dr Frank Boulton 26 October 2021 para 14 WITN3456002, Dr Frank Boulton Transcript 4 February 2022 pp13-14 INQY1000181. The position regarding the supply of concentrates by Liverpool to Alder Hey in the 1980s, after Dr Boulton left, may have been the same, although the evidence is less clear. In February 1985, Dr Martin wrote to BPL stating that “we normally receive our factor VIII via the adult centre at the Royal Liverpool Hospital, whose director is Dr [B] A McVerry.” Letter from Dr Martin to Dr Snape 21 February 1985 BPLL0010612. Dr Lynne Ball, who became the director at Alder Hey in 1989, also understood the position to be that products were supplied by the Royal Liverpool Adult Centre. Written Statement of Dr Lynne Ball 21 March 2021 paras 6(b) and 9 WITN4739001. However, Dr McVerry, who was the director of the Royal Liverpool Centre between 1980 and 1985, said in a statement to the Inquiry that he had no involvement with Alder Hey and that it was highly unlikely that the Royal Liverpool Hospital supplied it with blood products. Written Statement of Dr Bernard McVerry paras 22.1 and 30 WITN3502007. According to Dr Martin (in a draft statement prepared in around 1992) the purchase of commercial Factor 8 concentrates was undertaken via the Royal Liverpool Hospital, in part because the district health authority was able to get a better price per unit by buying in bulk, and supplied by the Royal Liverpool’s haemophilia ward to Alder Hey.
(1731) The main return shows treatment with cryoprecipitate (48,030 units), NHS Factor 8 (the figure is unclear but would appear to be around 46,000 units) and Factorate (24 bottles; the number of units is not given) but the return provided to the UKHCDO’s Home Therapy Working Party states that there were two Haemophilia A patients on home therapy, who received 38,490 units of Factorate and 23,054 units of Koate. The Koate is not accounted for on the main return. Annual Returns for Alder Hey Children’s Hospital 1978 p1, p13 HCDO0001274
(1732) 27,790 units of cryoprecipitate, 37,500 units of NHS Factor 8 and 14,000 units of Factorate. Annual Returns for Alder Hey Children’s Hospital 1979 HCDO0001343
(1733) 114 packs of cryoprecipitate, 136 bottles of NHS Factor 8 and 268 bottles of Factorate, all in hospital with no home treatment. Annual Returns for Alder Hey Children’s Hospital 1980 HCDO0001439
(1734) The return is confusing. It shows the use of 4 packs of cryoprecipitate, 386 bottles of NHS Factor 8 and 29 bottles of Factorate, all in hospital. It gives no figures for home treatment use, stating instead that all products for home treatment were supplied by the Royal Liverpool Hospital. It is clear therefore that there was some kind of home treatment programme but that Dr Martin did not record on the returns what products were used or in what quantities. Annual Returns for Alder Hey Children’s Hospital 1981 HCDO0001541
(1735) 16 packs of cryoprecipitate (equating to 1,120 units), 155 bottles of NHS Factor 8 (38,750 units) and 647 bottles of Factorate (161,750 units) are recorded, all of which was provided in hospital; there is no record of what may have been used for home treatment. Annual Returns for Alder Hey Children’s Hospital 1982 HCDO0001639
(1736) It used 11 packs of cryoprecipitate, 218 bottles of NHS Factor 8 (noted to equate to 54,500 units of NHS Factor 8) and 749 bottles of Factorate (representing 187,250 units), all in hospital. The return once more noted that home treatment products were not supplied by Alder Hey. Annual Returns for Alder Hey Children’s Hospital 1983 HCDO0001739
(1737) It used 339 bottles of NHS Factor 8 and 352 bottles of Factorate. Home treatment products were again said to be supplied by the Royal Liverpool Hospital. Annual Returns for Alder Hey Children’s Hospital 1984 HCDO0001831
(1738) The return recorded 28,750 units of NHS Factor 8 (of which 2,500 units were at home and the remainder in hospital), 14,250 units of Factorate in hospital and 9,000 of unspecified other human Factor 8. Annual Returns for Alder Hey Children’s Hospital 1986 HCDO0002021
(1739) Stephen was just nine years old when he died, Brian was sixteen. The Inquiry heard the powerful and moving evidence of Stephen’s and Brian’s mother Susan on 29 September 2022. Panel about the experiences of parents whose children were infected at Alder Hey Children’s Hospital Transcript 29 September 2022 INQY1000249
(1740) He was also treated on five occasions with NHS Factor 8 concentrate. His first ever treatment was with US concentrate; Dr Savidge noted “There is no documentation at that time to indicate that the treatment alternatives with single donor pool cryoprecipitate or NHS factor VIII concentrates were ever entertained.” Medical Report and Opinion of Dr Savidge 26 March 1992 pp1-2 DHSC0043164_068
(1741) Seven treatments with US commercial concentrates and two with NHS in 1983, four treatments with US and four with NHS in 1984. Medical Report and Opinion of Dr Savidge 26 March 1992 p2 DHSC0043164_068
(1742) Dr Savidge explained that “This unheated material was batch no. Y88908 which had not been administered to the patient before, and was not used subsequently. To my knowledge, at other Centres, much of this unheated batch had been returned to the manufacturer, who subsequently heated the product in one of their facilities in W. Germany.” Medical Report and Opinion of Dr Savidge 26 March 1992 p2 DHSC0043164_068. A DHSS analysis of legal claims acknowledges that “it would certainly be indefensible if any of the commercial concentrate given in 1985 was unheat-treated.” Report on Medical Negligence Cases 15 July 1991 p10 DHSC0045373_118
(1743) Medical Report and Opinion of Dr Savidge 26 March 1992 pp4-6 DHSC0043164_068
(1744) Medical Report and Opinion of Dr Savidge 26 March 1992 pp7-8 DHSC0043164_068
(1745) Hospital note on haemophilia treatment sheet WITN1267002
(1746) Medical Report by Dr Christopher Ludlam 6 April 1992 p9 DHSC0043164_067
(1747) Dr Martin also said that he did not lay down a particular treatment plan to the medical staff and placed no restrictions on any member of staff wishing to use cryoprecipitate; indeed, it was not even his practice to give new members of his team a talk in relation to haemophilia care – or, it would appear, any guidance whatsoever. Statement from Dr Martin on treatment of people with haemophilia pp2-3 DHSC0043164_070. The Inquiry has been unable to locate a copy of Dr McVerry’s statement.
(1748) Statement from Dr Martin on treatment of people with haemophilia p3 DHSC0043164_070
(1749) Statement from Dr Martin on treatment of people with haemophilia p3 DHSC0043164_070
(1750) Statement from Dr Martin on treatment of people with haemophilia p6 DHSC0043164_070
(1751) He claimed that this was because of his other clinical responsibilities at Alder Hey. Statement from Dr Martin on treatment of people with haemophilia p3 DHSC0043164_070
(1752) Report on Medical Negligence Cases 15 July 1991 DHSC0045373_118; HIV Medical Negligence Cases Status Report 5 September 1991 DHSC0045721_051
(1753) In relation to this patient, the DHSS document states that “NHS concentrate should have been preferred to commercial from about mid-1983 but supplies were inadequate to adhere entirely to this counsel of perfection.” Report on Medical Negligence Cases 15 July 1991 p19 DHSC0045373_118. To suggest that the avoidance of commercial concentrate in the treatment of children from mid 1983 was a “counsel of perfection” is quite wrong.
(1754) Report on Medical Negligence Cases 15 July 1991 p24 DHSC0045373_118
(1755) In relation to the elective surgery, although Dr Martin had said that he “did his best to discourage the operation, he did not do so in the specific context of the risk of viral infection or the risk of infection of AIDS and the parents were not warned in relation to these aspects.” HIV Medical Negligence Cases Status Report 5 September 1991 pp2-3 DHSC0045721_051
(1756) HIV Medical Negligence Cases Status Report 5 September 1991 p3 DHSC0045721_051
(1757) The child died in 1989. HIV Medical Negligence Cases Status Report 5 September 1991 p3 DHSC0045721_051
(1758) HIV Medical Negligence Cases Status Report 5 September 1991 p4 DHSC0045721_051
(1759) The case was “therefore difficult to defend.” HIV Medical Negligence Cases Status Report 5 September 1991 p5 DHSC0045721_051
(1760) Medical Report on Anon 6 April 1992 p4 DHSC0044718_072
(1761) The same report notes that “The treating doctor, Dr. Martin, will not make a good witness.” Status Report on Medical Negligence Cases 26 June 1992 p22 DHSC0043164_002
(1762) Statement from Dr Martin on treatment of people with haemophilia p8 DHSC0043164_070
(1763) Written Statement of Dr Lynne Ball 21 March 2021 para 15 WITN4739001. Dr Martin regarded it as “of limited value, and difficult to use with small children.” He made a conscious decision not to use it, although it was available at the hospital, because “we had an established form of treatment in place which I felt, at the time, to be safe and there was no reason to change my treatment methods.” Statement from Dr Martin on treatment of people with haemophilia pp3-4 DHSC0043164_070
(1764) Written Statement of Dr Lynne Ball 21 March 2021 p14 WITN4739001
(1765) Written Statement of Dr Lynne Ball 21 March 2021 p14 WITN4739001
(1766) NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 26 August 2022 p11 WITN3826020, Review of Main UK Cohorts of HIV Seropositive Cases 13 July 1987 p16 MRCO0000388_188, Written Statement of Dr Lynne Ball 21 March 2021 p13 WITN4739001
(1767) Written Statement of Dr Lynne Ball 21 March 2021 p13 WITN4739001
(1768) According to Dr Hill. Statement from Dr Hill 11 April 1992 para 1 OXUH0000005_011, Minutes of West Midlands Regional Health Authority Working Party meeting 18 December 1975 p5 SHIN0000045
(1769) Statement from Dr Hill 11 April 1992 p1 OXUH0000005_011
(1770) Dr Hill divided his time between the adult centre at QEH and BCH.
(1771) Written Statement of Professor Frank Hill 28 May 2019 para 5 WITN3087001
(1772) See the chapter on Hepatitis Risks 1970 and After.
(1773) Dr Stuart agreed with Dr Hill as to the hepatitis risk, but said that “in case of doubt”he would prefer to use cryoprecipitate for children rather than commercial concentrates. However, as the annual returns show, the region did not introduce a system of prioritising NHS concentrate for children and BCH/Dr Hill did not use cryoprecipitate in preference to commercial concentrates. Minutes of West Midlands Regional Health Authority Working Party 22 November 1976 p2 SHIN0000043
(1774) 615,000 units of cryoprecipitate were recorded, 156,138 units of Factorate and 11,130 units of Kryobulin. Annual Returns for Birmingham Children’s Hospital 1977 HCDO0001138
(1775) Agenda for Working Party on the Treatment of Haemophiliacs meeting 14 May 1979 p5 CBLA0000940
(1776) The 1978 return did not calculate units of cryoprecipitate but gave the number of bags as 4,541; the previous year had been 7,695. In contrast with 1977, NHS concentrate was used fairly substantially (194,510 units), commercial concentrate usage had increased to 287,198 units (of Factorate). Annual Returns for Birmingham Children’s Hospital 1978 HCDO0001232
(1777) Agenda for Working Party on the Treatment of Haemophiliacs meeting 14 May 1979 p7 CBLA0000940
(1778) Cryoprecipitate was still in use (3,325 bags), as was NHS concentrate (171,900 units) but Factorate was the predominant product (500,221 units). Annual Returns for Birmingham Children’s Hospital 1979 HCDO0001301
(1779) 1979 saw cryoprecipitate usage fall, some NHS concentrate was used (138,678) for both home and hospital treatment, but Factorate usage rose to 1,118,695 units for home and hospital treatment. Annual Returns for Birmingham Children’s Hospital 1980 HCDO0001395
(1780) Cryoprecipitate usage was broadly similar to the previous year: 246,506 units of NHS concentrate were used; 1,164,819 units of commercial (Factorate). Annual Returns for Birmingham Children’s Hospital 1981 HCDO0001494
(1781) Only 59,640 units of cryoprecipitate were used, compared to 222,681 units of NHS concentrate and 1,217,594 units of Factorate. Annual Returns for Birmingham Children’s Hospital 1982 HCDO0001597. BCH’s exclusive use of Factorate was well known at the time: a visit from a Cutter representative to Dr Hill in February 1981 observed that “Most of the West Midlands R.H.A. have been firm Armour accounts for about four years. Dr. Hill’s attitude was therefore one of ‘friendly hostility’.” Memo from Barry Barber to Brian Dyos 27 February 1981 BAYP0000019_024
(1782) Only 53,340 units of cryoprecipitate were used. NHS concentrate usage declined to 140,405 units, whilst commercial usage (all Factorate) increased to 1,395,101 units. Annual Returns for Birmingham Children’s Hospital 1983 HCDO0001693
(1783) 78,330 units of cryoprecipitate were used and 405,188 units of NHS concentrate. Annual Returns for Birmingham Children’s Hospital 1984 HCDO0001790
(1784) Although there was a rise in outpatient attendances in 1983 and 1984. Report on case for an additional Haemophilia Sister 21 October 1985 UBFT0000254
(1785) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 23 November 1981 p2 SHIN0000033
(1786) Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 28 June 1982 p3 SHIN0000032. By the time of the next meeting of the Working Party on 6 December 1982 there was reported to be an excess of cryoprecipitate. This was due to overstocking in anticipation of the reduction in NHS Factor 8 at BPL and the fact that, rather than reverting to cryoprecipitate, the centres had purchased commercial Factor 8. Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs meeting 6 December 1982 p2 SHIN0000031
(1787) Statement from Dr Hill 11 April 1992 p3 OXUH0000005_011
(1788) Notes of meeting with Immuno 24 January 1983 PRSE0002647
(1789) Letter from Dr Mounir Wassef to Dr Hill 29 June 1983 TREL0000335_020
(1790) This is a report produced for the purposes of a claim which was brought on behalf of the child, Jonathan Buggins. Medical Report and Opinion regarding the treatment of Jonathan Buggins 2 June 1992 p9 WITN1021004. A report was also produced by Professor Ingram, which explained that cryoprecipitate should have been used for treatment; that if on any occasion cryoprecipitate was not available, NHS product should have been used; that there was no evidence within the records of any consideration being given to prioritising the child for NHS concentrate; and that on any occasion when it was not possible to supply a safer product than commercial concentrate consideration should have been given, but was not, to the alternative of providing no product whatsoever. Professor Ingram also criticised the failure to use tranexamic acid. Short medico-legal report by Professor G Ingram OXUH0000005_015
(1791) The basis for Dr Savidge’s assertion that cryoprecipitate treatment of infants was the recommended policy of the hospital is not entirely clear, but Dr Hill, writing in 1992, suggested that “Patients of younger age prior to training for home therapy” were likely to be treated “more frequently”with cryoprecipitate. Treatment of infants “more frequently”with cryoprecipitate nonetheless suggests that such infants were treated at least some of the time with concentrates – and at BCH such treatment was likely to be with Factorate. Newly diagnosed infants would, he said, be treated “initially with cryoprecipitate”, which again suggests that they would in due course move to treatment with concentrates. Statement from Dr Hill 11 April 1992 p2, p4 OXUH0000005_011. Medical Report and Opinion regarding the treatment of Jonathan Buggins 2 June 1992 pp2-3 WITN1021004
(1792) Medical Report and Opinion regarding the treatment of Jonathan Buggins 2 June 1992 p7 WITN1021004
(1793) Medical Report and Opinion regarding the treatment of Jonathan Buggins 2 June 1992 p8 WITN1021004
(1794) See for example Patient medical record for Anon WITN1103010; Patient medical record for Anon WITN1103011, Professor Ian Franklin Transcript 27 October 2020 pp48-50 INQY1000068
(1795) Dr Hill claimed that cryoprecipitate was not appropriate for use at home because it had to be stored in a deep freeze and because of the risk of anaphylaxis occurring without immediate medical help. Statement from Dr Hill 11 April 1992 p5 OXUH0000005_011. However, it is clear from evidence available to the Inquiry that cryoprecipitate, whilst undoubtedly less convenient to use at home than concentrates, could appropriately and safely be used for home treatment, as it was at a number of centres in the 1970s.
(1796) Statement from Dr Hill 11 April 1992 p2 OXUH00000005_011. Dr Hill claimed to have set up a priority system for the use of the limited supplies of NHS concentrate that he had available: treating patients with NHS Factor 8 if they suffered an anaphylactic reaction to commercial concentrate, or for the treatment of individual patients who had received little or no commercial concentrate in the past and particularly mildly affected patients. Statement from Dr Hill 11 April 1992 p9 OXUH0000005_011. However, it is clear that most patients were given commercial concentrate from an early stage, at least if they were receiving home treatment, and it might be said that Dr Hill’s attitude was that once a child had received commercial concentrate they might as well go on receiving it.
(1797) Statement from Dr Hill 11 April 1992 p5 OXUH00000005_011
(1798) AIDS: transfusion patients may be at risk New Scientist 3 February 1983 WITN1213005
(1799) Andrew Evans Transcript 10 May 2019 pp4-7 INQY1000008
(1800) Minutes of West Midlands Regional Health Authority meeting 17 December 1984 pp1-2 SHIN0000026_002. On 15 February 1985 the Working Party held another meeting at which they noted that the interim guidance drawn up at the meeting on 17 December 1984 was at odds with the UKHCDO recommendations in the AIDS Advisory Document of 14 December 1984. A new treatment strategy was therefore recommended: DDAVP should be used in mild Haemophilia A patients and those with von Willebrand disorder if possible; for Haemophilia A patients not previously exposed to Factor 8 concentrate and children, cryoprecipitate or heat-treated NHS Factor 8 if possible; for patients with severe or moderate haemophilia previously treated with Factor 8, heat-treated NHS Factor 8 if available or heat-treated commercial material; for those with mild Haemophilia B fresh frozen plasma if possible, otherwise NHS Factor 9; for patients not previously exposed to concentrate, fresh frozen plasma (or NHS Factor 9 concentrate if essential); for patients with severe and moderate Haemophilia B previously exposed to concentrate, the recommendation was to continue to use NHS Factor 9. Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs 15 February 1985 p2 SHIN0000025
(1801) Annual Returns for Birmingham Children’s Hospital 1985 HCDO0001881. Annual Returns for Birmingham Children’s Hospital 1986 HCDO0001977. However, it is apparent from the discussion at an extraordinary meeting of the West Midlands Working Party on 13 October 1986 that Armour had been the sole supplier of heat-treated Factor 8 to the region up to the point at which it was discovered that previously HIV negative children at BCH treated with heated Factorate had been infected with HIV. Minutes of West Midlands Regional Health Authority Working Party on the Treatment of Haemophiliacs extraordinary meeting 13 October 1986 pp1-2 SHIN0000019
(1802) “Dear Frank … I have paid our first 1985 donation to your research fund to the Finance Department of the Central Birmingham Health Authority.”Letter from Robert Christie to Dr Hill 27 March 1985 ARMO0000370. There is no suggestion that Dr Hill benefited personally from the donation – it was paid to the health authority – but the receipt of donations for research from a particular pharmaceutical company may well influence a clinician in the choice of product.
(1803) The exclamation mark is Robert Christie’s. Dr Hill was said to be now testing parents and siblings of haemophilia patients. Memo from Robert Christie 30 April 1985 p2 ARMO0000375
(1804) Central Birmingham Health Authority, Consequences of AIDS to Haemophilia Services April 1986 p2 UBFT0000252
(1805) Memo from Robert Christie 29 September 1986 ARMO0000585. See the chapter on Viral Inactivation. Robert Christie had a follow-up meeting with Dr Hill in October 1986, in which detailed information about each patient (although not necessarily their names) was shared with Armour. Robert Christie’s internal memo following the meeting recorded the following: “Dr Hill was asked why he thought the boys had not sero-converted earlier. Although both boys were multiply treated, Number 2 was treated with NHS only during the period of maximum risk. Number 1 – just lucky as he had only moderate amount of treatment? Dr Hill thinks that Number 1 is probably product-related and Number 2 possibly, but evidence is not so good.” Memo (incomplete) from Robert Christie to Dr P A Harris 14 October 1986 ARMO0000612. It is unclear why it was thought appropriate to refer to a child who had been infected with HIV from their treatment as “lucky”, simply because they had been infected by heat-treated product rather than the unheated product.
(1806) Memo from Robert Christie to Dr Peter Harris 13 January 1987 CGRA0000532
(1807) The Nursing Times Home treatment for children with haemophilia 23 September 1981 p1 HSOC0002894. There was a smaller centre at Booth Hall Children’s Hospital, where Dr Evans was also the director. It was sometimes described as an associate centre of RMCH and the annual returns for each were generally filed together. Small numbers of patients were treated each year (by way of example in 1982 three patients with Haemophilia A and one with Haemophilia B were treated). See Counsel Presentation on Smaller Haemophilia Centres Booth Hall Children’s Hospital June 2021 INQY0000252 and Counsel Presentation on Smaller Haemophilia Centres Transcript 16 June 2021pp61-65 INQY1000129
(1808) Letter from Dr Evans to Professor Blackburn 27 January 1977 OXUH0003765_024
(1809) Whilst cryoprecipitate remained the main treatment for von Willebrand disorder during this period, there was some use of commercial concentrate in the late 1970s. It is not possible to discern from the annual returns why this was the case.
(1810) Annual Returns for Royal Manchester Children’s Hospital 1976 HCDO0001098
(1811) Annual Returns for Royal Manchester Children’s Hospital 1979 HCDO0001349
(1812) Annual Returns for Royal Manchester Children’s Hospital 1980 HCDO0001446
(1813) Annual Returns for Royal Manchester Children’s Hospital 1981 HCDO0001547, Annual Returns for Royal Manchester Children’s Hospital 1982 HCDO0001646. The treatment of Alistair Bennett, who was under the care of Royal Manchester Children’s Hospital from when he was a baby in 1972, illustrates this shift. Initially treated with concentrates, he started to receive Factor 8 concentrates in the late 1970s. He was treated exclusively with NHS concentrates, but by autumn 1982 he was being treated with commercial concentrates. He was infected with HIV and died in 1995 at the age of 22. Alison Bennett Transcript 2 July 2019 pp13-17, p31 INQY1000025
(1814) Cryoprecipitate was, however, being used for home treatment in the 1970s. Written Statement of Alison Bennett 22 November 2018 para 2.1 WITN0553001, Annual Returns for Royal Manchester Children’s Hospital 1977 p8 HCDO0001183
(1815) Letter from Dr Evans to Dr J Clark 15 September 1982 NHBT0059262_006
(1816) Haemophilia Society Haemophilia Today Seminar Report Manchester 1978 January 1979 p5 PRSE0000421, Salford Area Health Authority (Teaching) Introduction to Haemophilia May 1979p5 HSOC0022546
(1817) See two May 1981 letters from Dr Evans to Dr Aronstam, in which the former wrote that “I do not think it matters very much which product you use so long as the boys realise that they may need to change their concentrate from time to time”, “I think it sensible for the boys to realise that the product may need to be changed from time to time and not to become too dependent on one manufacturer’s concentrates.”Letter from Dr Evans to Dr Aronstam 12 May 1981 TREL0000108_022, Letter from Dr Evans to Dr Aronstam 12 May 1981 TREL0000299_010. See also by way of example Annual Returns for Royal Manchester Children’s Hospital 1977 p3 HCDO0001183, Annual Returns for Royal Manchester Children’s Hospital 1980 p4 HCDO0001446, Annual Returns for Royal Manchester Children’s Hospital 1982 p4 HCDO0001646
(1818) Annual Returns for Royal Manchester Children’s Hospital 1983 HCDO0001744, Annual Returns for Royal Manchester Children’s Hospital 1984 HCDO0001837
(1819) He attended the September 1980 meeting in Glasgow (at which he raised a question which led to a discussion about “the hepatitis risk with all concentrates”) which was followed by the symposium on Unresolved Problems in Haemophilia. Minutes of UK Haemophilia Centre Directors meeting 30 September 1980 p14 PRSE0003946. He did not attend the October 1983 UKHCDO meeting at which AIDS was discussed but was represented by Dr Stevens.
(1820) Letter from Dr Aronstam to Dr Evans 7 July 1983 TREL0000248_095
(1821) Letter from Norman Pettet to Regional Transfusion Directors/Dr Gunson 2 May 1985 p2 NHBT0089564, Counsel Presentation on Smaller Haemophilia Centres Royal Manchester Children’s Hospital June 2021 paras 41-42 INQY0000255. A list of patients for whom Dr Evans sought 8Y was provided to Dr Snape in October 1985. Letter from Dr Evans to Dr Snape 29 October 1985 BPLL0002377_002
(1822) Evans Twenty-one years of haemophilia Haemophilia 1997 p7 STHB0000259. The advice to which Dr Evans referred was the January 1983 Desforges article in The New England Journal of Medicine.
(1823) Letter from Juliet Morton to David Watters 13 March 1987 p14 HSOC0012997
(1824) Other hospital staff, for example nurses, may not have had the same knowledge as Dr Evans.
(1825) NHD and UKHCDO Pivot Table HIV results from 1979 to 2000 26 August 2022 WITN3826020
(1826) Although the report of an audit visit in 2000 suggested that children with haemophilia would transfer to the adult centre usually after their sixteenth birthday, Dr Dempsey, the consultant paediatric haematologist at the Royal Belfast Hospital for Sick Children from August 1980, recalled that fourteen was the age for transfer. Report of audit visit to the Belfast Comprehensive Care Haemophilia Centre 1-2 June 2000 p2 WITN4027002, Dr Stanley Dempsey Transcript 11 February 2022 pp6-7 INQY1000278
(1827) Written Statement of Professor John Bridges 23 November 2020 para 2 WITN4569001
(1828) Dr Stanley Dempsey Transcript 11 February 2022 p17 INQY1000278
(1829) Dr Stanley Dempsey Transcript 11 February 2022 p24 INQY1000278
(1830) Dr Stanley Dempsey Transcript 11 February 2022 pp24-26 INQY1000278
(1831) Dr Stanley Dempsey Transcript 11 February 2022 p100 INQY1000278
(1832) Dr Stanley Dempsey Transcript 11 February 2022 p27, p40 INQY1000278
(1833) Dr Stanley Dempsey Transcript 11 February 2022 p28 INQY1000278. His recollection was that this was primarily Armour. Dr Stanley Dempsey Transcript 11 February 2022 p98 INQY1000278
(1834) Dr Stanley Dempsey Transcript 11 February 2022 p48 INQY1000278
(1835) Dr Stanley Dempsey Transcript 11 February 2022 p40, p96 INQY1000278
(1836) Dr Stanley Dempsey Transcript 11 February 2022 pp49-50 INQY1000278. Dr Dempsey observed that there were risks with cryoprecipitate too over time but accepted that his cohort of patients were not in the same position as severe patients.
(1837) Written Statement of Dr Stanley Dempsey 2 September 2021 para 23.3 WITN5560001, Dr Stanley Dempsey Transcript 11 February 2022 p51 INQY1000278
(1838) Dr Stanley Dempsey Transcript 11 February 2022 pp51-53 INQY1000278
(1839) Dr Stanley Dempsey Transcript 11 February 2022 p57 INQY1000278
(1840) Dr Stanley Dempsey Transcript 11 February 2022 p62 INQY1000278
(1841) Dr Stanley Dempsey Transcript 11 February 2022 p64 INQY1000278
(1842) Dr Stanley Dempsey Transcript 11 February 2022 p104 INQY1000278
(1843) Notes of two meetings to discuss Haemophilia Centres in London 11 February 1970 p2 DHSC0100026_084
(1844) Unconfirmed Minutes of Haemophilia/Associate Haemophilia Centre and Blood Transfusion Centre Directors and Regional Health Authorities meeting 15 December 1976 p4 CBLA0000533
(1845) Unconfirmed Minutes of Haemophilia/Associate Haemophilia Centre and Blood Transfusion Centre Directors and Regional Health Authorities meeting 15 December 1976 p4 CBLA0000533
(1846) Minutes of Haemophilia, Associate Haemophilia and Blood Transfusion Centres Directors meeting 23 September 1977 p4 CBLA0000657
(1847) Minutes of Haemophilia Centre Directors and Blood Transfusion Centre Directors meeting 1 September 1978 p5 CBLA0000838
(1848) 229,320 units of cryoprecipitate, 231,669 units of commercial concentrates (of varying types) and 215 units of NHS Factor 8, for the treatment of 38 patients. Annual Returns for Great Ormond Street Hospital 1976 HCDO0001077
(1849) 66,990 units of cryoprecipitate, 417,802 units of commercial concentrates (of varying types) and 67,626 units of NHS Factor 8, for the treatment of 41 patients (including 1 with inhibitors). Annual Returns for Great Ormond Street Hospital 1977 HCDO0001160
(1850) A further reduction in the use of cryoprecipitate to 48,650 units, an increase in the use of NHS Factor 8 (173,765 units), but with most treatment (501,214 units) being with commercial concentrates (Factorate and Koate), for the treatment of 42 patients (including 1 with inhibitors). Annual Returns for Great Ormond Street Hospital 1978 p5 HCDO0001257
(1851) 463,441 units of Factorate were used (and a modest amount of Koate: 1,590 units), together with 159,675 units of NHS Factor 8 and 62,720 units of cryoprecipitate. Annual Returns for Great Ormond Street Hospital 1979 HCDO0001324
(1852) 432,326 units of Factorate were used (and 116,877 units of Kryobulin), together with 128,859 units of NHS Factor 8 and 22,890 units of cryoprecipitate. Annual Returns for Great Ormond Street Hospital 1980 HCDO0001421. The mother of a child treated at GOSH, Della Ryness-Hirsch, protested in 1980 when her son’s treatment was changed from cryoprecipitate to Factor 8, but was told that there was not enough cryoprecipitate available and that NHS Factor 8 was perfectly safe. Written Statement of Della Ryness-Hirsch paras 20-24 WITN0282001. She had previously highlighted to the doctors at GOSH concerns about the safety of US blood.
(1853) The return for 1981 is missing. In 1982, 1,339,864 units of Factorate were used (and 35,599 units of Hemofil), together with 205,348 units of NHS Factor 8 and 18,620 units of cryoprecipitate. Annual Returns for Great Ormond Street Hospital 1982 HCDO0001620
(1854) 416,515 units of Factorate were used (and 33,120 units of Koate), together with 419,467 units of NHS Factor 8 and 17,220 units of cryoprecipitate. Annual Returns for Great Ormond Street Hospital 1983 HCDO0001717
(1855) The annual return appears to show the use of 430,076 units of NHS Factor 8, 52,200 units of unheated Factorate, 9,600 units of heat-treated Factorate and 22,770 units of Koate. Annual Returns for Great Ormond Street Hospital 1984 HCDO0001812. Professor Hardisty had been added as an investigator to the clinical trial exemption for Armour’s heat-treated Factorate in 1984. Letter from Will Tarbit to the DHSS ARMO0000137
(1856) Letter from Professor Hardisty to Dr Snape 15 February 1985 CBLA0002042. GOSH had earlier written to BPL in December 1984 regarding the supply of NHS concentrate, in which it was observed that “it will come as no surprise to you that many of the parents of the children we treat here are very anxious about the use of commercial concentrate in use [sic] by their offspring.” Letter from Dr Evans to Norman Pettet 10 December 1984 BPLL0010481
(1857) This was said to be because “children may be safer on cryoprecipitate because of the possible toxic effects of the added chemicals, and also because of the need for considerable follow-up venepunctures which in the context of general ethical difficulties with working on children as experiments, must be a severely limiting factor.” Notes of meeting with Immuno 24 January 1983 pp2-3 PRSE0002647
(1858) Letter from Dr Raina Liesner and Dr Peter Steer to Brian Stanton 10 September 2018 WITN3774003, Written Statement of Matthew Shaw on behalf of Great Ormond Street Hospital 5 October 2020 p1 WITN4650001
(1859) NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1860) National Haemophilia Database Bleeding Disorder Statistics for the Penrose Inquiry April 2012 p31 PRSE0002887
(1861) Dr Anna Pettigrew Transcript 7 December 2020 p10 INQY1000081
(1862) Written Statement of Dr Anna Pettigrew 30 August 2020 p4 WITN3527002
(1863) Written Statement of Dr Anna Pettigrew 30 August 2020 p6 WITN3527002
(1864) Written Statement of Dr Anna Pettigrew 30 August 2020 p8 WITN3527002. Dr Pettigrew thought the SNBTS product might take 5-10 minutes to dissolve, as compared with less than 5 minutes for the Armour product. Dr Anna Pettigrew Transcript 7 December 2020 pp39-40 INQY1000081
(1865) Written Statement of Dr Anna Pettigrew 30 August 2020 p8 WITN3527002
(1866) Written Statement of Dr Anna Pettigrew 30 August 2020 pp10-11 WITN3527002
(1867) Professor Ian Hann Transcript 8 December 2020 p32 INQY1000082, Dr Anna Pettigrew Transcript 7 December 2020 p46 INQY1000081
(1868) Tables showing Glasgow Yorkhill Haemophilia Centre Comparison of product use 1979-1987 and source of F8 concentrate INQY0000242
(1869) Annual Returns for Royal Hospital for Sick Children Glasgow 1977 HCDO0002474
(1870) Annual Returns for Royal Hospital for Sick Children Glasgow 1978 HCDO0002475
(1871) Annual Returns for Royal Hospital for Sick Children Glasgow 1979 HCDO0002476
(1872) Annual Returns for Royal Hospital for Sick Children Glasgow 1980 HCDO0002477
(1873) Annual Returns for Royal Hospital for Sick Children Glasgow 1981 HCDO0002478
(1874) Annual Returns for Royal Hospital for Sick Children Glasgow 1982 HCDO0002479
(1875) Professor Ian Hann Transcript 8 December 2020 p46 INQY1000082. Dr Pettigrew said that there was never any advice from or discussion with Dr Willoughby about non-A non-B Hepatitis. Dr Anna Pettigrew Transcript 7 December 2020 p52 INQY1000081. Nor was there any system for providing junior doctors with updates about medical developments. Dr Anna Pettigrew Transcript 7 December 2020 p54 INQY1000081. Dr Willoughby did not raise or discuss AIDS with Dr Pettigrew at all in the second half of 1982 and she learnt about The New England Journal of Medicine paper from a leukaemia research fellow in 1982. Dr Anna Pettigrew Transcript 7 December 2020 p59 INQY1000081
(1876) The change of approach under Professor Hann is clear from the 1983 annual return, which shows that the vast bulk of treatment was with NHS Factor 8 (1,121,075 units) compared to only 36,850 units of Factorate. Annual Returns for Royal Hospital for Sick Children Glasgow 1983 HCDO0002480. The amount of Factorate used fell further in 1984 to 5,460 units. Annual Returns for Royal Hospital for Sick Children Glasgow 1984 HCDO0002481
(1877) Professor Hann observed that Dr Willoughby was a single-handed doctor and that it was difficult for him to get away. Professor Ian Hann Transcript 8 December 2020 p18 INQY1000082. That may be correct but would not absolve him of the responsibility to read UKHCDO minutes and keep up to date with developments and developing knowledge in medical literature. It appears that he did not, however, share with other staff the material produced by UKHCDO such as minutes or reports: see the evidence of Dr Anna Pettigrew Transcript 7 December 2020 p22 INQY1000081
(1878) Written Statement of Dr Willoughby to the Penrose Inquiry pp2-3 WITN3561002
(1879) Dr Anna Pettigrew Transcript 7 December 2020 pp27-29 INQY1000081
(1880) Professor Ian Hann Transcript 8 December 2020 p22 INQY1000082
(1881) Professor Ian Hann Transcript 8 December 2020 p24 INQY1000082
(1882) Professor Ian Hann Transcript 8 December 2020 pp25-27 INQY1000082
(1883) Written Statement of Dr Anna Pettigrew p6 WITN3527001, Written Statement of Dr Anna Pettigrew para 44 WITN3527002
(1884) As Dr Pettigrew accepted. Dr Anna Pettigrew Transcript 7 December 2020 p70 INQY1000081
(1885) The devastating impacts of these treatment policies were starkly described in the evidence of John McDougall, whose son Euan was treated at Yorkhill. Euan was treated with cryoprecipitate for the first 2-3 years of his life and then with Factor 8 concentrates initially on a reactive basis. But by the time he was 4 years old he was receiving prophylactic treatment. At first he received PFC concentrates, but soon the balance switched to Armour products. Euan was infected with HIV as a result. He became increasingly frail and ill, experienced seizures and went blind. He died in January 1994, just 16 years old. John McDougall Transcript 3 July 2019 pp48-51, pp77-90 INQY1000026. See further Written Statement of John McDougall paras 4-11 WITN2850001 and Written Statement of Kate McDougall para 2 and para 10 WITN2198001
(1886) Written Statement of Dr Anna Pettigrew para 46 WITN3527002
(1887) The extent of that harm was apparent from the evidence of Mr AB, whose sons were treated from the age of about 3 on a twice weekly prophylactic basis, sometimes with the PFC product but often with the Armour concentrate. Both boys were infected with HIV. One of his sons developed AIDS and died in September 1992 aged 17. Mr AB’s evidence powerfully described the horror of watching his child die of AIDS. ANON Transcript 11 July 2019 pp5-11, pp30-39 INQY1000032
(1888) Dr Anna Pettigrew Transcript 7 December 2020 p12 INQY1000081
(1889) Written Statement of Professor Ian Hann para 72 WITN3497005
(1890) Thus in a letter from Dr Geoffrey Scott to Dr Helena Daly (who was a senior registrar at the Royal Infirmary from 1979 to 1985) in anticipation of the latter’s evidence to the Lindsay Tribunal, Dr Scott described himself as the director of the Bristol Haemophilia Centre based at the Bristol Royal Infirmary and Bristol Children’s Hospital. Letter from Dr Scott to Dr Daly 29 June 2000 p2 WITN4685002
(1891) Letter from Dr Scott to Dr Daly 29 June 2000 p2 WITN4685002
(1892) Letter from Dr Scott to Dr Tovey 21 February 1978 BPLL0009270_006
(1893) Written Statement of Dr Helena Daly paras 19.1.1, 36.6, 18.1.1 WITN4685001
(1894) Medical notes relating to Lee Turton’s treatment July 1985 p1 WITN1575012, Colin and Denise Turton Transcript 8 October 2019 pp6-9 INQY1000037. Lee’s treatment was with NHS concentrates.
(1895) Letter from Dr Scott to Anon 3 October 1983 HSOC0003486
(1896) Colin and Denise Turton Transcript 8 October 2019 p10 INQY1000037. Far from there being no risk, Lee was infected with HIV, probably from “one particular batch of NHS concentrate just prior to the introduction of heat-treating.” Letter from Dr Scott to Dr Daly 21 November 1988 WITN1575006. Lee’s health began to deteriorate from 1986 onwards: “He couldn’t walk far, he couldn’t breathe, he couldn’t eat, he was fed eventually through a tube … He would say, ‘I’m frightened’.” Lee died in January 1992. He was ten years old. Colin and Denise Turton Transcript 8 October 2019 p24 INQY1000037
(1897) Written Statement of Professor Pratima Chowdary p2 WITN3826030
(1898) Professor Blackburn was the director of the Sheffield Haemophilia Centre with responsibility for adult haemophilia services until 1981 (and also chair of UKHCDO until 1979); he was succeeded by Dr Preston.
(1899) Written Statement of Professor Sir John Lilleyman para 7.2 and para 8.1 WITN5095001
(1900) Written Statement of Professor Sir John Lilleyman para 11.6 WITN5095001
(1901) Written Statement of Professor Sir John Lilleyman para 16.1 WITN5095001
(1902) The returns suggest that cryoprecipitate was used for hospital treatment and that NHS concentrate was used for home treatment. Annual Returns for Sheffield Children’s Hospital Haemophilia Centre1976 HCDO0001113, Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1977 HCDO0001201, Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1979 HCDO0001367, Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1980 HCDO0001465, Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1981 HCDO0001566. The annual return for 1978 is missing.
(1903) A small amount of Autoplex was used for the treatment of patients with inhibitors. Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1982 HCDO0001664
(1904) 79,450 units of cryoprecipitate were used and 173,807 units of NHS Factor 8; the amount of Factorate used was 13,766. Autoplex was used for the treatment of patients with inhibitors. Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1983 HCDO0000139_004
(1905) Other than, again, Autoplex. Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1984 HCDO0001854. In 1984 cryoprecipitate was used (to a small extent) for home treatment, although the mainstay of home treatment was NHS concentrate. In 1985 cryoprecipitate was again used to some extent for home treatment; Autoplex was used for those with inhibitors, and a small amount of Hyate C (porcine Factor 8) was used. Annual Returns for Sheffield Children’s Hospital Haemophilia Centre 1985 HCDO0001948
(1906) McGrath et al Liver disease complicating severe haemophilia in childhood Archives of Disease in Childhood 1980 OXUH0001751_003. This recorded the outcome of liver biopsies in five boys with severe haemophilia who had persistently abnormal liver function tests. Abnormal histology was present in all: four had chronic persistent hepatitis and the fifth chronic aggressive hepatitis with early cirrhosis. The conclusion was that cryoprecipitate should be used in preference to large pool Factor 8 concentrates in children with haemophilia.
(1907) As Professor Sir John Lilleyman explained in his statement, “we in Sheffield realised pretty early on that there was a potential problem of virus transfer in blood products used for haemophilia since nonA-nonB hepatitis was already recognised as a problem following the observation that abnormal liver function tests were not an infrequent finding in both adults and young boys with severe haemophilia.” Written Statement of Professor Sir John Lilleyman paras 17.1 and 18.1 WITN5095001
(1908) NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1909) A letter from Dr Preston to Dr Lilleyman on 27 June 1985 enclosed the results of 12 children tested for HIV and recorded 1 positive result p8 RHAL0000485. The statement of Lorraine Howgate-Gray confirms that her husband Mathew Machen was infected with HIV and Hepatitis C at Sheffield Children’s Hospital. Mathew died in 2003. He took his own life after being informed that he had AIDS with a limited life expectancy. Written Statement of Lorraine Howgate-Gray paras 20-21 WITN4453001
(1910) NHD and UKHCDO Pivot Table: HIV results from 1979 to 2000 WITN3826020
(1911) Written Statement of Dr Lynne Ball para 6(b) WITN4739001
(1912) See the list of treatments and batch numbers at WITN1805002
(1913) Written Statement of Christine Fowle paras 7-9 WITN1649001. Dr Michael McEvoy was the centre director at Harrogate. In his statement to the Inquiry Dr McEvoy said that the first choice was “the NBTS product either cryoprecipitate or factor concentrate” and, when these were not available, Armour’s product. Written Statement of Dr McEvoy para 12.1 WITN4742001. He could not now recall the consent process at the centre, but anticipated “that the process was influenced by the knowledge that these patients had previously received many and varied products and that these were patients that had been on cryoprecipitate. Therefore they would have been aware of possible issues associated with this type of therapy.” Written Statement of Dr McEvoy para 46.2 WITN4742001. This was not a proper approach to the obtaining of informed consent: even in the 1980s clinicians were not entitled to assume that patients were aware of the risks of treatment.
(1914) Alan and Christine Fowle Transcript 8 May 2019 p8 INQY1000006
(1915) Alan and Christine Fowle had not been asked to consent to testing for HIV nor even told that he was going to be tested. Christopher had also been infected with Hepatitis C, something which the family learned about almost in passing when they had taken him to hospital: Alan, Christopher’s father, said to the doctor “you must be worried about the HIV dangers and the doctor turned round and said, ‘I’m more worried about the hepatitis C’, and we went … we didn’t know, did we? … it was almost in passing conversation.” Alan and Christine Fowle Transcript 8 May 2019 pp18-19 INQY1000006
(1916) Alan and Christine Fowle Transcript 8 May 2019 p15 INQY1000006
(1917) Alan and Christine Fowle Transcript 8 May 2019 p17, pp20-23 INQY1000006
(1918) Alan and Christine Fowle Transcript 8 May 2019 p20 INQY1000006
(1919) Alan and Christine Fowle Transcript 8 May 2019 pp21-22 INQY1000006
(1920) Alan and Christine Fowle Transcript 8 May 2019 p28 INQY1000006
(1921) Patient treatment record for Martin White 1977-2003 p2 WITN1725002
(1922) Written Statement of Valerie White para 9 WITN1725001
(1923) Martin had been treated on a prophylactic basis since at least 1978: an entry in his medical records stated “Has been on thrice weekly prophylaxis”. Medical record of Martin White 31 July 1978 p2 WITN1725005. The notes also recorded “ENTERED IN HEPATITIS TRIAL 1.6.78. Please give Factor VIII marked H.S. only.” His parents were not told about this or asked to consent to it at the time and only learnt about it when receiving his notes after his death. Witness Statement of Valerie White para 24 WITN1725001.
(1924) Letter from Professor Bloom to Dr Mathews 8 March 1983 WITN1725003. March 1983 was the month in which Professor Bloom had a reply from Bruce Evatt of the CDC in the US, giving him a chilling account of the spread of AIDS amongst people with haemophilia. By then, at least, the risk that factor concentrates were causally linked to AIDS was clear. Letter from Dr Evatt to Professor Bloom 7 March 1983 p1 DHSC0001175
(1925) Written Statement of Valerie White para 22 WITN1725001. According to the UKHCDO records, which are not always complete, as at July 1984 he was negative, but a positive test result was recorded in March 1985. Medical record of Martin White WITN1725004
(1926) Written Statement of Valerie White para 31 WITN1725001
(1927) Written Statement of Valerie White para 52, para 56 WITN1725001
(1928) See the Written Statement of Janet Smith para 2, para 6 WITN1523001 and Written Statement of Colin Smith para 2 WITN1781001. See also the statements of Colin’s brothers Daniel, Patrick and Darren. Written Statement of Daniel Smith WITN1526001, Written Statement of Patrick Smith WITN1524001, Written Statement of Darren Smith WITN1525001
(1929) Medical notes for Colin Smith WITN3705028
(1930) Letter from Professor Bloom to Dr Carr 3 August 1983 WITN1523003. Colin was in all probability infected with non-A non-B Hepatitis in consequence of his treatment: a UKHCDO form AIDS/3 completed by Dr Dasani in 1989 reported “chronic Liver Disease presumed Non-A Non B Hepatitis”. Patient medical record and AIDS surveillance report of Colin Smith p2 CVHB0000004_038
(1931) Letter from Professor Bloom to Dr Carr 3 August 1983 WITN1523003
(1932) A written statement filed on behalf of Cardiff and Vale University Health Board suggests that the treatment administered to Colin on 21 July 1983 was not administered by Professor Bloom, but by a junior doctor, Dr Stephen May, following a call to Professor Bloom to seek advice: the advice being “for factor VIII or cryo if v puncture easy”: see the Written Statement of Len Richards pp1-2 WITN3705027, Medical notes for Colin Smith 21 July 1983 p2 WITN3705028. There are three observations from this evidence: first, it establishes that cryoprecipitate would have been available; secondly, it establishes that Professor Bloom, although not the author of the notes on 21 July 1983, had seen Colin on 7 July 1983 and would have known that he had not been previously treated with blood products (a fact that he would have been reminded of by Dr May); and thirdly, that Professor Bloom, in his advice to Dr May as to how to treat Colin, failed to advise him that cryoprecipitate was a far safer treatment for a baby who had never received blood products, irrespective of the ease or difficulty of the venepuncture. Moreover, not a word is said in the notes to suggest that the relative risks of these two treatments were discussed with Colin’s parents.
(1933) Colin and Janet Smith Transcript 24 July 2019 p4 INQY1000034
(1934) Colin and Janet Smith Transcript 24 July 2019 pp5-7 INQY1000034
(1935) Haemophilia treatment record of Colin Smith WITN1523006. The statement of Len Richards on behalf of Cardiff and Vale University Health Board indicates that this treatment may have taken place at the Royal Gwent Hospital rather than in Cardiff. Written Statement of Len Richards pp2-4 WITN3705027. Irrespective of the location of the treatment, a child of Colin’s age should not have been treated with commercial concentrates in 1983. The statement of Len Richards asserts that Professor Bloom “had a strict policy of using NHS factor VIII concentrate or cryoprecipitate for young children at this time.” It is not clear what the evidential basis is for that assertion, other than Cardiff’s Haemophilia Treatment Policy Guidelines 18 May 1983 WITN4029002. However, if that was indeed Professor Bloom’s “strict policy”, it suffers from the defect that it fails to distinguish between the relative risks of cryoprecipitate and NHS concentrate for previously untreated children. Further, if there was such a “strict policy”it begs the question as to (a) why Professor Bloom did not communicate such a policy through UKHCDO – his letter (Letter from Professor Bloom to Dr Rizza 24 June 1983 HCDO0000270_004) cannot sensibly be construed as advocating a strict policy for children of treatment only with NHS concentrate or cryoprecipitate; and (b) why Professor Bloom did not communicate that policy to the Royal Gwent Hospital, given that Colin’s care was shared by Cardiff and Royal Gwent. Colin’s case thus provides a stark illustration of systemic failure. It also suggests that Professor Bloom advocated, on paper, a policy of not using commercial concentrates, presumably because he saw them as higher risk. There is no trace of this policy in what he was saying publicly about the risks of concentrates conveying the cause of AIDS.
(1936) Colin and Janet Smith Transcript 24 July 2019 pp7-8 INQY1000034
(1937) Colin and Janet Smith Transcript 24 July 2019 pp10-11 INQY1000034
(1938) Colin and Janet Smith Transcript 24 July 2019 p25 INQY1000034
(1939) Colin and Janet Smith Transcript 24 July 2019 p32 INQY1000034
(1940) Written Statement of Patricia Harding para 7 WITN5513001, Medical notes of Lee Harding WITN5513002
(1941) Written Statement of Patricia Harding para 8 WITN5513001
(1942) Dr Muriel Seaman was a consultant haematologist; she became the director the Cambridge Haemophilia Centre in 1984, succeeding Dr Chalmers. Written Statement of Dr Muriel Seaman para 2 WITN3815002
(1943) Written Statement of Patricia Harding para 11 WITN5531001
(1944) Written Statement of Patricia Harding para 16 WITN5531001
(1945) The haemophilia centre at the Norfolk and Norwich Hospital was an associate centre: its annual return for 1984 suggests that most treatment was with NHS Factor 8; very small amounts of Armour and Koate were used; and no cryoprecipitate was used except for the treatment of two patients with von Willebrand disorder. Annual Returns for Norfolk and Norwich Hospital 1984 HCDO0001845
(1946) Written Statement of Gwynneth Walker paras 6-7, para 9 WITN1788001
(1947) Written Statement of Gwynneth Walker paras 11-12 WITN1788001
(1948) Written Statement of Gwynneth Walker para 15 WITN1788001
(1949) Written Statement of Gwynneth Walker paras 38-42 WITN1788001
(1950) Written Statement of Gwynneth Walker para 53 WITN1788001
(1951) Written Statement of Gwynneth Walker paras 57-59 WITN1788001. See also the statements of Steven’s brothers Christopher and Michael and his father John. Written Statement of Christopher Walker WITN1787001, Written Statement of Michael Walker WITN1790001, Written Statement of John Walker WITN1789001
(1952) Written Statement of Rosemary Calder para 6 WITN1134002, Medical records for Nicholas Calder 1977 WITN1134003
(1953) Written Statement of Rosemary Calder para 7 WITN1134001
(1954) Written Statement of Rosemary Calder para 9 WITN1134001, Haemophilia treatment records for Nicholas Calder WITN1134004. The recollection of Dr Cecil Reid, who was a senior registrar and then (from 1983) consultant at Northwick Park, was that patients were treated with cryoprecipitate until the centre switched to virally inactivated 8Y or Profilate in 1986. Written Statement of Dr Cecil Reid para 8a, para 8c WITN5248001. This is plainly incorrect in light of the records relating to the witness’ son, which he recognises. His statement was a failure of recollection which he has corrected. Dr Diana Samson, who was a consultant haematologist at Northwick Park from 1977-1983, (and was not herself involved in Nicholas’ treatment as described in the text) told the Inquiry that at the time she worked there “UK blood donors were already screened for hepatitis B, and at that time it was not appreciated that non-A non-B hepatitis could lead to chronic liver disease. I think we felt that blood products were very safe”. Written Statement of Dr Diana Samson para 54 WITN4673001. The view that blood products were, in the late 1970s and early 1980s, “very safe” was misguided and misinformed.
(1955) Written Statement of Rosemary Calder para 11 WITN1134001
(1956) Written Statement of Rosemary Calder paras 10-11 WITN1134001
(1957) Written Statement of Rosemary Calder paras 12-14, para 18 WITN1134001: “To receive a letter like that, at a time when there was so much hysteria in the media, and so little actual facts known, was devastating … A matter as confidential as this should have been approached much more personally and I feel it was deplorable treatment.” The letter stated that “I just wanted to let you know that we have received a positive result on the HTLV3 test sent a few weeks ago. As you probably know, more than one third of all haemophiliacs in this country have such antibodies, and the true clinical significance of this finding is unknown. Nevertheless, it seems pretty certain that a positive screen for antibodies alone, does not imply that an individual has either had or is going to develop the acquired immune deficiency syndrome.”Rosemary was invited to contact the consultant for a “brief chat”. Letter from Dr Reid to Rosemary Calder 23 August 1985 WITN1134005. Five years later, in 1990, a letter from the Royal Free Hospital informed Nicholas’s parents that their son had been infected with Hepatitis C. They had not been aware that Nicholas was being tested for Hepatitis C until the letter was received. Witness Statement of Rosemary Calder paras 15 and 20 WITN1134001
(1958) Witness Statement of Rosemary Calder para 2 WITN1134001. See also the statements of Nicholas’s wife Lyndsey and sister Julie Lear. Written Statement of Lyndsey Calder WITN4450001, Written Statement of Julie Lear WITN4703001
(1959) Patient Record of Stephen Finney p6 WITN1047002
(1960) As did his mother, through blood to blood contact. Written Statement of Stephen Finney para 6 WITN1047001. Hepatitis B caused significant adverse health effects for him in adulthood. Written Statement of Stephen Finney paras 26-28 WITN1047001
(1961) Patient Record of Stephen Finney pp6-7 WITN1047002
(1962) Written Statement of Stephen Finney paras 10-12 WITN1047001
(1963) Written Statement of Stephen Finney paras 8-9 WITN1047001
(1964) Written Statement of Stephen Finney paras 23-38 WITN1047001
(1965) He later developed Hepatitis D as well. Written Statement of Robert Hodgkins paras 22-23 WITN0009001
(1966) Written Statement of Robert Hodgkins para 15 WITN0009001
(1967) Written Statement of Robert Hodgkins para 11 WITN0009001. His mother Edna Hogkins says: “we were told that it was a new treatment from America which was freeze dried. They never spoke to my husband or I about any risks, or what it was.”Written Statement of Edna Hodgkins para 14 WITN3889001
(1968) Written Statement of Robert Hodgkins para 12 WITN0009001 and Written Statement of Edna Hodgkins para 22 WITN3889001
(1969) Written Statement of Robert Hodgkins paras 34-57, paras 70-71 WITN0009001
(1970) Written Statement of ANON p2 WITN1265002
(1971) Written Statement of ANON para 6 WITN1265001
(1972) Written Statement of ANON para 7, paras 12-13 WITN1265001
(1973) Written Statement of ANON para 33 WITN1265001
(1974) Written Statement of ANON paras 10-13, paras 20-22, para 38 WITN5340001
(1975) In fact Stuart suffers from Ehlers-Danlos syndrome, a connective tissue disorder which can lead to bruising. Stuart Mclean Transcript 17 October 2019 p1 INQY1000043
(1976) Letter from Dr Holman to Dr Naunton-Davies 4 April 1977 WITN0653003
(1977) Letter from Dr Naik to Mr Rhyce 31 August 1977 WITN0653005
(1978) Letter from Dr Rizza to Dr Naik 13 September 1977 WITN0653006, Letter from Dr Matthews to Dr Naik 18 October 1977 WITN0653007
(1979) Letter from Dr Naik to Dr Naunton-Davies 9 November 1977 WITN0653008
(1980) Letter from Dr Naik to Mr Stossell 6 September 1978 WITN0653009
(1981) Stuart Mclean Transcript 17 October 2019 pp23-24 INQY1000043
(1982) Written Statement of Stuart Mclean para 18 WITN0653001
(1983) There are, of course, some centres where children were not treated in the way described and were not infected; however, a clear overall picture emerges from the evidence available to the Inquiry.
(1984) See the Chapter on People’s Experiences and the very large number of written statements from people infected and affected that have been published on the Inquiry’s website.
(1985) Andrew died at the age of 22. Written Statement of Michael Saunders paras 7-8 WITN1506001
(1986) Written Statement of Paul paras 8-9, 13, 17-18, 32 WITN0053001
(1987) She discovered her sons had been tested for, and infected with, HIV only when she took one of them for dental treatment and the dentist came “in a space suit” and “didn’t want to come close”. When a newspaper reported that two brothers were in hospital with AIDS, the health authority put out a statement that the parents knew of the risks to their children – they did not – and were being counselled by senior doctors – they were not. Mrs C Transcript 8 May 2019 pp59-65 INQY1000006. She discovered only years after one of her sons had died that he had also been diagnosed with Hepatitis C. Mrs C Transcript 8 May 2019 pp83-84 INQY1000006
(1988) He learnt that he was Hepatitis C positive only in 1994 when attending a standard review at the Haemophilia Centre, not having been told that he was being tested. He was never informed that he had been infected with Hepatitis B, only learning this from an entry in his medical records. Written Statement of Sean Nevin paras 11-22 WITN1425001
(1989) Letter from Dr Rizza to Dr Ernest French 17 June 1976 WITN1003007. From 1980 onwards he was largely treated with commercial concentrates, with there never being any discussion with his parents about that or the reasons for it. Paul Transcript 10 October 2019 pp17-18 INQY1000039. He attended a routine clinic appointment in Nottingham in April 1985 following which his blood was tested for HIV without his knowledge. “I had no idea that’s what they were doing.” Paul Transcript 10 October 2019 p31 INQY1000039. On 24 June 1985 he received a letter from Dr Theodore Blecher referring to the results on recent blood samples and stating “I should like to briefly discuss one or two of these results with you personally. Could you therefore please come to see me for a short time one day next week.” Letter from Dr Blecher to Paul 24 June 1985 WITN1003015. He had no sense when he attended that appointment for a “brief chat” that he would learn that he had the virus that causes AIDS. Had he been told in April 1985 that he was having the test done, he would have had time to think about it; had the letter inviting him to the Centre given him “a bit of indication. If it said, you know, take the afternoon off, bring somebody with you or whatever”, he might have thought it a bit more serious. It seemed, unsurprisingly, “a very surreal moment.” He received no advice, no information, other than “Don’t tell anybody” and “Don’t have sex, wear a condom.” As he told the Inquiry, “I had no preparation for it. They knew what they were going to tell me. Because they knew what they were going to tell me … they should have prepared a lot – they should have known that telling someone – yes, telling someone, those doctors had treated me since I was a toddler. They’d known me. They know my family. They knew what I was like and everything. They just saw me for a few moments, gave me the most devastating news I’d ever had. Told me that I’ve only got a few years to live, telling me to keep it a secret. Everything went out the window that day. Everything changed that day.” He was 21 years old. Paul Transcript 10 October 2019 pp32-37 INQY1000039
(1990) Written Statement of Matthew Johnson paras 11-15, 27-32, 54-56 WITN1057001, Matthew Johnson Transcript 3 May 2019 pp1-5, pp8-9 INQY1000004. He was tested for Hepatitis C without consent in 1989, but his parents were not told that he had Hepatitis C until January 1992.
(1991) ANON Transcript 16 October 2019 pp2-5 INQY1000042. Mr AN’s father said that they were told that Factor 8 was “a revolutionary treatment, easier to use and more effective … There was no warning of risk of infection through using FVIII. If there had been any suggestion of risk, I would have jumped on it and all over it.” Written Statement of ANON para 7 WITN4711001
(1992) Written Statement of ANON para 14, para 52 WITN0194001, Completed Questionnaire for Medical Negligence Solicitors WITN0194002, Proof of Evidence concerning Litigation 9 June 1990 p4 WITN0194007
(1993) Colette Wintle Transcript 10 May 2019 pp118-120, pp123-125, pp136-137 INQY1000008, Written Statement of Colette Wintle para 16 WITN1056001. The treatment with concentrates in 1985 was all the more surprising because the previous year Dr Kernoff had written to her GP advocating the use of DDAVP precisely because “of the risk of hepatitis after transfusion of factor VIII concentrate being very high in infrequently-treated patients”. Letter from Dr Kernoff to Dr Hall 22 February 1984 p1 WITN1056010x
(1994) Written Statement of Irene Brierley paras 8-11 WITN5520001. Had her husband been warned of the possible risks from the use of unheated material in January 1985, he might well have opted to revert to the use of fresh frozen plasma. He had started treatment with Factor 9 in the mid to late 1970s and had never been warned about the risk of infection. As a pharmacist, he had begun to worry about treatment but was assured by clinicians at the haemophilia centre that it was safe. He asked several times if it was heat-treated and was told that it was (this was, at the time, incorrect), and was specifically told in early 1985 that it was safe to inject. In the summer of 1985 he was tested for HIV (having had to ask for a test) and was informed in a short letter “of no more than two or three sentences” that he was HIV positive. See also Status Report on Medical Negligence Cases 15 July 1991 p21 DHSC0045373_118
(1995) Nigel Hamilton Transcript 23 May 2019 pp5-6 INQY1000011, Simon Hamilton Transcript 22 May 2019 p3 INQY1000010. Simon died in 2023.
(1996) Written Statement of ANON paras 10-16, paras 22-24 WITN3160001
(1997) Written Statement of ANON paras 7-9 WITN0472001
(1998) Su Gorman Transcript 5 June 2019 p134 INQY1000014. Steve died in 2018 and Su died in 2023.
(1999) Alice Mackie Transcript 4 July 2019 pp23-33 INQY1000027. Professor Ludlam was asked whether in 1983/1984 he discussed with patients the risks of AIDS and offered them the choice of reverting to cryoprecipitate. He could not remember, but referred to the evidence of Dr Robert Carr. Professor Christopher Ludlam Transcript 2 December 2020 p40 INQY1000078. However, Dr Carr (who was at the time on the junior registrar rotation at Edinburgh) was not involved in discussions with patients: see Written Statement of Dr Robert Carr paras 40-43 WITN4677001. Professor Ludlam confirmed that he did not proactively raise the question of AIDS risks with patients, but stated that he would have answered questions if they were raised (although he could not remember such inquiries from patients). Professor Christopher Ludlam Transcript 2 December 2020 pp58-59 INQY1000078, Written Statement of Professor Christopher Ludlam para 237 WITN3428001
(2000) Written Statement of Carol Carruthers paras 6-10 WITN1850001, Carol Carruthers Transcript 30 October 2019 pp44-47 INQY1000047
(2001) Written Statement of ANON paras 11-13 WITN0850001
(2002) Written Statement of ANON para 7 WITN1291001, ANON Transcript 14 June 2019 pp9-10 INQY1000020
(2003) Letter from Alison Worsley to Dr Heatherington 13 July 1983 p6 WITN1212002, Perry Evans Transcript 30 April 2019 pp65-66 INQY1000001
(2004) Written Statement of Dr Anna Pettigrew p16 WITN3527002, Dr Anna Pettigrew Transcript 7 December 2020 pp42-3 INQY1000081
(2005) Professor Ian Hann Transcript 8 December 2020 pp52-3, p59, pp81-82 INQY1000082. As the father of a boy treated at the RHSC told the Inquiry, there was no discussion with parents about the risks: “What he [Dr Willoughby] certainly didn’t do was to discuss it with the parents or discuss it with us or to discuss it with other parents and to come to a consensus.” John McDougall Transcript 3 July 2019 p60 INQY1000026
(2006) Statement from Dr John Martin on treatment of people with haemophilia p7 DHSC0043164_070
(2007) Statement from Dr Hill 11 April 1992 para 28 OXUH0000005_011
(2008) Written Statement in Anon v Birmingham Central District Health Authority Provisional Individual Trial Bundle p1 OXUH0000005_010. See by way of example: Written Statement of ANON para 10, para 22 WITN1320001, Susan Threakall Transcript 8 October 2019 pp39-40 INQY1000037, Mr AN Transcript 16 October 2019 pp4-5 INQY1000042, John Cornes Transcript 11 June 2019 pp14-15 INQY1000017, Elisabeth Buggins, Brenda Haddock and Christine Woolliscroft Transcript 6 October 2022 p7, pp57-58, pp78-79 INQY1000253
(2009) RMCH Information pages 15 November 1978 p3 HSOC0022606. This is precisely the kind of practical document which parents might well have read, and would have been where the risks of treatment to the child could and should have been spelt out.
(2010) Susman-Shaw Home treatment for children with haemophilia Nursing Times 23 September 1981 p4 HSOC0002894
(2011) Dr David Bevan Transcript 12 January 2021 p39 INQY1000086
(2012) Dr Brian Colvin Transcript 6 October 2020 pp89-91 INQY1000061
(2013) Report from Professor Bloom in Haemophilia Litigation 19 September 1991 p7 DHSC0045373_049. In a report authored by Professor Bloom in May 1992 he said that he thought warnings should have been given prior to May 1983 as to the risks of hepatitis consequent to treatment with concentrate. Supplementary Report 11 May 1992 p6 OXUH0000005_020. The evidence available to the Inquiry indicates, however, that he did not do so. In his main report produced during the HIV Haemophilia Litigation, Professor Bloom commented “briefly on general information available with regard to hepatitis” by pointing to the manufacturers’ inserts in vial boxes of concentrates, which were usually issued to patients on home treatment, to the presence of Haemophilia Society representatives at UKHCDO meetings, and to Dr Jones’ book Living with Haemophilia. Haemophilia Litigation Report June 1990 p74 DHSC0001297
(2014) Dr Saad Al-Ismail Transcript 17 November 2020 pp101-108 INQY1000074. Dr Al-Ismail pointed to the fact that with every single concentrate there was a drug information leaflet. He had not seen them but “was assured by Professor Bloom that in each one of them a reference was made, for example, to the hepatitis, not to the AIDS.” The adequacy of what was in the drug information leaflets is addressed in the chapter on Pharmaceutical Companies but in any event (a) it was not sufficient for a doctor to rely on what was in a leaflet as a substitute to providing patients with information about the risks of treatment: it was (and remains) the responsibility of the doctor to provide that information to the patient; and (b) it was even less appropriate for the doctor to rely on the contents of a leaflet that he himself had not read and checked.
(2015) See for example Professor Christine Lee Transcript 21 October 2020 pp40-42 INQY1000066, Professor Christopher Ludlam Transcript 2 December 2020 pp58-61 INQY1000078
(2016) Except in exceptional cases.
(2017) Written Statement of Professor Christopher Ludlam to the Penrose Inquiry PRSE0004704. Draft dated 20 April 2011.
(2018) As I read it, it does not actually summarise what goes before, but makes a new and overriding point. The reader of this Report is entitled to draw their own conclusions. Written Statement of Professor Christopher Ludlam to the Penrose Inquiry pp11-12 PRSE0004704
(2019) Emphasis added. Jones Haemophilia Home Therapy 1980 pp88-89 RLIT0001201
(2020) As a further example, Professor Ludlam claimed that when he arrived at Edinburgh there seemed to be “sort of general knowledge” among patients about the risk of hepatitis, although the only evidence he could think of was that Dr Davies, in setting up home treatment for a small number of patients, asked them to sign a form to say that they agreed to treat themselves and that there was the possibility of hepatitis as a result of their therapy. However the form did not descend to specifics about Hepatitis B or NANBH, nor did it say anything about the seriousness of hepatitis or the possibility of developing a chronic condition or liver disease. Inherited Haemorrhagic Disorders Home Treatment Consent Form WITN3428006. Professor Ludlam said that he himself brought it “very explicitly” to all patients’ attention when he gave each patient a slip of paper to use if treated at other centres which said “Please give this patient if possible NHS Factor VIII”. He said he “would have explained to patients about hepatitis”, but this is implausible given that it was also his evidence that he did not at that time think NANBH was particularly serious, that he assumed that Dr Davies would have explored the risks with patients, and that what he would say to them would depend on how they responded to what he was telling them about liver tests. This falls far short of providing the information that ought to have been given for the purposes of informed consent. Professor Christopher Ludlam Transcript 1 December 2020 pp132-154 INQY1000077
(2021) Written Statement of Dr Peter Jones para 28(c) WITN0841005. In relation to knowledge of infection risks, Maureen Fearns the nursing sister at Newcastle, referred to the information leaflet which would state the size of the pool. She said that she “later realised, in hindsight, that this increased the risk of infection. I had not made the link between the size of the pool and infection risk until then.” If the nurse specialist had not made that link on the basis of the information leaflets, it is not reasonable to expect or assume that patients would be able to, nor is it consistent with Dr Jones’ evidence that all available information was provided to patients. Written Statement of Maureen Fearns para 74 WITN4042001
(2022) See the chapter on The Haemophilia Society.
(2023) National Blood Transfusion Service AIDS Leaflet 6 July 1983 p2 NHBT0020668
(2024) Thus, for example, at the Royal Hospital for Sick Children in Glasgow Dr Pettigrew accepted that people were unaware that sera was stored. Dr Anna Pettigrew Transcript 7 December 2020 p72 INQY1000081
(2025) Professor Christine Lee Transcript 21 October 2020 pp64-66 INQY1000066
(2026) Professor Christopher Ludlam Transcript 4 December 2020 p53 INQY1000080
(2027) Letter from Dr Katharine Adamson to unknown patient 12 February 1985 HIGH0000012
(2028) Written Statement of Bruce Norsworthy para 11 WITN3143001
(2029) Written Statement of Kathleen Algie paras 31-32 WITN3109001
(2030) Letter from Dr Thomas Taylor to William MacKerrow 20 October 1988 p2 HIGH0000020
(2031) See the chapter on Treloar’s.
(2032) Written Statement in Anon v Birmingham Central District Health Authority Provisional Individual Trial Bundle pp2-3 OXUH0000005_010. She was asked by the hospital to seek support elsewhere because staff at the hospital were becoming burdened. When she gave oral evidence to the Inquiry, her memory was quite clear that the doctors “encouraged us not to ask unless they felt we really needed to know”. Elisabeth Buggins Transcript 6 October 2022 pp15-18 INQY1000253
(2033) Brenda Haddock Transcript 6 October 2022 p58 INQY1000253. Her son, Andrew, was told that he was infected with HIV on his own at a meeting with Dr Hill, without his parents’ knowledge. He was around 12 years old. Brenda only discovered that Andrew had been infected with HIV accidentally when looking through his notes when he was a hospital inpatient. Brenda Haddock Transcript 6 October 2022 pp60-64 INQY1000253. During the time when the hospital knew that he was HIV positive, and his family did not, Brenda continued to treat him at home, thereby being put at risk herself. As she observed in her evidence to the Inquiry, “in the case of children, the parents should have been told before the child, so that we could be prepared to help our child accept and take on board that information. Whereas we didn’t even know he’d been told and we couldn’t understand why he changed so much, and lost interest in everything that he loved before, because he thought that he’d got no future.” Andrew died in 1996. Brenda Haddock Transcript 6 October 2022 p99 INQY1000253
(2034) Mr and Mrs BE Transcript 6 October 2022 pp118-9 INQY1000253
(2035) See for example the Written Statement of Alison Bennett para 2.12 WITN0553001, Counsel Presentation on Smaller Haemophilia Centres June 2021 para 62 INQY0000255
(2036) Letter from Dr Evans to Mr and Mrs Bennett 24 August 1985 WITN0553002, Letter from Dr Evans to Anon 31 May 1985 WITN1736002. The examples which the Inquiry holds suggest that letters were being sent out between May and August 1985. It is unclear why the tests were not carried out earlier. There is also some evidence of two group meetings for parents being held at the RMCH in the summer of 1985. Written Statement of Juliet Batten para 17 WITN0343001, Counsel Presentation on Smaller Haemophilia Centres Transcript 16 June 2021 p55 INQY1000129
(2037) As Alan Burgess told the Inquiry, “if the letter had gone to a neighbour, if it hadn’t been delivered, if it had gone missing, the connotations are horrific just to even think about it, because at the time -- I mean, the stigma is still about now, but the stigma then was pretty awful. You can only imagine what would’ve happened … I thought it was shocking. But that was indicative of the way we used to get treated, you know, by the medical profession, to be fair.” The shock of being informed of the HIV test result by letter “never went away really.” Alan Burgess Transcript 28 October 2019 pp9-11 INQY1000045, Letter from M S Edwards to Alan Burgess 25 September 1985 WITN1122004
(2038) Mersey Regional Haemophilia Centre Response to Questionnaire: HIV Litigation Main Statement of Claim p18 NHBT0085908. A publication in The Lancet in February 1985, of which Dr McVerry was a co-author, along with Dr Machin, Dr Rachanee Cheingsong-Popov and Dr Tedder, referred to the testing of people with haemophilia for HIV. Dr McVerry’s involvement suggests that some patients from Liverpool were amongst the cohort being tested and in any event shows that Dr McVerry had a working knowledge of the availability of testing and of the likelihood of positive test results. Machin et al Seroconversion for HTLV-III Since 1980 in British Haemophiliacs 9 February 1985PRSE0001758. A further publication in the British Journal of Haematology in 1986 (but sent to the journal in June 1985) was again co-authored by Dr McVerry and others, reported testing on 21 Liverpool patients with haemophilia, and an investigation of the wives of some patients. McVerry et al HTLVIII antibody and T cell subset ratios in haemophiliacs and their spouses 1986 RLIT0000127. Notwithstanding this work, and for no obviously good reason, there does not appear to have been a programme of testing all of the Liverpool patients at this time.
(2039) Written Statement of ANON para 9 WITN2783001
(2040) Written Statement of ANON paras 13-24 WITN1403001. Her husband’s medical records show that he was tested for HIV in January 1985. As at October 1985 they had still not been told that he was HIV positive. Indeed, the first official confirmation his widow had that he had HIV/AIDS was after his death in 1985 when she saw it recorded on his death certificate. The public health implications of such delays are obvious. See for example: Sun Times Time for a last fling?, Sun Times AIDS expert wants national screening, News of the World Wonder Potion Fights Off AIDS 26 October 1986 HSOC0015592. Under the heading “Wife infected in test delay” it explains how a man with haemophilia found to be infected with HIV following treatment at Liverpool was not told of the results for several months and in the meantime passed the infection to his wife. p2 HSOC0015592
(2041) See for example Written Statement of ANON para 8 WITN3664001, Written Statement of ANON para 7 WITN1808001
(2042) Derek Martindale Transcript 30 April 2019 pp23-24 INQY1000001
(2043) Patient HIV data for Peter Major p3 WITN2506007
(2044) Letter from Keith Myers to Dr Mukherjee 16 July 1984 WITN2506008
(2045) Letter from Guy Lucas to Dr Mukherjee 20 November 2004 WITN2506006
(2046) Written Statement of Ruth Major para 11 WITN2506001. Dr Guy Lucas, who wrote the 20 November 1984 letter, offered the “speculation” that this may have represented “caution about discussing an as yet unsubstantiated diagnosis”. Written Statement of Dr Guy Lucas p3 WITN3485003. That did not, however, prevent the suspicion being shared with the GP.
(2047) Clinical notes of Paul Summers WITN2406007
(2048) Letter from Professor Bloom to Dr Thomas 19 September 1984 WITN2406006
(2049) Monica Summers and Tony Summers Transcript 25 July 2019 pp8-12 INQY1000035
(2050) Letter from Professor Bloom to Dr Thomas 23 September 1985 WITN2406008
(2051) Monica Summers and Tony Summers Transcript 25 July 2019 pp14-15 INQY1000035
(2052) Letter from Dr P Greedharry to Dr J Stafford 18 September 1986 p3 WITN2406013
(2053) Monica Summers and Tony Summers Transcript 25 July 2019 p18 INQY1000035, Letter from A Prentice to Professor Bloom 26 November 1986 WITN2406014
(2054) See for example the evidence of Professor Ian Hann Transcript 8 December 2020 p89-90 INQY1000082. Professor Hann accepted that it should have been done differently.
(2055) See for example Inquest Bundle of Anon 1986 p11, p16 CRBI0000006
(2056) Mr AI Transcript 10 October 2019 pp140-142 INQY1000039
(2057) Christine Woolliscroft Transcript 6 October 2022 pp82-84 INQY1000253. Michael died in 1995 at the age of 25. She learnt that Michael had been infected with Hepatitis C after he had died. One of the doctors, in the course of a conversation in the car park, said “Well, of course he was hepatitis C positive as well.” Christine Woolliscroft Transcript 6 October 2022 p87 INQY1000253
(2058) Professor Christopher Ludlam Transcript 2 December 2020 pp89-91 INQY1000078. The Yorkshire Post article Tests on Haemophiliacs Positive NHS Blood Carries Killer AIDS Virus was published on 20 December 1984. PRSE0004577. An article in The Scotsman AIDS virus found in infirmary blood supply followed on 21 December 1984. p1 HSOC0016028
(2059) Letter from Professor Ludlam to Patients and Parents 12 December 1984 WITN3428009
(2060) Professor Christopher Ludlam Transcript 2 December 2020 p93 INQY1000078
(2061) Alice Mackie Transcript 4 July 2019 pp47-52 INQY1000027. See also the Witness Statement of Robert Mackie para 16 WITN2190001, “At the meeting, we were told that some people had been infected with HTLV-III by SNBTS PFC Factor VIII which they had received. Along with my wife and I, all the people at this meeting that I spoke to, thought that the people who had been infected had been informed before the meeting, so we all thought that we were all ‘safe’.” They learned that he had been infected at an appointment in 1987.
(2062) Advice Sheet for Adult Patients and Families Acquired Immune Deficiency (AIDS) pp1-3 PRSE0002785. The sheet also said that “About half the patients in England and about ten per cent in Scotland have had exposure and are HTLV III Ab-positive”, which again had the potential to suggest to readers that those infected had already been tested and informed. The information sheet concluded “Remember that you must continue to treat yourself with the concentrates as the risks are much greater of bleeding than of contracting the rare disease of AIDS.” Original emphasis.
(2063) Letter from Dr Wensley to Anon 4 January 1985 PMOS0000083. Given that the right tests were available, it is unclear why the letter was expressed in this way, rather than individuals being tested and given their individual test results.
(2064) At the meeting, in response to the question “Should we assume that we have got the HTLV-3 virus and inform the dentist?” Dr Delamore replied that “All patients will shortly be tested for the HTLV-3 antibody but until the results of those tests are available, it is best to assume that you might positive [sic] and to inform your dentist.” Dr Wensley is recorded as saying that “As home-treatment patients come in for more factor VIII supplies they will be changed onto heat-treated clotting factor or be given more of the same batch that they have been using.” Minutes of special haemophilia meeting on AIDS 3 February 1985 p1, p3 COLL0000003. It would appear, therefore, that no attempt was made to recall existing supplies of non-heat-treated concentrates.
(2065) Letter from Manchester Royal Infirmary Haemophilia Centre to Anon 22 May 1985 WITN3543003, Letter from Olive Redding to Anon 2 September 1985 DHSC0013118
(2066) Counsel Presentation on Manchester Royal Infirmary Haemophilia Centre January 2021 paras 123-125 INQY0000322
(2067) Nigel Hamilton Transcript 23 May 2019 pp7-11 INQY1000011, Written Statement of Louise Marsden para 26 WITN1371001, Louise and Trevor Marsden Transcript 9 October 2019 pp3-7 INQY1000038. Trevor Marsden was only told that he had Hepatitis C when he attended the Belfast Haemophilia Centre in 1996. Written Statement of Trevor Marsden paras 15-17 WITN1372001
(2068) Written Statement of Dr Elizabeth Mayne para 3.8.1 WITN0736005
(2069) Letter from Dr Pettigrew to Dr Taylor 17 May 1985 p1 GMCO0001690_055 and Written Statement of ANON para 4 WITN2149001. It is noteworthy that in May 1989 David Watters at the Haemophilia Society, writing to Dr Rizza, set out his understanding that “patients with haemophilia attending Raigmore Hospital in Inverness and Aberdeen Royal Infirmary are not necessarily being advised or [sic] their HIV status.” He referred to the case of a 14-year-old boy having recently and suddenly been told that he was HIV positive, his parents having assumed in the lack of information to the contrary that he was negative. Letter from David Watters to Dr Rizza 22 May 1989 LOTH0000006_028
(2070) Melbye et al HTLV-III Seropositivity in European Haemophiliacs Exposed to Factor VIII Concentrate Imported from the USA The Lancet 22 December 1984 PRSE0001630
(2071) Professor Gordon Lowe Transcript 10 December 2020 pp24-28, pp65-70 INQY1000084
(2072) Letter from Dr Lowe and Dr Forbes 8 January 1985 PRSE0000859
(2073) Letter from Dr Lowe and Dr Forbes April 1985 PRSE0003567
(2074) Minutes of Haemophilia Reference Centre Directors meeting 10 December 1984 p4 HCDO0000394_117. A further account of the meeting was provided by Dr Smithies in her minute to Dr Abrams on 12 December 1984. She recorded that “Patients who asked for their HTLV III antibody test results should be informed of them otherwise it is up to individual Directors to decide whether or not they wish to tell the patients their results.” Minute from Dr Smithies to Dr Abrams 12 December 1984 p1 DHSC0001117. No concern was voiced by Dr Smithies in this minute about this proposed approach. Nor was it questioned how patients could ask for their results if they did not know that they had been tested.
(2075) Dr Mark Winter Transcript 2 October 2020 p17 INQY1000060
(2076) Thomas Griffiths Transcript 2 July 2019 pp46-54 INQY1000025
(2077) ANON Transcript 10 July 2019 pp163-167 INQY1000031
(2078) Written Statement of Dr Audrey Dawson para 15 WITN3503001
(2079) Graeme Malloch Transcript 9 July 2019 p70 INQY1000030
(2080) Gerald Stone Transcript 23 July 2019 pp 48-52 INQY1000033
(2081) Written Statement of Colin Catterall para 11 WITN1145001
(2082) Written Statement of ANON para 17 WITN3245001
(2083) Written Statement of Rosamund Cooper para 12 WITN1168001
(2084) ANON Transcript 21 May 2019 pp85-86 INQY1000009, Written Statement of Professor Elizabeth Mayne para 3.1 WITN0736001
(2085) ANON Transcript 23 May 2019 pp83-84 INQY1000011
(2086) “I bumped into the senior registrar … and I said to him, ‘Oh, that blood test that you took off me, did you ever get the results for it?’ And he said, ‘Oh, yeah’, he said, ‘Yeah, you’re positive’, and just kind of walked off.” Bruce Norval Transcript 9 June 2021 pp8-9 INQY1000126
(2087) Colette Wintle Transcript 10 May 2019 pp140-148 INQY1000008
(2088) Virology results of Simon Hamilton WITN2339004
(2089) Simon Hamilton Transcript 22 May 2019 pp7-9 INQY1000010, Medical records extract of Simon Hamilton March 1994 WITN2339010
(2090) Written Statement of ANON paras 50-56 WITN5353001
(2091) Expert Report to the Infected Blood Inquiry: Medical Ethics April 2020 INQY0000241, Medical Ethics Expert Panel Transcript 26 January 2021 INQY1000090, Medical Ethics Expert Panel Transcript 27 January 2021 INQY1000091
(2092) Medical Ethics Expert Panel Transcript 26 January 2021 pp33-37 INQY1000090
(2093) (Professor Bobbie Farsides) Medical Ethics Expert Panel Transcript 26 January 2021 p29 INQY1000090
(2094) (Professor Julian Savulescu) Medical Ethics Expert Panel Transcript 26 January 2021 pp32-33 INQY1000090
(2095) (Professor Julian Savulescu) Medical Ethics Expert Panel Transcript 26 January 2021 p136 INQY1000090
(2096) Medical Ethics Expert Panel Transcript 26 January 2021 pp108-113 INQY1000090
(2097) Dr Rizza in his report for the HIV Haemophilia Litigation asserted, when dismissing the option of reverting to cryoprecipitate, that “few patients given the lack of knowledge of AIDS and its implications were prepared to modify their treatment and life routine to such an extent.” Health Authority Defendants Report by Dr Charles Rizza p136 HCDO0000394. However, this was almost certainly retrospective wishful thinking on his part: an assumption as to what patients would do and also an admission that patients were not given the information to make an informed choice. In general, patients were not given the option to revert to cryoprecipitate, nor were they given the information about risks that would have enabled them to make an informed decision, nor were regional transfusion directors asked if they could make more cryoprecipitate which the Inquiry has heard they could have done. See the chapter on the Blood Services and Addressing Risk: Response.
(2098) (Professor Bobbie Farsides) Medical Ethics Expert Panel Transcript 27 January 2021 p9 INQY1000091
(2099) (Professor Ian Kerridge) Medical Ethics Expert Panel Transcript 27 January 2021 p10 INQY1000091
(2100) John McDougall Transcript 3 July 2019 pp51-2 INQY1000026. As John told the Inquiry, there was no discussion with parents about the risks: “What he [Dr Willoughby] certainly didn’t do was to discuss it with the parents or discuss it with us or to discuss it with other parents and to come to a consensus.” John McDougall Transcript 3 July 2019 p60 INQY1000026
(2101) As the ethics panel explained, truth telling is a “central ethical duty”(Professor Emma Cave) and “From an ethical perspective, the goal is that the patient understands the situation and is able to navigate their life and the options that are available to them. So if you are not fully candid and including not telling the origin of the infection, you will close off options, such as the ability to seek rectification, the ability to exercise their legal rights and various other options that they are entitled to, even though the pursuit of those options will go against the interests of the doctor or the health system.” (Professor Julian Savulescu) Medical Ethics Expert Panel Transcript 27 January 2021 pp38-40 INQY1000091
(2102) (Dr Melinee Kazarian) Medical Ethics Expert Panel Transcript 27 January 2021 p20 INQY1000091
(2103) Medical Ethics Expert Panel Transcript 26 January 2021 pp79-82 INQY100090. As the expert panel noted, there is a distinction between two kinds of reasons: explanatory reasons and justificatory or normative reasons: “something can be an explanatory reason without it necessarily justifying it, and often those two kinds of reasons are run together but they are completely separate. One is descriptive and one is ethical or normative.”
(2104) This is the Report of a public inquiry that is intended to be accessible to the public. It is not necessary for the Inquiry, in fulfilling its terms of reference, to identify the chain of corporate responsibility involved in each and every decision taken decades earlier. It is not the role of the Inquiry to determine matters of civil liability – indeed, the Inquiry is precluded from so doing by section 2(1) of the Inquiries Act 2005.
(2105) It was generally the case that UK companies held the product licences for factor concentrates and were responsible for importing them into the UK and selling and supplying them to customers here. In contrast, the US (or in the case of Immuno, Austrian) companies were much larger entities that conducted the research and development that produced the concentrates and were responsible for obtaining the source plasma and for manufacture. The evidence seen by the Inquiry suggests that the UK companies had no material influence over matters such as the selection of plasma sources, pool sizes or approaches to donor screening or viral inactivation. For the users of blood products, however, these issues of corporate structuring were not important. Someone who was treated with (say) Factorate in an NHS haemophilia centre in the early 1980s would, understandably, consider himself to be receiving an Armour product, available because of the collective efforts of UK and US companies. It is therefore appropriate to adopt “Armour” as the relevant descriptor in this chapter and the same approach is taken for the other products.
(2106) Core participant status is voluntary: the Inquiry has no powers to compel a person to become a core participant.
(2107) As provided for under the Inquiry Rules 2006.
(2108) Starr Blood: An Epic History of Medicine and Commerce 1998 pp11-12 HSOC0019915
(2109) In respect of all of these products, the generic term is used to cover both the initial unheated product and later heat-treated variants, other than where is specified. The dates for the licences are taken from: Counsel Presentation on Overview Chronology of the Licensing of Commercial Blood Products in the United Kingdom during the 1970s and 1980s 6 December 2022 INQY0000411 (and its Appendix 1: Counsel Presentation on Overview of Commercial Blood Products 6 December 2022 INQY0000412), where further details can be found of the dates on which variations to the licence were granted, including in respect of heat treatment.
(2110) There were exceptions. As discussed in the chapter on Regulation of Commercial Factor Concentrates, Speywood Laboratories Limited, an independent company, held the product licence for Koate from 1976 to early 1980. From September 1979 until February 1985 the product licence for Profilate was held by a German registered company, Alpha Therapeutic GmbH.
(2111) Counsel Presentation on Overview Chronology of the Licensing of Commercial Blood Products in the United Kingdom during the 1970s and 1980s 6 December 2022 INQY0000411 (and its Appendix 1: Counsel Presentation on Overview of Commercial Blood Products 6 December 2022 INQY0000412)
(2112) As is discussed in the chapter on Viral Inactivation, commercially produced heat-treated Factor 9 was available before an equivalent NHS product in 1984 and 1985, which led to an increase in the use of such commercial products in this period.
(2113) Letter from J Ludgate to Regional Hospital Boards and others 24 October 1973 DHSC0003741_025, Memo from G Drewe and R Tunnard to Dr William d’A Maycock and others 25 June 1974 DHSC0100005_138. The contract price was 10p per IU. See the chapter on Regulation of Commercial Factor Concentrates.
(2114) Memo from G Drewe and R Tunnard to Dr Maycock and others 25 June 1974 p1 DHSC0100005_138
(2115) Memo from G Drewe to Dr Sheila Waiter 21 December 1976 DHSC0003719_118. The figures for the price per unit correlate closely with: Survey of commercially-produced and NHS-produced Factor VIII concentrates 11 March 1976 p4 DHSC0100007_004, Counsel Presentation on Pharmaceutical Companies Transcript 5 October 2021 p65 INQY1000152
(2116) Factorate High Purity.
(2117) Memo from C Wrigglesworth to John Parker and others 28 June 1983 p2 DHSC0002229_055. The minute also records that 0.8 million IU of Prothromplex, Immuno’s Factor 9 product, and 1.5 million IU of FEIBA, its product for inhibitor patients, were used. These have not been included when calculating the percentage proportions of the market share cited here. Some of the companies provided a range for the amount of product sold in the UK rather than a precise figure (eg Armour said that it sold between 15 and 20 million IU of Factorate). Where this was done, a mid-point has been used to calculate the percentage figures cited.
(2118) Counsel Presentation on Pharmaceutical Companies Transcript 5 October 2021 pp108-131 INQY1000152
(2119) Minutes of Haemophilia Reference Centre Directors meeting 13 February 1989 p1 HCDO0000432
(2120) See the chapter on Self-Sufficiency.
(2121) Starr Blood: An Epic History of Medicine and Commerce 1998 pp249-266 HSOC0019915
(2122) Starr Blood: An Epic History of Medicine and Commerce 1998 p251 HSOC0019915. The Inquiry has also heard evidence that Hyland operated a plasma centre in Puerto Rico until 1980, and in Lesotho until 1976. The latter was described in an internal document as “our only African plasma centre.” Memo from Maggie Eras to Dr Jeanne Noel 23 August 1985 p1 SHPL0000735_006
(2123) There are different theories as to the origin of AIDS, and why it should emerge in the late 1970s in the West Coast urban population of the US. Phylogenetic studies suggest that AIDS may have originated in Central and West Africa. Some theories centre on the fact that Haiti has a large French-speaking population, as does the Democratic Republic of Congo, and when its mineral wealth was exploited in the early twentieth century, engineers were recruited from Haiti to work there, since they spoke the language. As single men in a rapidly expanding urban environment it is postulated many were infected by local sex workers, who in turn may have been infected from eating bush meat from their villages where that bush meat had been infected by a zoonosis by which the virus causative of AIDS had spread from a simian species to humankind. An alternative possibility is that there was a UN programme to replace European administrators in Africa, so not only engineers but also doctors, teachers and lawyers travelled from Haiti. It is postulated that these engineers returning to Haiti in the early twentieth century, or those doctors, teachers, lawyers and engineers returning after the UN programme may have brought the infection with them to Haiti, and from there it may later have spread to homosexual men from the West Coast of the US for whom Haiti was a congenial holiday spot. Gilbert et al The emergence of HIV/AIDS in the Americas and beyond Proceedings of the National Academy of Sciences 20 November 2007 PRSE0003804
(2124) Starr Blood: An Epic History of Medicine and Commerce 1998 pp249-266 HSOC0019915
(2125) Starr Blood: An Epic History of Medicine and Commerce 1998 pp246-247 HSOC0019915
(2126) Starr Blood: An Epic History of Medicine and Commerce 1998 p247 HSOC0019915. The Bureau of Biologics and, from 1982, the Center for Drugs and Biologics, were the divisions of the FDA that had principal responsibility for blood products. For ease of reading, reference is made in this chapter to the FDA generically and this is intended to include the Bureau and the Center.
(2127) Counsel Presentation on Pharmaceutical Companies Transcript 24 September 2021 pp90-92 INQY1000147, Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p1 CBLA0000011_005
(2128) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 pp5-6 CBLA0000011_005. Dr Kingdon was medical director 1981-1984, vice president and medical director 1984-1990 and vice president and general manager from 1990 at Hyland Division. CV of Dr Henry Shannon Kingdon 14 August 1990 p1 CBLA0000011_076
(2129) As noted below, evidence seen by the Inquiry suggests that the FDA were prepared to license (and hence presumably inspect) a plasmapheresis plant in Belize as of 1984. This information came from a representative of Cutter, and it is possible that Dr Kingdon was unaware of this apparent exception. Draft Minutes of Infectious Hazards of Blood Products meeting 9 February 1984 p6 PRSE0003071
(2130) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p6 CBLA0000011_005
(2131) See the chapter Hepatitis Risks 1970 and After.
(2132) See the chapter Hepatitis Risks 1970 and After.
(2133) World Health Organization World Health Assembly Resolution 28 May 1975 p1 PRSE0003476
(2134) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p12 CBLA0000011_005. A letter sent by the US Assistant Secretary for Health to the UK Chief Medical Officer, date stamped 25 November 1975, confirmed that, by that date “Source plasma used in manufacturing licensed plasma derivatives, in the US or overseas, must be collected in facilities with US licenses.” Letter from Dr Theodore Cooper to Dr Henry Yellowlees 25 November 1975 pp1-2 DHSC0100001_036
(2135) An advantage it expressed clearly in the foreword to its report: “One of the advantages of conducting this study at this time is that many of the key participants in the 1982-1986 decisionmaking were available to speak to the Committee and staff. The Committee believed it was critical to hear firsthand accounts of the assumptions and beliefs that influenced critical decisions about the safety of the blood supply. Fact-finding interviews were held with 76 individuals knowledgeable about all aspects of the blood supply system. These interviews included representatives of FDA, CDC [Centers for Disease Control], NIH [National Institutes of Health], NHF [National Hemophilia Foundation], the Office of the Assistant Secretary of Health, industry, and blood banks; physicians and scientists; and individuals with hemophilia.” Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 p7 JREE0000019
(2136) “A formal compliance program for the plasma fractionation industry was established in 1977.” It noted that source identification for plasma (ie whether from a paid or voluntary donor) did not apply, though it did for whole blood for transfusion from 1978. Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 p65 JREE0000019
(2137) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p45 CBLA0000011_005. It should be noted that this was a reference to a heat-treated concentrate in the 1980s.
(2138) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 pp4-5 CBLA0000011_005
(2139) Sir Michael Rawlins Transcript 7 June 2022 p41 INQY1000211
(2140) Starr Blood: An Epic History of Medicine and Commerce 1998 p247 HSOC0019915
(2141) Written Statement of Dr Duncan Thomas para 2.17 WITN6405001
(2142) Its principal concern was the way in which it handled the question whether potentially contaminated batches should be recalled – rather than any criticism of its inspection regime.
(2143) Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decision making 1995 pp149-180, p227, pp242-243 JREE0000019
(2144) Armour Pharmaceutical Company Ltd application for Factor VIII product licence DHSC0003742_078, Annex C Factor 8 Product Licence Applications DHSC0003742_080
(2145) This is consistent with information provided in the product licence application for Abbott’s Factor 8 concentrate, Profilate. This specified that plasma was obtained from locations in California, Arizona, Texas, Oregon and Washington by United Biologics donor centres, which was owned by Abbott. See the report of Dr Thomas in November 1974: Abbott Laboratories Ltd application for Antihemophilic Factor product licence November 1974 pp2-3 MHRA0000091_005. A later variation to the product licence application added further donor centres, all still in the continental US, but now including those run by a second company, American Blood Components. No information was provided about the ownership and management of American Blood Components, but it appears to be a plasmapheresis company. Letter from J Marriott to Dr Mary Duncan 14 January 1975 p2 MHRA0000091_012
(2146) The application was withdrawn and Speywood took over the application. By the time the licence was granted, Cutter had confirmed that all plasma was being collected from FDA licensed and inspected centres. Letter from J M Boult to Medicines Division at DHSS 18 August 1976 BAYP0000001_123, Letter from Lori Evans to J M Boult 25 February 1976 WITN6984054, Letter from J M Boult to R D Andrews 4 March 1976 BAYP0000001_113. No products were provided under licence to the UK until 1976.
(2147) The approach taken by Immuno to the sourcing of plasma, and its successful application to vary the licence to allow for the use of American plasma is considered in detail in the chapter on Regulation of Commercial Factor Concentrates.
(2148) Armour Pharmaceutical Company Ltd application for Factor VIII product licence p1, p5 DHSC0003742_078
(2149) Letter from DHSS to C Collins 31 July 1984 p9 ARMO0000320
(2150) Letter from S Brooks to G Deveney 2 February 1976 p2 ARMO0000005
(2151) Written Statement of Robert Christie 10 November 2022 para 31(c) WITN7500001. It should be noted that Robert Christie gave this statement more than 45 years after the original Factorate licence application, at a time when he was 90 years old. It does not follow from what he says in his statement that he would not have known more about the sources of plasma at the time of the licence application. He joined Armour Pharmaceutical Company Ltd in 1956 and retired from it in 1997, working as a consultant on a part-time basis for a number of years thereafter. He was employed by the UK company and hence was not responsible for decisions made on how plasma should be obtained by the US parent company for use in the manufacture of blood products. He was, however, responsible for matters related to the licensing and regulation of blood products in the UK. Written Statement of Robert Christie 10 November 2022 paras 1-2, 7 WITN7500001
(2152) Armour Pharmaceutical Company Ltd application for High Potency Factorate product licence 20 November 1978 p14 ARMO0000023
(2153) In his report of visit to plasmapheresis centres in 1980, discussed further below, Dr Peter Jones commented that: “It is imperative that the Revlon Health Care Group [which owned Armour] became totally self-sufficient in terms of source plasma.” Emphasis in the original. Revlon Health Care Group Report on Plasmapheresis in the United States June 1980 p26 PJON0000040_001
(2154) Armour Plasma Perspectives No1 July 1981 p2 ARMO0000229
(2155) Telex from Dr Michael Rodell to W Tarbit 23 June 1983 ARMO0000263. There is some ambiguity in that telex exchanges before this one suggested that Armour might still, on occasion, be reliant on external purchases, but when read together it seems that this may have been a provisional view expressed by the officers of the UK subsidiary before the definitive answer was received from Dr Rodell of the US parent company: see Telex from W Tarbit to Dr Rodell 20 June 1983 ARMO0000264, Telex from H L Shaw to KAS Egerton 21 June 1983 p1 ARMO0000266, Counsel Presentation on Pharmaceutical Companies Transcript 29 September 2021 p69 INQY1000149
(2156) Puerto Rico was, and is, an unincorporated US territory with local self-government.
(2157) Note of Dr Cleghorn interview 9 October 1975 p1 MGIL0000053. An internal Hyland document from 1985 records that the Puerto Rico plasma centre was not closed until 1980, which implies that it was available as a base material for US production. This does not however conclusively establish that plasma from that plant was used in the production of factor concentrates until then, or that it was used in other blood products that were provided to the UK. Its Mexican centre, harvesting Mexican plasma, did not close until the following year, 1981. Memo from Maggie Eras to Dr Noel 23 August 1985 p1 SHPL0000735_006
(2158) Many of these are not attributed to sources who had actual knowledge of what they were describing, and so would better justify the word “rumours”: they are called reports because some would be reasonably reliable hearsay, such as Dr Jones’ account which follows.
(2159) Memo to Dr Jones 17 September 1979 p1 PJON0000055_001
(2160) Peter Coombes worked for Immuno Ltd 1976-1997 and was a marketing manager 1979-1982 before becoming the marketing director. Written Statement of Peter Coombes 15 March 2022 paras 2.4-2.8, para 23.5 WITN6409001
(2161) Memo from Maggie Eras to Dr Noel 23 August 1985 p1 SHPL0000735_006
(2162) Memo from C Chard to G Hardy 2 February 1979 p1, p3 PJON0000054_001, Counsel Presentation on Pharmaceutical Companies Transcript 28 September 2021 pp56-61 INQY1000148. The documents discussed, which date from February 1979, indicate that plasma from Lesotho and Belize was used in albumin products that were sent to the UK, contrary to the terms of the UK licence. The recommendation from the author of the report was that “this should be submitted to the DHSS or plasma from these sources should not be used for UK products.” The Inquiry has not been able to identify what steps, if any, were taken in response.
(2163) Written Statement of Edward Harriman paras 5-23 WITN0696001. It should be pointed out that the source, Dr Ramos, was someone who has been blamed for the assassination of a newspaper editor, had been denied entry to some Central American states and expelled from three, ran a business which from Ed Harriman’s description was sensitive to inquiry being made about it, and there is no independent verification of what he had had to say. Ed Harriman’s article went on to note that “Not surprisingly, Dr Z F Hantchef, head of the Red Cross’s Blood Transfusion Service in Geneva, hotly denies Ramos’s claim. For years, he has been speaking out against unscrupulous dealers.” New Scientist Blood Money 13 March 1980 p2 WITN0696003. The words “not surprisingly” echo a desire to have some objective verification of what Ed Harriman had been told. The Inquiry has found no such evidence, since there is no document to suggest that blood products derived from Plasmaferesis plasma were used in the UK.
(2164) New Scientist Blood Money 13 March 1980 p2 WITN0696003. The Inquiry has no independent verification of this.
(2165) Written Statement of Edward Harriman para 26 WITN0696001
(2166) Memo from C Wrigglesworth to John Parker 28 June 1983 DHSC0002229_055. In the case of Immuno, some of their plasma also came from European plasmapheresis centres.
(2167) Product Licence Application for Koate Attachment 5 - List of Source Plasma (Human) Centers 8 February 1983 pp2-5 BAYP0000002_169, Hyland Division of Travenol Laboratories Limited: Source Plasma (Human) October 1983 pp29-30 BAXT0000011_002. The Travenol document does refer, without further details to “Cherry Street Plasma Center, Inc.” but it is a reasonable inference that this was also located in the US and that the lack of a full address was an administrative error.
(2168) Abbott Laboratories Ltd application for Antihemophilic Factor product licence November 1974 pp2-3 MHRA0000091_005, Annex C Factor 8 Product Licence Applications DHSC0003742_080
(2169) Draft Minutes of Infectious Hazards of Blood Products meeting 9 February 1984 pp5-6 PRSE0003071. This seems likely to have been that run by Plasmaferesis, as described by Ed Harriman above.
(2170) Travenol Laboratories Ltd application for Hemofil product licence January 1973 p15 DHSC0105593_006
(2171) World in Action Blood Money Transcript 1 and 8 December 1975 pp4-7 PRSE0004591
(2172) World in Action Blood Money Transcript 1 and 8 December 1975 p8 PRSE0004591
(2173) Starr Blood: An Epic History of Medicine and Commerce 1998 p256 HSOC0019915
(2174) Dr Gray produced a 286 paragraph witness statement including five full annexes. In it, he addressed issues of relevance to the Inquiry with contemporaneous documents. He summarised his views at the conclusion, and ended by saying: “On behalf of Bayer [he had earlier defined this as “Bayer plc”] I would like to say that we are truly sorry that this tragic situation occurred and that therapies that were developed by us, and that were prescribed by doctors to save and improve lives, in fact ended up causing so much suffering to so many.” Written Statement of Dr Brendon Gray paras 283-285 WITN6984001. Other pharmaceutical companies did not provide equivalent statements.
(2175) Written Statement of Dr Brendon Gray paras 63-65, pp119-120 WITN6984001
(2176) Written Statement of Dr Brendon Gray p119 WITN6984001
(2177) Instruction Booklet for Plasmapheresis Inspection Checklist and Report Form 1 September 1981 p3 WITN6984016
(2178) Written Statement of Dr Brendon Gray para 63 WITN6984001
(2179) Written Statement of Dr Brendon Gray para 65 WITN6984001. Examples of the Cutter System of Plasmapheresis documents can be found at: Letter from Dr John Petricciani to Dr Steven Ojala 4 January 1982 WITN6984018, Letter from Dr Moshe Sternberg to Dr Elaine Esber 7 July 1987 BAYP0005978
(2180) Written Statement of Dr Brendon Gray para 66 WITN6984001
(2181) See, for example, the discussion of the Travenol procedures, as set out in 1976 and 1977 documents that formed part of the Donor Centre Technical Guide. Counsel Presentation on Pharmaceutical Companies Transcript 28 September 2021 pp29-32 INQY1000148, Travenol Laboratories Guidance for Donor Requirements Check List 30 April 1976 SHPL0000279_012, Travenol Laboratories Guidance for Permanent Donor Records 11 May 1976 SHPL0000279_031, Travenol Laboratories Guidance for Source Plasma (Human) Label 29 October 1976 SHPL0000279_029, Travenol Laboratories Guidance for Whole Blood and Plasma Processing Log 18 January 1977 SHPL0000279_018
(2182) Revlon Health Care Group Report on Plasmapheresis in the United States June 1980 p11, pp19-20 PJON0000040_001. Armour subsequently stated publicly that Dr Jones’ recommendations “have been implemented wherever possible in order to maintain the highest standards throughout the Plasma Alliance Group.” Emphasis added. Armour Plasma Perspectives No1 July 1981 p8 ARMO0000229. The circumstances in which Dr Jones was invited to make the inspection are described at: Memo to Dr Jones 17 September 1979 pp3-4 PJON0000055_001, Counsel Presentation on Pharmaceutical Companies Transcript 29 September 2021 pp29-54 INQY1000149
(2183) Memo from Stewart Mueller to W Biles 27 April 1983 p1 ARMO0000243. The term “recently” suggests a favourable comparison with the situation not quite so recently, but the Inquiry has no details.
(2184) Memo from Robert Spiller to Dr Harry Meyer 7 May 1982 pp3-4 MULL0003336
(2185) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p6 CBLA0000011_005
(2186) Deposition of William Hartin Transcript 24 April 1989 p184 MULL0000282
(2187) Letter from Dr Rodell to Dr Paul Kaufman 3 August 1982 p3 CGRA0000287, Memo from Dr Ojala to Dr Wilhelm Schaeffler and others 13 December 1982 p1 CGRA0000425
(2188) Memo from William Srigley to David Castaldi 20 October 1983 p2 CGRA0000291, Counsel Presentation on Pharmaceutical Companies Transcript 28 September 2021 pp38-41 INQY1000148
(2189) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p45 CBLA0000011_005. It should be noted that this was a reference to a heat-treated concentrate in the 1980s.
(2190) Written Statement of Dr Brendon Gray para 86 WITN6984001
(2191) Memo from Robert Barden to Dr John Hink 3 June 1982 p1 MULL0000913_017
(2192) These were Arizona State Prison, the Southern Desert Correctional Center and the Northern Nevada Correction Center. Product Licence Application for Koate Attachment 5 - List of Source Plasma (Human) Centers 8 February 1983 pp2-3 BAYP0000002_169. There is no documentary evidence to suggest that the DHSS took any particular note of the fact that prisons were on the list of the plasmapheresis centres from which Cutter obtained source material.
(2193) Dr Hink was at that time director of plasma procurement for Cutter. Memo from Dr Hink to Dr K Fischer and others 6 January 1983 pp3-4 CGRA0000300, Summary Report on Workgroup to Identify Opportunities for Prevention of Acquired Immune Deficiency Syndrome 4 January 1983 CGRA0000301. The meeting on 4 January 1983 is discussed further below. After February 1983, the evidence is that any remaining stocks of factor concentrates that had been prepared by Cutter using prison plasma were used for research and development purposes only. Minutes of Biological Management Committee meeting 15 February 1983 p2 BAYP0004434
(2194) Written Statement of Dr Brendon Gray paras 88-89 WITN6984001, Deposition of Edmund Potere Transcript 7 April 1995 pp44-45 MULL0000417
(2195) Cutter Laboratories Inspection Instructions for Fractionation Runs of Plasma Products 16 March 1983 p4 WITN6984027
(2196) Cutter pushed back on this, since “prison plasma was the source of Cutter Inc’s hyperimmunised donors”, whereupon the FDA suggested that it be excluded from production of factor concentrate. Written Statement of Dr Brendon Gray para 88 WITN6984001
(2197) Deposition of prisoner at Wade Prison and Louisiana State Penitentiary Transcript 4 August 1998 MULL0000531. It should be noted that this prisoner was first incarcerated at Wade in 1986 or 1987, and at Louisiana State Penitentiary in 1990, so after the period of time of most relevance to this Report. However, this is open to the comment that if after it had become notorious that prison plasma might give rise to a disproportionate risk of transmitting AIDS these practices were happening, then how much worse were they before the risk of plasma transmitting AIDS was fully appreciated?
(2198) Deposition of prisoner at Louisiana State Penitentiary Transcript 4 August 1998 MULL0000532
(2199) Deposition of prisoner at Wade Prison and Louisiana State Penitentiary Transcript 4 August 1998 p12 MULL0000531, Deposition of prisoner at Louisiana State Penitentiary Transcript 4 August 1998 pp19-20 MULL0000532
(2200) Deposition of prisoner at Wade Prison and Louisiana State Penitentiary Transcript 4 August 1998 pp12-13, p16, pp18-19 MULL0000531
(2201) Deposition of prisoner at Wade Prison and Louisiana State Penitentiary Transcript 4 August 1998 pp13-15, p17 MULL0000531, Deposition of prisoner at Louisiana State Penitentiary Transcript 4 August 1998 p24 MULL0000532
(2202) Deposition of prisoner at Louisiana State Penitentiary Transcript 4 August 1998 p22 MULL0000532
(2203) Amongst practices reported to him were pimps amongst the male inmates sending their male prostitutes to be bled; the widespread use of bribery or the use of alternative names to enable donations to be made which appeared within regulation, the re-use of tubing from one person to another; the switching of labels, a practice of inmates bleeding inmates, and a discovery that more than 38 persons who were ineligible to sell their blood had done so regularly twice a week for over a year. Written Statement of Kelly Duda paras 68, 73, 86, 89-92, 114 WITN0838001
(2204) Written Statement of Kelly Duda para 104, para 108, para 110, paras 117-118, para 120, para 122 WITN0838001. The FDA had suspended ADC’s licence to distribute plasma on 5 August 1983, given notice to revoke on 21 February 1984 and in March 1984 ADC voluntarily surrendered the licence to distribute plasma and it was revoked on 17 May 1984.
(2205) Written Statement of Kelly Duda para 161 WITN0838001 and a copy of the letter Kelly Duda wrote to a QC about this: Letter from Kelly Duda to Stephen Grimes 12 November 2003 p2 WITN0838032
(2206) Written Statement of Dr Brendon Gray para 86 WITN6984001
(2207) Memo from Dr Ojala to Dr Schaeffler and others p1 13 December 1982 CGRA0000425
(2208) Memo from Dr Ojala to Dr George Akin and others 15 April 1985 p2 CGRA0000545, Written Statement of Robert Christie 10 November 2022 para 31c WITN7500001
(2209) Letter from Thomas Drees to Charles Carman and Dr Louis Aledort 9 November 1982 CGRA0000262. See also an internal training document dated 15 December 1982, which stated that “Alpha does not collect plasma from penal institutions.”Memo from Alpha Sales Department to Sales Force Regional Managers 15 December 1982 CGRA0000376
(2210) Letter from Dr Clyde McAuley to Hemophilia Treatment Centers 22 December 1982 CGRA0000265
(2211) Deposition of Dr Edward Shanbrom Transcript 30 October 2002 p7 CGRA0000495
(2212) Memo from Robert Spiller to Dr Harry Meyer 7 May 1982 pp3-4 MULL0003336
(2213) See the chapter on Blood Services and Addressing Risk: Response.
(2214) “Antibody” and “immunoglobulin” are interchangeable labels.
(2215) See for example the advertisements for donors at: Advocate The National Gay News Magazine advertisements 9 July 1981 UCSF0000058, Blood plasma donation advertisement 13 May 1982 MULL0006827_015, Trimar and Alpha blood plasma donation advertisements CGRA0000204_018, Hyland Plasma Centre advertisement 3 December 1982 CGRA0000294_053 among other examples.
(2216) Trimar blood plasma donation advertisement 13 May 1982 MULL0006827_015
(2217) Trimar and Alpha blood plasma donation advertisements p2 CGRA0000204_018
(2218) See the chapter on Knowledge of the Risks of AIDS.
(2219) Dr Kingdon, vice president and general manager at Hyland Division, recorded in January 1983 that Hyland had been closely monitoring AIDS since December 1981. Memo from Dr Kingdon to Sharon Northup 5 January 1983 CGRA0000668. William Srigley of Cutter Pharmaceutical was aware before July 1982 (“very early”) that a homosexual donor who was hepatitis positive risked transmitting AIDS. Deposition of William Srigley 1 May 1995 p79 MULL0000490
(2220) See for example: Cossart et al Post-Transfusion Hepatitis in Australia The Lancet 23 January 1982 p5 NHBT0000080_004; and the chapter on Hepatitis C Surrogate Screening generally.
(2221) See the chapter on Hepatitis C Surrogate Screening.
(2222) These were produced at a fourth or fifth stage of fractionation, and the process of fractionation appears to have some effect in lessening the likelihood of viral transmission.
(2223) Trimar and Alpha blood plasma donation advertisements p2 CGRA0000204_018. The date is likely to be May or June 1982 from the announcements.
(2224) It did so until mid 1982 – see the combined effect of a letter from Cutter reporting in one paragraph on Hyland’s policy of collecting plasma for anti-HBs, but not making AHF from it, and a letter of 9 December 1982 which ascribes this policy to having been in operation for “several months”. Memo from Dr Hink to Dr Lee Hershberger 30 August 1982 BAUM0000008, Letter from Dr Rodell to Charles Carman and Dr Aledort 9 December 1982 CGRA0000655
(2225) Counsel Presentation on Pharmaceutical Companies Transcript 28 September 2021 pp66-79 INQY1000148, Memo from Dr Hink to Dr Lee Hershberger 30 August 1982 p1 BAUM0000008, Letter from Dr Rodell to Charles Carman and Dr Aledort 9 December 1982 p2 CGRA0000655. See also extracts from the deposition of William Hartin of Alpha on 27 April 1995, in which he accepted that the “standard” procedure was for Alpha to mix high-titred plasma with other plasma in pools used to make factor concentrates. Although he noted that there were exceptions to this practice, the examples that he gave did not include the exclusion of plasma intentionally obtained from gay men in order to produce immunoglobulins. It is important to note that the Inquiry holds extracts from William Hartin’s deposition and does not have the whole transcript. Extracts from Deposition of William Hartin Transcript 27 April 1995 pp21-22 MULL0000040
(2226) Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 pp242-243 JREE0000019. This is not a criticism, here, of the FDA approach, but rather a statement of fact.
(2227) Letter from Dr Rodell to Dr Meyer 15 September 1982 CGRA0000246, Internal Cutter Memo from Dr Hershberger 9 September 1982 p2 CGRA0000330
(2228) Letter from Dr Rodell to Charles Carman and Dr Aledort 9 December 1982 p2 CGRA0000655. Emphasis added.
(2229) Letter from Marietta Carr to Dr Meyer 30 August 1982 CGRA0000277
(2230) Letter from Marietta Carr to Dr Meyer 7 September 1982 CGRA0000657
(2231) Letter from Thomas Drees to Charles Carman and Dr Aledort 9 November 1982 CGRA0000262. With regard to the claim that “We have no centers … in San Francisco”, an internal memorandum dated 15 December 1982 recorded a list of action points from what was described as an AIDS meeting that had taken place that day and one of these referred to “our recently closed San Francisco center”. Emphasis added. Memo from Edward Mealey to the Executive Committee 15 December 1982 p1 CGRA0000599. An Alpha plasma centre in San Francisco was listed in an advertisement seeking donors that was placed in a gay newspaper in July 1981. Advocate The National Gay News Magazine advertisements 9 July 1981 p3 UCSF0000058
(2232) Memo from Dr Hink to Dr Hershberger and others 30 August 1982 p2 MULL0007803
(2233) Dr Hershberger was director of regulatory affairs for Cutter. Internal Cutter Memo from Dr Hershberger 9 September 1982 p2 CGRA0000330
(2234) Memo from Dr Hink to Dr Hershberger and others 30 August 1982 p2 MULL0007803
(2235) Memo from Dr Hink to Dr Hershberger and others 30 August 1982 p1 MULL0007803
(2236) Internal Cutter Memo from Dr Hershberger 9 September 1982 p2 CGRA0000330
(2237) “Our data would suggest that ... due to the high risk of gonorrhea, syphilis, and hepatitis B for homosexuals, it would seem that they should be advised to refrain from blood donations.” Szmuness et al On the Role of Sexual Behavior in the Spread of Hepatitis B Infection Annals of Internal Medicine October 1975 p6 CGRA0000648
(2238) Expert Witness Report of Dr Donald Francis in US litigation 2 October 2002 pp2-3 CGRA0000404
(2239) Prior to August 1982 there was no regulation or recommendation from the FDA which prevented the use of plasma from male homosexual populations.
(2240) See the chapter on Regulation of Commercial Factor Concentrates.
(2241) Expert Witness Report of Dr Donald Francis 2 October 2002 p6 CGRA0000404. Emphasis in original.
(2242) Expert Witness Report of Dr Donald Francis 2 October 2002 p7 CGRA0000404
(2243) He finished by adding: “Instead, Cutter viewed the problem in terms of political manoeuvring to maintain a profitable plasma source, rather than recognizing the danger to hemophiliac patients in continuing to market the products.” Expert Witness Report of Dr Donald Francis 2 October 2002 p7 CGRA0000404
(2244) Written Statement of Dr Brendon Gray para 71 WITN6984001. The relevant regulation was #640.102(d) Manufacture of Immune Serum Globulin (Human): Extract from the Code of Regulations: Food and Drugs Administration 1974 pp3-4 WITN6984022. Similar points were made in an expert report dated 5 October 1994 and produced by Dr Milton Mozen, of Cutter, in US litigation. Expert Report of Dr Milton Mozen 5 October 1994 p14 WITN6407003
(2245) Letter from S Brooks to G Deveney 2 February 1976 p1 ARMO0000005
(2246) Letter from Christopher Bishop to Dr Rosemary Biggs November 1977 p1 OXUH0003868_011
(2247) Christopher Bishop Transcript 4 November 2021 pp43-44 INQY1000158
(2248) Christopher Bishop Transcript 4 November 2021 p49 INQY1000158
(2249) Written Statement of Robert Christie para 33b WITN7500001
(2250) Armour Plasma Perspectives No1 July 1981 p3 ARMO0000229
(2251) Armour Plasma Perspectives No1 July 1981 p2 ARMO0000229
(2252) Armour Plasma Perspectives No1 July 1981 p4 ARMO0000229
(2253) Travenol Laboratories Ltd application for Hemofil product licence January 1973 p15 DHSC0105593_006
(2254) Letter from G Hardy to Dr R Andrews 22 June 1976 p1 MHRA0033317_077. A litre of plasma in the UK would usually contain approximately 5 donations: since only plasma was being taken and the body replaces it much more quickly than it does red blood cells it may be that the donations of plasma taken by plasmapheresis were larger.Cutter suggested in an application to license Koate in 1976 that the donation size it used was 600ml. If Hyland/Travenol used donations of the same size, a pool of 6000 litres would contain plasma from 10,000 donations.
(2255) Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p9 CBLA0000011_005
(2256) Letter from J Boult to Dr Andrews 27 February 1976 p2 IPSN0000312_109, Written Statement of Dr Brendon Gray para 79 WITN6984001
(2257) Letter from Dr Akin to Dr Leonard Klein 23 November 1983 BAYP0004975
(2258) Letter from Linda Frith to Dr Archibald Prentice, Dr Richard Lee, Dr G Smith and Mr Gardiner 21 October 1986 p1 BAYP0000009_030
(2259) Letter from Craig Simpson to Medicines Control Agency 2 November 1989 p4 BAYP0000005_143
(2260) Written Statement of Dr Brendon Gray paras 70-79 WITN6984001
(2261) Kernoff et al Letter to the Editor on Wet Heating for Safer Factor VIII Concentrate? The Lancet 28 September 1985 RLIT0000186
(2262) Serological Products Ltd application for Kryobulin product licence January 1973 p7 MHRA0033322_060
(2263) Product label for Kryobulin Red SHPL0000071_130. See also discussion of the date of this labelling. Counsel Presentation on Pharmaceutical Companies Transcript 24 September 2021 p31 INQY1000147
(2264) Packaging for Prothromplex TIM 4 29 November 1984 p8 SHPL0000168_025
(2265) Serological Products Ltd application for Kryobulin product licence January 1973 p5 MHRA0033322_060. See also the draft label provided with the product licence application for heat-treated Kryobulin in February 1985: Packaging for Kryobulin 15 March 1985 p4 SHPL0000067_044
(2266) Draft Minutes of NIBSC Infectious Hazards of Blood Products meeting 9 February 1984 p3 PRSE0003071. Dr Rodell recorded that he gave the summary of the commercial pool sizes and that “one donor probably would not contribute more than four units in a particular pool.” Memo from Marietta Carr to members of Alpha Operations Committee 21 February 1984 p3 CGRA0000610
(2267) Travenol said on 10 June 1975, in a meeting held with haemophilia centre directors in the wake of reports that Hemofil had caused an outbreak of hepatitis in Bournemouth, further discussed below, that: “the incidence of hepatitis B was explained by manufacture of stock-piled plasma, the donors of which had been screened only by CEP ... it was agreed that while we could expect a drop in cases of hepatitis B as material screened by HA [hemagglutination assay] and RIA [radioimmunoassay] techniques came through, the problem on non-B hepatitis would remain.” Letter from Dr Cleghorn to members of National Blood Transfusion Service 25 July 1975 OXUH0001590_001. Craske wrote in The Lancet in August 1975: “Testing the pooled plasma or the factor-VIII concentrate by the current radioimmunoassay techniques is not a reliable method of excluding hepatitis-B virus. Individual donations should be screened by R.I.A. before being pooled.” Craske An Outbreak of Hepatitis Associated with Intravenous Injection of Factor-VIII Concentrate The Lancet 2 August 1975 p3 PRSE0001794
(2268) There will come a point when the pool is of such a large size that it is probable that infection will follow use from within it.
(2269) Murray Viral Hepatitis Bulletin of the New York Academy of Medicine May 1955 MHRA0023509. See the chapter on Pool Sizes.
(2270) Trip Report of Meeting of Blood Products Advisory Committee on the Safety and Purity of Plasma Derivatives 19 July 1983 pp7-8 CBLA0000056_215. Dr J Derrick recorded the public meeting on 19 July 1983 of the Blood Products Advisory Committee of the Center for Biologics Evaluations and Research, a standing committee which advised the US Secretary of Health (and the FDA). Minutes of Blood Products Advisory Committee meeting 19 July 1983 pp2-3 BAYP0004674
(2271) Minutes of Blood Products Advisory Committee meeting 19 July 1983 p3 BAYP0004674
(2272) It should be noted that there is evidence of there having been some recalls, but there was no overriding principle applied as to the circumstances in which this should take place.
(2273) A colloquial way of expressing the lesson to be drawn from this is that in manufacturing medicinal products “don’t put all your eggs in one basket.”
(2274) The cheap sources from abroad declined after 1975; but plasmapheresis centres which operated in the US tended to be placed in large urban areas where there were substantial economically disadvantaged populations.
(2275) As the text makes clear, this was not a practice adopted by all companies, and most made efforts after August 1982 to avoid using hyperimmune plasma in making their products.
(2276) In general, the data sheets included in the ABPI compendium would be prepared or reviewed in the final quarter of the year before the compendium was published so that a data sheet appearing in the 1985-86 edition would have been prepared or reviewed in late 1984. Counsel Presentation on Pharmaceutical Companies Transcript 24 September 2021 p21 INQY1000147
(2277) Written Statement of Dr Brendon Gray para 120 WITN6984001
(2278) Letter from Marie Tatt to Elias Greene and others 15 September 1986 BAYP0000015_060, Fax from Elias Greene to Marie Tatt and others 15 September 1986 BAYP0000015_061, Written Statement of Linda Frith paras 155-158 WITN6407001. Koate HS was the variant heated in solution; it should be noted that Koate HS did not receive a licence in the UK. Written Statement of Dr Brendon Gray paras 242-250 WITN6984001
(2279) Written Statement of Peter Coombes para 45.2 WITN6409001
(2280) Written Statement of Ronald Feakes para 18.1, paras 20.2-20.4 WITN7302001
(2281) Written Statement of Robert Christie para 9, para 14 WITN7500001
(2282) Written Statement of Linda Frith paras 53, 56 WITN6407001
(2283) Christopher Bishop Transcript 4 November 2021 p17 INQY1000158
(2284) Written Statement of Robert Christie para 29 WITN7500001
(2285) Written Statement of Peter Coombes para 9.4, para 16, para 44.1, para 45.1 WITN6409001
(2286) Written Statement of Ronald Feakes para 7.1 WITN7302001
(2287) Patient information leaflets became a legal requirement in the UK for all medicines in 1999. Council Directive 92/27/EEC 31 March 1992 RLIT0002237
(2288) See for example the package insert for Koate, as submitted to the UK licensing authority in 1975 reproduced in the next section and the internal Cutter memorandum discussing the addition of a warning about AIDS 29 December 1982, which refers to the need to “demonstrate diligence in passing along whatever we do know to the physicians who prescribe the product.” Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 BAYP0000001_098, Memo from Edward Cutter to Jack Ryan and others 29 December 1982 p1 CGRA0000434
(2289) Appendix 5 of Travenol Laboratories Ltd application for Hemofil product licence p5 SHPL0000275_013
(2290) Travenol Laboratories Ltd application for Hemofil product licence January 1973 p4 DHSC0105593_006
(2291) Travenol Laboratories Ltd application for Hemofil product licence January 1973 p14 DHSC0105593_006. This conclusion is discussed in more detail in the chapter on Regulation of Commercial Factor Concentrates.
(2292) The recommendations of the meeting “made in order to limit as far as possible the incidence of hepatitis” were:
“1. Use of Factor VIII concentrate should be confined to severely affected haemophiliacs, and preferably to those haemophiliacs who have a history of frequent transfusion.
2. Young children and mildly affected haemophiliacs should always receive cryoprecipitate in preference to concentrate, unless there is an overriding clinical reason for using concentrate. (i.e., in the event of a severe bleed when Cryoprecipitate is not available, or for the treatment of factor VIII antibodies or when home therapy is strongly indicated.)
3. That Drs Cleghorn and Dane should explore the possibility of preparing immune plasma for use in a passive immunological protection programme by IV [intravenous] injection to haemophiliacs who are likely to receive concentrate.” Note from Dr Jones regarding Factor VIII Concentrates and Hepatitis June 1975 p1 PJON0000047_001
(2293) Letter from Dr Cooper to Dr Yellowlees 25 November 1975 p3 DHSC0100001_036
(2294) Letter from Dr Cooper to Dr Yellowlees 25 November 1975 pp2-3 DHSC0100001_036. It would follow that if plasma was supplied from Lesotho or Belize (for example) to the Travenol plant at Lessines in Belgium neither the plasma nor the manufacturing of the product would be subject to any US licensing requirements or regulatory control.
(2295) No reply from the Chief Medical Officer has been traced.
(2296) ie the generalised risk from products of this sort, rather than the “every lot is infective” type. If she meant the latter, it would mean that every time a doctor gave Hemofil to a patient they knew they were giving the patient infected material, and ought to have told the patient they would have treatment but would be put at serious risk of contracting Hepatitis B.
(2297) Letter from Dr Waiter to Dr Raison 30 December 1975 DHSC0100001_023
(2298) Draft Letter from Dr Maycock to Dr Raison 23 January 1976 pp1-2 DHSC0100001_018. By way of comment, Dr Maycock was here saying that US commercial products carried such risks of Hepatitis B (despite the availability of testing for Hepatitis B) that if UK factor concentrate was available the US products would be too risky to use. As has been considered in the chapter on Self-Sufficiency, this makes the point that there was a pressing health need to proceed to redevelop BPL immediately. As has been considered in the chapter on Hepatitis Risks 1970 and After, it confirms the view that the risks of Hepatitis B from commercial concentrate were significant, and that precautions were needed to meet them; and it demonstrates that non-A non-B Hepatitis was already known to be likely to become significantly problematic.
(2299) Serological Products Ltd application for Kryobulin product licence 11 December 1972 p25 SHPL0000071_181
(2300) Serological Products Ltd application for Kryobulin product licence 11 December 1972 p30 SHPL0000071_181
(2301) Letter from Dr Dane to Norman Berry 14 July 1975 p2 MHRA0033321_108. Emphasis in original.
(2302) Letter from Norman Berry to Dr Dane 15 July 1975 p2 MHRA0033321_105
(2303) Letter from Dr Dane to Norman Berry 18 July 1975 p1 MHRA0033321_102
(2304) Minute from Dr John Holgate to Dr Andrews 15 July 1975 MHRA0033321_107. A similar warning that “transmitting hepatitis cannot be entirely excluded”is contained in a data sheet in the ABPI Data Sheet Compendiums of 1978, 1979-1980, 1981-1982, 1984-1985 and 1985-1986. ABPI Data Sheet Compendium 1978 for Immuno Ltd: Prothromplex and Kryobulin p4 ABPI0000016, Counsel Presentation on Pharmaceutical Companies Transcript 24 September 2021 pp17-23 INQY1000147
(2305) Abbott Laboratories Ltd application for Antihemophilic Factor product licence November 1974 p3 MHRA0000091_005. The same warning had appeared in literature provided by Alpha to UK doctors in March 1973, prior to the award of a product licence. Information pages on Antihemophilic Factor (Human) by Abbott Scientific Product Division p4 BPLL0008067, Counsel Presentation on Pharmaceutical Companies Transcript 5 October 2021 pp53-59 INQY1000152
(2306) Counsel Presentation on Pharmaceutical Companies Transcript 5 October 2021 pp63-65 INQY1000152
(2307) ABPI Data Sheet Compendium 1976 for Abbott Laboratories Ltd: Profilate p3 ABPI0000008
(2308) ABPI Data Sheet Compendium 1976 for Abbott Laboratories Ltd: Profilate p3 ABPI0000008, ABPI Data Sheet Compendium 1978 for Abbott Laboratories Ltd: Profilate p3 ABPI0000014
(2309) Alpha Therapeutic UK Ltd application for Profilate Heat Treated product licence 3 January 1985 MHRA0033388_033, Alpha Therapeutic Corporation application for Profilate Heat Treated product licence renewal p6 MHRA0033388_029
(2310) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p10 BAYP0000001_098
(2311) Kasper and Kipnis Letter to the Editor on Hepatitis and Clotting-Factor Concentrates Journal of the American Medical Association 31 July 1972 PRSE0003913
(2312) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p11 BAYP0000001_098
(2313) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p11 BAYP0000001_098
(2314) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p11 BAYP0000001_098
(2315) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p11 BAYP0000001_098
(2316) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p20 BAYP0000001_098
(2317) Product information leaflet for Hemofil by Hyland Laboratories 1979 p1 SHPL0001055_023
(2318) Emphasis added. Information pages on Dried Factor VIII Fraction BP (Koate) by Cutter Laboratories Ltd January 1981 p2 BAYP0000019_012
(2319) Product information leaflet for Koate by Cutter Biological December 1981 p1 BAYP0000019_087. The leaflet was printed in the US and did not specify the UK product licence number, but did include reference to the UK subsidiary that held that licence. The March 1981 leaflet contained details for the US company and licence only. Product information leaflet for Koate by Cutter Biological March 1981 p1 BAYP0000019_025
(2320) Armour Pharmaceutical Company Ltd application for Factorate (Factor VIII) product licence 25 March 1975 p60 ARMO0000002
(2321) Armour Pharmaceutical Company Ltd application for High Potency Factorate product licence 20 November 1978 p12 ARMO0000023
(2322) Armour Pharmaceutical Company Ltd application for Factorate (Factor VIII) product licence 25 March 1975 p66 ARMO0000002
(2323) Counsel Presentation on Pharmaceutical Companies Transcript 29 September 2021 pp109-130 INQY1000149. An application for a product licence renewal for Factorate HP in May 1984 contained a slight variation advising personnel handling the concentrate to “also exercise appropriate caution.” Armour Pharmaceutical Company Ltd application for High Potency Factorate product licence renewal 10 May 1984 p11 ARMO0000145
(2324) Travenol Laboratories Ltd application for Hemofil product licence January 1973 p4 DHSC0105593_006
(2325) Appendix 5 of Travenol Laboratories Ltd application for Hemofil product licence - package leaflet p5 SHPL0000275_013
(2326) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p11 BAYP0000001_098
(2327) Bayer UK Ltd application for Anti-Haemophilic Factor (Human) Koate product licence 16 October 1975 p11 BAYP0000001_098
(2328) Serological Products Ltd application for Kryobulin product licence 11 December 1972 p25, p30 SHPL0000071_181
(2329) Abbott Laboratories Ltd application for Antihemophilic Factor product licence November 1974 p3 MHRA0000091_005, ABPI Data Sheet Compendium 1976 for Abbott Laboratories Ltd: Profilate p3 ABPI0000008
(2330) Armour Pharmaceutical Company Ltd application for Factorate (Factor VIII) product licence 25 March 1975 p60 ARMO0000002, Armour Pharmaceutical Company Ltd application for High Potency Factorate product licence November 1978 p12 ARMO0000023
(2331) Letter from Dr Waiter to Dr Raison 30 December 1975 DHSC0100001_023
(2332) Letter from Dr Dane to Norman Berry 18 July 1975 p1 MHRA0033321_102, Draft Letter from Dr Maycock to Dr Raison 23 January 1976 DHSC0100001_018
(2333) Draft Letter from Dr Maycock to Dr Raison 23 January 1976 p2 DHSC0100001_018
(2334) Except for Alpha, which issued a press release on 7 January 1983 warning of a risk of AIDS from the use of its concentrates. Letter from Ian Marshall to Professor Bloom 16 March 1983 CBLA0000060_067
(2335) Memo from Dave Gury to Plasma Center Directors 16 December 1982 CGRA0000627
(2336) Letter from Ian Marshall to Professor Arthur Bloom 16 March 1983 p2 CBLA0000060_067
(2337) Letter from Ian Marshall to Professor Bloom 16 March 1983 p4 CBLA0000060_067
(2338) Letter from Ian Marshall to Professor Bloom 16 March 1983 p2 CBLA0000060_067. In a letter to Professor Arthur Bloom of 16 March 1983, enclosing this press release, the date of 27 December is given instead. Letter from Ian Marshall to Professor Bloom 16 March 1983 CBLA0000060_067. In a letter to The Lancet of 3 September 1983, David Gury of Alpha said that the corporation had started to screen donors at high risk for AIDS on 21 December 1982. Though the word “screen” is used, this can refer only to some form of assessment of whether a donor belonged to one of the groups identified, and not to any medical test as such. Letters to the Editor Gury AIDS and the Paid Donor The Lancet 3 September 1983 MACK0000237
(2339) Package insert for Antihaemophilic Factor (Human) dried Profilate Heat-Treated 11 March 1985 pp2-3 MHRA0033388_007
(2340) Package insert for Antihaemophilic Factor (Human) dried Profilate Heat-Treated 11 March 1985 p8 MHRA0033388_007
(2341) Counsel Presentation on Pharmaceutical Companies Transcript 5 October 2021 pp97-98 INQY1000152
(2342) Letter from Dr Duncan to G Marshall 18 January 1985 MHRA0033388_018, Counsel Presentation on Pharmaceutical Companies Transcript 5 October 2021 pp101-106 INQY1000152
(2343) This represents a recognition that in reality patients would be unlikely to read the package inserts: if their doctors did not do so, then it would be less likely still that they would.
(2344) Memo from Edward Cutter to Jack Ryan and others 29 December 1982 CGRA0000434
(2345) Though this is on the basis of limited information.
(2346) Letter from Dr Steven Ojala to Dr Elaine Esber 8 November 1983 p3 WITN6984039
(2347) Product information leaflet for Antihemophilic Factor (Human) Koate December 1983 p1 BAYP0000027_080
(2348) Draft Minutes of UK Haemophilia Centre Directors meeting 17 October 1983 p10 PRSE0004440
(2349) Product information leaflet for Antihaemophilic Factor (Human) Dried Factor VIII Fraction Koate March 1984 WITN6407005, Written Statement of Dr Brendon Gray paras 126-127 WITN6984001
(2350) Memo from Dr Kingdon to Sharon Northup 5 January 1983 CGRA0000668
(2351) See Dr Bruce Evatt’s journal article: “In early 1982, the author received a call reporting a hemophilic patient who, treated with FVIII [Factor 8] concentrates, had died of PCP [pneumocystis carinii pneumonia]. The physician reasoned that the clotting factor was contaminated with P. carinii and was transmitted directly to the patient. However, the manufacturing process would have removed contaminating P. carinii, and the rarity of PCP in hemophilia suggested the possibility that the patient had acquired the same syndrome that was affecting homosexuals. After investigating, the author determined that the patient’s clinical record was consistent with the new disorder, but the patient’s death precluded confirmatory tests. Almost simultaneously, the CDC received reports of a similar immune disorder in Haitian patients and i.v. drug abusers. As anal intercourse or use of amyl nitrites, prevailing theories regarding the cause of the homosexual disease, were not common practices for hemophilic patients, Haitians or i.v. drug abusers, the author reasoned that these four groups had very little in common except for one thing, a risk for blood-borne diseases.” Evatt The tragic history of AIDS in the hemophilia population 1982-1984 Journal of Thrombosis and Haemostasis 2006p4CVHB0000042. The Krever Report notes that by March 1982, 257 cases of PCP or Kaposi’s sarcoma (including 25 of both) had been linked to immunosuppression (demonstrated by a reversal of the usual T-helper/suppressor ratio) and identified to the CDC task force. The Krever Report 1997 p193 KREV0000001. See also footnote 2368.
(2352) Travenol Laboratories Ltd Hemofil product licence variation May 1983 p5 DHSC0105556_028, Travenol Laboratories Ltd Hemofil product licence variation 14 September 1983 DHSC0003951_006, Travenol Laboratories Ltd application for Antihaemophilic Factor (Human) Method Four-Heat Treated Hemofil-T product licence 30 November 1984 p17 SHPL0000283_005
(2353) Christopher Bishop Transcript 4 November 2021 pp35-39 INQY1000158
(2354) Counsel Presentation on Pharmaceutical Companies Transcript 24 September 2021 pp20-26 INQY1000147. The absence of an AIDS warning is seemingly confirmed by a letter from the then managing director of Immuno Ltd, Peter Coombes, to David Watters of the Haemophilia Society dated 10 February 1987. Letter from Peter Coombes to David Watters 10 February 1987 HSOC0023097
(2355) Counsel Presentation on Pharmaceutical Companies Transcript 29 September 2021 pp112-130 INQY1000149
(2356) The Krever Report 1997 p408 KREV0000001
(2357) Counsel Presentation on Pharmaceutical Companies Transcript 29 September 2021 pp130-131 INQY1000149
(2358) Letter from Ian Marshall to Professor Bloom 16 March 1983 p2 CBLA0000060_067
(2359) Product withdrawal is discussed in more detail below.
(2360) Letter from Ken Fitch to Haemophilia Centre Directors 19 May 1983 p1 BART0000863
(2361) Letter from Ken Fitch to Haemophilia Centre Directors 19 May 1983 p2 BART0000863
(2362) Letter from Ken Fitch to Haemophilia Centre Directors 19 May 1983 pp4-5 BART0000863
(2363) Letter from Travenol Laboratories Ltd to DHSS 9 May 1983 p1 PRSE0004496. The Committee on Safety of Medicines Biological Subcommittee subsequently “strongly deprecated” what they saw as “unjustified claims on improved safety margins in respect of infection and AIDS” in letters sent by Hyland/Travenol. That criticism may well relate to comments made in this letter about the hopes for heat-treated Hemofil: “Hyland Therapeutics believes that administration of the heat treated product, designed to reduce viral content, may increase patient and centre personnel safety.” Travenol Laboratories Ltd Hemofil product licence variation 14 September 1983 DHSC0003951_006, Letter from Travenol Laboratories Ltd to DHSS 9 May 1983 p2 PRSE0004496, Counsel Presentation on Pharmaceutical Companies Transcript 24 September 2021 pp143-147 INQY1000147
(2364) See the chapter on Haemophilia Centres: Policies and Practice.
(2365) Letter from Ian Marshall to Professor Bloom 16 March 1983 p3 CBLA0000060_067
(2366) Letter from Ken Fitch to Haemophilia Centre Directors 19 May 1983 p4 BART0000863,
Letter from Travenol Laboratories Ltd to DHSS 9 May 1983 p1 PRSE0004496. The letter from Ken Fitch did say that Armour had taken steps to reduce the contribution to its fractionation pools from high risk donors.
(2367) Letter from Reverend Tanner to members of the Haemophilia Society 4 May 1983 DHSC0001228, Minutes of special meeting of Haemophilia Reference Centre Directors 13 May 1983 pp1-3 HCDO0000003_008
(2368) Durack Opportunistic infections and Kaposi’s sarcoma in homosexual men The New England Journal of Medicine 10 December 1981 PRSE0000746, Gottlieb et al Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men The New England Journal of Medicine 10 December 1981 CGRA0000243, Masur et al An outbreak of community-acquired pneumocystis carinii pneumonia The New England Journal of Medicine 10 December 1981 PRSE0004831, Siegal et al Severe Aquired Immunodeficiency in Male Homosexuals, Manifested by Chronic Perianal Ulcerative Herpes Simplex Lesions The New England Journal of Medicine 10 December 1981 RLIT0002412
(2369) Memo from Dr Kingdon to Sharon Northup 5 January 1983 CGRA0000668
(2370) CDC Epidemiologic Notes and Reports Update on Kaposi’s Sarcoma and Opportunistic Infections in Previously Healthy Persons – US Morbidity and Mortality Weekly Report 11 June 1982 p1 PRSE0000431
(2371) Florida (a New York resident), Colorado and Ohio – all diagnosed some distance from the epicentre of the outbreaks in New York, San Francisco and Los Angeles. CDC Epidemiologic Notes and Reports Pneumocystis carinii Pneumonia among Persons with Hemophilia A Morbidity and Mortality Weekly Report 16 July 1982 PRSE0000523
(2372) Letter from Dr Meyer to Manufacturers of Plasma Fractionation Products 9 July 1982 CGRA0000288
(2373) CDC Epidemiologic Notes and Reports Pneumocystis carinii Pneumonia among Persons with Hemophilia A Morbidity and Mortality Weekly Report 16 July 1982 PRSE0000523
(2374) National Hemophilia Foundation Hemophilia Newsnotes: Hemophilia Patient Alert #1 14 July 1982 MULL0006612_002
(2375) See the chapter on Blood Services and Addressing Risk: Response.
(2376) The committee was established by the Public Health Service (“PHS”). The account here is an overview, given by Justice Krever, which I accept: The Krever Report 1997 pp197-198 KREV0000001. It fits with the CDC’s own report of the meeting, which says that the meeting concluded that “AIDS has characteristics which suggest an infectious etiology.” This is taken from Summary Report on Open Meeting of PHS Committee on Opportunistic Infections in Patients with Hemophilia provided by CDC director Dr William Foege in Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 p277, p282 JREE0000019. There were two differing views also given by participants at the meeting. According to a retrospective article, The tragic history of AIDS in the hemophilia population, 1982-1984, written 20 years later by Dr Evatt of the CDC, he and his colleagues had come to the conclusion that “Only the high risk for blood-borne infections could explain a risk common to all four groups”, namely drug users, Haitians, gay men and people with haemophilia. However, those attending did not appear to accept this proposition and, in his words, “the audience expressed an almost universal reluctance to act.” Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p4CVHB0000042. Dr Rodell’s account of the meeting records that a representative of the American Red Cross commented that “CDC has not yet proven that AIDS is transmissible by blood or blood products, and that no donor population should be implicated at this time.” Letter from Dr Rodell to Dr Kaufman 3 August 1982 p3 CGRA0000287
(2377) Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p5CVHB0000042
(2378) Memo from Dr Ojala to Dr Schaeffler and others 17 January 1983 p2 CGRA0000321
(2379) Counsel Presentation on Pharmaceutical Companies: Response to Risk pp9-37 INQY0000311
(2380) CDC Update on Acquired Immune Deficiency Syndrome (AIDS) among Patients with Hemophilia A, Possible Transfusion-Associated Acquired Immune Deficiency Syndrome (AIDS) – California Morbidity and Mortality Weekly Report 10 December 1982 PRSE0003276
(2381) Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p5CVHB0000042
(2382) Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p6CVHB0000042
(2383) Memo from Dr Hink to Dr Fischer and others 6 January 1983 p1 CGRA0000300, Counsel Presentation on Pharmaceutical Companies: Response to Risk pp25-29 INQY0000311
(2384) The Cook Report: Profits Before Patients 23 July 1990 08:07-09:14 ITVN0000052, Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p6CVHB0000042
(2385) Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p6CVHB0000042
(2386) Memo from the American Red Cross National Headquarters 5 February 1983 in Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 p277, p301 JREE0000019. Emphasis in original. The Institute of Medicine Report recorded that the Red Cross official recalled that when Dr Francis suggested at the meeting that Hepatitis B core testing should be introduced, as a surrogate test for the presence of the putative virus, he was not supported by any of his superiors. Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 pp130-131 JREE0000019
(2387) The Krever Report 1997 pp202-203 KREV0000001, Summary Report on Workgroup to Identify Opportunities for Prevention of Acquired Immune Deficiency Syndrome 4 January 1983 MULL0001034_004
(2388) CDC Current Trends Prevention of Acquired Immune Deficiency Syndrome (AIDS): Report of Inter-Agency Recommendations Morbidity and Mortality Weekly Report 4 March 1983 PRSE0001115, Joint Statement on Acquired Immune Deficiency Syndrome Related to Transfusion 13 January 1983 MULL0003601
(2389) Letter from Dr Petricciani to all Licensed Manufacturers of Plasma Derivatives 24 March 1983 DHSC0001203
(2390) Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p5CVHB0000042
(2391) The request came from Dr Donohoe of the FDA. Memo from Dr Ojala to Dr Schaeffler and others 13 December 1982 CGRA0000425, Counsel Presentation on Pharmaceutical Companies: Response to Risk pp18-19 INQY0000311
(2392) Counsel Presentation on Pharmaceutical Companies: Response to Risk pp20-22 INQY0000311
(2393) Letter from Ian Marshall to Professor Bloom 16 March 1983 p2 CBLA0000060_067
(2394) Alpha Hemophilia Letter Winter 1982 p1 HCDO0000276_025
(2395) Memo from Dr Ojala to Dr Schaeffler and others 17 January 1983 p1 CGRA0000321
(2396) Alpha Hemophilia Letter Summer 1983 p1 CGRA0000665_001
(2397) Memo from William Srigley to David Castaldi and others 14 June 1983 p2 CGRA0000267
(2398) As is discussed below, Alpha appears to have been aware from 15 December 1982 that it had obtained and processed plasma from a donor from the Irwin Memorial Blood Bank who was later identified as having contracted AIDS.
(2399) Letter from Thomas Drees to Charles Carman and Dr Aledort 9 November 1982 CGRA0000262, Memo from Edward Mealey to the Executive Committee 15 December 1982 CGRA0000599
(2400) Alpha Hemophilia Letter Winter 1982 p1 HCDO0000276_025
(2401) Letter from the American Blood Resources Association to members 28 January 1983 p2 BAYP0004385
(2402) Counsel Presentation on Pharmaceutical Companies: Response to Risk pp34-36 INQY0000311. The Blood Policy Advisory Committee was a standing committee that provided advice to the FDA. It comprised various individuals drawn from relevant medical, commercial and charitable establishments. The blood banking industry was particularly strongly represented. Counsel Presentation on Pharmaceutical Companies: Response to Risk p5 INQY0000311
(2403) Counsel Presentation on Pharmaceutical Companies: Response to Risk p39 INQY0000311
(2404) Memo from William Srigley to David Castaldi 20 October 1983 p2 CGRA0000291
(2405) See the chapter on Regulation of Commercial Factor Concentrates.
(2406) These included antibodies to Hepatitis B core antigen (anti-HBc), T-cell ratio measurement, cytomegalovirus, Epstein-Barr virus, beta-2 microglobulin, immune complexes, neopterin, thymosinal and alpha interferon: Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decision making 1995 pp131-135 JREE0000019
(2407) See for example the comments of Dr Evatt at the BPAC meeting: Minutes of Blood Products Advisory Committee meeting 3-4 December 1982 p9 CGRA0000674
(2408) Minutes of Blood Products Advisory Committee meeting 3-4 December 1982 p10 CGRA0000674
(2409) Summary Report on Workgroup to Identify Opportunities for Prevention of Acquired Immune Deficiency Syndrome 4 January 1983 p4 CGRA0000301, Evatt The tragic history of AIDS in the hemophilia population, 1982-1984 Journal of Thrombosis and Haemostasis 2006p6CVHB0000042
(2410) The Institute of Medicine Committee’s report was later critical of the CDC’s approach. It commented: “A careful reading of the evidence shows why people could not agree about the frequency of anti-HBc in people who could transmit AIDS. The CDC claimed that 90 percent of AIDS patients had anti-HBc. This statement appeared in public statements and letters, but the Committee was unable to find any 1982-1984 account that described the clinical characteristics and size of their AIDS study population, the methods for measuring anti-HBc, or a table of results. In other words, the standard basis for evaluating a scientific claim, a published report, was missing. Because those that claimed a much lower impact on anti-HBc published their work, it is possible to evaluate its relevance to preventing the transmission of AIDS by excluding donors who had anti-HBc.” Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 p127 JREE0000019
(2411) Memo from Dr Hink to Dr Fischer and others 6 January 1983 p2 CGRA0000300
(2412) Memo from Dr Ojala to Dr Schaeffler and others 17 January 1983 p1 CGRA0000321. The American Blood Resources Association (“ABRA”) was a trade body for pharmaceutical companies and plasma collection companies.
(2413) The Inquiry has a number of memoranda written by Dr Ojala of Cutter that contain his accounts of what occurred at such meetings, including that held on 14 January 1983. See Memo from Dr Ojala to Wilhelm Schaeffler and others 13 June 1983 CGRA0000231, Memo from Dr Ojala to M Sternberg 29 November 1983 MULL0000841_042 and Memo from Dr Ojala to Wilhelm Schaeffler 19 December 1983 UCSF0000034
(2414) Memo from Dr Ojala to Dr Schaeffler and others 17 January 1983 p1 CGRA0000321
(2415) National Hemophilia Foundation Medical and Scientific Advisory Council Hemophilia Newsnotes: Medical Bulletin #5 14 January 1983 p3 ARMO0000250_002
(2416) Memo from Dr Ojala to Dr Schaeffler and others 17 January 1983 p3 CGRA0000321
(2417) Memo from Dr Ojala to Dr Schaeffler and others 17 January 1983 p3 CGRA0000321
(2418) Memo from Dr Ojala to Dr Schaeffler and others 19 December 1983 UCSF0000034
(2419) Interim Summary Statement of Hepatitis B Core Antibody Testing Study Group MHRA0000076_010. The minutes also record that “members of the majority group indicated that they would likely be compelled to follow suit if any of the organizations represented initiated Anti-HBc testing programs.”
(2420) Interim Summary Statement of Hepatitis B Core Antibody Testing Study Group MHRA0000076_010
(2421) Memo from Dr Hink to Biological Management Committee Members and others 13 March 1984 p1 CGRA0000319
(2422) It is unclear if this refers just to the cost to Armour, by whom Dr Rodell was now employed, or to all the members of the Plasma Manufacturers’ Association. Memo from Dr Hink to Biological Management Committee Members and others 13 March 1984 p3 CGRA0000319. See also Counsel Presentation on Pharmaceutical Companies: Response to Risk November 2021 paras 191-195 INQY0000311
(2423) See the chapter on HIV screening.
(2424) Cutter News Release 2 April 1984 CGRA0000240, Written Statement of Dr Brendon Gray para 102, para 139 WITN6984001. Announcing its cessation, the company stated that this was a consequence of “the success of our heating process against viral contaminants.” It also noted that the company was participating in the development of a specific test for HTLV-3. See Cutter The Biological Bulletin: Marketing Bulletin 17-84 12 November 1984 p3 BAYP0005475_001
(2425) Memo from Dr Ojala to Wilhelm Schaeffler and others p2 UCSF0000034
(2426) In summary, the advantages were:
(a) The reduction of risk of future product withdrawals.
(b) “Cutter has an obligation to use all reasonable means to provide safe effective products.” This point was made with reference to non-A non-B Hepatitis as well as other viruses.
(c) Testing should result in higher customer acceptance and sales. It was noted that Cutter needed a way to differentiate itself from its rivals.
(d) Separation of anti-HBc plasma would allow for more efficient identification of plasma with other hepatitis markers.
(e) Start-up costs were already sunk and testing costs were not significant – the exclusion of plasma was the “real expense”.
(f) The testing might allow for stronger claims to be made about non-A non-B Hepatitis reduction.
The disadvantages were:
(a) Cost: the costs already incurred amounted to some $100,000, and continuation would add $0.3 to each litre of plasma procured.
(b) 15% of plasma tested had proved to be anti-HBc positive. Exclusion of that plasma and any resulting concentrates would have “significant but indeterminate costs.”
(c) The test was not AIDS-specific, and hence the risk of needing to withdraw product because of AIDS remained.
(d) More specific AIDS tests would be available in the (relatively near) future.
(e) Heat treatment might inactivate the AIDS agent, meaning that testing and heat treatment would be considered “a ‘belt and suspenders’ redundancy.’”
(f) Removing anti-HBc plasma should also reduce the prevalence of Hepatitis B surface antibody, which could have the unintended consequence of rendering a plasma pool at greater risk of transmitting Hepatitis B virus (because of the low prevalence of antibodies).
(g) Flexibility of plasma production was considerably reduced, and many suppliers were unable or unwilling to comply with the necessary procedures.
(h) The identification, separation and isolation of anti-HBc plasma had placed “a large burden on Cutter employees and staff.”
Memo from Dr Hink to Biological Management Committee Members 25 May 1984 pp2-4 CGRA0000362
(2427) Memo from Dr Hink to Biological Management Committee Members and others 13 March 1984 p1 CGRA0000319. Emphasis in original. Counsel Presentation on Pharmaceutical Companies: Response to Risk pp59-61 INQY0000311
(2428) The issue of the withdrawal of Factorate HT, Armour’s heat-treated product, from the UK market, is considered in the chapter on Viral Inactivation.
(2429) Memo from Edward Mealey to the Executive Committee 15 December 1982 p2 CGRA0000599
(2430) Memo from Dave Gury to AIDS Task Force and others 22 February 1983 p2 CGRA0000278. Marietta Carr was Vice President for Regulatory Affairs at Alpha.
(2431) Letter from Travenol Laboratories Ltd to DHSS 9 May 1983 PRSE0004496. See also The Krever Report 1997 p778 KREV0000001 and Institute of Medicine Committee to Study HIV Transmission Through Blood and Blood Products HIV and the Blood Supply: An analysis of crisis decisionmaking 1995 pp88-89 JREE0000019
(2432) Letter from Dr John Ashworth to Dr Keith Fowler 3 June 1983 p2 BAYP0000002_183
(2433) Memo from Dr Ojala to Dr Schaeffler and others 13 June 1983 p1 CGRA0000231
(2434) Memo from David Castaldi to William Srigley 14 June 1983 p1 CGRA0000267
(2435) Memo from Dr Ojala to Dr Schaeffler and others 13 June 1983 p1 CGRA0000231
(2436) Memo from Marietta Carr to L Coffey and others 13 June 1983 p2 CGRA0000598
(2437) Memo from William Srigley to David Castaldi 14 June 1983 p2 CGRA0000267. For a summary of the views expressed, see Counsel Presentation on Pharmaceutical Companies: Response to Risk pp45-47 INQY0000311
(2438) Memo from Dr Ojala to Dr Schaeffler and others 13 June 1983 p2 CGRA0000231
(2439) Memo from Marietta Carr to L Coffey and others 13 June 1983 p2 CGRA0000598
(2440) Memo from Dr Ojala to Dr Schaeffler and others 13 June 1983 p2 CGRA0000231
(2441) Minutes of Blood Products Advisory Committee meeting 19 July 1983 pp2-3 BAYP0004674
(2442) Minutes of Blood Products Advisory Committee meeting 19 July 1983 p3 BAYP0004674
(2443) Minutes of Blood Products Advisory Committee meeting 19 July 1983 p3 BAYP0004674
(2444) Trip Report of Meeting of Blood Products Advisory Committee on the Safety and Purity of Plasma Derivatives 19 July 1983 p8 CBLA0000056_215. It was Dr Derrick whose note refers to the effect of Dr Rodell’s presentation being that four donors might, in theory at least, jeopardise the world supply of Factor 8. See the further discussion of this point in the chapter on Regulation of Commercial Factor Concentrates.
(2445) National Hemophilia Foundation Hemophilia Newsnotes: Medical Bulletin #7 11 May 1983 p2 MULL0006352
(2446) Minutes of Blood Products Advisory Committee meeting 19 July 1983 pp3-4 BAYP0004674. Emphasis added.
(2447) National Hemophilia Foundation Hemophilia Newsnotes: Medical Bulletin #9 22 October 1983 p2 DHSC0001272. Interestingly this National Hemophilia Foundation bulletin recommends that regional and community blood centres in regions with a very low incidence of AIDS should increase their capacity for cryoprecipitate production to be used locally and in other regions and that those centres should evaluate the feasibility of preparing small pool lyophilised cryoprecipitate.
(2448) Draft Minutes of NIBSC Infectious Hazards of Blood Products meeting 9 February 1984 pp9-10 PRSE0003071. Dr Petricciani agreed the minutes. Letter from Dr Petricciani to Dr Thomas MHRA0000076_007. See also Counsel Presentation on Pharmaceutical Companies: Response to Risk pp56-59 INQY0000311
(2449) Memo from Marietta Carr to members of Alpha Operations Committee 21 February 1984 p6 CGRA0000610
(2450) Dr Kingdon dates the inspection regime he described to 1975. Draft Written Statement of Dr Henry Kingdon for HIV Litigation 30 October 1990 p12 CBLA0000011_005
(2451) World in Action Blood Money Transcript 1 and 8 December 1975 pp4-7 PRSE0004591
(2452) ie imported into the US.
(2453) That is relatively cheap compared with other available sources for all plasma had a significant market value, such that Douglas Starr called it “among the world’s most precious liquids.” Starr Blood: An Epic History of Medicine and Commerce 1998 p11 HSOC0019915
(2454) See the chapter on Hepatitis Risks 1970 and After.
(2455) Trip Report of Meeting of Blood Products Advisory Committee on the Safety and Purity of Plasma Derivatives 19 July 1983 p8 CBLA0000056_215
(2456) Wellcome Witnesses to Twentieth Century Medicine – Haemophilia: Recent History of Clinical Management seminar Transcript 10 February 1998 pp65-66 RLIT0000022
(2457) Long-time chair of the Society, from 1975 for 22 years.
(2458) Being “manned entirely by volunteers” was described by him as “a very, very important aspect of the whole organization”. Wellcome Witnesses to Twentieth Century Medicine – Haemophilia: Recent History of Clinical Management seminar Transcript 10 February 1998 p66 RLIT0000022
(2459) The Inquiry had little evidence which bore out the claim that the Society had been aggressive in dealing with doctors. Though this plainly was the view Reverend Alan Tanner had in retrospect, for most of the period from 1970 to 1986 the Society actually tended to defer to the clinicians who were most involved with advising it.
(2460) This description is the way the Society described itself in Haemophilia Society Annual Report 1986 31 December 1986 p5 HCDO0000276_033
(2461) Notably The Bulletin, and (starting in 1983 when the AIDS crisis had loomed) a series of supposed fact sheets, Haemofacts.
(2462) Wellcome Witnesses to Twentieth Century Medicine – Haemophilia: Recent History of Clinical Management held on 10 February 1998 pp66-67 RLIT0000022. Because of the reference to television, it is likely that this was in or just after December 1975 when Granada World in Action screened a documentary about plasma collection from down-and-outs in the US, and the resultant increased risk of hepatitis carried by products made from such plasma – World in Action Blood Money Part 1 1 December 1975 MDIA0000113, World in Action Blood Money Part 2 8 December 1975 MDIA0000114, transcript of both episodes World in Action Blood Money Transcript 1 and 8 December 1975 PRSE0004591. It seems likely that the date was 11 December, since a departmental note of a meeting between Dr David Owen, Reverend Tanner and others on this date mentioned that the Society was keen to encourage greater use of plasmapheresis in order to help achieve self-sufficiency (although the note is silent about the Society also saying it was not prepared to accept the risk of hepatitis coming from the US). Note of meeting between Minister of State for Health and Haemophilia Society 11 December 1975 DHSC0100006_093. The Society thus could be said to have campaigned for the greater use of plasmapheresis, as argued in its final submissions to this Inquiry. Closing Submissions of Haemophilia Society 16 December 2022 pp32-33, Closing Submissions of Haemophilia Society 16 December 2022 p103 SUBS0000065
(2463) In succession to Jim Hunter.
(2464) It never fluctuated, although there was something of a wobble in the mid 1980s about the Society’s position, when Ken Milne, a trustee thought by his peers to be particularly knowledgeable about the science, began to question the policy he had previously advocated. See for instance, Letter from Ken Milne to Dr Brian Colvin 29 February 1984 BART0002309
(2465) See the chapter Macfarlane Trust.
(2466) Written Statement of David Watters para 5 WITN3429001, David Watters Transcript 9 February 2021 p3 INQY1000094
(2467) David Watters Transcript 9 February 2021 p28 INQY1000094
(2468) Peter Wetherell (a member of the Executive Committee 1983-85) for instance, said it made decisions which it feltwould be in accordance with the wishes of the membership at any one time. Peter Wetherell Transcript 25 May 2021 pp15-17 INQY1000122
(2469) During David Watters’ term of office. David Watters explained that: “There were also regional meetings where the Executive Committee would not just meet with representatives from the local groups but would also meet with the membership of the local groups and anyone else who was interested in the work of The Society”. Written Statement of David Watters para 12 WITN3429001
(2470) David Watters described there as having been a problem with trust from the members’ perspective when he began work. David Watters Transcript 9 February 2021 p29 INQY1000094
(2471) Written Statement of David Watters para 13 WITN3429001. Although haemophilia tends to run in families, it might be that one family member belonged to the Society and the others benefited through him (or, less likely, her). David Watters Transcript 9 February 2021 pp25-26 INQY1000094
(2472) David Watters Transcript 9 February 2021 p28 INQY1000094
(2473) David Watters Transcript 9 February 2021 p23 INQY1000094
(2474) David Watters also indicated that other sources of information included pharmaceutical companies, journalists and regular meetings with DHSS civil servants. David Watters Transcript 9 February 2021 pp31-32, pp64-65 INQY1000094, David Watters Transcript 12 February 2021 p56 INQY1000097
(2475) David Watters Transcript 9 February 2021 p28 INQY1000094
(2476) Haemophilia Society The Bulletin No3 1980 p1 HSOC0022893
(2477) The advice was not often given to the Executive Committee in writing, but usually by verbal report from the member who had spoken to the clinician. Simon Taylor Transcript 25 May 2021 pp15-16 INQY1000277. This had the added disadvantage that it was bound to be overlaid with the subjective recollection and emphasis of the person reporting it.
(2478) At least in the early 1980s if not later.
(2479) David Watters Transcript 9 February 2021 p41 INQY1000094
(2480) David Watters Transcript 9 February 2021 pp42-43 INQY1000094
(2481) David Watters Transcript 9 February 2021 p48 INQY1000094. Also the evidence of Simon Taylor: Simon Taylor Transcript 25 May 2021 pp22-29 INQY1000277
(2482) Written Statement of David Watters para 112 WITN3429001. David Watters referenced Dr Mark Winter as an example of one of the younger haematologists he might have had in mind. David Watters Transcript 9 February 2021 p53 INQY1000094
(2483) Peter Wetherell Transcript 25 May 2021 pp54-55 INQY1000122. He had previously been chair of the Cambridge branch of the Society, so had experience of both its local and central workings.
(2484) Closing Submissions of Haemophilia Society 16 December 2022 p41 SUBS0000065
(2485) Letter from David Watters to Professor Bloom 19 January 1983 BPLL0001351_071
(2486) Letter from Professor Bloom to David Watters 20 January 1983 HCDO0000003_066
(2487) This represents the approach of looking to know theprecise cause why A should lead to B before responding to an apparent risk that A may lead to B.
(2488) Which Professor Bloom had in the 1970s regarded as an unavoidable consequence of haemophilia treatment: on 10 February 1975 he wrote to a local GP, concerning a patient, to say that “a small percentage of these freeze-dried preparations contain, unavoidably, the virus of serum hepatitis and therefore potentially dangerous to the patient, his relatives etc.” (emphasis added). Letter from Professor Bloom to Anon 10 February 1975 WITN0047002
(2489) In March 1983 Professor Bloom was told by Dr Bruce Evatt from the US Centers for Disease Control (“CDC”) that AIDS generally was evolving “with a frightening pace” – 80 new cases were reported in December 1982, 120 in January 1983, February approaching 20% higher still – and about 40% of all cases having been reported between November 1982 and February 1983. Letter from Dr Evatt to Professor Bloom 7 March 1983 DHSC0001175. In the absence of any good reason to distinguish the syndrome in patients with haemophilia from the general population, there was nothing to suggest that infections amongst them would not follow a similar course. No good reason was known.
(2490) David Watters Transcript 9 February 2021 pp92-94 INQY1000094. In a surprising exchange he described being shown a “very heavily redacted letter that came from a branch of the Department of Health … in which Professor Bloom was told in no uncertain terms that … he at all costs should make sure that the advice was always given to patients that they should continue to take their blood products as … the benefits far outweighed the risks because this was going to be a small problem”. There is no suggestion from elsewhere of such a letter; the Inquiry has attempted to locate it but has been unable to do so.
(2491) Editor of The Bulletin and member of the Society’s Executive Committee.
(2492) David Watters Transcript 9 February 2021 p92 INQY1000094. There would be similar wishful thinking in a paper drafted by Ken Milne: Minutes of Haemophilia Society Blood Products Sub-Committee meeting 9 January 1984 PRSE0002290. The paper contains much that is surprising and was heterodox even at the time. (It asserted, for instance, that the NBTS screening of high-risk donors compared unfavourably with that adopted by commercial companies in the US; that the moral arguments in favour of self-sufficiency adopted by WHO were designed to protect states south of the equator, and had no real relevance to imports from the US. It reads like a document which in what it said was heavily influenced by a manufacturer of commercial concentrate). The Executive Committee seems to have broadly endorsed the paper and circulated it to members of the Medical Advisory Panel. Drs Charles Rizza and Brian Colvin questioned aspects of it and Professor Bloom commented: “personally I am not quite so complacent about importing American blood products as he and presumably the Subcommittee feel. We must bear in mind that we may not have had the AIDS problem in the UK had we been self-sufficient in blood products.” Letter from Professor Bloom to David Watters 28 February 1984 p2 BPLL0001351_094
(2493) Haemophilia Society The Bulletin No1 1983 p12 PRSE0004120. Compare with footnote 2488. The Inquiry has noted that in December 1982 Dr Peter Kernoff had begun testing his own haemophilia patients at the Royal Free Hospital to see if their T-cell ratios showed a relationship with their receipt of imported commercial concentrates. Lindsay Tribunal Transcript of Professor Christine Lee 25 July 2001 p6 LIND0000326. A lower than normal ratio of T4 (helper) cells to T8 (killer) cells was by then thought by many in the US to indicate an early stage in a progressive deterioration of the immune system which might manifest itself as AIDS. His doing so thus indicates that he thought there was some risk that commercial concentrates might transmit a cause of AIDS, and that the risk was sufficiently high to justify the time and care involved in running a study to help determine if this was so. When the findings were reported to The Lancet in July 1983 it showed that indeed a much larger number of those who had received commercial concentrates had low T4/T8 ratios. By comparison all but one of those in the low exposure group, and all the patients who had received NHS Factor 9 products, had normal ratios; and it was recognised that those treated with cryoprecipitate generally were likewise unaffected. Lee et al Plasma Fractionation Methods and T-cell Subsets in Haemophilia The Lancet 16 July 1983 CBLA0000059_033. None of this was reflected in the advice he gave the Society: if indeed a low T4/T8 ratio was indicative of the start of a slide into AIDS it might actually justify the description “epidemic” which Dr Kernoff was holding up for ridicule. Dr Kernoff answered the question: “Are there any blood tests that can predict if you’re going to get AIDS?” by saying: “A: No. Typically, patients with AIDS have abnormalities of the distribution and function of their blood lymphocytes. The simplest test, which is also the least meaningful, is to measure the ratio of T4 to T8 lymphocytes (the T4/T8 ratio). Patients with AIDS have low ratios. However, low ratios are not unique to AIDS – similar results may be found in a variety of other circumstances. So the finding of a low ratio doesn’t diagnose AIDS, and there’s no evidence that it predicts it, either. Q: I’ve heard that American haemophiliacs who’ve been treated with commercial factor VIII concentrates have, on average, low T4/T8 ratios. Doesn’t that mean something? A: Nobody knows what it means. But it’s an interesting observation, because haemophiliacs who’d been treated with cryoprecipitate usually had normal ratios. But it’s only an observation about a test. In these studies, none of the patients with low ratios had AIDS.” Haemophilia Society The Bulletin No1 1983 p12 PRSE0004120. By contrast, when he wrote for Haemofact No4 in September 1984 he began by saying “The possibility that the acquired immunodeficiency syndrome (AIDS) might be caused by an unusual virus has always been a strong one.” Haemophilia Society Haemofact No4 24 September 1984 p2 PRSE0002824. This publication followed a contribution in May from his junior colleague, Dr Christine Lee, which began by stating that the occurrence of AIDS in patients with haemophilia strongly suggested transmission by blood products. Haemophilia Society Haemofact No3 11 May 1984 p2 DHSC0001264. The strength of these later opinions suggest that Dr Kernoff was understating the position when he advised the Society in 1983.
(2494) The Haemophilia Society do not think it had, but the recollection mentioned in the evidence of David Watters about the difficulties he and Clive Knight had in persuading others that there was a risk may well refer to the meeting held at the Kennedy Hotel in the autumn of 1982; by the time of the 1983 meeting there, the Society had on the evidence begun to realise there was a real and serious risk, and some thought Professor Bloom was downplaying the risk. David Watters Transcript 9 February 2021 p92, pp95-96 INQY1000094, Closing Submissions of Haemophilia Society 16 December 202 pp23-24 SUBS0000065
(2495) Haemophilia Society The Bulletin No 2 December 1983 pp2-3 PRSE0000411. In the course of his talk Professor Bloom stated that he was “unaware of any definite cases in British haemophiliacs”. His choice of the adjective “definite” must have been deliberate: a patient under Professor Bloom’s care was admitted to University Hospital Wales on 14 March 1983 with symptoms consistent with AIDS. The UKHCDO AIDS form subsequently completed by Professor Bloom on 26 April 1983 indicated that the patient was first suspected to be suffering from AIDS on 17 March 1983. UK Haemophilia Centre Directors Hepatitis Working Party Form 26 April 1983 WITN3408009
(2496) It is difficult to know what this was intended to convey. Where AIDS was identified in a patient, it was more likely than not to result in death in the near future. If he meant to say that changes in a patient’s blood identified in a laboratory did not indicate that the patient had AIDS, the comment is understandable – but to suggest that “the disease” (ie AIDS rather than infection with a virus) might not be serious flew in the face of the information available at the time. The comment is perhaps best understood as an attempt to downplay AIDS by words which, though possibly meaningless on analysis, sounded reassuring, so that people would continue their treatment as before. He might have known of Dr Kernoff’s study as described in footnote 2492.
(2497) Haemophilia Society The Bulletin No2 December 1983 p5 PRSE0000411
(2498) The Mail on Sunday Hospitals using killer blood 1 May 1983 PRSE0000199
(2499) Letter from Professor Bloom to Reverend Tanner 3 May 1983 CBLA0000060_158
(2500) Letter from Reverend Tanner to members of the Haemophilia Society 4 May 1983 DHSC0001228
(2501) Though it is doubtful that any member of the Executive Committee thought about this wording at the time, this is a policy of looking for “proof” not of risk, but of effect. It is a theme common to the way in which haemophilia clinicians and government pronouncements at the time expressed their view of the issues. What should have been of concern is whether there was evidence that there was a real risk that current treatment programmes were exposing patients to the development of AIDS.
(2502) Minutes of Haemophilia Society Executive Committee meeting 12 April 1983 pp2-3 HSOC0029476_024. The Executive Committee also noted that at the Society’s next meeting with a minister the agenda item would include “That there will be no attempt to suspend the importation of US commercial products without definite evidence that this would be necessary.”
(2503) Written Statement of Peter Wetherell para 26 WITN3912001, Peter Wetherell Transcript 25 May 2021 p21 INQY1000122
(2504) Applying the balance of probability standard, this therefore means it was identified as a case of AIDS: a point made elsewhere in this Report. See the chapters on Knowledge of the Risks of AIDS and Haemophilia Centres: Policies and Practice.
(2505) Such as Dr Evatt of the CDC, to whom Professor Bloom had gone to seek information, and from whom came the chilling response on 7 March 1983 that in the US the “AIDS epidemic” was evolving with a frightening pace; that 13 cases of AIDS had already been identified in people with haemophilia with 5 highly suspect cases under investigation; and that 12 patients without haemophilia had developed AIDS after transfusion. Letter from Dr Evatt to Professor Bloom 7 March 1983 DHSC0001175
(2506) Closing Submissions of Haemophilia Society 16 December 2022 p16 SUBS0000065. A further example is shown by the minutes of the Executive Committee of 14 June 1983, which show that it was reported that the “confirmed” Cardiff case (of AIDS) was now back at work and in reasonably good health. This information almost certainly came from Professor Bloom (there is no other source from whom it could realistically have come, and the case was his own patient) and it was untrue. Minutes of Haemophilia Society Executive Committee meeting 14 June 1983 p2 HSOC0029476_025. In its final submissions the Society records that “There are instances, most of them authored by Professor Bloom, of the Society being misinformed”. Closing Submissions of Haemophilia Society 16 December 2022 p18 SUBS0000065. I have no reason to think that this is an exaggeration.
(2507) Evidence of David Watters. David Watters Transcript 10 February 2021 p37 INQY1000095
(2508) The words “at the time” are important. Prior to this there had been the question and answer article quoting Dr Kernoff, but he does not appear to have been asked for advice after The Mail on Sunday article. As to later, an article from Dr Tony Pinching was published in The Bulletin for 1983 – but this came some time after the events being described in the text, probably in late summer or early autumn. It is interesting in that Dr Pinching, an immunologist, said (a) that he thought the cause was most probably a virus, (b) that there was a long period between exposure to it and a person becoming ill, (c) that there was no reliable screening test, (d) that there was no treatment for it, and (e) there was a high mortality rate: “a major objective must be to try to reduce the risk of transmitting the disease further … On the other hand, this new and to some extent theoretical hazard of using concentrates has to be set against the enormous benefits of such concentrates in haemophiliacs, especially for home therapy … the USA is the only country capable of providing the quantity of Factor VIII currently needed by UK haemophiliacs … The source of Factor VIII concentrates will need to be kept under constant review, as will blood donor policy, both by the medical profession and the relevant industrial concerns, to minimise or eliminate the risks.” Haemophilia Society The Bulletin No2 December 1983 pp11-12 PRSE0000411. It seems probable that the Society approached Dr Pinching (who was not a haemophilia clinician) because he had been quoted by The Mail on Sunday on 8 May 1983 as saying that he “wouldn’t dream of giving a patient American blood products. We have to find an alternative immediately.” The Mail on Sunday Action to Ban Danger Blood 8 May 1983 p1 PJON0000001_101. Dr Pinching thinks in retrospect that he may have qualified the first sentence of this quoted reply later, with words such as “unless there is no alternative in a clinical situation of definite clinical need” or similar. Written Statement of Professor Anthony Pinching para 7.1, para 7.4 WITN7652001
(2509) Letter from Professor Bloom to David Watters 25 July 1983 CBLA0000060_048
(2510) This very phrase was used by John Prothero in a letter of 15 July 1983 to Dr Colvin describing the main feeling of attendees at the World Haemophilia Congress in Stockholm, giving a picture of resigned acceptance. In fairness to him, he described the feeling of attendees at that conference as being that the risk was “minimal”. Letter from John Prothero to Dr Colvin 15 July 1983 BART0002363
(2511) Letter from the Irish Haemophilia Society to David Watters 27 May 1983 HSOC0014373_001
(2512) These are the words used by the Society itself in its closing submission: Closing Submissions of Haemophilia Society 16 December 2022 p53 SUBS0000065
(2513) Council of Europe Recommendation R-83-8 23 June 1983 p3 MACK0000307. David Watters Transcript 10 February 2021 pp38-40 INQY1000095
(2514) Letter from Dr Spence Galbraith to Dr Ian Field 9 May 1983 CBLA0000043_040
(2515) Letter from David Watters to Professor Bloom 19 July 1983 p2 CBLA0000060_048, Letter from Reverend Tanner to Professor Bloom 26 July 1983 BPLL0001351_089
(2516) Letter from Professor Bloom to David Watters 25 July 1983 CBLA0000060_048, Letter from Professor Bloom to Reverend Tanner 2 August 1983 CBLA0000060_050. It should be noted that the epidemic nature of the increase of AIDS infections in the population generally had continued, and by now an indicator of the extent to which the syndrome had become established in the UK was that the Terrence Higgins Trust was approaching its first anniversary: yet Professor Bloom modified neither his view that a response similar to that to hepatitis was indicated nor that the problem was largely one internal to the US.
(2517) Letter from David Watters to Steven Green at DHSS 15 August 1983 HSOC0020344. The highlighted point (emphasis added) was one of three main areas for discussion, the others being an assurance that there would be self-sufficiency within two years and that the Government would give “adequate support to research into AIDS in the UK.” The two words to which emphasis has been added show that the Society was not taking an approach of addressing a serious risk by taking precautions, but was advocating an approach akin to that of no action without “conclusive proof”.
(2518) The Society’s discussion as recorded in the minutes of the Executive Committee for 15 September 1983 strikes an odd note. After reporting the fact that the “first” AIDS-related death had “now been confirmed”, it immediately says: “The Co-ordinator presented the view that this fact would eventually reach the press and that the Society should immediately issue a statement to all members advising them of the death and pointing out all the steps taken so far by the Society in relation to AIDS. It was agreed that this would place people with haemophilia in a position of some strength when the subject hit the pages of the popular press and would serve to prevent some of the panic which followed the May reports in the media.” Minutes of Haemophilia Society Executive Committee meeting 15 September 1983 p2 HSOC0029476_028. The main concern appears not so much to have been the risks this indicated to other people with haemophilia, and what best should be done to avoid them, but to the consequences of press coverage.
(2519) Briefing paper of Lord Glenarthur meeting 8 September 1983 HSOC0020347, David Watters Transcript 10 February 2021 pp48-49 INQY1000095
(2520) In March 1983 the FDA recommended to pharmaceutical companies that blood products should thereafter only be made from plasma pools to which no one in a high-risk donor group had contributed. This did not prevent the distribution of products already in stock which had been made from “pre-March” (ie riskier) plasma. See the chapter Regulation of Commercial Factor Concentrates.
(2521) Minutes of Haemophilia Society Executive Committee meeting 15 September 1983 p2 HSOC0029476_028, reporting on the Society’s meeting with Lord Glenarthur.
(2522) Notes on Lord Glenarthur meeting 8 September 1983 HSOC0020347, David Watters Transcript 10 February 2021 pp53-55 INQY1000095
(2523) Peter Wetherell Transcript 25 May 2021 pp46-48 INQY1000122, building on the Written Statement of Peter Wetherell para 34 WITN3912001, Minutes of Haemophilia Society Council meeting 8 October 1983 p2 HSOC0019923_006
(2524) Minutes of Haemophilia Society Executive Committee meeting 6 December 1983 p2 HSOC0029476_031. Peter Wetherell’s evidence continued: “But once again, of course, we did note that it was within Professor Bloom’s area. Quietly noted, I think. Q. In what way? What do you mean by that? A. I think we all knew that that was Professor Bloom’s area. Q. Did that raise any particular concerns or discussion amongst the Committee? A. No, it didn’t. I mean, it does say, you know ... Professor Bloom was still, so far as I was aware at the time anyway, a chairman of the Medical Advisory Panel, a panel upon whom, you know, we relied, pretty much exclusively, along with the Centre Directors, that we were all attached to in our centres. Q. So were any questions raised by the Executive Committee about the advice that had previously been given by Professor Bloom in light of this new information? A. Not that I can recall.” Peter Wetherell’s evidence was that the Executive Committee was “undoubtedly too trusting” of his advice, and (further) was deferential to Reverend Tanner. Peter Wetherell Transcript 25 May 2021 pp54-55, p64, p66 INQY1000122
(2525) Notes on Lord Glenarthur meeting 8 September 1983 p48 HSOC0020347, David Watters Transcript 10 February 2021 p48 INQY1000095
(2526) Simon Taylor Transcript 26 May 2021 p6, pp8-9 INQY1000277, Haemophilia Society The Bulletin No4 November 1991 WITN4500002
(2527) David Watters Transcript 10 February 2021 pp68-69 INQY1000095
(2528) Haemophilia Society Haemofact No2 22 September 1983 p2 PRSE0004474. The fact sheet said in terms that “Our message remains unchanged” andhad in bold capitals: “THE ADVANTAGES OF TREATMENT FAR OUTWEIGH ANY POSSIBLE RISK.” This Haemofact also reported as a fact that “There remains one suspected case in Cardiff”, whereas it had been determined to be a probable case back in April.
(2529) It was wishful thinking in the light of the information and views current in mid 1983 to think that AIDS was unlikely to be transmitted by blood and blood products: the opposite was the case. This answer also shows that an influence in not alerting members to the likelihood that this was the case (what could be done if it were the case?) was logically irrelevant to whether it was true or not. If true, why should members have been insulated from that truth?
(2530) It is to be noted that the Society had in fact had advice to this very effect from Dr Pinching.
(2531) David Watters Transcript 10 February 2021 pp70-72 INQY1000095
(2532) There is evidence that apart from wishful thinking, a further reason for sending out the messages the Society did was to “alleviate anxiety” of members. Peter Wetherell described the purpose as being “to inform and try and reduce unnecessary anxiety”. Peter Wetherell Transcript 25 May 2021 p61 INQY1000122. The Haemophilia Society annual report for 1983 states that the Executive Committee “acted speedily to provide accurate information to all our members about AIDS”, and it boasts of “such effective means of communication as the special issues of HAEMOFACT” being the means to alleviate “much unnecessary anxiety”. It also formally states the policy “as being that the benefits arising from the continued use of blood products far outweighed any risk involved with regard to AIDS.”Haemophilia Society Annual Report 1983 p5 HSOC0019506
(2533) Minutes of Haemophilia Society Executive Committee meeting February 1984 p2 HSOC0029476_033. A policy of “wait and see” suggests that the Executive Committee would be given relevant information as and when it arose. The evidence, however, of Peter Wetherell shows that there may have been input from members of the Medical Advisory Panel which was not passed to it from the Society’s internal Blood Products Sub-Committee as arguably it should have been. Peter Wetherell Transcript 25 May 2021 p74 INQY1000122. Though it should be noted that he missed the relevant meeting, and the suggestion thus relates to information not being circulated between meetings.
(2534) The Haemophilia Society submission made this point, noting that Professor Bloom attended the December 1983 Medical Research Council Working Group which was briefed on information from the CDC about the wife of a person with haemophilia who had recently developed AIDS. Minutes of Medical Research Council Working Party on AIDS 20 December 1983 p2 DHSC0002239_079. Closing Submissions of Haemophilia Society 16 December 2022 p52 SUBS0000065. Regarding the meeting of 8 October 1983, Peter Wetherell said Professor Bloom “tried to give some sort of reassurances about sexual transmission, and it was unlikely that women could contract it. But, I think, you know, frankly, I mean, some eyebrows went up around the room at that point. You know, it was now there as an issue for members to reflect upon”, which shows that Professor Bloom knew of the possibility of sexual transmission, but that it was downplayed as a real risk. Peter Wetherell Transcript 25 May 2021 p49 INQY1000122. The Morbidity and Mortality Weekly Report for 7 January 1983 had reported that two women who were steady sexual partners of male intravenous drug users had themselves shown signs of AIDS, and commented that “Conceivably these male drug abusers are carriers of an infectious agent that has not made them ill but caused AIDS in their infected female sexual partners”, ie there was highly likely to be a viral cause of AIDS, transmissible by sex, as was also well known to be the case with Hepatitis B infection. Centers for Disease Control Immunodeficiency among Female Sexual Partners of Males with Acquired Immune Deficiency Syndrome (AIDS) – New York Morbidity and Mortality Weekly Report 7 January 1983 p2 BAYP0000028_011
(2535) When it was suggested in evidence to Peter Wetherell that one finds no sense of any grappling with the difficulties in the Society’s Council meeting minutes of 8 October 1983, he responded: “we didn’t have the ability, seemingly, to explicitly discuss, I think, how we were feeling about it as individuals.” Peter Wetherell Transcript 25 May 2021 p53 INQY1000122
(2536) The Guardian Panic and the blood 2 November 1983 DHSC0003824_107
(2537) Though it may be that this would be read as a reference to male homosexual practice, it nonetheless suggests that sex in general was capable of transmitting the infection. It is a little surprising that there is no evidence it was discussed at all, especially given the developing scepticism amongst some members of the views of Professor Bloom as he expressed them to the Society. The Society did not advise its members about safe sexual practices until Haemofact No7 in May 1985, when it advised the use of condoms “even if your partner is pregnant or male.” Haemophilia Society Haemofact No7 22 May 1985 p2 DHSC0001268
(2538) Haemophilia Society The Bulletin No1 1984 p2 PRSE0002925. The probable date of this is mid summer 1984. It is undated but comes after 23 March, which is a date referred to in The Bulletin. Since Ken Milne reported to the Executive Committee on behalf of the Blood Products Sub-Committee, and introduced a “short and helpful discussion on attitudes to commercial factor VIII”, Minutes of Haemophilia Society Executive Committee meeting 10 May 1984 p2 HSOC0029476_036, and was then asked to prepare a paper which the Executive Committee approved on 14 June 1984, Minutes of Haemophilia Society Executive Committee meeting 14 June 1984 p2 HSOC0029476_037, it was after those dates, but probably before the August holiday rush since the edition contained a box about holiday insurance, talking of the office being besieged each year with inquiries about it.
(2539) Haemophilia Society The Bulletin No1 1984 p2 PRSE0002925
(2540) It must also follow that concentrates made from US plasma collected earlier, at a time when there would have been less prevalence of infection in the UK, would be even riskier by comparison.
(2541) There is a similar lack of clarity about “risk” of disease and its “incidence” from the contributions of haemophilia clinicians in two successive publications in Haemofact No3 and No4. In May 1984, Dr Lee, then a senior registrar at the Royal Free Hospital, authored “Acquired Immunodeficiency Syndrome: An Update” in which she said “In Great Britain the number of haemophiliacs who have been reported with AIDS remain at 2. Thus the incidence is less than 1 in 1,000 patients at risk.” Haemophilia Society Haemofact No3 11 May 1984 p2 DHSC0001264. In September 1984, Dr Kernoff, the director of the Royal Free centre, said simply that “perhaps one reason why the risk of AIDS in haemophilia is so low (around 1 in 1000) is that many patients are immune to it.” Haemophilia Society Haemofact No4 24 September 1984 p2 PRSE0002824. Dr Kernoff conflated “risk” and “incidence” since the risk was not 1 in 1,000 – that was simply the incidence to date. Dr Lee’s words were less than clear. Interestingly, both contributions begin similarly, saying that: “The occurrence of acquired immunodeficiency syndrome (AIDS) in haemophilic patients has strongly suggested transmission of the order [sic] by blood products and epidemiological studies have suggested it may be related to a transmissible agent” (Dr Lee) and “The possibility that the acquired immunodeficiency syndrome (AIDS) might be caused by an unusual virus has always been a strong one” (Dr Kernoff), although the Society had spent the previous year expressing Professor Bloom’s view that there was no proof that blood products could transmit AIDS, and on that basis had continued to advise members to keep on taking factor concentrates. Haemophilia Society Haemofact No3 11 May 1984 p2 DHSC0001264
(2542) Haemophilia Society Haemofact No5 3 December 1984 p3 HCDO0000675
(2543) Haemophilia Society Haemofact No6 22 April 1985 p1 HSOC0008753
(2544) Emphasis added.
(2545) Haemophilia Society Haemofact No5 3 December 1984 p3 HCDO0000675
(2546) There is, however, reference to current practice favouring cryoprecipitate for those under four and for previously untreated patients and referring to the use of fresh frozen plasma for the same categories of patient with Haemophilia B and to DDAVP for patients with mild or moderate haemophilia or von Willebrand disorder. Haemophilia Society Haemofact No5 3 December 1984 p4 HCDO0000675. The Haemofact publications also mention that the Society was pressing for the use of heat-treated concentrates.
(2547) Since the auditors’ report is dated 17 May 1985.
(2548) Haemophilia Society Annual Report 1984 p6 HSOC0019505. It is important not to overlook the fact that many of those within the Society were themselves infected: Ken Milne, who worked tirelessly for the Society until his death in 1993, learned in 1985 that he had been infected with HIV as a result of his treatment with factor concentrates. Written Statement of Barbara Milne para 19, paras 36-38 WITN4580001
(2549) So far as revealed by the sources available to the Inquiry.
(2550) Minutes of Haemophilia Society Council meeting 24 November 1984 pp1-2 HSOC0019923_011
(2551) Haemophilia Society Annual Report 1986 p7 HCDO0000276_033
(2552) In general, the law is that it is not for an outsider (such as an incorporated charity) to make a claim for the benefit of someone who might have a claim against another. It is for the individual entitled to make such a claim to do so, and not a third party.
(2553) It must be borne in mind that at the time individuals with limited resources of their own would have to seek legal aid, and to do so would have to satisfy the Legal Aid Area Committee not only of their limited means but that their claim had “merit” (ie, in general terms, was more than 50% likely to succeed). For the only national body representative of people with haemophilia at the time to describe the chances as significantly less than that, on the basis of advice from Counsel, would make it very much more difficult to obtain funding for a claim, for the Area Committee would be bound to have regard to its view in assessing the merits.
(2554) Letters from David Watters to Professor Bloom and Dr Tony Aronstam 29 January 1987 HSOC0023111, Letter from David Watters to Dr Peter Jones 28 January 1987 PJON0000095_069, Letter from David Watters to Drs Elizabeth Mayne and Edward Tuddenham 16 February 1987 HSOC0023188
(2555) David Watters Transcript 11 February 2021 p82 INQY1000096
(2556) Haemophilia Society AIDS, Haemophilia and the Government October 1987 p2 BART0000603. The written statement of Simon Taylor says that the document was drafted by Dr Jones and David Watters with input from Reverend Tanner and himself, as well, possibly, as others. “It was a distillation of the Society’s case, based on the evidence of need that we had identified at the time, and as a result of the Government’s intransigence in acceding to any financial support for those infected as a result of successive government’s failures. Based on the advice that we had received from a number of sympathetic MPs, a clear statement of need, together with a costed proposal for financial support, was put together.” Written Statement of Simon Taylor 22 April 2021 paras 347-350 WITN4500001
(2557) The Society’s approach was highly unusual but there is no reason to infer that the trustees had any other motive. They were people who sacrificed a lot of their time – unpaid – to be of service to those who, like them, were closely affected by haemophilia.
(2558) Simon Taylor explained a double rationale for making the overall assessment public: that it was known to the Society’s membership that it had sought legal advice, and the expectation would be that it would become known; and that it was felt that the Government were keen to push those infected with HIV into taking legal action because that would inevitably be protracted and be “the easy way out” for it. Simon Taylor Transcript 26 May 2021 pp98-99 INQY1000277
(2559) David Watters Transcript 11 February 2021 para 81 INQY1000096
(2560) The right to confidentiality in legal advice given in contemplation of litigation is absolutely privileged against disclosure. Although this absolute protection would as a matter of law be sacrificed by sharing the document with a third party, it is right to note that the letter to clinicians enclosing a copy did ask them to regard the documents they were sent “in the very strictest confidence”. Letters from David Watters to Professor Bloom and Dr Aronstam HSOC0023111
(2561) Haemophilia Society The Bulletin No4 1987 p1HCDO0000276_043
(2562) Haemophilia Society Haemofact No17 14 December 1987 p4 HSOC0019910
(2563) Haemophilia Society Update No3 3 June 1989 p1 HCDO0000276_047
(2564) This was despite the fact that the Society was not party to the litigation. It was probably because there had been close liaison between the Executive Committee and the steering committee of lawyers involved on the plaintiffs’ behalf: such a liaison does not appear to be in dispute.
(2565) Minute from Strachan Heppell to the Minister’s Private Secretary 10 November 1989 DHSC0004415_155
(2566) Minute from Strachan Heppell’s colleague to the Minister’s Private Secretary 16 November 1989 DHSC0002536_061. David Watters had no recollection of having made such a call, and suggested it was the sort of topic that he would not have addressed in one. David Watters Transcript 11 February 2021 pp92-93 INQY1000096. However, it became plain the next day that indeed he had most probably done so, for the minute of the earlier meeting with Strachan Heppell had by then been turned up by the Inquiry team, and he recalled that meeting and accepted that the minute was a broadly accurate account of it. David Watters Transcript 12 Feb 2021 pp1-4 INQY1000097. The inference is that both the call and the meeting occurred, and the note of the phone call is accurate.
(2567) Letter from David Watters to Haemophilia Society members 24 October 1990 RFLT0000004
(2568) This is difficult to square with what had happened the previous autumn when the Society was naming figures for a potential settlement.
(2569) The use of the word “our” maintained an image of close involvement in what was taking place, despite the letter saying that the Society was not itself involved in negotiations.
(2570) Letter from David Watters to Haemophilia Society members 24 October 1990 RFLT0000004
(2571) Minutes of Haemophilia Society Executive Committee meeting 11 January 1990 p3 HSOC0010409. There may have been previous discussions of which no record exists.
(2572) By which it meant staff; further, at that time the settlement of the litigation in which it had played a role as intermediary was not yet concluded.
(2573) Minutes of Haemophilia Society Policy Committee meeting 9 June 1990 p2 HSOC0017204
(2574) Letter from Graham Barker (Policy and Development Manager) to Drs Charles Hay, Lee and Mayne and Professor Francis Preston 23 September 1991 pp2-3 HSOC0012305
(2575) This does not faithfully report what was actually being said to the Society. Whereas Dr Hay said this, Professor Preston told the Society that “Most authorities accept that, of those individuals who have been exposed to the hepatitis C virus, 50% will develop chronic liver disease and that approximately 20% of these patients will have cirrhosis of the liver. There is also now increasing evidence that hepatocellular carcinoma is a complication of chronic HCV liver disease.” In retrospect, Simon Taylor thinks that the risk was being downplayed by some of the clinicians from whom advice was sought. Simon Taylor Transcript 26 May 2021 p59 INQY1000277, Letter from Dr Hay to Graham Barker 7 October 1991 pp4-9 HSOC0003297, Letter from Professor Preston to Graham Barker 16 October 1991 pp14-15 HSOC0003297
(2576) The use of this phrase shows a lack of knowledge as to the extent to which Hepatitis C caused progressive liver disease: it might be thought that the realistic worst should have been assumed rather than the best.
(2577) Minutes of Haemophilia Society Executive Committee meeting 14 November 1991 p3 HSOC0010385
(2578) David Watters accepted when it was put to him in testimony that this is what the minutes show, though he had no broader recollection of his own. David Watters Transcript 12 February 2021 pp24-25 INQY1000097. The letter to the clinicians said they wanted to be reassuring: “We want to be able to reassure our members with some clear factual statements. We would, in particular like to be able to reassure parents with children under a certain age, that provided they have only received certain blood products they are not at risk of hepatitis. Can we reassure others that although they may have hepatitis they do not require any treatment and that there is little for them to worry about? I would be grateful for any information or references you might have on the scale and nature of hepatitis and haemophilia. I would welcome any ideas you might have on what reassuring statements we might be able to make.” Letter from Graham Barker to Dr Hay 23 September 1991 p2 HSOC0003297
(2579) Indeed, David Watters could not recall any direct consultation with the membership as a whole. David Watters Transcript 12 February 2021 p27 INQY1000097. However, there was a weekend meeting in Liverpool in November 1990, at which workshop leaders presented their suggested priorities for the coming year. The highest priorities remained the HIV compensation campaign and the quality of care for people with haemophilia; a close second was the impact of the NHS review; and the next priorities included “the problems of hepatitis for people with haemophilia who were suffering severe liver damage.” Minutes of Council of the Haemophilia Society meeting 25 November 1990 p4 HSOC0019923_034
(2580) Indeed, the Society’s own HCV worker seems to have had a view that from 1986 onwards all Factor 8 concentrate was treated such that any hepatitis virus was inactivated. This was not the case, certainly so far as commercial concentrates were concerned, nor as regards to Scottish concentrates until the development of Z8 in 1987. The report Haemophilia and Hepatitis C stated “Since 1986, heat treatment of blood products has minimised the risk that they harbour HCV. Therefore, those treated only after 1986 should be safe from hepatitis C infection.” Haemophilia Society Haemophilia and Hepatitis C 1995 p7 WITN6392250
(2581) Written Statement of David Watters para 163 WITN3429001
(2582) Minutes of Haemophilia Society Committee B meeting 15 July 1993 p4 HSOC0010414
(2583) Minutes of Haemophilia Society Hepatitis Task Group meeting 16 September 1993 HSOC0023467_006
(2584) Evidence of David Tonkin, chairman of the Manor House Group. Written Statement of David Tonkin para 13 WITN1567008. The name comes from a group of cottages in Nantwich, in one of which the Manor House Group had its formative meeting.
(2585) Reported as such not only by David Tonkin in his statement but also by Karin Pappenheim, CEO of the Society between 1998 and 2004. Written Statement of Karin Pappenheim paras 21-23 WITN4504001. She also described tensions between the Manor House Group and the Society which led to the Manor House Group later separating from the Society.
(2586) The minutes of the Hepatitis Task Group meeting in December 1995 record that congratulations were due to the Manor House Group for securing the meeting on 18 December 1995. Minutes of Haemophilia Society Hepatitis Task Group meeting 13 December 1995 p2 HSOC0003755
(2587) On 16 November 1994, Norma Guy suggested this but there was opposition. Minutes of Haemophilia Society Service Committee meeting 10 November 1994 p2 HSOC0023353
(2588) The Independent Contaminated blood kills 12 16 November 1994 p9 HSOC0026719
(2589) Haemophilia Society press release 16 November 1994 HSOC0021550. The Independent the next day reported that the Government resisted calls to compensate Hepatitis C victims, and in an editorial added “For the Government to rule out all compensation at this stage, as it did yesterday, is both insensitive and unfair”. The Independent Government resists call to compensate hepatitis C victims 17 November 1994 HSOC0016716_012
(2590) Haemophilia Society The campaign in the media p1 HSOC0026719
(2591) Written Statement of Anne Anakin and Gregory Murphy paras 121-126 WITN1944002
(2592) The Society had resolved to seek “the maximum help for people affected by hepatitis” and written to members to inform them that they were seeking “equitable treatment in financial terms” with those infected with HIV. Haemophilia Society policy statement 21 November 1994 HSOC0010091_004, Haemophilia Society special mailing 23 November 1994 p2 HSOC0005112_001
(2593) Karin Pappenheim Transcript 27 May 2021 p5 INQY1000123
(2594) Written Statement of Karin Pappenheim para 121 WITN4504001
(2595) Written Statement of Karin Pappenheim para 122 WITN4504001, Letter from Frank Dobson to Chris Hodgson 28 July 1998 DHSC0016534
(2596) Hepatitis C Campaign: future directions 25 September 1998 HSOC0016864
(2597) Especially Susan Deacon, Minister for Health.
(2598) Minute from Health Care Policy Division 15 July 1999 SCGV0000176_118, Susan Deacon Transcript 29 July 2022 pp19-36 INQY1000237
(2599) Minute from Health Care Policy Division 5 August 1999 WITN4436004. This minute also revealed that the UK Government expected that it would be found liable in court to compensate individuals who had contracted Hepatitis C from transfusions given in England between May 1991 and September 1991 when a reasonably effective test for the virus was available, and so struck a rather different tone from that adopted in the July minute (see the preceding footnote).
(2600) Chris Hodgson, Philip Dolan and Karin Pappenheim, respectively. Note of Haemophilia Society and Minister for Health meeting WITN4436005
(2601) Letter from the Haemophilia Society to Susan Deacon 27 October 2000 HSOC0011980. See the chapter on Scotland.
(2602) Minutes of Haemophilia Society Extraordinary Trustee meeting 19 January 2001 p3 WITN4500028
(2603) Minutes of Haemophilia Society HCV Campaign meeting 11 September 2000 p4 HSOC0029689_034
(2604) Weber Shandwick. This gave way, on cost grounds, to the use of a single low-cost freelancer for selected public affairs and campaign functions. See Minutes of Board of Trustees meeting 20 March 2002 pp3-4 HSOC0029689_043 and Karin Pappenheim Transcript 27 May 2021 p127 INQY1000123
(2605) See the chapter Skipton Fund.
(2606) Karin Pappenheim Transcript 27 May 2021 pp134-135 INQY1000123
(2607) Letter from Karin Pappenheim to Richard Gutowski 17 October 2003 DHSC0004520_002. See also Karin Pappenheim Transcript 27 May 2021 p142 INQY1000123
(2608) When told of UKHCDO’s collective view in 2006 that “a public enquiry … is not in the patients’ best interests and is likely to harm rather than enhance patient care” (Letter from Dr Hay to Margaret Unwin 27 September 2006 HSOC0001265) the Haemophilia Society did not defer to the UKHCDO as it had appeared to do in the early 1980s. This may support a view that the Society had learned a lesson from the events of that time.
(2609) The Society may have believed that the goal of self-sufficiency was going to be achieved: its April 1977 Bulletin reported that “The Society now has a date to aim for from both the Department of Health and the Medical Research Council with regard to National Health Service self-sufficiency in Factor VIII.” Haemophilia Society The Bulletin No2 April 1977 p1 HSOC0022508. In December 1980 Ken Milne wrote to Dr Richard Lane expressing the Society’s concern at the large amounts of commercial concentrates being imported and adding “You may perhaps know that the Society has been able in the past to meet with the Health Minister at the D.H.S.S. to discuss various topics of concern to us. We have it in mind to raise the question of Factor VIII supply and demand at the next opportunity, and I have been asked to coordinate a small (three-man) ‘fact-finding’ group on this subject.” He asked for a meeting with Dr Lane. Letter from Ken Milne to Dr Lane 17 December 1980 CBLA0001220
(2610) This is indicated by the terms of a note prepared in advance for a meeting with Dr Gerard Vaughan, Minister of Health, on 21 October 1981 at which the Society aimed to press a case for self-sufficiency. The note makes no reference to the dangers of hepatitis, even though it is plainly thought desirable that concentrates should be manufactured which were free of it. Briefing paper of Dr Gerard Vaughan meeting 21 October 1981 HSOC0020339
(2611) An example from the Newcastle branch of the Society (an active branch) was its newsletter for Autumn 1980. Dr Jones, director of the local haemophilia centre, wrote an “update” on hepatitis, in which (with the express intent of reassuring families who had concern) he quoted himself, when as chair of an international symposium in Tel-Aviv the previous year he had asked “Is chronic hepatic damage really one of the expected side effects of intensive, multi-donor transfusion, or do we play with fears based on serological and histological findings with little relevance to clinical fact?” and answered his own question by saying “it is interesting to note that neither the serological nor the abnormal biopsy findings reported in haemophilia seem to match the incidence of clinically apparent disease, and there has been no increase in the death rate from liver failure, even in those patients who have received numerous transfusions of commercial, large pool blood product for over a decade … although risks remain they are probably of less consequence than might be suggested by the literature, and are certainly outweighed by the need to treat haemophilic bleeding in the only way we know – by the rapid replacement of the relevant clotting factor.” Haemophilia Society Northern Branch newsletter autumn 1980 HSOC0021600. It could not be expected that the Society would have noticed that in dealing with a question about chronic disease, initially indicated by changes which would produce no symptoms in themselves (ie asymptomatic), he should rely on the (absence of) clinical presentation (ie symptomatic) in the individuals concerned. Symptomatology in chronic disease may often depend on the time lag between infection and its consequence: the underlying assumption in what he was saying was that he would have expected it by now if it were to happen. However, this would need to be made clear, and would have to be reconciled with previous papers showing how long term many of the consequences of hepatitis could be. His somewhat dismissive contribution in 1980 echoed one he had made following the World in Action documentary screened in December 1975 in the Northumbrian branch spring newsletter of 1976. Haemophilia Society Northumbrian Branch newsletter spring 1976 p3 HSOC0021641
(2612) David Watters Transcript 9 February 2021 p72 INQY1000094
(2613) Dr Diana Walford was clear on this in her evidence but nonetheless the evidence is that the Society understood, erroneously, that non-A non-B Hepatitis was mild; that NHS concentrates from voluntary non-remunerated donors were “pure as the driven snow”, and preferable to US commercial concentrates from paid donors; that donations from prisons and military donors were concerning; and that after the commitments made by the Government when Dr Owen was the Minister, self-sufficiency had been less and less of a priority for expenditure in succeeding administrations, but that there had been a renaissance in 1981-82 with the Government’s now enthusiastic conversion to the policy. The evidence of Dr Walford regarding her minute dated 15 September 1980 was that she “copied it pretty widely”. Letter from Dr Walford to Mr Harley p1 WITN0282008. See also Dr Diana Walford Transcript 19 July 2021 pp110-114 INQY1000136, David Watters Transcript 9 February 2021 pp78-83 INQY1000094
(2614) Agenda for Haemophilia Society meeting 21 October 1981 DHSC0002490_047
(2615) There is also force in a complaint made by a witness who was a trustee in 2006-2007, speaking about the 1970s and 1980s, that “There was no challenge offered by the Society to the UKHCDO’s way of doing things and there was an acceptance of the concept that hepatitis was the price to be paid for clotting therapies. This acceptance was naïve because even if one accepts that hepatitis was perceived as harmless (which I do not) there was no consideration given to the fact that eventually, a new blood-borne pathogen would emerge and that haemophiliacs would inevitably be infected with it.” Written Statement of ANON para 11 WITN1387015
(2616) The first reference to non-A non-B Hepatitis in the Society’s publications to its members was one of its Bulletins in 1982. David Watters Transcript 9 February 2021 pp81-84 INQY1000094, Haemophilia Society The Bulletin No1 1982 BART0002327_001
(2617) The Society acknowledged that with hindsight some early Society publications downplayed the risks, reflecting the medical views they were receiving. Closing Submissions of Haemophilia Society 16 December 2022 p138 SUBS0000065
(2618) Simon Taylor Transcript 26 May 2021 p102 INQY1000277